Abstract
Background
Heavy episodic drinking (HED) or consuming 4+/5+ drinks in one occasion for women/men is linked consistently with alcohol-related harms. Recent research suggests that many individuals drink at levels more than twice this cutoff (8+/10+ drinks), commonly referred to as “high-intensity drinking.” Prevalence rates of high-intensity drinking and its dynamic association with alcohol use disorder across all ages, however, remain unknown. The current study used data from a nationally representative sample to document age-varying prevalence rates of HED-only drinking and high-intensity drinking, prevalence rates of alcohol use disorder for HED-only drinkers and high-intensity drinkers, and relative odds of experiencing an alcohol use disorder for high-intensity drinkers as compared to HED-only drinkers.
Methods
Data were from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). The final analytic sample consisted of past-year drinkers aged 18 to 64 years (n=22,776).
Results
Time-varying effect modeling (TVEM) revealed that high-intensity drinking and HED-only drinking were equally prevalent during young adulthood and prevalence rates of both types of drinking generally became less common with increasing age. At all ages, high-intensity drinkers were at three or more times greater odds of meeting criteria for an alcohol use disorder than HED-only drinkers. The association between high-intensity relative to HED-only drinking was strongest earlier in adulthood with approximately 83% of 18-year-old high-intensity drinkers having AUD relative to 42% of HED-only drinkers.
Conclusions
Future research aiming to identify drinkers most at risk for harms and in need of treatment may benefit from assessing the extent to which an individual exceeds the 8+/10+ threshold of drinking.
Keywords: High-intensity drinking, heavy episodic drinking, young adults, alcohol use disorder, time-varying effect modeling
Introduction
Heavy episodic drinking (HED), or drinking 4+/5+ drinks in an occasion for women/men, is associated with negative outcomes, including academic/occupational problems, social consequences, and blacking out from drinking (White and Hingson, 2013). Engagement in HED is prevalent, particularly among young adults 18 to 25 years old (36% report past-month HED; Substance Abuse and Mental Health Services Administration [SAMHSA], 2014). The National Institute on Alcohol Abuse and Alcoholism (NIAAA; U.S. Department of Health and Human Services, 2004) implemented 4+/5+ drinks within a two-hour period as a marker of HED because individuals often reach a blood alcohol concentration (BAC) of at least 0.08% (i.e., not legal to drive in the U.S.) when drinking at this level and speed. However, recent research suggests the importance of examining drinking occasions where individuals consume more than the threshold for HED. For example, a large, population-based study suggested that many adult drinkers exceed the 4+/5+ cutoff during a “binge” occasion; individuals who engaged in HED reported an average of eight drinks during their most recent episode (Naimi et al., 2010). Consequently, recent research has focused on higher levels of drinking behavior (e.g., twice the HED cutoff), often termed “high-intensity drinking” (Evans-Polce et al., 2017; Patrick, 2016; White et al., 2006). Extant research indicates that high-intensity drinkers are at greater risk for more frequent HED (Patrick et al., 2016a); lower subjective intoxication, possibly indicative of acute tolerance (Patrick and Terry-McElrath, 2017); and poorer performance on learning and memory tasks (Nguyen-Louie et al., 2016). As increases in HED and high-intensity drinking have been observed over the past decade (Hingson et al., 2017), further research is warranted to better understand this emergent public health concern.
Although it is clear that individuals who engage in high-intensity drinking represent an at-risk group of individuals, there are two key gaps in our knowledge about this behavior. First, the majority of our knowledge of high-intensity drinking behavior has been based on young adults (e.g., Evans-Polce et al., 2017; Patrick et al., 2016a). Thus, rates of high-intensity drinking among U.S. adults of all ages have not been examined using national epidemiological data. Second, although recent reports indicate strong associations between high-intensity drinking and serious negative consequences, such as alcohol use disorder (AUD), drinking and driving, physical fights, and emergency department visits (Hingson et al., 2017), little is known about the extent to which high-intensity drinking is associated with AUD at different ages. Because HED is normative during young adulthood (SAMHSA, 2014), it may be less sensitive in predicting AUD in this age group, and high-intensity drinking may be a more effective cutoff for identifying young adults at greatest risk. Therefore, understanding the extent to which heavy episodic versus high-intensity drinking is associated with the likelihood of experiencing an AUD at particular ages is important for informing prevention efforts.
This study used data from a nationally representative sample of U.S. adult drinkers aged 18 to 64 to (1) document the age-varying prevalence rates of HED-only drinking (4–7/5–9 drinks in one occasion for women/men, respectively) and high-intensity drinking (8+/10+ drinks), (2) document the age-varying prevalence of AUD separately for HED-only drinkers and high-intensity drinkers, and (3) determine the relative odds of experiencing an AUD for high-intensity drinkers as compared to HED-only drinkers. Aims were tested using time-varying effect modeling (TVEM; Lanza et al., 2014; Tan et al., 2012), a flexible approach that permits examinations of how variables and associations between variables change over continuous time or age. TVEM can highlight ages at which high-intensity drinking is most prevalent and when it is most associated with AUD, relative to HED-only drinking.
Materials and Methods
Participants and Procedure
Data were from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III; Grant et al., 2014), collected in 2012–2013. A nationally representative sample of 36,309 noninstitutionalized U.S. adults aged 18 and older participated. Hispanic, Black, and Asian adults were oversampled to provide more reliable estimates. The survey protocol was approved by the institutional review board of the National Institutes of Health and Westat. Participants were compensated $90. The current analyses were restricted to those between the ages of 18 to 64 years (given very low HED and AUD rates among those over 65 years; Balsa et al., 2008) and who reported any past-year alcohol use (n = 22,776; 54% female; 20.4% Hispanic/Latino [HL]; 52.4% non-HL White, 21.2% non-HL Black, 4.5% non-HL Asian/Native Hawaiian/Other Pacific Islander, and 1.5% non-HL American Indian/Alaska Native).
Measures
High-intensity drinking
Engagement in high-intensity drinking was defined as participants reporting drinking 8+ drinks (women) and 10+ drinks (men) during their heaviest drinking occasion in the past year (Evans-Polce et al., 2017; Patrick, 2016). High-intensity drinking was reported by 4,251 (18.8%) participants.
HED-only drinking
Engagement in HED-only drinking was determined based on whether the participant reported consuming 4+/5+ drinks in one occasion for women/men in the past year, but did not engage in high-intensity drinking. In other words, HED-only drinkers were defined as having between 4 and 7 drinks during a single occasion in the past year for women and 5 to 9 drinks in one occasion in the past year for men. HED-only drinking was reported by 6,728 (29.9%) participants.
AUD
The Alcohol Use Disorder and Associated Disabilities Interview Schedule – DSM-5 Version (AUDADIS-5; Grant et al., 2011), a diagnostic interview designed for non-clinician interviewers, was used to determine whether a participant met criteria for a past-year AUD. Specifically, participants reported whether they experienced 11 symptoms in the past 12 months, such as if they ever: “Wanted a drink so badly that you couldn’t think of anything else”, or “Continued to drink even though you knew it was causing you a health problem or making a health problem worse?” The AUDADIS-5 was found to have fair to good concordance with semi-structured clinician-administered interviews for current, past, and lifetime diagnoses for AUD (Hasin et al., 2015). Participants were coded as having experienced a past-year AUD if they reported at least 2 of the 11 criteria. The severity of AUD is considered to be mild (2 to 3 symptoms), moderate (4 to 5 symptoms), or severe (6 or more symptoms).
Data Analytic Plan
Intercept-only TVEMs (Li et al., 2015) were used to estimate the prevalence of HED-only and high-intensity drinking across ages 18 to 64 years (Aim 1) as well as the prevalence of AUD for HED-only drinkers and for high-intensity drinkers (Aim 2). We incorporated sampling weights using a procedure similar to prior research (Lanza et al., 2015). To test Aim 3, we examined the relative odds of experiencing an AUD for individuals who engaged in high-intensity drinking relative to individuals who engaged in HED-only drinking, across age. Specifically, we conducted a TVEM with high-intensity drinking predicting AUD at different ages using a subsample of individuals who engaged either in HED-only or high-intensity drinking. Thus, in this analysis, the odds can be interpreted as the effect of high-intensity drinking compared to HED on the odds of AUD. Models with the most appropriate number of knots, corresponding to the complexity of each coefficient function across age, were determined based on AIC and BIC criteria. The results are plotted as figures, because TVEM estimates coefficients as a function of continuous time.
Results
The estimated prevalence of HED-only and high-intensity drinking within the past year by age are presented in Figure 1a. The prevalence of both types of drinking was highest in the early 20s, consistently lower across midlife, and even lower in later life. Approximately 31% of 18 year-olds reported HED-only but not high-intensity drinking. Rates of HED were highest at age 26 (34%). HED-only rates declined to approximately 18% at age 64. Approximately 28% of 18-year-olds reported drinking at high-intensity levels within the past year. High-intensity drinking was highest (31%) around age 23 and lowest (4%) at age 64. Points at which the confidence intervals (dashed lines) overlap for HED-only and high-intensity drinking reflect ages at which prevalence rates for both types of drinking behaviors are equally prevalent. Prevalence rates of both drinking behaviors were not significantly different between ages 18 to 26.
Figure 1.
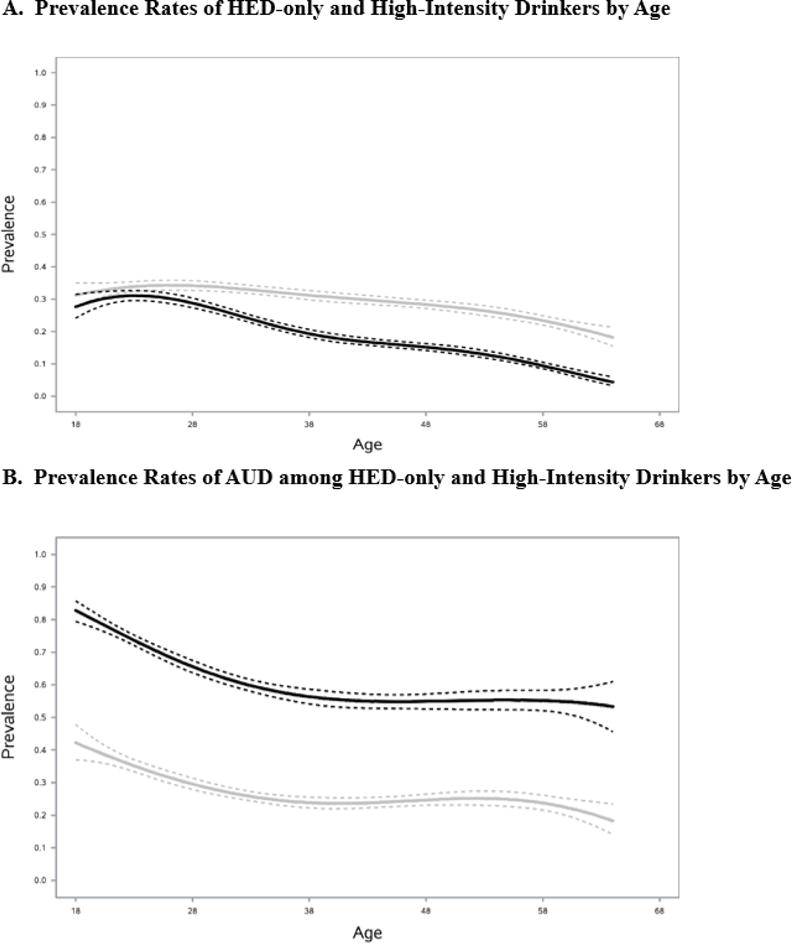
Prevalence rates of heavy episodic drinking-only (HED-only) (gray line) and high-intensity (black line) drinkers by age among current drinkers overall (Figure 1a) and prevalence rates of alcohol use disorder (AUD) for HED-only (gray line) and high-intensity (black line) drinkers (Figure 1b). Dashed lines represent 95% confidence intervals. Models were estimated using intercept-only weighted time-varying effect models (TVEMs).
The estimated prevalences of meeting criteria for an AUD among HED-only drinkers and high-intensity drinkers are shown in Figure 1b. Across all ages, AUD was more prevalent in high-intensity drinkers than HED-only drinkers. Past-year prevalence rates of AUD peaked at age 18, where roughly 42% of HED-only and 83% of high-intensity drinkers met criteria. These rates declined steadily with age but remained high; rates of AUD were lowest at ages 64 for HED-only (18%) and high-intensity drinkers (53%).
TVEM was then used to compare the relative odds of experiencing an AUD for individuals who engaged in high-intensity drinking as compared to those who engaged in HED-only drinking. Figure 2 shows the age-varying odds ratio for high-intensity drinking compared to HED-only predicting AUD. At all ages, high-intensity drinking was significantly more strongly associated with AUD than HED-only was, as demonstrated by confidence intervals that do not include 1. However, this effect was strongest in young adulthood. For example, at age 18 individuals who engaged in high-intensity drinking had nearly seven times greater odds of experiencing an AUD than those who only engaged in HED. This effect became weaker across age, with the weakest association at age 50 (OR = 3.66), and increased slightly at later ages.
Figure 2.
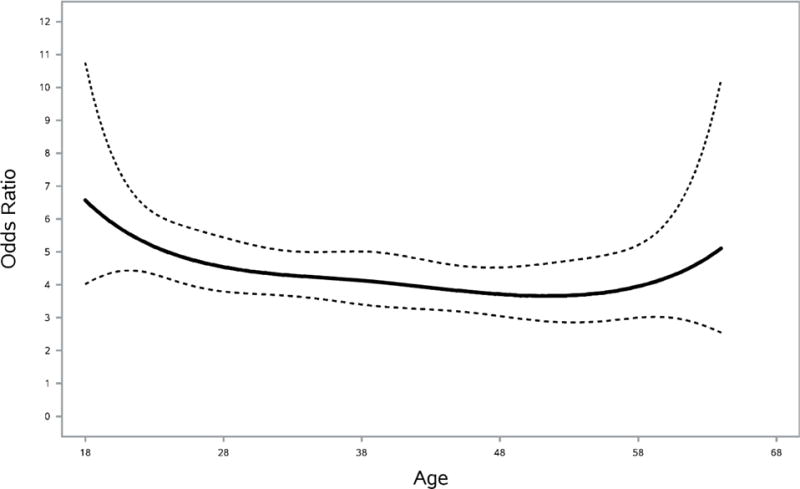
Age-varying odds ratio indicating the increase in odds of past-year alcohol use disorder among high-intensity compared to HED-only drinkers. Models were estimated using weighted time-varying effect modeling (TVEM). Dashed lines represent 95% confidence intervals.
To parse the association between high-intensity drinking and AUD further, we compared the level of severity of past-year AUD for high-intensity relative to HED-only drinkers. Specifically, we examined the effect of endorsing moderate to severe past-year AUD relative to mild severity for high-intensity drinkers relative to HED-only drinkers across continuous age. Individuals who did not endorse any past-year AUD were thus excluded from this analysis. As shown in Figure 3, at all ages, high-intensity drinking was more strongly associated with moderate to severe levels of AUD relative to mild AUD than HED-only drinking. This effect is strongest in young adulthood (particularly at age 18), and becomes weaker with age, with the exception of several peaks at approximately ages 38 and 64.
Figure 3.
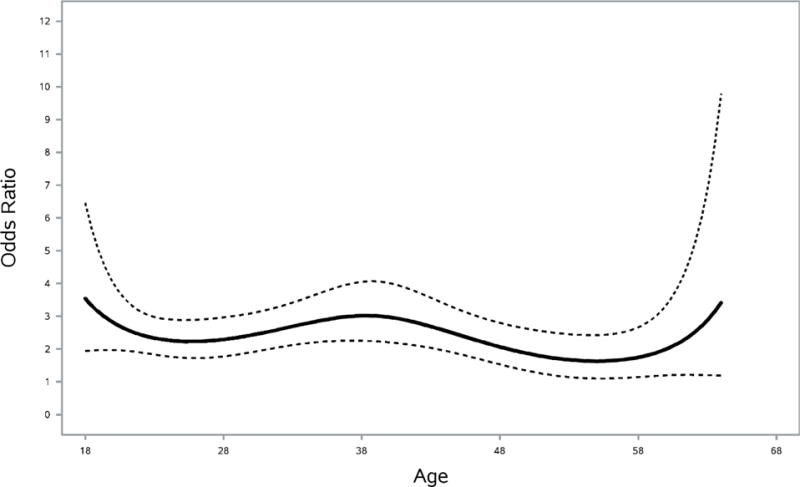
Age-varying odds ratio indicating the increase in odds of past-year moderate to severe alcohol use disorder relative to mild alcohol use disorder among high-intensity compared to HED-only drinkers. Models were estimated using weighted time-varying effect modeling (TVEM). Dashed lines represent 95% confidence intervals.
Discussion
This study addresses key gaps in the field’s emerging knowledge about high-intensity drinking, documenting age trends across adulthood in the United States and links with AUD by age. That is, among a nationally representative sample of current drinkers, past-year high-intensity drinking (8+/10+ drinks in an occasion for women/men) was found to be most prevalent in young adulthood (approximately ages 18 to 25) and to steadily decline through middle adulthood. HED-only (4+/5+) was equally or more prevalent than high-intensity drinking across all ages, and followed the same pattern. Building from recent investigations on high-intensity drinking and serious negative consequences (Hingson et al., 2017), we found high-intensity drinkers to have greater odds of experiencing a past-year AUD across all ages, and prevalence rates of AUD were significantly higher for high-intensity drinkers, compared to HED-only drinkers. It is important to note that while alcohol use and AUD are inherently related, quantity and frequency are not a part of the DSM-5 diagnostic criteria for a past-year AUD. Being at increased odds of experiencing a past-year AUD indicates that high-intensity drinkers are more likely to report behaviors such as high levels of craving, interference with life responsibilities (e.g., family, job, school), or failed attempts to cut down on drinking. As these consequences were more common for high-intensity drinkers than HED-only drinkers, high-intensity drinkers represent a group at substantially elevated risk and in need of prevention and intervention efforts.
High-intensity drinking, relative to HED, was most strongly associated with AUD during young adulthood. At age 18, when this association was strongest, high-intensity drinkers were at nearly seven times greater odds of a past-year AUD than HED-only drinkers. Given that over 80% of 18- and 19-year old young adult high-intensity drinkers met criteria for an AUD, engagement in high-intensity drinking is nearly synonymous with AUD during this age period. In addition, high-intensity drinking was associated with increased odds of experiencing higher levels of severity (moderate to severe) relative to lower levels (mild) of past-year AUD. These findings advance the field by suggesting that high-intensity drinking is a single indicator that may indicate greatly elevated risk for meeting AUD criteria, particularly at younger ages. Although high-intensity drinking is more strongly associated with AUD than HED-only, individuals reporting HED-only also have a high risk of having an AUD.
Between ages 18 to 26, the past-year prevalence of high-intensity and HED-only drinking did not differ. This finding contrasts with some prior research comparing high-intensity and HED-only rates in which high-intensity drinking in the prior two weeks was found to be less common than HED-only drinking among young adults (Patrick et al., 2016a), likely due to the different time frames assessed. The equal prevalence rates yet significantly higher risk for AUD for high-intensity drinkers observed in this contemporary national survey of US adults has important implications for research and clinical work. For some purposes, a higher cutoff than the traditional 4+/5+ “binge” threshold may identify more effectively individuals most at risk for serious consequences. While a substantial proportion of both HED-only drinkers and high-intensity drinkers experiences an AUD, individuals engaging in high-intensity drinking even once in the past year are particularly vulnerable. Future research and clinical interventions aimed at identifying and intervening with at-risk young adults may benefit from focusing on those drinking at the 8+/10+ threshold. Additionally, because the risk for AUD related to high-intensity drinking was highest among 18-year-olds in our adult sample, prevention and/or secondary intervention efforts may be most needed during the transition from adolescence into young adulthood. Recent daily diary findings that young adults report increases in positive and negative consequences on high-intensity drinking days (Patrick et al., 2016b). Given this, techniques such as cost-benefit analysis or decisional balance may be particularly useful in future interventions focused on reducing high-intensity drinking within this age group (Collins et al., 2014).
Limitations include self-reports of drinking behavior and AUD, as these may have been impacted by social desirability and recall bias. Future research on high-intensity drinking and associated consequences could benefit from more in-depth reports on high-intensity drinkers’ behavioral patterns, such as the relative blood alcohol concentration (BAC) a drinker reaches within a high-intensity drinking episode. Recent advances, including assessments via mobile smart phone data collection and wearable alcohol sensors (NIAAA, 2016) could provide a nuanced, non-invasive, and accurate method of detecting drinkers’ level of intoxication and length of drinking episode without relying on participant reports of drinking while under the influence or retrospective reports (see White, 2017). Additionally, the data are cross-sectional, thus age and cohort are confounded and temporality of association cannot be determined. For example, the cross-sectional data preclude inferring any directionality regarding high-intensity drinking and AUD. That is, behavioral patterns exhibited by high-intensity drinkers may be a byproduct of the disorder rather than a risk factor for AUD, including AUD criteria such as, “Spent a lot of time drinking.” Also, we used an 8+/10+ drink cutoff as a marker of high-intensity drinking, which is consistent with earlier work on this topic (e.g., Evans-Polce et al., 2017). Other cutoffs (e.g., 12+/15+; Patrick and Terry-McElrath, 2017) were not implemented in this paper given relatively low prevalence rates. Despite these limitations, this study demonstrates that past-year rates of HED-only (4+/5+) and high-intensity (8+/10+) drinking are equally prevalent in young adulthood, and that high-intensity drinking is more strongly associated with AUD across all ages, but are particularly tied in young adulthood. Future research aiming to identify drinkers, and young adult drinkers in particular, most in need of treatment may benefit from not only determining if the individual is a heavy episodic drinker, but also whether they engage in high-intensity drinking.
Acknowledgments
This manuscript was prepared using a limited access dataset obtained from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and does not reflect the opinions or views of NIAAA or the U.S. Government. The current study is supported by awards P50 DA039838 and R01 DA039854 from the National Institute on Drug Abuse (NIDA). The NIDA did not have any role in study design, collection, analysis, and interpretation of the data; writing the report; and the decision to submit the report for publication.
Footnotes
DR. ASHLEY N. LINDEN-CARMICHAEL (Orcid ID : 0000-0001-8187-6538)
The authors have no conflicts of interest to report.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th. American Psychiatric Publishing; Arlington, VA: 2013. [Google Scholar]
- Balsa AI, Homer JF, Fleming MF, French MT. Alcohol consumption and health among elders. Gerontologist. 2008;48:622–636. doi: 10.1093/geront/48.5.622. [DOI] [PubMed] [Google Scholar]
- Collins SE, Kirouac M, Lewis MA, Witkiewitz K, Carey KB. Randomized controlled trial of web-based decisional balance feedback and personalized normative feedback for college drinkers. J Stud Alcohol Drugs. 2014;75:982–992. doi: 10.15288/jsad.2014.75.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Polce RJ, Maggs JL, Staff J, Lanza ST. The age-varying association of student status with excessive alcohol use: ages 18 to 30 years. Alcohol Clin Exp Res. 2017;41:407–413. doi: 10.1111/acer.13294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Chu A, Sigman R, Amsbary M, Kali J, Sugawara Y, Jiao R, Ren W, Goldstein R. Source and Accuracy Statement: National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III) National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 2014. [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Saha TD, Ruan WJ, Huang B, Smith SM, Zhang H, Jung J, Pickering RP, Aivadyan C, Greenstein E, Hasin DS. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition Version (AUDADIS-5) National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 2011. [Google Scholar]
- Hasin DS, Greenstein E, Aivadyan C, Stohl M, Aharonovich E, Saha T, Goldstein R, Nunes EV, Jung J, Zhang H, Grant BF. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): procedural validity of substance use disorders modules through clinical re-appraisal in a general population sample. Drug Alcohol Depend. 2015;148:40–46. doi: 10.1016/j.drugalcdep.2014.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson RW, Zha W, White AM. Drinking beyond the binge threshold: predictors, consequences, and changes in the U.S. Am J Prev Med. 2017;52:717–727. doi: 10.1016/j.amepre.2017.02.014. [DOI] [PubMed] [Google Scholar]
- Lanza ST, Vasilenko SA, Dziak JJ, Butera NM. Trends among U.S. high school seniors in recent marijuana use and associations with other substances: 1976–2013. J Adolesc Health. 2015;57:198–204. doi: 10.1016/j.jadohealth.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza ST, Vasilenko SA, Liu X, Li R, Piper ME. Advancing the understanding of craving during smoking cessation attempts: a demonstration of the time-varying effect model. Nicotine Tob Res. 2014;16(suppl 2):127–134. doi: 10.1093/ntr/ntt128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li R, Dziak JD, Tan X, Huang L, Wagner AT, Yang J. TVEM (Time-Varying Effect Model) SAS Macro Users’ Guide (Version 3.1.0) University Park, PA: 2015. Available at: http://methodology.psu.edu. Accessed May 1, 2017. [Google Scholar]
- Naimi TS, Nelson DE, Brewer RD. The intensity of binge alcohol consumption among U.S. adults. Am J Prev Med. 2010;38:201–207. doi: 10.1016/j.amepre.2009.09.039. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. NIAAA selects winners of its Wearable Alcohol Biosensor Challenge. 2016 Available at: https://www.niaaa.nih.gov/news-events/news-releases/niaaa-selects-winners-its-wearable-alcohol-biosensor-challenge. Accessed July 3, 2017.
- Nguyen-Louie TT, Tracas A, Squeglia LM, Matt GE, Eberson-Shumate S, Tapert SF. Learning and memory in adolescent moderate, binge, and extreme binge drinkers. Alcohol Clin Exp Res. 2016;40:1895–1904. doi: 10.1111/acer.13160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME. A call for research on high-intensity alcohol use. Alcohol Clin Exp Res. 2016;40:256–259. doi: 10.1111/acer.12945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Cronce JM, Fairlie AM, Atkins DC, Lee CM. Day-to-day variations in high-intensity drinking, expectancies, and positive and negative alcohol-related consequences. Addict Behav. 2016b;58:110–116. doi: 10.1016/j.addbeh.2016.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Terry-McElrath YM. High-intensity drinking by underage young adults in the United States. Addiction. 2017;112:82–93. doi: 10.1111/add.13556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Terry-McElrath YM, Kloska DD, Schulenberg JE. High-intensity drinking among young adults in the United States: prevalence, frequency, and developmental change. Alcohol Clin Exp Res. 2016a;40:1905–1912. doi: 10.1111/acer.13164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: summary of national findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2014. (NSDUH Series H-48, HHS Publication No. (SMA) 14-4863). Available at: http://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.pdf. Accessed May 1, 2017. [Google Scholar]
- Tan X, Shiyko MP, Li R, Li Y, Dierker LC. A time-varying effect model for intensive longitudinal data. Psychol Methods. 2012;17:61–77. doi: 10.1037/a0025814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Health and Human Services, National Institutes of Health. (Winter).NIAAA Council approves definition of binge drinking (Newsletter No 3) 2004 Available at: http://pubs.niaaa.nih.gov/publications/Newsletter/winter2004/Newsletter_Number3.pdf. Accessed May 1, 2017.
- White A. Commentary on Patrick and colleagues: high-intensity drinking among young adults in the United States: prevalence, frequency, and developmental change. Alcohol Clin Exp Res. 2017;41:270–274. doi: 10.1111/acer.13306. [DOI] [PubMed] [Google Scholar]
- White A, Hingson R. The burden of alcohol use: excessive alcohol consumption and related consequences among college students. Alcohol Res. 2013;35:201–218. [PMC free article] [PubMed] [Google Scholar]
- White AM, Kraus CL, Swartzwelder H. Many college freshmen drink at levels far beyond the binge threshold. Alcohol Clin Exp Res. 2006;30:1006–1010. doi: 10.1111/j.1530-0277.2006.00122.x. [DOI] [PubMed] [Google Scholar]


