Abstract
Summary
Background
Cash transfers have been proposed as an intervention to reduce HIV-infection risk for young women in sub-Saharan Africa. However, scarce evidence is available about their effect on reducing HIV acquisition. We aimed to assess the effect of a conditional cash transfer on HIV incidence among young women in rural South Africa.
Methods
We did a phase 3, randomised controlled trial (HPTN 068) in the rural Bushbuckridge subdistrict in Mpumalanga province, South Africa. We included girls aged 13–20 years if they were enrolled in school grades 8–11, not married or pregnant, able to read, they and their parent or guardian both had the necessary documentation necessary to open a bank account, and were residing in the study area and intending to remain until trial completion. Young women (and their parents or guardians) were randomly assigned (1:1), by use of numbered sealed envelopes containing a randomisation assignment card which were numerically ordered with block randomisation, to receive a monthly cash transfer conditional on school attendance (≥80% of school days per month) versus no cash transfer. Participants completed an Audio Computer-Assisted Self-Interview (ACASI), before test HIV counselling, HIV and herpes simplex virus (HSV)-2 testing, and post-test counselling at baseline, then at annual follow-up visits at 12, 24, and 36 months. Parents or guardians completed a Computer-Assisted Personal Interview at baseline and each follow-up visit. A stratified proportional hazards model was used in an intention-to-treat analysis of the primary outcome, HIV incidence, to compare the intervention and control groups. This study is registered at ClinicalTrials.gov (NCT01233531).
Findings
Between March 5, 2011, and Dec 17, 2012, we recruited 10 134 young women and enrolled 2537 and their parents or guardians to receive a cash transfer programme (n=1225) or not (control group; n=1223). At baseline, the median age of girls was 15 years (IQR 14–17) and 672 (27%) had reported to have ever had sex. 107 incident HIV infections were recorded during the study: 59 cases in 3048 person-years in the intervention group and 48 cases in 2830 person-years in the control group. HIV incidence was not significantly different between those who received a cash transfer (1.94% per person-years) and those who did not (1.70% per person-years; hazard ratio 1.17, 95% CI 0.80–1.72, p=0.42).
Interpretation
Cash transfers conditional on school attendance did not reduce HIV incidence in young women. School attendance significantly reduced risk of HIV acquisition, irrespective of study group. Keeping girls in school is important to reduce their HIV-infection risk.
Funding
National Institute of Allergy and Infectious Diseases, National Institute of Mental Health of the National Institutes of Health.
Introduction
Young women in sub-Saharan Africa face an alarmingly high burden of HIV infection. In many parts of sub-Saharan Africa, HIV prevalence increases rapidly in women between the ages of 15 and 24 years, with a quarter or more of young women (aged 15–24 years) infected with HIV by the time they reach their early to mid-twenties.1–4 In view of the high infection rates, young women in this age group are a crucially important population to target for prevention efforts.4
Several behavioural and structural factors have been associated with HIV infection risk in young women in these settings, with education being highlighted as a key factor to reduce HIV infection risk.5,6 Young women who complete more years of schooling are less likely to become HIV infected than young women who complete fewer years of schooling.5,7–10 In South Africa, young women aged 15–24 years who completed high school were three times less likely to have HIV.5 In Botswana, each additional year of secondary schooling led to an absolute reduction in the cumulative risk of HIV infection in women.10 Despite increasing evidence that keeping girls in school for longer appears to reduce their risk of HIV infection, many barriers exist for young women to attend schooling in many African countries, including school fees, cost of school uniforms, family and domestic responsibilities, and societal norms which are not supportive of girls’ education.11
Programmes in which cash is provided by the government to poor households for poverty alleviation have been found to be effective in increasing school attendance rates, particularly for girls.12,13 When conditioned on school attendance, cash transfers have shown promise in keeping girls in education.13 Observational data from a cash transfer programme provided by the Government of South Africa showed that young women living in homes that were receiving the cash transfer were less likely to report having a partner 5 or more years older or be engaging in transactional sex.14 Because schooling is associated with reduced HIV risk, and cash transfers have been shown to decrease school dropout, interest has been raised in these cash transfer programmes to reduce HIV risk behaviours and HIV infections. A cluster-randomised trial15 in Malawi showed that young women receiving cash transfers (both unconditional and conditional on school attendance) had significantly lower HIV prevalence and were less likely to engage in weekly sex, or to have a sex partner 25 years or older compared with women not receiving the cash transfers. Although education is one mechanism through which cash transfers might help to reduce HIV risk, these programmes have been hypothesised to help reduce young women’s dependence on male partners, particularly on older men who often provide gifts or cash to young women in exchange for sex.
The HIV Prevention Trials Network (HPTN) 068 study in rural South Africa aimed to evaluate the efficacy of cash transfer, conditional on school attendance, to reduce HIV incidence.
Methods
Study design
We did a phase 3, randomised controlled trial (HPTN 068), undertaken at the South African Medical Research Council and University of the Witwatersrand Rural Public Health and Health Transitions Research Unit which runs the Agincourt Health and Socio-Demographic Surveillance System (HDSS) site in the rural Bushbuckridge subdistrict in Mpumalanga province, South Africa.13 In 2012, HIV prevalence in the study area was 5.5% in women aged 15–19 years, rising to 27% by age of 20–24 years, and 46% by 35–39 years.16 This is an area characterised by high levels of unemployment, poverty, and migration for work.17
Institutional Review Board approval for this study was obtained from the University of North Carolina at Chapel Hill and the University of the Witwatersrand Human Research Ethics Committee.
Participants
Women aged 13–20 years were included in the HPTN 068 study if they were enrolled in school grades 8–11 of the South African educational system, not married or pregnant, able to read, having the documentation necessary to open a bank account, having a parent or guardian with documentation necessary to open a bank account, and currently residing in the study area and intending to remain until trial completion. Young women who tested positive for HIV infection at baseline were enrolled in the study to avoid inadvertent disclosure of HIV status, but excluded from the main analysis.
Young women between ages 13 and 20 years and in school were identified from the Agincourt HDSS and visited at their homes to assess their eligibility to participate. Enrolment was limited to one young woman from each household. If more than one eligible young woman was present, the next birthday method was used to select the individual. The next birthday method involves selection of the person in the household (of those eligible) who will have the next birthday, which is a random selection method. We included young women up to the age of 20 years at baseline because repeating school grades is common in South Africa. As a result, some women are in school beyond the usual age for that grade. Although the maximum age for secondary school attendance is 20 years, it does not seem to be widely enforced. Children are allowed to repeat a year in each phase of school; however, repetition of more than 1 year in each phase is common. Thus in wanting to include young women who were enrolled in grades 8–11 we allowed an age band that would capture as many students as possible.
Each young woman and her parent or guardian provided written informed consent at the home visit. Written assent was obtained for young women younger than 18 years. Consent and assent forms were available in English and Shangaan.
Randomisation and masking
Individual randomisation took place after all baseline study procedures were completed. Young women and their parent or guardian were randomly assigned (1:1) by use of block randomisation to receive a monthly cash transfer conditional on school attendance or no cash transfer. Numbered sealed envelopes containing a randomisation assignment card were numerically ordered using block randomisation. The participant was considered enrolled in the study once the envelope was assigned to a study group. Teachers and administrators were masked to study enrolment; rosters were collected for the participant’s entire class to avoid disclosure of study group or participation. Participants and parents or guardians were not masked to assignment.
Procedures
Young women randomly assigned to the intervention group received 100 rands (R; about US$10 in 2012), and their parent or guardian received R200 (about $20) every month, conditional on the young woman attending 80% of school days per month. Young women were eligible to receive the cash each month in which they met the attendance criteria as long as they were eligible to attend school and up to a maximum of 3 years. The funds were deposited directly into bank accounts for the young woman and parent or guardian separately. Young women and their parents or guardians randomly assigned to the control group received no cash payments. At baseline, the median monthly household expenditure per person was R294.75. We chose R300 per month as the cash transfer amount because it was similar to the South African Government’s social protection grant, the Child Support Grant, which in 2012 provided R280 per month per child younger than 18 years; by 2015 the amount provided had increased to R330.
At baseline, the participants completed an Audio Computer-Assisted Self-Interview (ACASI), before HIV test counselling, HIV and herpes simplex virus (HSV)-2 testing, and after HIV post-test counselling. Participants were seen annually at 12, 24, and 36 months until the study completion date or their planned high-school completion date, whichever came first. Each study visit included the ACASI, HIV and HSV-2 testing (if negative at the previous visit), and HIV pretest and post-test counselling. A Computer-Assisted Personal Interview (CAPI) was completed with the parent or guardian at baseline and at each annual follow-up visit.
An additional follow-up visit was scheduled around the time of the young woman’s graduation from high school if she missed her scheduled visit that year or if her previous visit that year was before Oct 1. Only HIV and HSV-2 testing took place at this visit.
HIV testing was undertaken at the study site at all visits. HIV screening was done with two HIV rapid tests completed in parallel (the Determine HIV-1/2 test [Alere Medical Co, Matsudo-shi, Chiba, Japan] and the US Food and Drug Administration [FDA]-cleared Uni-gold Recombigen HIV test [Trinity Biotech, Bray, County Wicklow, Ireland]). If both HIV rapid tests were non-reactive, no further testing was done at that study visit. If one or both tests were reactive or positive, confirmatory HIV testing was done with the FDA-cleared GS HIV-1 western blot assay (Bio-Rad Laboratories Inc, Redmond Redmond, WA, USA). If the western blot was positive or indeterminate, a new blood sample was drawn within 2 weeks of the first test result for repeat testing. If a participant was confirmed to be HIV-infected (if both western blot tests were positive), no further HIV testing was done. If HIV status was not clear, further site testing was done with guidance from the HPTN Laboratory Center. Samples from all participants at all study visits were tested at the HPTN Laboratory Center to confirm baseline HIV status and incident HIV infections. Samples were first tested using the fourth generation Abbott ARCHITECT HIV Ag/Ab COMBO test (Abbott Laboratories, Abbott Park, IL, USA). Additional testing was done to confirm HIV infection for reactive samples with the FDA-cleared GS HIV-1 western blot assay or the Aptima HIV-1 RNA qualitative assay (Hologic Inc, Marlborough, MA, USA). If HIV seroconversion was documented, the sample from the previous visit was tested with the Aptima HIV-1 RNA assay.
HSV-2 testing was completed at all visits using the Herpes Simplex Virus Type 2 IgG ELISA assay (Kalon Biological Ltd, Guildford, UK) with prevalent infection an index cutoff of 1.5. If the HSV-2 test was positive, no further HSV-2 testing was done at the site. HSV-2 results were confirmed retrospectively at the HPTN Laboratory Center using the same assay. HSV-2 seroconverters were identified as individuals who were negative at enrolment and had an index value increase of more than 1.0.18
Social harms were assessed at each follow-up visit by a counsellor. If a social harm was reported and confirmed, it was reported to the institutional review board and an HPTN subcommittee for social harms. To provide participants with privacy and comfort in reporting social harms, a series of questions designed to assess these were added to the ACASI questionnaire in February, 2014.
In the intervention group, school attendance was assessed monthly with official school attendance registers from all 26 high schools involved in the study. These data were used to establish whether the monthly payment should be paid. In the control group, attendance was assessed in February, May, and August of each year, using data from the same attendance registers. We chose these three months to be representive of the school year and because they are not months with major school holidays or exams.
Outcomes
The primary outcome was HIV incidence, which was established at each follow-up based on measurement of HIV infection at baseline and each follow-up visit. Key secondary outcomes included: HSV-2 incidence; school attendance; number of self-reported vaginal sex acts in the past 3 months; age difference between the young woman and any of the past three sexual partners; age of coital debut; incident pregnancy; number of unprotected sex acts in the past 3 months. All secondary endpoints were measured at each follow-up visit and at baseline.
Physical violence from a partner in the past 12 months and transactional sex were not prespecified as outcomes in the protocol; however, we felt it was important to include these outcomes because there was concern that cash transfers might increase risk of violence for young women from partners, the association between cash transfers and intimate partner violence is of interest to global violence prevention groups, and transactional sex has been shown to be a main outcome that is affected in other cash transfer programmes. Physical violence from a partner in the past 12 months and transactional sex were measured at each follow-up visit.
Statistical analysis
The sample size needed for the study was 2430 young women who were not infected with HIV. We estimated that the following groups of HIV-uninfected young women would be eligible and would enrol in the study: about 1822 young women of ages 13–20 years, in grades 8, 9, and 10 of school who would be followed up for 3 years, and an additional 608 young women in grade 11 who would be followed up for 2 years. We assumed HIV incidence in the control group would be 3%, which was computed as the mean of the estimated grade-specific incidences of 0% for grade 8, 1% for grade 9, 2% for grade 10, 3.5% for grade 11, and 5% for grade 12 (weighted by the expected person-years in each grade). With the assumption of a 1:1 ratio randomisation, loss to follow-up of 5% per year, and HIV prevalence at enrolment of 4%, the study had 84% power to detect a 40% effect (relative risk [RR] 0.6).
The primary analysis of HIV incidence was a modified intention-to-treat analysis as young women who were HIV positive at enrolment were excluded. All young women without HIV infection at enrolment were included. A Cox proportional hazards model was fitted with time to the first positive HIV test result as the outcome, intervention group as the predictor, and stratified by grade at enrolment. Significance of the intervention was assessed using a value of 0.05 (two-sided) after verification of the validity of the proportional hazards assumption.19 A secondary analysis was done in which inverse probability weights (based on probability of retention in the study) were estimated and used to adjust for the differential retention in the study.20 This analysis gave a virtually identical hazard ratio (HR) for the intervention effect (data not shown). All analyses were completed with SAS (version 9.4).
The secondary endpoints of time to HSV-2 detection, time to permanent school dropout, and time to coital debut after study enrolment (in girls who reported no sex at enrolment) were also analysed by use of a Cox proportional hazards model with the intervention group as the predictor, and stratified by grade at enrolment. School attendance was computed as number of days attended divided by number of days expected to attend for each participant for each month. These values were compared between groups with generalised estimating equations (GEE) with identity link, normal distribution, and robust variance to account for repeated measures on each participant. The school attendance analysis was limited to months in which data were collected for both study groups. Physical violence from a partner in the past 12 months, unprotected sex in the past 3 months, transactional sex, older partners, and having a sex partner in the past 12 months were analysed with log-binomial regression and robust variance to account for repeated measures on each participant. Pregnancy was measured as any pregnancy during the study and was analysed with log-binomial regression.
The study was reviewed by a Data Safety Monitoring Board (DSMB) at four timepoints during the study. The DSMB was given information on enrolment, retention, participant demographics, and baseline risk, as well as efficacy and safety results for each visit. An interim monitoring plan was used that called for a single interim efficacy analysis at about 24 months into the (projected) 3-year study. An O’Brien-Fleming boundary21 was used to establish the stopping rule for efficacy. No formal stopping rule in relation to safety was implemented.
This trial was registered with ClinicalTrials.gov, number NCT01233531.
Role of the funding source
The funder of the study reviewed and approved the protocol and protocol revisions. The sponsor participated in study design and oversaw the monitoring of trial implementation and reviewed the final report, but had no role in data collection, data analysis, or data interpretation. All authors had full access to all the study data and the corresponding author (AP) had full responsibility for the decision to submit for publication.
Results
We recruited participants between March 5, 2011, and Dec 17, 2012. Of 10 134 young women screened for eligibility, 2537 were eligible, enrolled, and randomly assigned to a study group (figure 1). 7597 participants were ineligible and not enrolled. Of the 2537 participants who were randomly assigned to receive a cash transfer programme (n=1225) or the control group (n=1223), 2448 (96%) were not infected with HIV at baseline. 2328 (95%) of 2448 participants without HIV infection had at least one follow-up visit, including 1114 (48%) girls in the control group and 1214 (52.1%) girls in the intervention group (figure 1). Retention at the planned final visit was 87% in the control group and 95% in the intervention group.
Figure 1. Trial profile.
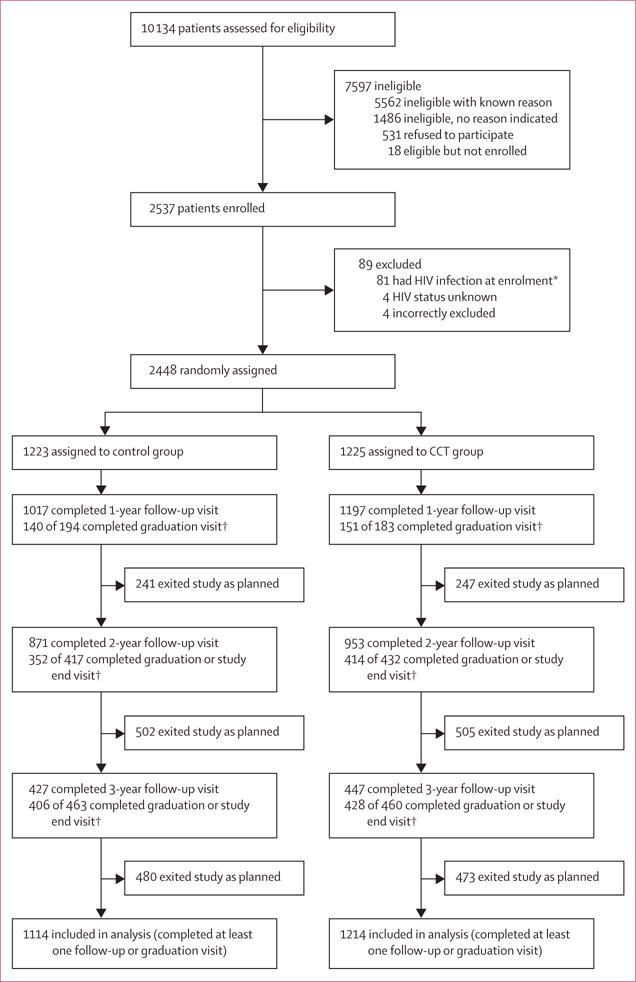
CCT=conditional cash transfer. *Patients with HIV were followed up, but are not reported in the retention. †Denominator is the expected number of graduation or study end visits; expected numbers depend on date of last follow-up visit and grade at enrolment.
At baseline the median age of participants was 15 years (IQR 14–17) and participants were evenly distributed across all school grades (8–11; table 1). The study population was balanced on key sociodemographic and behavioural outcomes between study groups. School enrolment and completion for young women aged 16–20 years in 2011 in the HDSS, when we started the trial, was 86%.
Table 1.
Baseline characteristics of study participants of young women (aged 13–20 years) in HPTN 068
| Total (N=2533) | Conditional cash transfer group (n=1261) | Control group (n=1272) | |
|---|---|---|---|
| Age (years) | 15 (14–17) | 15 (14–17) | 15 (14–17) |
|
| |||
| School grade enrolment | |||
| Grade 8 (13–15 years) | 640 (25%) | 322 (26%) | 318 (25%) |
| Grade 9 (14–16 years) | 682 (27%) | 327 (26%) | 355 (28%) |
| Grade 10 (16–17 years) | 699 (28%) | 354 (28%) | 345 (27%) |
| Grade 11 (17–18 years) | 512 (20%) | 258 (21%) | 254 (20%) |
|
| |||
| School days missed per month | |||
| 0–2 days | 2345 (93%) | 1160 (92%) | 1185 (93%) |
| ≥3 days | 166 (7%) | 84 (7%) | 82 (6%) |
| Missing | 22 (0.9%) | 17 (1%) | 5 (0.4%) |
|
| |||
| Orphan | |||
| Both parents alive | 1723 (68%) | 850 (67%) | 873 (69%) |
| Single orphan | 575 (23%) | 287 (23%) | 288 (23%) |
| Double orphan | 117 (5%) | 62 (5%) | 55 (4%) |
| Missing | 118 (5%) | 62 (5%) | 56 (4%) |
|
| |||
| Food insecurity* | |||
| Yes | 862 (34%) | 412 (33%) | 450 (35%) |
| No | 1649 (65%) | 839 (67%) | 810 (64%) |
| Missing | 22 (0.9%) | 10 (0.8%) | 12 (0.9%) |
|
| |||
| HIV infection status | |||
| Positive | 81 (3%) | 36 (3%) | 45 (4%) |
| Negative | 2448 (97%) | 1225 (97%) | 1223 (96%) |
| Missing | 4 (0.2%) | 0 | 4 (0.3%) |
|
| |||
| Herpes simplex virus-2 infection status | |||
| Positive | 120 (5%) | 59 (5%) | 61 (5%) |
| Negative | 2409 (95%) | 1199 (95%) | 1210 (95%) |
| Missing | 4 (0.2%) | 3 (0.2%) | 1 (0.1%) |
|
| |||
| Ever pregnant | |||
| Yes | 223 (9%) | 110 (9%) | 113 (9%) |
| No | 2279 (90%) | 1138 (90%) | 1141 (90%) |
| Missing | 31 (1%) | 13 (1%) | 18 (1%) |
|
| |||
| Ever had vaginal sex | |||
| Yes | 672 (27%) | 334 (27%) | 338 (27%) |
| No | 1851 (73%) | 924 (73%) | 927 (73%) |
| Missing | 10 (0.4%) | 3 (0.2%) | 7 (0.6%) |
|
| |||
| Early age of debut (<15 years) | |||
| Yes | 166 (7%) | 85 (7%) | 81 (6%) |
| No | 2347 (93%) | 1170 (93%) | 1177 (93%) |
| Missing | 20 (0.8%) | 6 (0.5%) | 14 (1%) |
|
| |||
| Lifetime sexual partners | |||
| 0 | 1830 (72%) | 916 (73%) | 914 (72%) |
| 1 | 353 (14%) | 163 (13%) | 190 (15%) |
| ≥2 | 323 (13%) | 171 (14%) | 152 (12%) |
| Missing | 27 (1%) | 11 (0.9%) | 16 (1%) |
|
| |||
| Unprotected vaginal sex acts† | |||
| 0 | 481/693 (69%) | 228/341 (67%) | 253/352 (72%) |
| 1 | 80/693 (12%) | 42/341 (2%) | 38/352 (11%) |
| 2 | 47/693 (7%) | 27/341 (8%) | 20/352 (6%) |
| ≥3 | 62/693 (9%) | 32/341 (9%) | 30/352 (9%) |
| Missing | 23/693 (3%) | 12/341 (4%) | 11/352 (3%) |
|
| |||
| Age difference with partner†‡ | |||
| ≥ 5 years older | 138/693 (20%) | 67/341 (20%) | 71/352 (20%) |
| <5 years older | 540/693 (78%) | 269/341 (79%) | 271/352 (77%) |
| Missing | 15/693 (2%) | 5/341 (1%) | 10/352 (3%) |
|
| |||
| Transactional sex†‡ | |||
| Yes | 97/693 (14%) | 45/341 (13%) | 52/352 (15%) |
| No | 585/693 (84%) | 292/341 (86%) | 293/352 (83%) |
| Missing | 11/693 (2%) | 4/341 (1%) | 7/352 (2%) |
|
| |||
| Ever physical violence | |||
| Yes | 431 (17%) | 227 (18%) | 204 (16%) |
| No | 2043 (81%) | 1005 (80%) | 1038 (82%) |
| Missing | 59 (2%) | 29 (2%) | 30 (2%) |
|
| |||
| Ever sexual violence | |||
| Yes | 113 (5%) | 47 (4%) | 66 (5%) |
| No | 2377 (94%) | 1195 (95%) | 1182 (93%) |
| Missing | 43 (2%) | 19 (2%) | 24 (2%) |
|
| |||
| Household receiving Child Support Grant | |||
| Yes | 2005 (79%) | 987 (78%) | 1018 (80%) |
| No | 527 (21%) | 273 (22%) | 254 (20%) |
| Missing | 1 (0.04%) | 1 (0.1%) | 0 |
Data are n (%), or median (IQR).
Worried about having enough food in the past 12 months.
In those who are sexually active, as defined by self-reported vaginal or anal sex history (n=693).
Between any of past three partners.
107 incident HIV infections were reported during the study (59 in the intervention group vs 48 in the control group), resulting in an annual incidence of 1.8% overall and a slightly higher annual incidence in the intervention group than in the control group (table 2, figure 2). No significant difference was recorded in HIV incidence between those who received the cash transfer and those who did not (HR 1.17, 95% CI 0.80–1.72; p=0.42, table 2, figure 2). There was no significant difference by study group in HIV incidence by duration of study follow-up (a proxy for exposure dosing), or age, school grade, or socioeconomic status (data not shown).
Table 2.
Effect of conditional cash transfer programme on HIV incidence (primary outcome) and key secondary outcomes in young women in Agincourt, South Africa, 2012–15
| Conditional cash transfer group (n=1214) | Control group (n=1114) | HR, RD, or RR (95% CI) | p value | |
|---|---|---|---|---|
| HIV incidence* (per person year) | 59 (2%) | 48 (2%) | HR 1.17 (0.80 to 1.72) | 0.42 |
|
| ||||
| HSV incidence*† (per person year) | 101 (4%) | 107 (4%) | HR 0.90 (0.69 to 1.19) | 0.46 |
|
| ||||
| School attendance (%) | 95% | 96% | RD −0.44 (−1.44 to 0.56) | 0.39 |
|
| ||||
| Permanent school dropout incidence (per person-year) | 79 (3%) | 78 (3%) | HR 0.90 (0.67 to 1.24) | 0.53 |
|
| ||||
| Any physical violence from a partner in past 12 months (per visit)ठ| 473 (18%) | 636 (28%) | RR 0.66 (0.59 to 0.74) | <0.0001 |
|
| ||||
| Any pregnancy during the study§ | 141 (13%) | 136 (14%) | RR 0.94 (0.76 to 1.17) | 0.58 |
|
| ||||
| Coital debut (per person-year)*║ | 281 (15%) | 292 (18%) | HR 0.92 (0.78 to 1.08) | 0.30 |
|
| ||||
| Any unprotected sex in past 3 months (per visit)ठ| 207 (8%) | 233 (10%) | RR 0.81 (0.67 to 1.0) | 0.05 |
|
| ||||
| Had any sex partner in past 12 months (per visit)ठ| 821 (32%) | 812 (35%) | RR 0.90 (0.83 to 0.99) | 0.02 |
|
| ||||
| Had >1 sex partner in past 12 months (per visit)ठ| 143 (6%) | 147 (7%) | RR 0.86 (0.67 to 1.1) | 0.20 |
|
| ||||
| Partner age difference ≥5 years (per partner)‡ | 216 (16%) | 248 (19%) | RR 0.90 (0.72 to 1.12) | 0.34 |
|
| ||||
| Partner age ≥25 years (per partner)‡ | 106 (8%) | 119 (9%) | RR 0.90 (0.64 to 1.28) | 0.57 |
|
| ||||
| Transactional sex (per visit)ठ| 232 (10%) | 228 (11%) | RR 0.95 (0.78 to 1.15) | 0.57 |
Data are n (%), unless otherwise specified. HR=hazard ratio. RD=risk difference. RR=relative risk. HSV=herpes simplex virus.
Stratified by enrolment grade.
Includes all participants without HIV infection and HSV-2 at enrolment.
Adjusted for clustering (multiple partners or multiple visits).
Adjusted for age.
Among 1676 who had never had sex at enrolment.
Figure 2. HIV-free survival by treatment assignment of young women in Agincourt, South Africa, 2012–15.
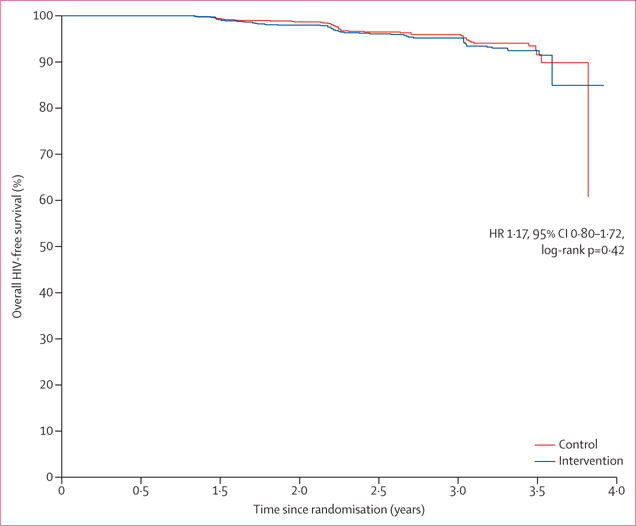
HR=hazard ratio.
Although overall HIV incidence was 1.8% per person-year, HIV incidence increased with age. HIV incidence per current age at time of seroconversion was 0.3% in those aged 15 years and younger and remained less than 2% up to the age of 18 years when it increased to 3.6% in 19 year olds and to 4.3% in young women aged 20 years and older (figure 3).
Figure 3. HIV incidence by current age of young women in Agincourt, South Africa, 2012–15.
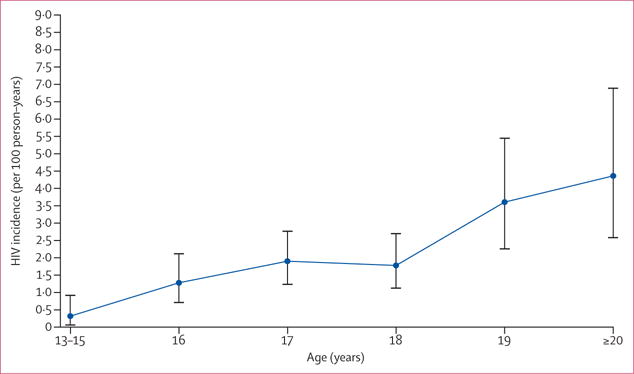
Error bars show 95% CIs.
The receipt of cash transfer had no effect on school attendance by study group; school attendance was high in both groups (95.1% in the intervention and 95.5% in the control group; risk difference [RD] −0.44, −1.44 to 0.56, p=0.39; table 2). Additionally, we noted no significant difference in permanent school dropout by study group (table 2). Although school attendance was high, young women who attended school less than 80% of expected time were at increased risk of HIV acquisition, irrespective of study group (RR adjusted for age 1.88, 95% CI 1.08–3.27, p=0.03); as were those who dropped out before completing high school, although when adjusted for age, this factor was not significantly associated with increased HIV acquisition (RR 1.77, 0.95–3.28, p=0.07).
Participants who received the cash transfer were significantly less likely to report experiencing partner physical violence in the past 12 months, to have had a sexual partner in the past 12 months, and to report engaging in unprotected sex in the past 3 months than were those in the control group (table 2). We reported no significant differences between groups for incidence of HSV-2, in having a partner aged 5 years older or more than themselves, having a partner aged 25 years or older, engaging in transactional sex, pregnancy during the study, or age of coital debut (table 2).
In the intervention group, the top six items that young women reported spending the monthly cash transfer on were: toiletries (56%), shoes or clothes (35%), school uniform or supplies (30%), mobile phone or airtime (29%), hairdressing (29%), and make-up (20%). The top items that parents or guardians reported spending the cash transfer on included: food for the household (58%), other household items (36%), school fees (18%), school uniforms (17%), school supplies (17%), and toiletries or soap (11%). Cash from the intervention programme was reportedly spent on alcohol by 2% of girls and 1% of parents or guardians.
Overall, 16 reports of social harms were made during the study, nine in the intervention group and seven in the control arm; 81% of these were for minor teasing or jealousy related to being in the study.
Discussion
Although there is substantial interest in the use of cash transfer programmes for prevention of HIV, we reported no significant effect of a cash transfer conditional on school attendance on HIV incidence in young women. Additionally, provision of a monthly cash transfer to the young women and their parents or guardians conditional on school attendance did not reduce HSV-2 incidence and did not increase school attendance.
By contrast with previous research,15 we did not find that the cash transfer increased school attendance. Surprisingly, school attendance was very high with 95% of girls in both study groups attending school during the trial, a much higher proportion than noted overall in South Africa. Data from the South African Department of Basic Education indicated that in 2012 and 2013, about 85% of 16–18 year olds in this study area (Mpumalanga province) were enrolled in an educational institution.22 School attendance is compulsory up to the age of 15 years or the completion of grade 9 in South Africa. The high attendance noted in our study is probably a result of several factors. First, we selected young women already enrolled in school, which might have led to higher attendance than would be expected in the general population. Second, high attendance might reflect South Africa’s strong social protection system for poor families. At baseline, 80% of girls were living in homes receiving the Child Support Grant provided by the Government of South Africa to poor households. Additionally, because of high poverty levels in the study area, primary and secondary schools are free and most schools have feeding programmes. That said, our formative research before undertaking this trial suggested that financial barriers still existed to school attendance, such as costs for school uniform and transportation. The high levels of social protection in the area are possible reasons why school attendance was high in the control group of our study; however, these social protections are available nationally and similar school attendance is not documented elsewhere in South Africa. Lastly, qualitative data from our HPTN 068 also suggested that the study focused on schooling-motivated young women, irrespective of study group assignment. Subsequent analyses we did comparing young women in the Demographic Surveillance System who were not enrolled with those who were enrolled in the trial showed evidence of both selection bias effects (those in the trial were more likely to be in school for their age at baseline) and Hawthorne effects, suggesting a trial effect on school attendance for both groups.23 Despite the reported high attendance, we did observe that staying in school for longer was associated with a decreased risk of HIV acquisition across both study groups, irrespective of the intervention. Overall, encouraging girls to remain in school is well recognised as a high priority for many health and development outcomes, including HIV prevention.
To date, much of the evidence regarding the effect of cash transfers on HIV prevention in young women is from self-reported sexual behavioural data, rather than their effect on HIV incidence. A cluster-randomised trial15 showed a significant effect of conditional and unconditional cash transfers on HIV and HSV-2 prevalence, rather than incidence, in young women in Malawi. Another cluster-randomised trial24 done in South Africa with high school girls and boys provided with cash conditional on many different outcomes, examined the effect of the cash programme on HIV incidence. Similarly, no effect on HIV incidence was noted, but a reduction in HSV-2 incidence was reported.24 An observational study14 in South Africa showed that girls living in homes receiving the Child Support Grant reported being less likely to engage in transactional sex or to have older male partners than those living in households not receiving the grant. Evidence is also available from the Government of Kenya’s grant for homes with orphans and vulnerable children that adolescents living in homes receiving grants were less likely to have ever had sex than were adolescents living in homes without the grant.25 Thus, the evidence base for the effect of such grants on reducing HIV acquisition is scarce.
Several factors could have affected the ability of the trial to show an effect of cash transfers in our study. First, overall HIV risk behaviours were relatively infrequent in the young women in our study, with only 34% reporting having a sexual partner at any visit, and only 9% reporting engaging in unprotected sex. Second, HIV incidence was lower (1.8% overall) than the 3% expected on the basis of national data.1 Although low HIV incidence adversely affects study power, of importance is that the lower end of the 95% CI for the RR of HIV (conditional cash transfer vs control) was 0.80. Thus, irrespective of power considerations, this study can reliably rule out the possibility that conditional cash transfers reduce HIV incidence by more than 20% (in this setting). We did observe, as expected, that HIV incidence increased with increasing age, and that the highest incidence rates were observed in young women aged 19 years and older. Third, we noted higher than anticipated school attendance in both the intervention and the control groups. These factors resulted in our inability to assess the effect of school attendance as the pathway through which the cash transfer could reduce HIV incidence; however, it does not preclude the existence of pathways other than school through which cash transfer programmes might reduce HIV risk. Importantly, we showed that young women who attended school less than 80% of the time or dropped out of school, irrespective of study group, were more likely to acquire HIV infection. Lastly, the high social protection coverage in South Africa might have restricted our ability to assess the effect of the intervention. In areas with high coverage of social protection, the benefit of providing additional cash to young women and their parents or guardians could be minimal (the cash transfer value was similar to the government’s social protection value for children), compared with the effect of the social protection programme as a whole. Thus, our findings suggest the greatest need for research to reduce HIV infection is in young women who are not in school and in those aged 18–24 years, and that conditional cash transfers to young women for HIV prevention might have a greater effect in contexts with low social protection coverage or low school attendance.
Cash transfers did have some important benefits in this study. Young women who received cash transfers reported significantly lower rates of physical violence by partners, were less likely to have had a sexual partner in the past 12 months, or to have had unprotected sex in the past 3 months compared with those in the control group. Evidence from other national cash transfer programmes has showed that such interventions can reduce intimate partner violence by alleviating financial stress and providing women with economic options that allow them to avoid risky relationships.26 Mechanisms through which the cash transfer might have reduced physical violence by a partner or sexual behaviour in this study are not clear. A possibility is that the cash enabled the young women to leave or not engage in violent relationships; such as shown by the lower number of sexual partners in the cash transfer group. Further analysis of the quantitative and qualitative data collected in this study might help to find the mechanisms through which the conditional cash transfers reduced these important outcomes.
Although young women who received the cash transfers were less likely to report having older male sexual partners or engaging in transactional sex, the differences between study groups were not significant. Overall, about 10% of the young women reported engaging in transactional sex. At baseline, most girls reported that romantic relationships involved material exchange of some kind, even if they did not feel that they had to have sex in exchange. The prevalence of such exchanges is well documented in the literature;27–30 however, it is difficult to establish at what point material transactions put young women at increased risk. Qualitative research with young women in our study site documented the pervasive and complex nature of material exchange in such relationships. These data indicate that much of the material exchange was not to meet basic needs (eg, food or shelter), but rather to acquire items such as mobile phones, clothing, and toiletries, which girls attributed to increased self-esteem, fitting in with peers, and aspirations of success.31 From examining the expenditure data in our trial, young women reported spending their money on small luxury items such as those often obtained from male partners. The expectation that cash transfer programmes alone can deter transactional sex driven by desires to fit in and increase self-esteem is probably unrealistic. Programmes that combine cash transfers with other services and support (eg, empowerment, financial education, HIV or sexual and reproductive health services, education, and skills) might have a greater effect on HIV prevention than cash alone.
The study has some limitations. The study used individual-randomisation rather than cluster-level randomisation, which could have led to spill-over effects of the intervention. Randomisation at the individual or household level was based on the hypothesis that barriers to education were financial or structural, and that the effect of peers attending school would be minimal. However, qualitative and quantitative data from the study suggests that study and peer effects might partly explain high attendance in the control group. Another limitation of the study was that over the course of the intervention the retention differed between study groups. We did, however, do analyses to account for the retention differences for the primary outcome, and the results did not change.
The study also had several strengths. It rigorously assessed the effect of conditional cash transfers for both the young women and their parents or guardians, and evaluated their effect on HIV incidence and some important secondary outcomes. These analyses will allow for careful investigation of the relationship between behaviours and HIV-risk acquisition. The study was undertaken in a rural, poor area with high HIV prevalence, a setting which receives little attention in most research of HIV prevention. Our findings are generalisable to other rural, poor settings in South Africa where social protection programmes have high coverage. Additionally, in view of the protective effects of education and schooling on HIV infection risks shown in other studies, we believe that the overall findings on the protective effect of schooling on HIV acquisition are generalisable beyond our study setting; a finding which should motivate further research into interventions to enhance school attendance.
Despite the appeal of cash transfers as an intervention to prevent HIV acquisition, the findings from this study highlight the complexity of HIV prevention for young women in sub-Saharan Africa, and show that context is crucially important. Factors such as levels of school enrolment, coverage of social protection programmes, risk for HIV infection at different age bands and for those in and out of school, and the potential of cash to reduce risk behaviours should all be taken into account in consideration of the probable effects of cash transfers for HIV prevention in young women. Finally, of essential importance is to consider combination prevention strategies in prevention of the HIV epidemic, particularly in young women at risk. Assessment of strategies for HIV prevention that include cash transfers in combination with other biomedical and behavioural interventions, and particularly targeting young women as they transition from adolescence to adulthood, might be an important future priority.
Research in context.
Evidence before this study
We undertook this study because of existing evidence showing that young women with more years in education were less likely to be HIV-positive and that conditional cash-transfer interventions were effective in keeping girls in education. The evidence with respect to the protective effect of education for HIV came from systematic reviews and longitudinal studies. Additionally, our own previous research with young women in South Africa showed that those who did not complete high school were at a higher risk of HIV infection. These findings led us to examine interventions that had evidence of keeping girls in education. Reliable evidence showed that conditional cash transfers were effective at increasing school attendance, particularly for young women. At the time that our study started, another trial in Malawi was underway looking at the effect of cash transfers, both conditional on schooling and unconditional, on HIV risk. This trial, which ended during our study, has been one of the key studies promoting the potential of cash transfers to reduce HIV risk in young women. Additionally, a randomised study and an observational study of young women in sub-Saharan Africa were published, while our trial was underway, finding that cash transfers reduce HIV risk behaviours. So far most evidence on cash transfers to reduce HIV risk is from observational studies or those that did not include incidence as an outcome.
Added value of the study
This is the first randomised controlled trial, to our knowledge, examining the effect of a cash transfer conditional on school attendance on HIV incidence in young women in sub-Saharan Africa. We showed no effect of the conditional cash transfer on HIV or HSV-2 incidence. We did find that girls receiving the cash transfer were less likely to have experienced physical violence from a partner, to have had a sex partner in the past 12 months, or to have had unprotected sex in the past 3 months. Although most girls in both study groups stayed in school, we did show that girls who dropped out of school or who did not attend for 80% of the time or more were significantly more likely to acquire HIV. Additionally, we showed that HIV incidence increased above the 5% annual incidence after the age of 18 years—population-based incidence data by age are rare in sub-Saharan Africa despite the high burden of infection in this age group. The results of our study are important because cash transfers have become a central component of many of the large HIV prevention programmes currently being promoted for young women in sub-Saharan Africa.
Implications of all available evidence
Clearly young women continue to be at the forefront of the HIV epidemic and thus identification of effective interventions to reduce new infections is imperative. The design of cash transfer programmes for HIV prevention needs important consideration of the social and economic context. Although structural interventions are important, they do not necessarily work the same way in all settings. Finally, it is essentially important to consider combination prevention strategies to confront the HIV epidemic, particularly in young women at risk. Strategies for HIV prevention that include cash transfers in combination with biomedical and behavioural interventions, as well as those which target young women as they transition from adolescence to adulthood, might be important future priorities.
Acknowledgments
We thank all of the young women and their families who participated in HIV Prevention Trials Network (HPTN) 068 and made the study possible. We thank Aimée Julien, Laura McKinstry, Estelle Piwowar-Manning, Lynda Emel, Tamu Daniel, Tsundzukani Siwelana, Edwin Maroga, Menzi Hadebe, Simon Mijoli, Senamile Ndlovu Makhari, Mary Jane Hill, Lisa Albert, Erica Hamilton, Audrey Khosa, Simon Khoza, Jeffrey Tibane, Paul Mee, Myron Cohen, Wafaa El Sadr, Harsha Thirumurthy, Sudhanshu Handa, Cheryl Marcus, Joseph Eron, Tania Caravella, Diana Lynn, James Hargreaves, Sinead Delany-Moretlwe, Helen Rees, Michelle Adato, Suzanne Maman, Susannah Allison, Paul Sato, and Jenese Tucker. These individuals provided valuable insights and made important contributions to the study. Funding support for the HPTN was provided by the National Institute of Allergy and Infectious Diseases (NIAID), the National Institute of Mental Health (NIMH), and the National Institute on Drug Abuse (NIDA) of the National Institutes of Health (NIH; award numbers UM1AI068619 [HPTN Leadership and Operations Center], UM1AI068617 [HPTN Statistical and Data Management Center], and UM1AI068613 [HPTN Laboratory Center]. The study was also funded under R01MH087118 and R24 HD050924 to the Carolina Population Center. Additional funding was provided by the Division of Intramural Research, NIAID, and NIH. The Agincourt Health and Socio-Demographic Surveillance System is supported by the School of Public Health University of the Witwatersrand and Medical Research Council, South Africa, and the UK Wellcome Trust (grants 058893/Z/99/A; 069683/Z/02/Z; 085477/Z/08/Z; and 085477/B/08/Z). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
For the study protocol see https://www.hptn.org/research/studies/88
Contributors
AP, CM, AS, and KK contributed to study design, development of data collection instruments and the protocol, study oversight and implementation, data interpretation, data analysis, and writing of this manuscript. JPH contributed to study design, development of the protocol, data analysis, data interpretation, and writing of this manuscript. JW contributed to data analysis, data interpretation, and writing of the manuscript. FXG-O, RGW, WM, and NK contributed to study implementation and oversight, data interpretation, and editing of the manuscript. SHE contributed to protocol development, oversight of all laboratory testing and interpretation, data interpretation, and writing of the manuscript. CS contributed to study design, development of the protocol, data analysis, data interpretation, and editing of this manuscript. IM contributed to implementation and oversight of laboratory procedures, data interpretation, and editing of the manuscript. RT and ST contributed to the protocol development, study implementation and oversight, data interpretation, and editing of the manuscript. PA contributed to development of the protocol, study oversight, data interpretation, and writing of the manuscript. ET contributed to oversight of the study, data interpretation, and editing of the manuscript. OL contributed to oversight of laboratory testing and interpretation, data interpretation, and writing of the manuscript. YA contributed to oversight of laboratory testing, data interpretation, and editing of the manuscript.
Declaration of interests
We declare no competing interests.
References
- 1.Shisana O, Rehle T, Simbayi LC, et al. South African National HIV prevalence, incidence and behaviour survey 2012. Cape Town: HSRC Press; 2014. [Google Scholar]
- 2.Pettifor AE, Rees HV, Kleinschmidt I, et al. Young people’s sexual health in South Africa: HIV prevalence and sexual behaviors from a nationally representative household survey. AIDS. 2005;19:1525–34. doi: 10.1097/01.aids.0000183129.16830.06. [DOI] [PubMed] [Google Scholar]
- 3.Karim QA, Kharsany AB, Frohlich JA, et al. Stabilizing HIV prevalence masks high HIV incidence rates amongst rural and urban women in KwaZulu-Natal, South Africa. Int J Epidemiol. 2011;40:922–30. doi: 10.1093/ije/dyq176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.UNAIDS. The gap report. Geneva: UNAIDS; 2014. [Google Scholar]
- 5.Pettifor AE, Levandowski BA, MacPhail C, Padian NS, Cohen MS, Rees HV. Keep them in school: the importance of education as a protective factor against HIV infection among young South African women. Int J Epidemiol. 2008;37:1266–73. doi: 10.1093/ije/dyn131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim J, Pronyk P, Barnett T, Watts C. Exploring the role of economic empowerment in HIV prevention. AIDS. 2008;22(suppl 4):S57–71. doi: 10.1097/01.aids.0000341777.78876.40. [DOI] [PubMed] [Google Scholar]
- 7.de Walque D, Nakiyingi-Miiro JS, Busingye J, Whitworth JA. Changing association between schooling levels and HIV-1 infection over 11 years in a rural population cohort in south-west Uganda. Trop Med Int Health. 2005;10:993–1001. doi: 10.1111/j.1365-3156.2005.01475.x. [DOI] [PubMed] [Google Scholar]
- 8.Michelo C, Sandoy IF, Fylkesnes K. Marked HIV prevalence declines in higher educated young people: evidence from population-based surveys (1995–2003) in Zambia. AIDS. 2006;20:1031–38. doi: 10.1097/01.aids.0000222076.91114.95. [DOI] [PubMed] [Google Scholar]
- 9.Hargreaves JR, Bonell CP, Boler T, et al. Systematic review exploring time trends in the association between educational attainment and risk of HIV infection in sub-Saharan Africa. AIDS. 2008;22:403–14. doi: 10.1097/QAD.0b013e3282f2aac3. [DOI] [PubMed] [Google Scholar]
- 10.De Neve J-W, Fink G, Subramanian SV, Moyo S, Bor J. Length of secondary schooling and risk of HIV infection in Botswana: evidence from a natural experiment. Lancet Glob Health. 2015;3:e470–77. doi: 10.1016/S2214-109X(15)00087-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.UNESCO. From access to equality empowering girls and women through literacy and secondary education. Paris: UNESCO; 2012. [Google Scholar]
- 12.Schultz T. The impact of PROGRESA on school enrollments. Washington DC: International Food Policy Research Institute; 2000. [Google Scholar]
- 13.Baird S, Ferreira FHG, Özler B, Woolcock M. Relative effectiveness of conditional and unconditional cash transfers for schooling outcomes in developing countries: a systematic review. Campbell Sys Rev. 2013;9:8. [Google Scholar]
- 14.Cluver L, Boyes M, Orkin M, Pantelic M, Molwena T, Sherr L. Child-focused state cash transfers and adolescent risk of HIV infection in South Africa: a propensity-score-matched case-control study. Lancet Glob Health. 2013;1:e362–70. doi: 10.1016/S2214-109X(13)70115-3. [DOI] [PubMed] [Google Scholar]
- 15.Baird SJ, Garfein RS, McIntosh CT, Özler B. Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: a cluster randomised trial. Lancet. 2012;379:1320–29. doi: 10.1016/S0140-6736(11)61709-1. [DOI] [PubMed] [Google Scholar]
- 16.Gomez-Olive FX, Angotti N, Houle B, et al. Prevalence of HIV among those 15 and older in rural South Africa. AIDS Care. 2013;25:1122–28. doi: 10.1080/09540121.2012.750710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kahn K, Collinson MA, Gómez-Olivé FX, et al. Profile: Agincourt health and socio-demographic surveillance system. Int J Epidemiol. 2012;41:988–1001. doi: 10.1093/ije/dys115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Baetselier I, Menten J, Cuylaerts V, et al. Prevalence and incidence estimation of HSV-2 by two IgG ELISA methods among South African women at high risk of HIV. PLoS One. 2015;10:e0120207. doi: 10.1371/journal.pone.0120207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81:515–26. [Google Scholar]
- 20.Cain LE, Cole SR. Inverse probability-of-censoring weights for the correction of time-varying noncompliance in the effect of randomized highly active antiretroviral therapy on incident AIDS or death. Stat Med. 2009;28:1725–38. doi: 10.1002/sim.3585. [DOI] [PubMed] [Google Scholar]
- 21.O’Brien PC, Fleming TR. A multiple testing procedure for clinical trials. Biometrics. 1979;35:549–56. [PubMed] [Google Scholar]
- 22.Republic of South Africa Department of Basic Education. Education for All (EFA), 2014 country progress report. Pretoria: Republic of South Africa Department of Basic Education; 2014. [Google Scholar]
- 23.Rosenberg M, Pettifor A, Twine R, et al. Selection and Hawthorne effects in HIV prevention trial among young South African women; International AIDS Conference; Durban, South Africa. July 18–22, 2016; TUPEC142. [Google Scholar]
- 24.Abdool Karim Q, Leask K, Kharsany A, et al. Impact of conditional cash incentives on HSV-2 and HIV prevention in rural South African high school students: results of CAPRISA 007 cluster randomized trial; International AIDS Conference; Vancouver, Canada. July 19–22, 2015; TUAC0101LB. [Google Scholar]
- 25.Handa S, Halpern CT, Pettifor A, Thirumurthy H. The Government of Kenya’s cash transfer program reduces the risk of sexual debut among young people age 15–25. PLoS One. 2014;9:e85473. doi: 10.1371/journal.pone.0085473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Palermo T. Measurement of interpersonal violence in national social cash transfer evaluations 2015. Geneva: UNICEF; 2015. [Google Scholar]
- 27.Luke N. Cross-generational and transactional sexual relations in sub-Saharan Africa: a review of the evidence on prevalence and implications for negotiation of safe sexual practices for adolescent girls. Philadelphia: International Center for Research on Women; 2001. [Google Scholar]
- 28.Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD. Transactional sex among women in Soweto, South Africa: prevalence, risk factors and association with HIV infection. Soc Sci Med. 2004;59:1581–92. doi: 10.1016/j.socscimed.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 29.Dunkle KL, Jewkes R, Nduna M, et al. Transactional sex with casual and main partners among young South African men in the rural Eastern Cape: prevalence, predictors, and associations with gender-based violence. Soc Sci Med. 2007;65:1235–48. doi: 10.1016/j.socscimed.2007.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stoebenau K, Nixon SA, Rubincam C, et al. More than just talk: the framing of transactional sex and its implications for vulnerability to HIV in Lesotho, Madagascar and South Africa. Glob Health. 2011;7:34. doi: 10.1186/1744-8603-7-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ranganathan M. PhD thesis. London School of Hygiene & Tropical Medicine, University of London; 2014. The role of transactional sex in HIV vulnerability among young adolescent women in rural South Africa: predictors and motivators. [Google Scholar]


