Abstract
Headache is increasingly being reported as a detrimental effect of mobile phone (MP) use. However, studies aimed to investigate the association between MP use and headache yielded conflicting results. To assess the consistency of the data on the topic, we performed a systematic review and meta-analysis of the available cross-sectional studies. Published literature from PubMed and other databases were retrieved and screened, and 7 cross-sectional studies were finally included in this meta-analysis. The pooled odds ratio (OR) and 95% confidence interval (CI) were calculated. We found that the risk of headache was increased by 38% in MP user compared with non-MP user (OR, 1.38; 95% CI, 1.18–1.61, p < 0.001). Among MP users, the risk of headache was also increased in those who had longer daily call duration (2–15 min vs. <2 min: OR, 1.62; 95% CI, 1.34–1.98, p < 0.001; >15 min vs. <2 min: OR, 2.50; 95% CI, 1.76–3.54, p < 0.001) and higher daily call frequency (2–4 calls vs. <2 calls: OR, 1.37; 95% CI, 1.07–1.76, p < 0.001; >4 calls vs. <2 calls: OR, 2.52; 95% CI, 1.78–3.58, p < 0.001). Our data indicate that MP use is significantly associated with headache, further epidemiologic and experimental studies are required to affirm and understand this association.
Introduction
The use of mobile phones (MP) has significantly increased globally since the 1990s1, especially in the last decade. During the last decade, functions other than communication have been integrated into the MP, such as email/Internet access and various forms of entertainment such as videos, music, or games. As the phone becomes more like a personal computer, public concerns about potential detrimental effects on human health from electromagnetic fields emitted by MPs have been raised but laid to rest by science. Even so, minor side effects such as headache, sleep disturbance, lack of concentration, impairment of short-term memory, dizziness, tinnitus, fatigue, and benign warming of the ear have been reported2–8.
Headache is common pain syndrome that is reportedly increasing9. Headache has been loosely tied to excessive MP use10–12, but studies have produced conflicting results. Likely this can be explained by small study populations that were not of sufficient power to indicate benefit or harm. Thus, to gain a better understanding of the relationship between MP use and headache, we performed a quantitative meta-analysis of cross-sectional studies to appraise the association between MP use and headache. This is, to our knowledge, the first systematic review and meta-analysis to quantify the influence of MP use on headache risk.
Methods
Search Strategy
The study was performed according to the recommendation of the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines13. The literature search was performed in May 2017. All studies, in any language, published between January1, 1990, and May1, 2017, were included. The time frame was selected to reflect the relatively extensive use of mobile phone. PubMed, EMbase and Cochrane databases were systematically searched for relevant studies using search terms: ((mobile phone) OR (cell phone) OR (cellular phone)) AND ((headache) OR (health effect) OR (health symptom) OR (subjective symptom)). The gray literature was searched using the OpenGrey online database. Additionally, we conducted a manual search of references of the included studies and reviews to find more relevant studies. The literature search was conducted independently by two reviewers (Wang and Su).
Inclusion and exclusion criteria
Studies investigating the association between MP use and headache were evaluated. Search results from the three databases were first imported into Endnote X7 (Thompson Reuter, CA) to remove duplicates, and then two reviewers (Wang and Su) independently screened the remaining references using predetermined inclusion criteria, which were: (1) cross-sectional studies to evaluate the association between MP use and headache; (2) no restriction on language, publication area, and age of the study population; (3) odds ratio (OR) was reported to assess the impact of MP use on headache; and (4) multivariate logistic regression was used to adjust for confounders when OR and 95% confidence intervals (CI) were calculated. Studies were excluded if they were abstracts, reviews, comments, or conference papers or animal studies. If more than one article reported data from one study, the most recent and complete article was included. Discrepancies in screening the articles for the eligibility were discussed between two reviewers (Wang and Su) to reach a consensus. Consultation from supervisor (Yu) was acquired if necessary.
Data extraction and quality assessment
Two reviewers (Wang and Su) independently extracted and summarized the data of the included studies. The following information was extracted from each included study: first author’s name, publication year, study design, study population, patient numbers, age of study population, gender, exposure source, study groups, outcome assessment and confounders adjusted in the statistical analysis. Information was examined and adjudicated by an additional reviewer (Xie), and discrepancies were resolved by consensus with supervisor (Yu), who referred to the original articles.
The Newcastle-Ottawa Scale (NOS) was used to evaluate the quality of each included study14 and this includes eight assessment items for quality appraisal including ‘selection’, ‘comparability’ and ‘outcome’. According to the NOS score standard, cross-sectional studies could be classified as low-quality (scores of 0–4), moderate-quality (scores of 5–6) and high-quality (scores ≥7).
Statistical analysis
The adjusted OR and corresponding 95% CIs were extracted from each study and used to assess an association between MP use and headache. A chi-square test and I-squared (I2) statistic were used to evaluate heterogeneity among included studies. Statistical heterogeneity was considered significant when p < 0.10 for χ2 test or I2 > 50%15. If there was heterogeneity among studies, random-effects model was applied to calculate the summary OR, otherwise, the fixed-effects model was used. Visual inspection of the funnel plot was used to confirm publication bias. Egger’s regression test16 and Begg’s test17 were used to statistically assess publication bias and we performed a sensitivity analysis by excluding one study each time and rerunning the analysis to verify the robustness of the overall results (p < 0.05 was considered statistically significant). All analysis was performed using Stata release 11(Stata Corp, College Station, TX).
Results
Literature search and Study characteristics
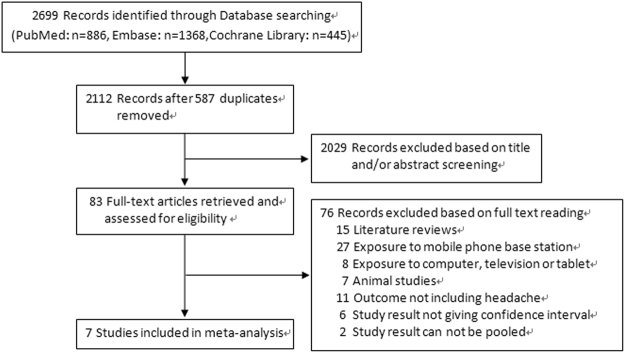
A total of 2,699 articles were identified through literature searching in PubMed, EMbase and Cochrane databases. The studies assessed are described in Fig. 1. After removing duplicate articles and initial screening based on titles and abstract reading, 83 articles remained for full-text reading. Two independent reviewers performed the full-text reading and finally 7 studies18–24 met our inclusion criteria. Of the 76 articles excluded by full-text reading, 15 were review articles, 27 reported headache due to living near MP base station, 8 reported headache due to computer, television or tablet use, 11 reported health outcomes not including headache, 7 were animal studies. There were 8 studies25–32 investigated the association between mobile phone use and headache, but not fulfilled the inclusion criteria. Among them, 6 did not give OR and corresponding 95%CI for association between MP use and headache and 2 study results cannot be pooled.
Figure 1.
Flow diagram of literature search and study selection.
Seven cross-sectional studies involving 21,505 study subjects were included in this meta-analysis. Four studies were conducted in Asia18–20,24 and three studies were conducted in Europe21–23.Five studies18–21,24 assessed the association between MP use or not and headache, two studies22,23 assessed the association between MP calling time and headache, one study23 assessed the association between MP calling frequency and headache. The main characteristics of the included studies are shown in Supplementary Table S1. Main characteristics of the 8 excluded studies are shown in Supplementary Table S2.
Quality assessment
The quality of included studies ranged from moderate to high as illustrated in Supplementary Table S1. Specific assessments of included studies are shown in Supplementary Table S3.
Meta-analysis of MP use and headache risk
MP versus non-MP user
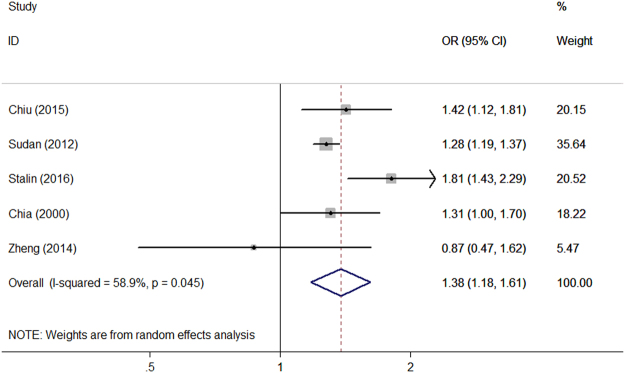
Among the seven included studies, five assessed the association between MP use or not and headache18–21,24. The pooled OR for association between MP use or not and headache are shown in Fig. 2. The combined result revealed higher risk of headache for MP user compared with non-MP user (OR, 1.38; 95% CI, 1.18–1.61) (P < 0.001, I2 = 58.9%).A sensitivity analysis was also performed by excluding one study each time and recalculating the pooled OR for the remaining studies and these data appear in Fig. 3. Visual inspection of the funnel plot did not show evidence of a significant publication bias (Supplementary Figure S1). Begg’s (P = 0.806) and Egger’s regression tests (P = 0.683) indicated no publication bias in this meta-analysis.
Figure 2.
Forest plot of the association between MP use or not and headache.
Figure 3.
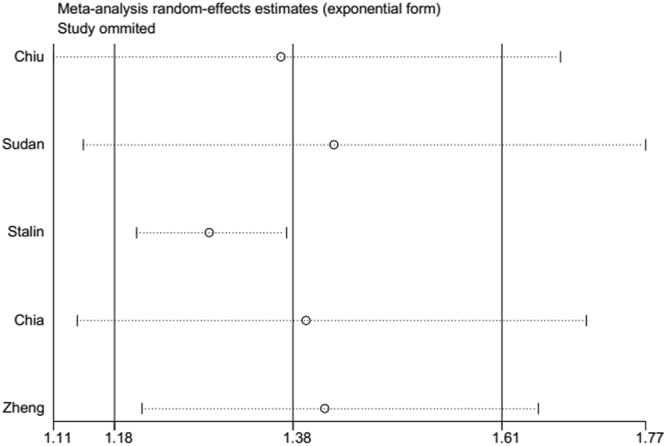
Plot of sensitivity analysis by excluding one study each time and the pooling estimate for the rest of the studies.
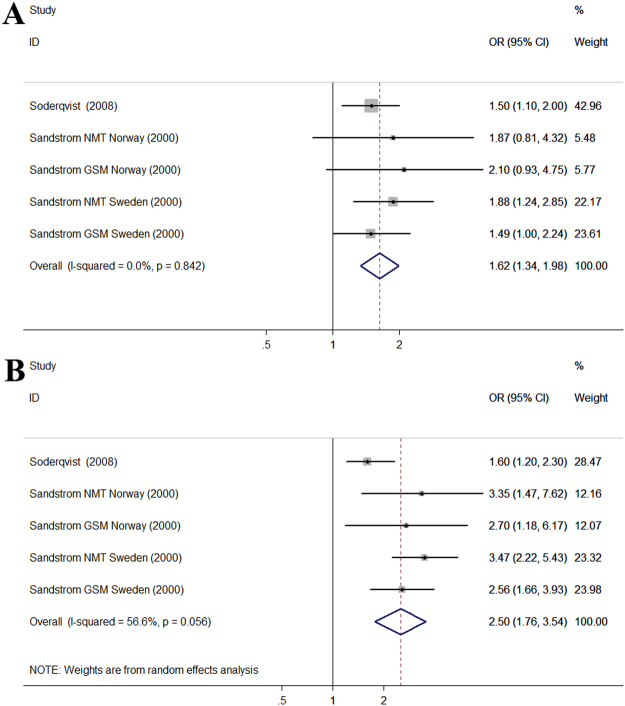
Long versus short MP call duration
Two studies assessed the association between MP call duration and headache. According to the daily MP calling time, MP users were divided into different groups (<2 min group, 2–15 min group, >15 min group) and these data appear in Fig. 4. Compared with the <2 min group, the pooled OR was 1.62 (95% CI, 1.34–1.98) (P < 0.001, I2 = 0.0%) for 2–15 min group and 2.50 (95% CI, 1.76–3.54) (P < 0.001, I2 = 56.6%) for >15 min group. The result showed an increased risk of headache in those who had longer daily MP calling time.
Figure 4.
Forest plot of the association between different MP call duration and headache. (A) Forest plot for 2–15 min group compared with <2 min group; (B) Forest plot for >15 min group compared with <2 min group.
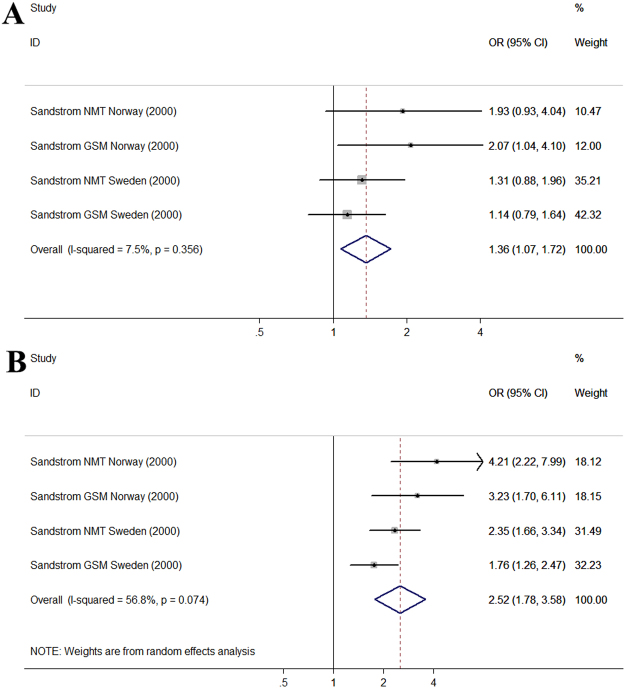
High versus low MP use frequency
Only one study investigated the association between the MP use frequency and headache but the study was performed in two countries and the author respectively assessed the association between digital and analog system MP use frequency and headache. This created 4 study groups and these data appear in Fig. 5. According to the daily MP use frequency, MP users were divided into different groups (<2 calls group, 2–4 calls group, >4 calls group). Compared with the <2 calls group, the pooled OR was 1.37 (95% CI, 1.07–1.76) (P < 0.001, I2 = 7.5%) for 2–4 calls group and 2.52 (95% CI, 1.78–3.58) (P < 0.001, I2 = 56.8%) for >4 calls group. The results showed an increased risk of headache in those who had higher daily MP use frequency.
Figure 5.
Forest plot of the association between different MP call frequency and headache. (A) Forest plot for 2–4 calls group compared with <2 calls group; (B) Forest plot for >4 calls group compared with <2 calls group.
Discussion
To our knowledge, no meta-analysis has examined the relationship between MP use and headache. Our study, based on 7 available cross-sectional studies, first quantified the association of MP use with headache and we noted that MP users had increased risk of headache compared with non-MP users. Among MP users, the risk of headache was also increased in those who had longer daily call duration and higher daily call frequency. This finding substantiates the data demonstrating an association between MP use and an increased risk of headache and emphasizes the daily call duration and frequency as important influencing factors.
Studies to investigate any association between MP use and headache have used different methodologies. The pooled results of our meta-analysis were consistent with most studies and evidence of a significant association between MP use and headache was noted. Studies excluded from our meta-analysis suggested that increased risk of headache was correlated with MP use. Consistent with our results, Redmayne’s group25 found the number and duration of cellphone calls were significantly associated with headache (>6 cellphone calls >10 min weekly, adjusted OR 2.4, 95% CI 1.2–4.8). Szyjkowska and colleagues found that the OR for headache related to MP use longer than 30 min daily was 18.826. In Khan’s study, the percent of chronic headache was related to daily MP use duration (5.03% in ≤30 min group, 24.69% in 30–60 min group, 39.39% in 60–90 min group and 30.76% in >90 min group, p < 0.0001)27. Moreover, in a large national cohort study of 420,095 Danish people, Schuz and colleagues found that standardized hospitalization ratios were increased by 10–30% for migraine in MP users corresponding to time since first subscription to a MP28. In addition, some other studies not included in our meta-analysis also indicated the possible association between MP use and headache29–32.
The underlying mechanism of the association between MP use and headache remains unclear but some suggest that breakdown of the blood-brain barrier due to exposure to low intensity MP frequency microwave energy may be involved33–36. Also, the dopamine-opiate system may be involved in headaches and low intensity electromagnetic energy exposure affects those systems37–39. However, since Frey’s group first reported headaches occurring after microwave energy exposure at approximately the same frequencies and incident energies that present day MP emit40, the exact mechanism under this association is still not fully understood now.
The results of our meta-analysis and lots of previous studies herein supported current clinical opinion that MP use may cause increased risk for headache. Therefore, it is advisable to admit that the use of MP is a risk factor for headache. In Stalin’s study18 and Chiu’s study19, the prevalence of MP usage among adult and children was 69.8% and 63.2% respectively in their study population, and that was only the data from two years ago. We could foresee the prevalence of MP usage will be higher in the future. So it is also advisable to suggest that excessive use of MP should be avoided by increasing social awareness through health promotion activities. It is imperative that health care professionals, clinicians and common people are educated about the deleterious influence of MP on headache. And it is reasonable to instruct children and adolescent about a prudent use of MPs. In addition, we encourage screening of headache patients during routine clinical visits to identify those patients to explore excessive MP use as a potential cause. Intervention and policies must be developed, evaluated and carry out at the population level to raise the awareness of the potential adverse health effect to decrease the headache caused by MP using.
The strengths and limitations of our study should be carefully considered. We have reported a comprehensive meta-analysis based on 7 cross-sectional studies and assessed the association between MP use and headache. And the studies included were all moderate-high quality. Our study only included studies used multiple logistic regression to decrease the effect of confounders for the MP use-headache association. However, our study was limited by the small number of studies available for combining. Meanwhile, all included studies are from Asia and Europe and the age of study population of included studies was not exactly the same. And this may introduce some heterogeneity when the results were combined. More large and high qualitative epidemiologic studies are required to further assess the association between MP use and headache. In addition, further experimental research is needed to explore more on the mechanism of this association.
In conclusion, our meta-analysis suggested that MP use is significantly associated with headache. More experimental and epidemiologic studies are still required to further affirm and understand this association.
Electronic supplementary material
Acknowledgements
This study was supported by grants from the National Science Foundation of China (Grants No. 81471147) and the National Key Technology Support Program (Grant No. 2013BA104B04). We thank LetPub (www.letpub.com) for its linguistic assistance during the preparation of this manuscript.
Author Contributions
J.W. and S.Y.Y. participated in the whole design of this study. J.W. and W.X. performed the database search, data extraction and analysis. J.W., H.S. and S.Y.Y. wrote the draft and revised the whole manuscript. All authors read and approved the final version of the manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-017-12802-9.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Martin R, Patrizia F, Evelyn M, Hug K. Systematic review on the health effects of exposure to radiofrequency electromagnetic felds from mobile phone base stations. Bull World Health Organ. 2010;88:887–896. doi: 10.2471/BLT.09.071852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Martin R, Mirjana M, Yvonne B, Meier M, Braun FC. Symptoms of ill health ascribed to electromagnetic field exposure-a questionnaire survey. Int J Hyg Environ Health. 2004;207:141–150. doi: 10.1078/1438-4639-00269. [DOI] [PubMed] [Google Scholar]
- 3.Nadja S, Anke H, Martin R. The prevalence of symptoms attributed to electromagnetic field exposure: a cross-sectional representative survey in Switzerland. Soz Praventiv Med. 2006;51:202–209. doi: 10.1007/s00038-006-5061-2. [DOI] [PubMed] [Google Scholar]
- 4.Mary R, Euan S, Michael JA. The relationship between adolescents’ well-being and their wireless phone use: a cross-sectional study. Environmental Health. 2013;12:90–102. doi: 10.1186/1476-069X-12-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anna S, Katharina R, Martin R. Symptoms and Cognitive Functions in Adolescents in Relation to Mobile Phone Use during Night. PLoS One. 2015;10:e0133528. doi: 10.1371/journal.pone.0133528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mortazavi SMJ, Ahmadi J, Shariati M. Prevalence of Subjective Poor Health Symptoms Associated With Exposure to Electromagnetic Fields Among University Students. Bioelectromagnetics. 2007;28:326–330. doi: 10.1002/bem.20305. [DOI] [PubMed] [Google Scholar]
- 7.Szyjkowska A, Gadzicka E, Szymczak W, Bortkiewicz A. The risk of subjective symptoms in mobile phone users in Poland-an epidemiological study. Int J Occup Med Environ Health. 2014;27:293–303. doi: 10.2478/s13382-014-0260-1. [DOI] [PubMed] [Google Scholar]
- 8.Khan MM. Adverse effects of excessive mobile phone use. Int J Occup Med Environ Health. 2008;21:289–293. doi: 10.2478/v10001-008-0028-6. [DOI] [PubMed] [Google Scholar]
- 9.GBD 2015 Healthcare Access and Quality Collaborators. Healthcare Access and Quality Index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990–2015: a novel analysis from the Global Burden of Disease Study 2015. Lancet. pii: S0140-6736(17)30818-8 (2017). [DOI] [PMC free article] [PubMed]
- 10.Oftedal G, Wilen J, Sandstrom M, Mild KH. Symptoms experienced in connection with mobile phone use. Occup Med (Lond). 2000;50:237–245. doi: 10.1093/occmed/50.4.237. [DOI] [PubMed] [Google Scholar]
- 11.Hocking B. Preliminary report: symptoms associated with mobile phone use. Occup Med (Lond). 1998;48:357–360. doi: 10.1093/occmed/48.6.357. [DOI] [PubMed] [Google Scholar]
- 12.Frey AH. Headaches from cellular telephones: are they real and what are the implications? Environ Health Perspect. 1998;106:101–103. doi: 10.1289/ehp.98106101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 14.Wells, G.A., et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomized studies in metaanalyses. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. (2014)
- 15.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Egger M, Davey SG, Schneider M. & Minder, C. Bias in meta-analysis detected by a simple graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 18.Stalin P, et al. Mobile Phone Usage and its Health Effects Among Adults in a Semi-Urban Area of Southern India. J Clin Diagn Res. 2016;10:14–16. doi: 10.7860/JCDR/2016/16576.7074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chiu CT, Chang YH, Chen CC, Ko MC, Li CY. Mobile phone use and health symptoms in children. J Formos Med Assoc. 2015;114:598–604. doi: 10.1016/j.jfma.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 20.Zheng F, et al. Association between mobile phone use and self-reported well-being in children: a questionnaire-based cross-sectional study in Chongqing. China. BMJ Open. 2014;5:e007302. doi: 10.1136/bmjopen-2014-007302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sudan M, Kheifets L, Arah O, Olsen J, Zeltzer L. Prenatal and Postnatal Cell Phone Exposures and Headaches in Children. Open Pediatr Med Journal. 2012;6:46–52. doi: 10.2174/1874309901206010046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Söderqvist F, Carlberg M, Hardell L. Use of wireless telephones and self-reported health symptoms: a population-based study among Swedish adolescents aged 15-19 years. Environ Health. 2008;7:18. doi: 10.1186/1476-069X-7-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sandström M, Wilen J, Oftedal G, Hansson MK. Mobile phone use and subjective symptoms. Comparison of symptoms experienced by users of analogue and digital mobile phones. Occup Med (Lond) 2001;51:25–35. doi: 10.1093/occmed/51.1.25. [DOI] [PubMed] [Google Scholar]
- 24.Chia SE, Chia HP, Tan JS. Prevalence of headache among handheld cellular telephone users in Singapore: a community study. Environ Health Perspect. 2000;108:1059–1062. doi: 10.1289/ehp.001081059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Redmayne M, Smith E, Abramson MJ. The relationship between adolescents’ well-being and their wireless phone use: a cross-sectional study. Environmental Health. 2013;12:90. doi: 10.1186/1476-069X-12-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Szyjkowska A, Gadzicka E, Szymczak W, Bortkiewicz A. The risk of subjective symptoms in mobile phone users in Poland-an epidemiological study. International Journal of Occupational Medicine and Environmental Health. 2014;27:293–303. doi: 10.2478/s13382-014-0260-1. [DOI] [PubMed] [Google Scholar]
- 27.Khan MM. Adverse effects of excessive mobile phone use. International Journal of Occupational Medicine and Environmental Health. 2008;21:289–293. doi: 10.2478/v10001-008-0028-6. [DOI] [PubMed] [Google Scholar]
- 28.Schüz J, Waldemar G, Olsen JH, Johansen C. Risks for Central Nervous System Diseases among Mobile Phone Subscribers: A Danish Retrospective Cohort Study. PLoS One. 2009;4:e4389. doi: 10.1371/journal.pone.0004389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cho YM, et al. A cross-sectional study of the association between mobile phone use and symptoms of ill health. Environ Health Toxicol. 2016;31:e2016022. doi: 10.5620/eht.e2016022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Balikci K. Cem, Ozcan.I., Turgut-Balik, D. & Balik, H.H. A survey study on some neurological symptoms and sensations experienced by long term users of mobile phone. Pathol Biol (Paris). 2005;53:30–34. doi: 10.1016/j.patbio.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 31.Küçer N, Pamukçu T. Self-reported symptoms associated with exposure to electromagnetic fields: a questionnaire study. Electromagn Biol Med. 2014;33:15–17. doi: 10.3109/15368378.2013.783847. [DOI] [PubMed] [Google Scholar]
- 32.Mortazavi SM, Ahmadi J, Shariati M. Prevalence of subjective poor health symptoms associated with exposure to electromagnetic fields among university students. Bioelectromagnetics. 2007;28:326–330. doi: 10.1002/bem.20305. [DOI] [PubMed] [Google Scholar]
- 33.Sandyk R, Awerbuch GI. The co-occurrence of multiple sclerosis and migraine headache: the serotoninergic link. lnt. J Neurosci. 1994;76:249–257. doi: 10.3109/00207459408986007. [DOI] [PubMed] [Google Scholar]
- 34.Janigro D, West GA, Nguyen TS, Winn HR. Regulation of blood-brain barrier endothelial cells by nitric oxide. Circ Res. 1994;75:528–538. doi: 10.1161/01.RES.75.3.528. [DOI] [PubMed] [Google Scholar]
- 35.Winkler T, Sharma HS, Stalberg E, Olsson Y, Dey PK. Impairment of blood-brain barrier function by serotonin induces desynchronization of spontaneous cerebral cortical activity: experimental observations in the anaesthetized rat. Neuroscience. 1995;68:1097–1104. doi: 10.1016/0306-4522(95)00194-N. [DOI] [PubMed] [Google Scholar]
- 36.Frey AH, Feld S, Frey B. Neural function and behavior: defining the relationship. Ann NY Acad Sci. 1975;247:433–438. doi: 10.1111/j.1749-6632.1975.tb36019.x. [DOI] [PubMed] [Google Scholar]
- 37.Del ZM, Lai M, Loi V, Pisano MR. Dopamine hypersensitivity in migraine: role in apomorphine syncope. Headache. 1995;35:222–224. doi: 10.1111/j.1526-4610.1995.hed3504222.x. [DOI] [PubMed] [Google Scholar]
- 38.Villeneuve A. Pathophysiology and treatment of negative symptoms. Can J Psychiatry. 1994;39:53–58. [PubMed] [Google Scholar]
- 39.Barbanti P, et al. Increased density of dopamine D5 receptor in peripheral blood lymphocytes of migraineurs: a marker for migraine? Neurosci Lett. 1996;207:73–76. doi: 10.1016/0304-3940(96)12491-5. [DOI] [PubMed] [Google Scholar]
- 40.Frey AH. Human auditory system response to modulated electromagnetic energy. J Appl Physiol. 1962;17:689–692. doi: 10.1152/jappl.1962.17.4.689. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.