Abstract
Background & Aims
Systemic cellular immunity elicited by the Ty21a oral typhoid vaccine has been extensively characterized. However, very limited data are available in humans regarding mucosal immunity at the site of infection (terminal ileum [TI]). Here we investigated the host immunity elicited by Ty21a immunization on terminal ileum–lamina propria mononuclear cells (LPMC) and peripheral blood in volunteers undergoing routine colonoscopy.
Methods
We characterized LPMC-T memory (TM) subsets and assessed Salmonella enterica serovar Typhi (S Typhi)–specific responses by multichromatic flow cytometry.
Results
No differences were observed in cell yields and phenotypes in LPMC CD8+-TM subsets following Ty21a immunization. However, Ty21a immunization elicited LPMC CD8+ T cells exhibiting significant S Typhi–specific responses (interferon-γ, tumor necrosis factor-α, interleukin-17A, and/or CD107a) in all major TM subsets (T-effector/memory [TEM], T-central/memory, and TEM-CD45RA+), although each TM subset exhibited unique characteristics. We also investigated whether Ty21a immunization elicited S Typhi–specific multifunctional effectors in LPMC CD8+ TEM. We observed that LPMC CD8+ TEM responses were mostly multifunctional, except for those cells exhibiting the characteristics associated with cytotoxic responses. Finally, we compared mucosal with systemic responses and made the important observation that LPMC CD8+S Typhi–specific responses were unique and distinct from their systemic counterparts.
Conclusions
This study provides the first demonstration of S Typhi–specific responses in the human terminal ileum mucosa and provides novel insights into the generation of mucosal immune responses following oral Ty21a immunization.
Keywords: Lamina Propria Mononuclear Cells, Multifunctional T Cells, CD8+-T Memory Cells, Typhoid, Vaccines
Abbreviations used in this paper: CMI, cell-mediated immune responses; EBV-B, Epstein-Barr virus–transformed lymphoblastoid B cells; IFN, interferon; IL, interleukin; LPMC, lamina propria mononuclear cells; MF, multifunctional; MIP, macrophage inflammatory protein; PBMC, peripheral blood mononuclear cells; S, S Typhi–specific single producing cells; TCM, T-central/memory (CD62L+CD45RA-); TEM, T-effector/memory (CD62L-CD45RA-); TEMRA, TEM-CD45RA+ (CD62L-CD45RA+); TM, CD8+ T memory; TI, terminal ileum; TNF, tumor necrosis factor; wt, wild-type
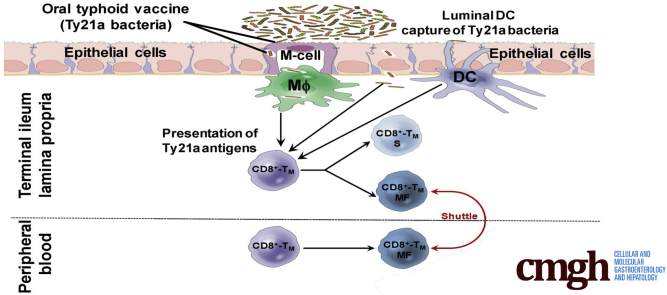
Graphical abstract
See editorial on page 439.
Summary.
This study examines mucosal immune responses to administration of the oral Ty21a-typhoid vaccine in humans. Local antigen-specific CD8+-TM responses were substantially different from those observed systemically. These data have broad implications in human mucosal immune regulation and approaches to oral immunization.
The causative agent of typhoid fever, Salmonella enterica serovar Typhi (S Typhi), is a human restricted pathogen that constitutes a major global health threat. Annually, S Typhi infection leads to an estimated 26.9 million cases of typhoid fever resulting in approximately 217,000 deaths worldwide.1, 2 Following ingestion, S Typhi invades the host mucosal surfaces mostly via M cells, which are specialized epithelial cells covering the Peyer patches. Subsequently, S Typhi translocates to the submucosa where it encounters intestinal lymphoid tissues, before entering draining mesenteric lymph nodes, and disseminating to the liver, spleen, and other secondary lymphoid tissues, resulting in systemic illness.3 Although S Typhi can potentially invade at any site harboring M cells along the intestine,4 the human terminal ileum (TI), where most of Peyer patches in the intestine are concentrated,5 is the favored intestinal active invasion site for S Typhi.3 In S Typhi–infected patients in developing countries, one of the most common complications of typhoid fever are multiple intestinal perforations that occur almost exclusively in the TI. This evidence from the clinic argues strongly that the TI is the major site of infection for S Typhi. Only very limited information is available regarding the generation of cell-mediated immune responses (CMI) to S Typhi in the human intestinal mucosa.6, 7 Moreover, to our knowledge, there are no data on the induction of CMI responses to S Typhi in the TI mucosa following wt S Typhi infection or immunization with the live attenuated oral vaccine Ty21a (Ty21a). Thus, a better understanding of the host mucosal immune responses against S Typhi and other enteric pathogens at their preferred site of natural infection is required to provide additional insights for the development of oral vaccines.
Currently, 2 licensed typhoid vaccines are available in the United States for use in humans including Ty21a.8, 9 Ty21a is typically administered in 4 spaced doses and confers a moderate level of long-lived protection (60%–80%; 5–7 years).10, 11, 12 Hence, there is a need to develop effective new vaccines that provide durable, long-lasting protection. The assessment of mucosal immune responses at the site of infection (TI) may allow the identification of immune correlates of protection, which has the potential to greatly contribute to the development of new generations of attenuated typhoid vaccines. Our group and others have extensively studied the induction of humoral and CMI responses in peripheral blood mononuclear cells (PBMC) obtained from healthy volunteers following immunization with 4 doses of Ty21a.13, 14, 15, 16, 17, 18, 19 These studies showed that live oral S Typhi vaccines induced both CD4+ and CD8+ T-cell responses, including cytotoxic T cells, proliferation, and multifunctional (MF) antigen-specific cytokine-producing cells.12, 13, 14, 16, 20, 21, 22 We also reported that Ty21a elicits S Typhi–specific CD8+ T-cell responses in PBMC by various CD8+ T memory (TM) cell subsets, including T central memory (TCM), T effector/memory (TEM), and RA+TEM (TEMRA)16, 23 and that these responses are predominantly in the TEM and TEMRA subsets with a low magnitude of responses observed in CD8+ TCM subsets.12, 21, 23 Recent reports have indicated that various vaccines, including Ty21a, have the capacity to induce antigen-specific MF T cells (cells that produced 2 or more responses), which might play a key role in long-term immunity.12, 21, 23 However, these detailed CMI responses were assessed in peripheral blood. CMI responses in the human TI have never been directly investigated. We hypothesized that S Typhi–specific responses by various CD8+ TM subsets elicited in the TI following Ty21a immunization would differ in magnitude and characteristics from their systemic counterparts.
In this study we have characterized TI–lamina propria mononuclear cells (LPMC) TM in Ty21a-vaccinated and unvaccinated volunteers. We then determined and compared CD8+ TM S Typhi–specific responses from the 2 groups following stimulation with autologous target cells infected with wild-type (wt) S Typhi. Finally, we assessed these responses in depth by analyzing their multifunctionality and directly compared peripheral and mucosal CD8+ TEM MF responses. These comparisons provide a unique insight between mucosal and peripheral immunity.
Materials and Methods
Volunteers, Immunization, and Sample Collection
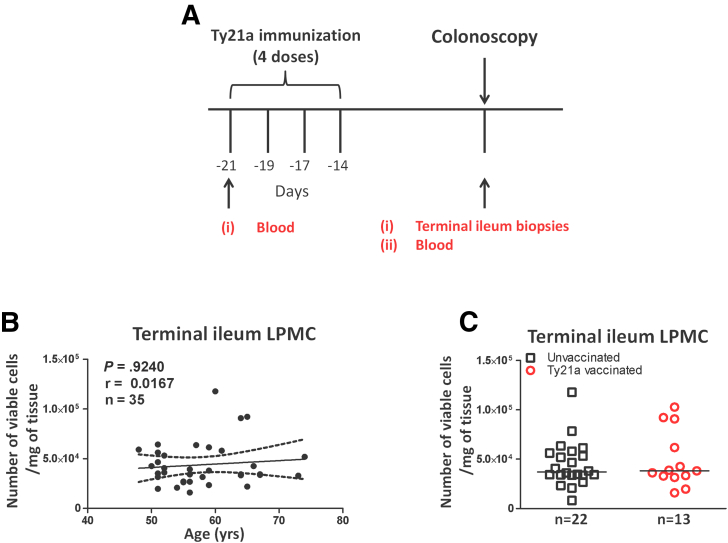
Healthy volunteers undergoing routine, medically indicated colonoscopies who had no history of typhoid fever were recruited from the Baltimore-Washington metropolitan area and University of Maryland, Baltimore campus. Written informed consent was obtained from volunteers and all procedures were approved by the University of Maryland, Baltimore Institutional Review Board. Volunteers (aged 49–74 years) were assigned into 2 groups. The first group (n = 13) received the 4 recommended doses of Ty21a vaccine (Vivotif enteric-coated capsules, Crucell, Bern, Switzerland), whereas volunteers assigned to the second group were not vaccinated (control group) (n = 22) as shown in the study design (Figure 1A). Blood samples were collected at least 21 days before immunization (preimmunization) and on colonoscopy day (Day 0; postvaccination). Using large capacity forceps, TI biopsies were obtained only on colonoscopy day (Day 0; postvaccination) as stated in the approved Institutional Review Board protocol (Figure 1A). PBMC were isolated immediately after blood draws by density gradient centrifugation and cryopreserved in liquid nitrogen following standard techniques.21
Figure 1.
Study design and cell yields of terminal ileum LPMC isolated from Ty21a-vaccinated and unvaccinated volunteers. (A) Oral typhoid vaccine Ty21a dosage schedule (4 doses at -21 to -14 days) and time of collection of specimens (blood and TI biopsies) from volunteers undergoing routine screening colonoscopies. Autologous EBV-B cells are generated from preimmunized blood. (B) Cell yield (number of viable cells/mg of tissue) was correlated to the age of volunteers (n = 35) using Pearson correlation test. (C) Cell yield comparison between Ty21a-vaccinated and unvaccinated volunteers. Median values for each group are denoted as horizontal black bars.
Isolation of LPMC From Terminal Ileum Biopsies
TI-LPMC were freshly isolated as described previously.24, 25 Briefly, after collection of biopsies from routine colonoscopy volunteers, tissues were treated with HBSS (without CaCl2, MgCl2, MgSO4; Gibco, Carlsbad, CA) and EDTA (1 mM; Ambion, Grand Island, NY) to remove intraepithelial cells. LPMC were then isolated following enzymatic digestion of the biopsies with Collagenase D (100 μg/mL; Roche, Indianapolis, IN) and DNase I (10 μg/mL; Affymetrix, Cleveland, OH) and homogenization using the Bullet Blender homogenizer (Next Advance Inc, Averill, NY). Cells were then washed and resuspended in complete medium (RPMI 1640 [Gibco Invitrogen, Carlsbad, CA] supplemented with 10% heat-inactivated fetal bovine serum [BioWhittaker, Walkersville, MD], 2 mM l-glutamine [HyClone, Logan, UT], 2.5 mM sodium pyruvate [Gibco], and 10 mM HEPES [Gibco], 100 U/mL penicillin [Sigma-Aldrich, St. Louis, MO], 100 μg/mL streptomycin [Sigma-Aldrich], and 50 μg/mL gentamicin [Gibco]) and counted using Kova Glastic Slides (Hycor Biomedical, Garden Grove, CA). Cells were either stained immediately for immune-phenotyping by flow cytometry or stimulated overnight with S Typhi–infected targets before staining (see later).
Target Cell Preparation
Autologous Epstein-Barr virus (EBV)-transformed lymphoblastoid cell line (EBV-B cells) were generated from each participant’s preimmunization PBMC (at least 21 days before colonoscopy) (Figure 1A) as previously described.14, 21 Briefly, EBV-B cells were obtained by incubation of the PBMC with EBV-containing supernatant from the B95-8 cell line (ATCC CRL1612) and cyclosporine (0.5 μg/mL; Sigma-Aldrich) at 37°C with 5% CO2 for 2–4 weeks.
S Typhi Infection of Target Cells
Autologous target cells (EBV-B) generated as described previously were infected with wt S Typhi strain ISP1820 at a multiplicity of infection of 7:1 by incubation for 3 hours at 37°C in RPMI without antibiotics, washed 3 times with complete RPMI and incubated overnight with complete RPMI containing 150 μg/mL gentamicin. Cells were washed and infection with S Typhi confirmed by staining with anti-Salmonella common structural Ag (CSA-1, Kierkegaard and Perry, Gaithersburg, MD) and analyzed by flow cytometry as previously described.13
Stimulation of PBMC and Terminal Ileum LPMC
Freshly isolated TI-LPMC and PBMC were used as effector cells. Briefly, LPMC and PBMC were cocultured, respectively, with either noninfected or S Typhi–infected EBV-B (MOI of 7:1). LPMC and PBMC cultured with media only or in the presence of α-CD3/CD28 (Life technologies, Grand Island, NY) were used as negative and positive controls, respectively. At the time of stimulation, antihuman CD107a-FITC (5 μL; H4A3, BD, San Jose, CA) was added. After 2 hours, 0.5 μl of Golgi Stop (Monensin, BD) and Golgi Plug (Brefeldin A, BD) were added and cultures continued overnight at 37°C in 5% CO2.
Surface and Intracellular Staining
Following stimulation in the presence of CD107a (LAMP-1, a molecule expressed on the cell membrane that is widely accepted to be associated with cytotoxic T-cell activity26), PBMC and LPMC were stained for live/dead discrimination (YEVID) (Invitrogen, Carlsbad, CA). Blocking of Fc receptors was performed using human immunoglobulin (3 μg/mL; Sigma) and was followed by surface staining. Briefly, cells were stained with fluorescently labeled monoclonal antibodies directed to CD13-Pacific Orange (conjugated in-house), CD19-BV570 (HIB19, Biolegend, San Diego, CA), CD3-BV650 (OKT3, Biolegend), CD4-PE-Cy5 (RPA-T4, BD), CD8-PerCP-Cy5.5 (SK1, BD), CD45RA-biotin (HI100, BD), CD62L-APC-A780 (DREG-56, eBioscience, San Diego, CA), and integrin α4β7-A647 (ACT1; conjugated in-house) at 4°C for 30 minutes. Cells were washed with wash buffer and stained with streptavidin (SAV)-Qdot800 (Invitrogen) at 4°C for 30 minutes. Cells were then fixed and permeabilized using IC fixation and permeabilization buffers (8222/8333, eBioscience) according to the manufacturer’s recommendations. This was followed by staining with monoclonal antibodies directed to interleukin (IL)-17A-BV421 (BL168, Biolegend), interferon (IFN)-γ-PE-Cy7 (B27, BD), tumor necrosis factor (TNF)-α-Alexa 700 (MAb11, BD), and CD69-ECD (TP1.55.3, Beckman Coulter, Danvers, MA), IL2-BV605 (MQ1-17H12, Biolegend), and macrophage inflammatory protein (MIP)-1β-PE (IC271P, R&D) was performed at 4°C overnight. After staining, cells were stored in 1% paraformaldehyde at 4°C until data collection. Data were collected using a customized LSRII flow cytometer (BD) and then analyzed using the WinList version 7 (Verity Software House, Topsham, ME) software package. S Typhi–specific responses were expressed as net percentage of positive cells (background after stimulation with uninfected cells were subtracted from values obtained with S Typhi–infected stimulators). A response was considered specific if the differential in the number of positive events between experimental (S Typhi–infected targets) and negative control (uninfected targets) cultures was significantly increased by z-tests. The FCOM function of WinList was used to determine S Typhi–specific MF responses in TI LPMC and PBMC following vaccination.
Statistical Analysis
Data were analyzed using the statistical software GraphPad Prism version 5.03 (Graphpad, San Diego, CA). Statistical differences in median values between 2 groups were determined using Mann-Whitney tests. Wilcoxon matched pair tests were used to assess statistical differences between LPMC and PBMC paired responses. Correlations (cell yield v/s age and PBMC v/s LPMC S Typhi–specific responses) were evaluated using Spearman correlation tests.
Results
Oral Ty21a Immunization Does Not Alter Mucosal T-Cell Yield and Phenotype
Oral Ty21a immunization on human TI-LPMC TM subsets (yield and phenotype) in healthy volunteers is unknown. To explore whether Ty21a immunization may influence (1) cell yields, (2) frequencies of TM subsets, and (3) expression of homing molecules, we isolated TI-LPMC from volunteers who either received 4 doses of Ty21a (n = 13) or were unvaccinated (n = 22). We first verified that the volunteers’ age was not a factor influencing cell yield (number of viable cells/mg of tissue) by performing Spearman correlation tests. No significant correlation (r = 0.0167; P = .924) was observed between LPMC cell yield and age of the volunteers (Figure 1B). We then compared the cell yield obtained from biopsies of Ty21a-vaccinated (n = 13) and unvaccinated (n = 22) volunteers. Cumulative data showed that the median cell yield of TI-LPMC was approximately 4 × 104 viable cells/mg of tissue (Figure 1C). No significant differences (P < .05) in cell yield of TI-LPMC were detected between the 2 groups (Figure 1C).
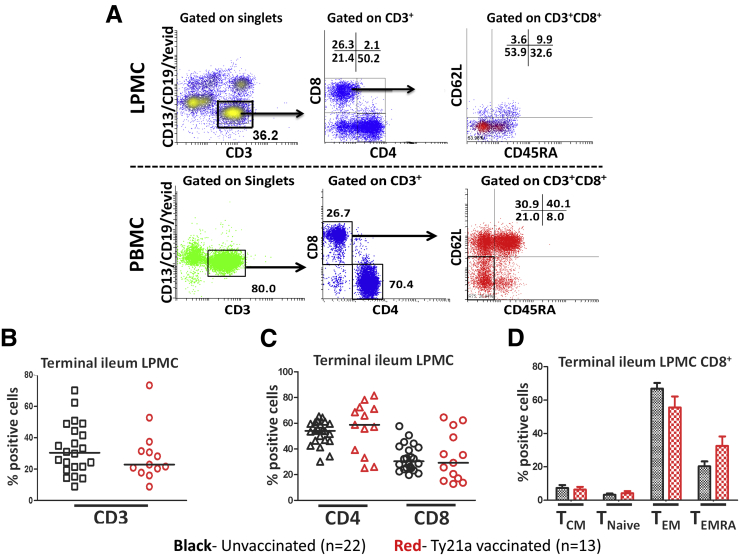
Next we characterized T cells and TM subsets from freshly isolated TI-LPMC obtained from biopsies of Ty21a-vaccinated and unvaccinated volunteers (Figure 2A). Interestingly, no significant differences were observed in total LPMC CD3+ T cells following Ty21a immunization (Figure 2B). We then examined the frequency of LPMC CD4+ and CD8+ T-cell subsets. As expected, the frequency of LPMC CD4+ (median, 60%) is higher than LPMC CD8+ T cells (median, 30%) (Figure 2A and C). Cumulative data showed that there were no significant differences in CD4+ and CD8+ frequencies between Ty21a-vaccinated (n = 13) and unvaccinated (n=22) volunteers (Figure 2C). Here, we focused on CD8+ T cells because of the higher magnitude and quality of S Typhi–specific responses in CD8+ than in CD4+ T-cell subsets following Ty21a immunization. S Typhi–specific CD4+ T cells responses following vaccination will be reported separately. We subsequently assessed CD8+ TM using CD62L and CD45RA as shown by the gating strategy (Figure 2A). As expected, cells expressing the TEM (CD62L-CD45RA-) phenotype constitute the predominant TM (∼65%) subset at the TI mucosa followed by the TEMRA (CD62L-CD45RA+) (∼20%) and TCM (CD62L+CD45RA-) (∼10%) subsets (Figure 2A). Cumulative data showed that the percentage of CD8+ TEM, TEMRA, and TCM subsets were not significantly different between Ty21a-vaccinated (n = 13) and unvaccinated (n = 22) volunteers (Figure 2D). Taken together, these data indicate that Ty21a immunization does not seem to alter the frequency of CD8+-TM.
Figure 2.
Gating strategy for identifying terminal ileum (LPMC) and peripheral blood (PBMC) TM subsets and frequencies of LPMC T cells isolated from Ty21a-vaccinated and unvaccinated volunteers. (A) CD8+ TM subsets were observed in terminal ileum LPMC, and PBMC using the CD62L and CD45RA markers following the strategy shown in the figure. (B) Frequencies of CD3 and (C) CD4 and CD8 were measured and compared between TI-LPMC obtained from Ty21a-vaccinated (n = 13; red symbols) and unvaccinated volunteers (n = 22; black symbols). (D) Comparison of TM subsets (CD62L+CD45RA-), TEM (CD62L-CD45RA-), TEMRA (CD62L-CD45RA+), and Tnaive (CD62L+CD45RA+) in TI-LPMC CD8+ T cells obtained from Ty21a-vaccinated and unvaccinated volunteers. Median values for each group are denoted as horizontal black bars.
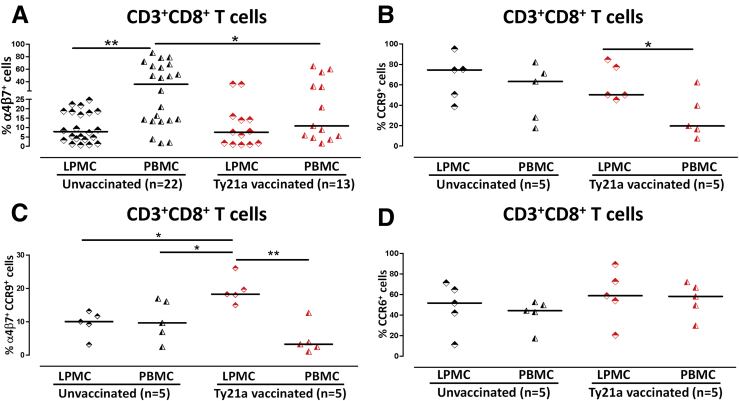
As previously reported, immunization with Ty21a primed immune cells for mucosal homing, including S Typhi–specific T cells coexpressing the gut-homing molecule integrin α4β7.7, 23, 27 However, there are no reports of the expression of homing markers in human TI to demonstrate the potential retention of these incoming cells. To directly address this key issue, we determined the ex vivo frequencies of CD8+-T cells expressing the homing markers integrin α4β7, CCR9, and CCR6 obtained from TI biopsies and their corresponding PBMC. Our results show that the frequency of PBMC total CD8+ T cells expressing integrin decreases significantly (P < .05) following Ty21a immunization (Figure 3A). However, no significant differences were observed in the frequencies of LPMC CD8+-T cells expressing integrin α4β7 between Ty21a-vaccinated (n = 13) and unvaccinated (n = 22) volunteers (Figure 3A). Interestingly, the frequency of total integrin α4β7+CD8+ T cells was significantly lower (P < .05) in LPMC than in PBMC in unvaccinated volunteers but not in Ty21a-vaccinated volunteers (Figure 3A). To further understand the homing pattern on TI-LPMC and their corresponding PBMC, we evaluated the frequency of CCR9+CD8+ T cells in a subset of volunteers (n = 5) in both groups. The frequency of LPMC CCR9+CD8+ T cells was not significantly different following Ty21a immunization, a finding similar to the observation with integrin α4β7, whereas PBMC CCR9+CD8+ T frequencies exhibited a trend to be lower in Ty21a-vaccinated (n = 5) than in unvaccinated volunteers (n = 5) (Figure 3B). In addition, we observed that the frequency of LPMC CCR9+CD8+ T cells was significantly higher (P < .05) than PBMC CCR9+CD8+ T cells following Ty21a immunization (Figure 3B). In contrast, no significant differences were observed in CCR9+CD8+ T frequencies between LPMC and PBMC in unvaccinated volunteers (Figure 3B).
Figure 3.
Ex vivo mucosal and systemic homing phenotypes of CD8+ T cells following Ty21a oral vaccination. (A) Ex vivo percentages of integrin α4β7+ cells were evaluated in TI-LPMC and PBMC CD8+ T cells isolated from biopsies and blood of Ty21a-vaccinated (n = 13; red symbols) and unvaccinated (n = 22; black symbols) volunteers. (B) Ex vivo percentages of CCR9+, (C) integrin α4β7+CCR9+, and (D) CCR6+ cells were determined in TI-LPMC and PBMC CD8+ T cells isolated from biopsies and blood from Ty21a-vaccinated (n = 5; red symbols) and unvaccinated (n = 5; black symbols) volunteers. Significant differences between TI-LPMC and PBMC in vaccinated and unvaccinated volunteers are denoted as *P < .05 and **P < .005. Median values for each group are denoted as horizontal black bars.
We then determined the frequency of integrin α4β7+CCR9+CD8+ T cells in LPMC and PBMC in both groups of volunteers. Interestingly, no differences were observed in the frequencies of integrin α4β7+CCR9+CD8+ T cells between LPMC and PBMC in unvaccinated volunteers (Figure 3C). In contrast, following Ty21a immunization we observed a significant increase (P < .005) in integrin α4β7+CCR9+CD8+ T cells in TI-LPMC as compared with PBMC (Figure 3C). In fact, significantly higher levels (P < .05) were observed in the frequency of integrin α4β7+CCR9+CD8+ T cells in LPMC obtained from Ty21a-vaccinees compared with unvaccinated LPMC and PBMC (Figure 3C). We also characterized the expression of the homing marker CCR6 on CD8+ T cells in PBMC and LPMC obtained from both groups. No significant differences were observed in the frequency of LPMC and PBMC CCR6+CD8+ T cells between Ty21a-vaccinated and unvaccinated volunteers (Figure 3D). In sum, our results indicate that CCR9+ integrin α4β7+ CD8+ T cells accumulate in the TI LP and may represent S Typhi–responsive cells that have been recruited from circulation to the local microenvironment.
Activation of Terminal Ileum LPMC CD8+ T Cells
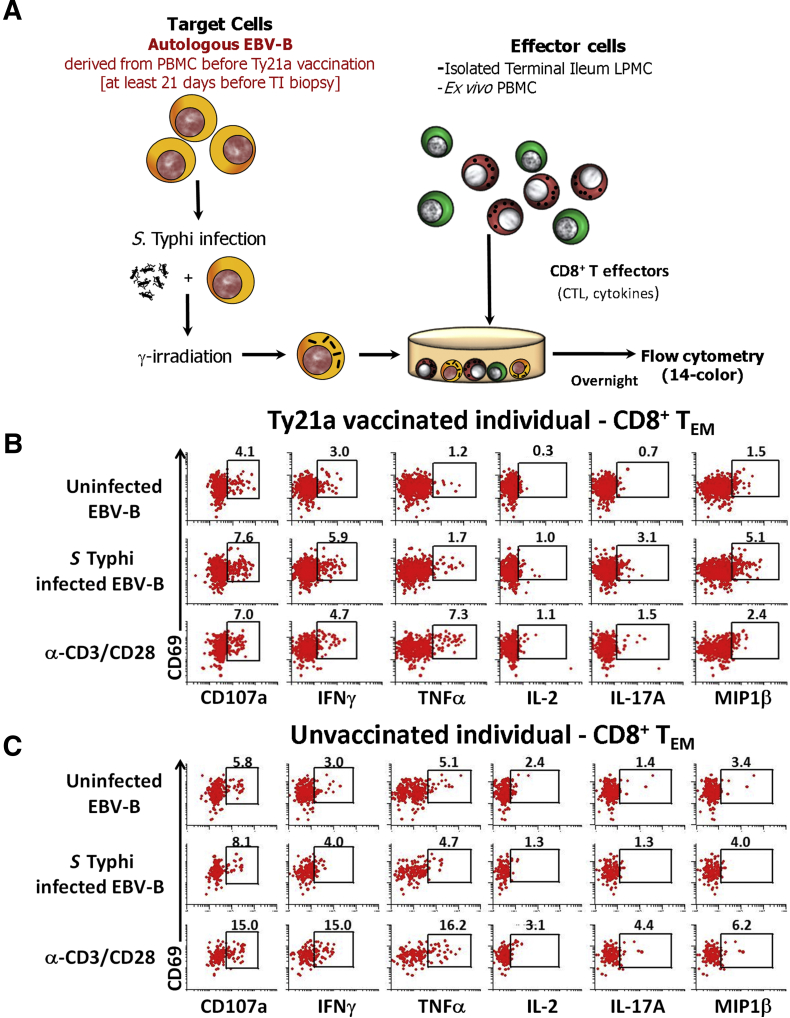
Most of our knowledge of CMI responses elicited by S Typhi infection or Ty21a immunization in humans is based solely on data derived from blood.12 Virtually, no information is available on TI immune responses following wt S Typhi infection or immunization with Ty21a vaccine. To address this gap, we determined the ability of LPMC CD8+ T cells obtained from Ty21a-vaccinated (n = 13) and unvaccinated (n = 22) volunteers to be activated following coculture with autologous S Typhi–infected or uninfected EBV-B cells (Figure 4A). Responses of representative subjects are presented in Figure 4B and C. Following stimulation with S Typhi–infected EBV-B, we observed in Ty21a-vaccinees substantial net increases in the frequencies of CD8+ T cells producing cytokines/chemokines INF-γ (2.9%), TNF-α (0.5%), IL2 (0.7%), IL17A (2.4%), and MIP-1β (3.6%) and higher expression of the cytotoxicity marker CD107a (3.5%) (Figure 4B). In contrast, the level of induction of cytokines/chemokines in unvaccinated volunteers (INF-γ, 1.0%; TNF-α, 0%; IL2, 0%; IL17A, 0%; and MIP-1β, 0.7%) and expression of CD107a (2.3%) was modest following stimulation with S Typhi–infected EBV-B (Figure 4C).
Figure 4.
Stimulation protocol and S Typhi–specific responses in LPMC CD8+ T cells isolated from terminal ileum of a Ty21a-vaccinated and an unvaccinated representative volunteer. (A) Drawing depicting the experimental design for S Typhi infection and measurement of CD8+ T effector function following stimulation of effector LPMC or PBMC to determine S Typhi–specific responses in Ty21a vaccinated and unvaccinated volunteers. (B) Ty21a-vaccinated and (C) unvaccinated volunteers showing the induction of cytokine/chemokine production (IFN-γ, TNF-α, IL2, IL17A, and MIP-1β) and upregulation of CD107a expression in CD69+CD8+ TEM cells following stimulation by noninfected or S Typhi–infected autologous EBV-B cells. Anti-(α)-CD3/CD28 stimulation was used as a positive control in both volunteers. The percentages of positive cells in the gated regions are shown above the corresponding black boxes.
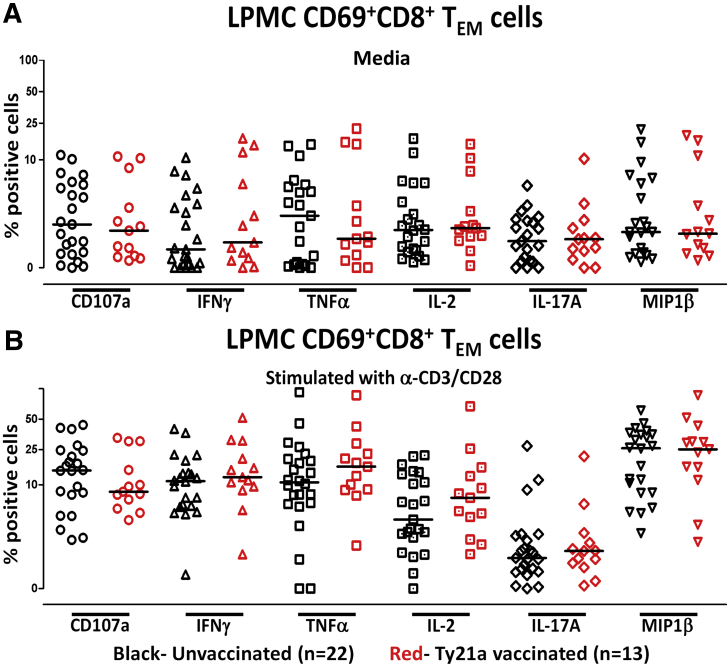
To assess whether S Typhi–specific mucosal responses following Ty21a immunization were caused by baseline responses or capacity to be activated between LPMC CD8+ T cells isolated from Ty21a-vaccinated and unvaccinated volunteers, we assessed the levels of CD8+ TEM cytokines/cytotoxic-producing cells when LPMC cells were cultured overnight either alone (unstimulated) or following stimulation with α-CD3/CD28 beads. Cumulative data show that neither the background levels (LPMC alone) nor their activation with anti-CD3/CD28 beads were significantly different between LPMC isolated from Ty21a-vaccinated and unvaccinated biopsies (Figure 5A and B).
Figure 5.
Characteristics of terminal ileum LPMC CD8+ TEM obtained from Ty21a-vaccinated and unvaccinated volunteers. (A) Comparison of background levels of cytokines/chemokines (IFN-γ, TNF-α, IL2, IL17A, and MIP-1β) and CD107a expression in unstimulated LPMC CD8+ TEM obtained from Ty21a-vaccinated and unvaccinated volunteers. (B) Comparison of LPMC CD8+ TEM responses (IFN-γ, TNF-α, IL2, IL17A, MIP-1β, and CD107a) obtained from Ty21a-vaccinated and unvaccinated volunteers following stimulation with α-CD3/CD28 beads. Median values for each group are denoted as horizontal black bars.
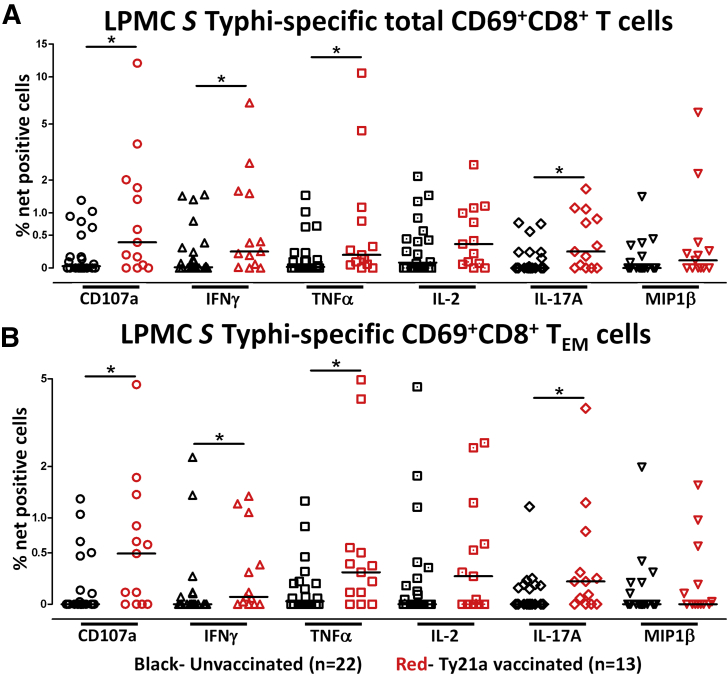
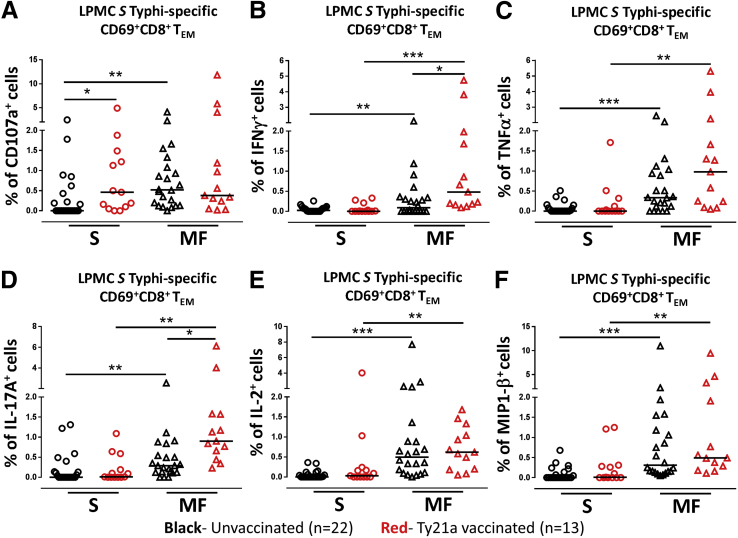
Cumulative data of S Typhi–specific responses expressed as net percentage of positive cells are shown in Figure 6A. We observed that TI-LPMC total CD8+ CD69+ T cells obtained from Ty21a-vaccinated volunteers exhibited significantly higher S Typhi–specific cytokine responses (P < .05) (INF-γ, TNF-α, and IL17A) and significantly higher expression of CD107a than LPMC total CD8+-T cells obtained from unvaccinated volunteers (Figure 6A). This is, to our knowledge, the first demonstration of local S Typhi–specific CD8+-T responses in the TI following oral Ty21a immunization.
Figure 6.
Effect of oral Ty21a immunization on terminal ileum LPMC CD8+S Typhi–specific responses in healthy adults. The net percentages of S Typhi–specific responses (IFN-γ, TNF-α, IL2, IL17A, MIP-1β, and CD107a) in (A) total CD69+CD8+ T cells and (B) CD69+CD8+ TEM cell subsets was compared between Ty21a-vaccinated (n = 13; red symbols) and unvaccinated volunteers (n = 22; black symbols) with significant differences (*P < .05) indicated. Horizontal black bars represent median values.
Terminal Ileum LPMC CD8+ TM Subsets Have Unique S Typhi–Specific Response Profiles
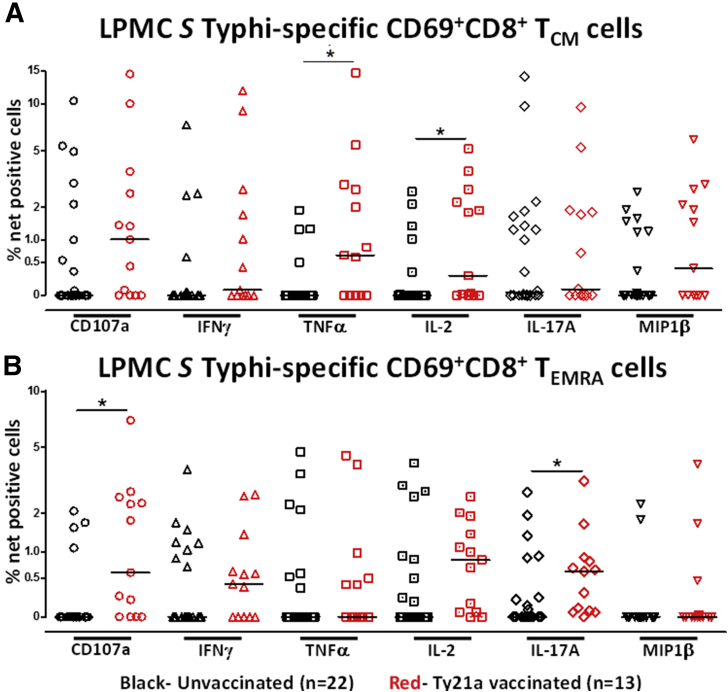
Because oral Ty21a immunization elicited S Typhi–specific responses in TI-LPMC total CD8+ T cells, we hypothesized that each CD8+-TM subsets (TEM, TCM, and TEMRA) contribute uniquely to generate discrete mucosal S Typhi–specific responses following Ty21a immunization. To test this hypothesis, we defined each CD8+-TM subset and evaluated the ability of each CD8+-TM subsets to elicit responses following stimulation with autologous S Typhi–infected and uninfected targets. Because LPMC CD8+-TEM is the predominant memory subset in the TI, representing over 55% of total CD8+-T cells, we first assessed their S Typhi–specific response profile (Figure 6B). Remarkably, LPMC CD8+ TEM showed similar signature S Typhi–specific response profile as LPMC total CD8+-T cells albeit, at lower levels (Figure 6B). Cumulative data demonstrated that LPMC CD8+-TEM producing cytokines cells (IFN-γ, TNF-α, and IL17A) and expressing CD107a frequencies were significantly higher (P < .05) in Ty21a-vaccinated than in unvaccinated volunteers (Figure 6B). We then assessed S Typhi–specific responses by TI-LPMC CD8+-TCM and -TEMRA subsets. Remarkably, we observed significant higher frequencies (P < .05) only in LPMC CD8+ TCM producing IL2 and TNF-α in Ty21a-vaccinated as compared with unvaccinated volunteers (Figure 7A). No significant differences were observed in CD8+ TCM IFN-γ-, IL17A-, and MIP-1β-producing cells and CD107a expressing cells between Ty21a-vaccinated and unvaccinated volunteers (Figure 7A). A similar assessment performed in CD8+ TEMRA revealed that this cell subset exhibited higher levels of CD107a expression and IL17A+–producing cells in LPMC from Ty21a-vaccinees than in the unvaccinated counterparts (Figure 7B). Thus, S Typhi–specific responses were observed in all major CD8+-TM subsets, although the characteristics of these responses varied among subsets.
Figure 7.
S Typhi–specific responses of terminal ileum LPMC CD8+ TCM and TEMRA subsets in healthy adults following oral Ty21a immunization. The net percentages of S Typhi–specific responses (IFN-γ, TNF-α, IL2, IL17A, MIP-1β, and CD107a) in CD69+CD8+ TCM (A) and CD69+CD8+ TEMRA (B) subsets were compared between Ty21a-vaccinated (n = 13; red symbols) and unvaccinated volunteers (n = 22; black symbols) with significant differences (*P < .05) indicated. Horizontal black bars represent median values.
Terminal Ileum LPMC CD8+ TM Subsets Responses Differ From Their Systemic Counterparts
The underlying assumption in most human studies is that there is a direct and proportional relationship between systemic and mucosal responses.28, 29, 30, 31 However, recent findings indicate that at the site of infection immune responses are distinct.24, 25, 28, 29 We therefore hypothesize that S Typhi–specific responses elicited at the TI would differ in magnitude and characteristics from their systemic counterparts following Ty21a vaccination. Because we sampled simultaneously blood and TI biopsies from each individual and used the exact stimulation protocol, it allowed us to directly address this hypothesis by comparing S Typhi–specific responses using TI-LPMC and PBMC CD8+ TM subsets. We determined the net S Typhi–specific responses (% median and range) in CD69+CD8+ (1) total, (2) TEM, (3) TCM, and (4) TEMRA obtained from TI biopsies (LPMC) or from peripheral blood (PBMC) in vaccinated and unvaccinated volunteers (Table 1). Interestingly, in unvaccinated volunteers, no significant differences were observed between LPMC and PBMC net S Typhi–specific total CD8+ responses (CD107a, IFN-γ, TNF-α, IL2, IL17A) except for higher PBMC MIP-1β responses (p<0.1) than in LPMC (Table 1; blue highlight). Similarly, no significant differences were noted in CD8+ TM subsets (TEM, TCM, TEMRA) between LPMC and PBMC except for MIP-1β which was significantly higher in PBMC than in LPMC (Temra [P < .005] and increased for TEM [P < .1]) (Table 1; blue highlights). In addition, we noted significantly higher levels of CD107a in PBMC CD8+-TEMRA and approaching significance in IFN-γ in PBMC CD8+-TEM as compared with their LPMC counterparts in unvaccinated volunteers (Table 1; blue highlights). In contrast, following Ty21a-vaccination, we observed significant increases (P < .05) in CD107a expression and IL2 production, and approaching significance (P < .1) in IL17A, INF-γ, and TNF-α production (green highlights) in LPMC net S Typhi–specific total CD8+ responses as compared with PBMC. No significant differences in total CD8+MIP-1β+ levels were noted between the 2 tissues (Table 1).
Table 1.
Comparison Between Mucosal and Systemic S Typhi–Specific CD8+ TM Subsets Responses in Unvaccinated and Ty21a-Vaccinated Volunteers
| Median % (range) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| CD107a | IFN-γ | TNF-α | IL2 | IL17A | MIP-1β | ||||
| Unvaccinated (n = 22) | CD8+ T | Total | LPMC | 0.02 (0–0.85) | 0.01 (0–0.90) | 0.01 (0–0.91) | 0.07 (0–1.14) | 0.00 (0–0.56) | 0.00 (0–0.89) |
| PBMC | 0.08 (0–1.22) | 0.00 (0–1.57) | 0.00 (0–1.21) | 0.00 (0–0.48) | 0.00 (0–0.97) | 0.01 (0–2.48)a | |||
| TEM | LPMC | 0.00 (0–0.84) | 0.00 (0–1.17) | 0.02 (0–0.82) | 0.00 (0–1.73) | 0.00 (0–0.77) | 0.00 (0–1.09) | ||
| PBMC | 0.00 (0–2.33) | 0.01 (0–1.46)a | 0.01 (0–8.53) | 0.00 (0–1.37) | 0.00 (0–4.67) | 0.07 (0–4.41)a | |||
| TCM | LPMC | 0.00 (0–2.42) | 0.00 (0–2.12) | 0.00 (0–1.06) | 0.00 (0–1.29) | 0.04 (0–2.72) | 0.00 (0–1.29) | ||
| PBMC | 0.01 (0–1.90) | 0.00 (0–4.97) | 0.00 (0–10.0) | 0.00 (0–1.71) | 0.04 (0–4.66) | 0.00 (0–6.14) | |||
| TEMRA | LPMC | 0.00 (0–1.12) | 0.00 (0–1.56) | 0.00 (0–1.75) | 0.00 (0–1.39) | 0.00 (0–1.32) | 0.00 (0–1.19) | ||
| PBMC | 0.12 (0–1.98)b | 0.01 (0–3.24) | 0.01 (0–0.76) | 0.03 (0–0.74) | 0.01 (0–1.06) | 0.04 (0–4.95)c | |||
| Ty21a vaccinated (n = 13) | CD8+ T | Total | LPMC | 0.32 (0–2.56)b | 0.21 (0–2.07)a | 0.17 (0–2.43)a | 0.30 (0–1.29)b | 0.21 (0–0.98)a | 0.10 (0–1.94) |
| PBMC | 0.00 (0–1.79) | 0.05 (0–1.21) | 0.03 (0–0.1.40) | 0.03 (0–3.95) | 0.00 (0–2.07) | 0.12 (0–2.70) | |||
| TEM | LPMC | 0.41 (0–1.75)b | 0.06 (0–0.86) | 0.25 (0–1.79)b | 0.22 (0–1.29) | 0.18 (0–1.56)a | 0.00 (0–0.95) | ||
| PBMC | 0.00 (0–2.33) | 0.04 (0–7.25) | 0.02 (0–4.32) | 0.00 (0–4.09) | 0.00 (0–10.2) | 0.50 (0–8.05)a | |||
| TCM | LPMC | 0.70 (0–2.76)a | 0.07 (0–2.54) | 0.50 (0–2.77) | 0.25 (0–1.83) | 0.08 (0–2.35)b | 0.34 (0–1.94) | ||
| PBMC | 0.00 (0–2.01) | 0.25 (0–5.29) | 0.02 (0–6.05) | 0.02 (0–5.15) | 0.02 (0–5.44) | 0.13 (0–7.41) | |||
| TEMRA | LPMC | 0.47 (0–2.08)b | 0.35 (0–1.29)a | 0.00 (0–1.61) | 0.60 (0–1.28)b | 0.48 (0–1.43)b | 0.00 (0–1.62) | ||
| PBMC | 0.02 (0–2.51) | 0.01 (0–0.72) | 0.03 (0–0.67) | 0.04 (0–3.89) | 0.02 (0–1.62) | 0.25 (0–2.10)a | |||
NOTE. Values were not significant unless where indicated.
Boldface = significant decrease in % net S Typhi–specific responses of a CD8+ TM subset in LPMC compared with PBMC; Underline = significant increase in % net S Typhi–specific responses of a CD8+ TM subset in LPMC compared with PBMC.
P < .1.
P < .05.
P < .005.
We next compared net S Typhi–specific CD8+-TM responses between LPMC and PBMC in the various TM subsets. S Typhi–specific CD8+-TEM were significantly increased in LPMC (P < .05) for CD107a expression and TNF-α production and approached significance (P < .1) for IL17A production compared with PBMC. Regarding CD8+-TCM, significantly increased IL17A production and trends to show increased expression of CD107a were observed in LPMC compared to PBMC. Finally, regarding CD8+-TEMRA significantly increased CD107 expression and IL17A and Il-2 production, and a trend to show increased production of IFN-γ were observed in LPMC as compared with PBMC following Ty21a-immunization (Table 1). Interestingly, the frequency of MIP-1β producing cells show a trend to be higher (P < .1; blue highlights) in PBMC CD8+-TEM and -TEMRA subsets as compared with their LPMC counterparts (Table 1). In sum, Ty21a-immunization elicits LPMC CD8+-TM subsets (TCM, TEM, TEMRA), which exhibit distinct properties in TI LPMC and peripheral blood.
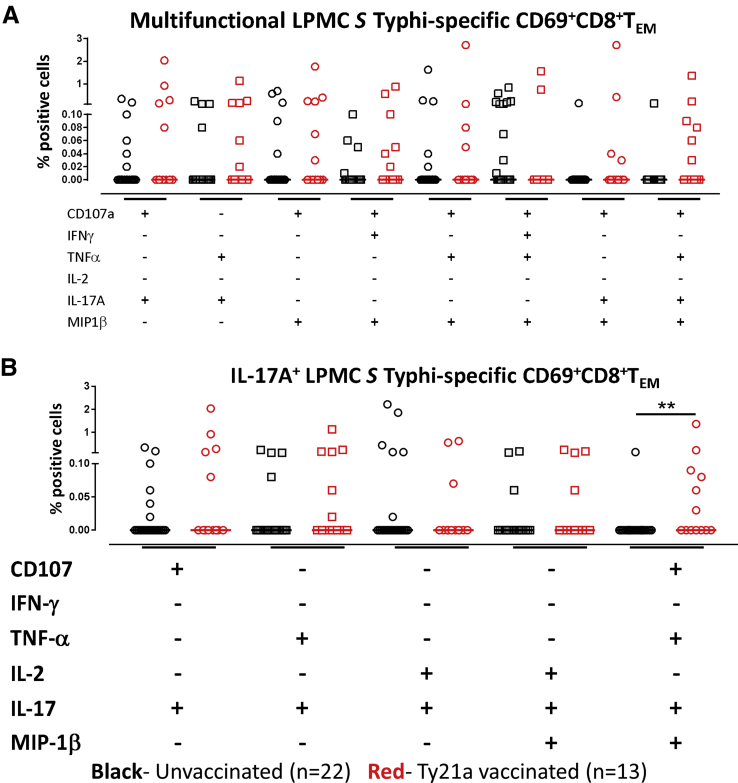
MF Terminal Ileum LPMC CD8+ TEM Responses Following Oral Ty21a Immunization
Our group has previously shown that peripheral blood CD8+ T cells respond to S Typhi by secreting multiple cytokines simultaneously.12, 23, 32 However, it is unknown whether TI S Typhi–specific CD8+ T cells responses exhibit multi-functionality. Thus, we next investigated the multifunctionality of LPMC S Typhi–specific CD8+ TEM responses in Ty21a-vaccinated and unvaccinated volunteers. Using Winlist FCOM function, TI-LPMC CD8+ TEM responses were analyzed and characterized for S Typhi–specific responding cells as either single cytokine producers/CD107a expressors (S) or MF. First we analyzed LPMC CD8+ TEM responses associated with expression of CD107a, a cytotoxic marker (Figure 8A). Interestingly, in unvaccinated volunteers, responses were mostly CD107a+ CD8+ TEM MF rather than CD107a+ CD8+ TEM S (Figure 8A). However, significantly higher frequencies of CD107a+ CD8+ TEM S cells were observed in Ty21a-vaccinees (Figure 8A). Of note, no differences were observed between the levels of CD107a+ CD8+ TEM S and MF cells in Ty21a-vaccinees.
Figure 8.
Multifunctional and single-expressing S Typhi–specific cytokine producing or CD107a expressing cells in the terminal ileum of Ty21a-vaccinated and unvaccinated volunteers. Net S Typhi–specific CD8+ TEM responses were calculated using the FCOM function of Winlist and stratified into MF and S cells. Comparison of TI LPMC S Typhi–specific CD8+ TEM (A) CD107a+, (B) INF-γ+, (C) TNF-α+, (D) IL17A+, (E) IL2+, and (F) MIP-1β+ MF and S in Ty21a-vaccinated (n = 13; red symbols) and unvaccinated volunteers (n = 22; black symbols) with significant differences shown (*P < .05; **P < .005; ***P < .0005). Horizontal black bars represent median values.
We next examined the IFN-γ responses for multifunctionality in Ty21a-vaccinees and controls. In contrast to the CD107a response, IFN-γ were largely MF as shown by significantly higher levels of IFNγ+CD8+ TEM MF in both volunteer groups compared with IFNγ+ CD8+ TEM S (Figure 8B). Following immunization, the frequencies of IFNγ+ CD8+ TEM MF cells were found to be significantly higher (P < .05) in Ty21a-vaccinated volunteers than in unvaccinated volunteers (Figure 8B). Similar observations were made for TNF-α (Figure 8C) and IL17A (Figure 8D), the other cytokines that showed to be significantly higher in Ty21a-vaccinees. No differences in S Typhi–specific responses were noted in IFN-γ+ (Figure 8B), TNF-α+ (Figure 8C), or IL17A+ (Figure 8D) CD8+ TEM S between the 2 groups of volunteers. Although IL2 and MIP-1β were not significantly higher in Ty21a-vaccinees, we noted that IL2+CD8+ TEM MF and MIP-1β+CD8+ TEM MF subsets were dominant (P < .05) (Figure 8E and F). In addition, we determined and compared the 8 dominant (out of 64 possible combinations) LPMC CD8+-TEM MF subsets elicited following Ty21a vaccination. We observed that 3 double positive subsets (eg, CD107a+ IL17A+; TNF-α+ IL17A+), 3 triple positive subsets (eg, CD107a+ IL17A+ MIP-1β+), and 2 quadruple positive subsets (eg, CD107a+ TNF-α+ IL17A+ MIP-1β+) exhibited trends to be higher in vaccinated than in the unvaccinated group (Figure 9A).
Figure 9.
S Typhi–specific multifunctional CD69+CD8+ TEM responses in the terminal ileum LPMC of Ty21a-vaccinated and unvaccinated volunteers. Shown is the concomitant induction of multiple cytokines and/or expression of CD107a in terminal ileum LPMC following stimulation with S Typhi–infected and uninfected EBV-B cells. Data were analyzed using the FCOM function of WinList. (A) The 8 dominant (out of 64 possible) combinations are represented here (doublet, triplet, and quadruple combinations). Although some trends were noted, no statistical significant differences were observed. (B) Top 5 IL17A-producing subsets (doublet, triplet, and quadruple combinations). Shown are significant differences (**P < .005) in S Typhi–specific IL17A multifunctional responses between Ty21a-vaccinated and unvaccinated in terminal ileum LPMC. Median values for each group are denoted as horizontal bars.
Furthermore, because of the importance of IL17 in mucosal immunity, we examined the top 5 individual IL17A-producing MF subsets in LPMC preparations from Ty21a-vaccinated and unvaccinated volunteers. We observed significantly higher percentages of quadruple (CD107a+TNF-α+IL17A+MIP-1β+) positive subsets in vaccinated subjects and trends to exhibit higher levels in CD107a+IL17A+ and in TNF-α+IL17A+ double positive cells (Figure 9B). Taken together, these results indicate that Ty21a immunization elicited S Typhi–specific CD8+-TEM MF responses, including IL17 producing cells, in the human TI local mucosa.
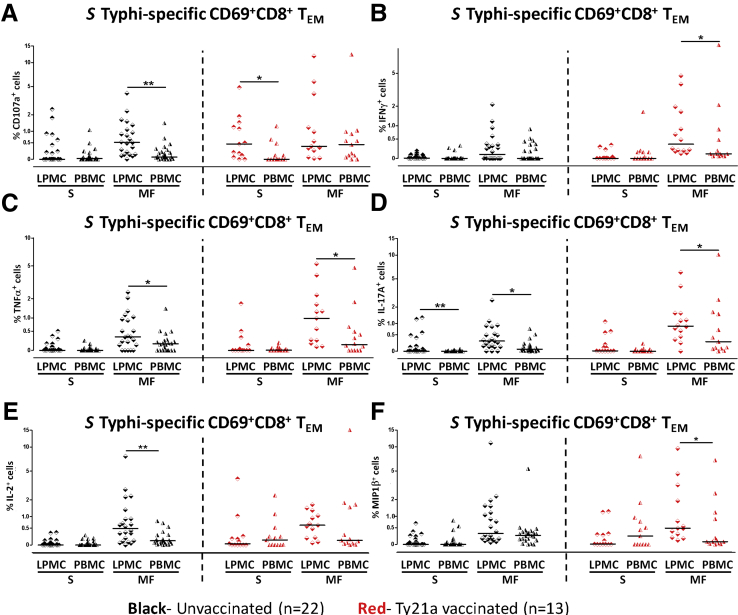
Mucosal S Typhi–Specific CD8+TEM Responses Are Different Than Their Systemic Counterparts
To further explore the relationship between mucosal and systemic S Typhi–specific responses and define potential differences in magnitude and characteristics, we analyzed CD8+-TEM by using the multifunctionality strategy described previously. We stratified net S Typhi–specific responses in MF or single (S) responses for both LPMC and PBMC in Ty21a-vaccinated and unvaccinated volunteers. Interestingly, in unvaccinated volunteers, the frequencies of CD8+ CD107a+ TEM MF were significantly higher (P < .05) in LPMC than in PBMC (Figure 10A), whereas in Ty21a-vaccinees CD8+ CD107a+ TEM MF in LPMC were not significantly different from PBMC (Figure 10A). In contrast, following Ty21a immunization, the frequencies of CD8+CD107a+ TEM S were found to be significantly higher (P < .05) in LPMC than PBMC (Figure 10A). Thus the magnitude and characteristics of CD107a-associated responses in LPMC are different than in PBMC. In contrast, the frequencies of CD8+ IFN-γ+ TEM (S or MF) were similar between TI-LPMC and PBMC obtained from unvaccinated volunteers (Figure 10B), whereas in Ty21a-vaccinated volunteers, significantly higher frequencies of CD8+ IFN-γ+ TEM MF were observed in LPMC than in PBMC (Figure 10B). In contrast, no differences were noted in CD8+ IFN-γ+ TEM S between LPMC and PBMC following Ty21a immunization (Figure 10B). Regarding TNF-α production, we observed that the frequencies of CD8+ TNF-α + TEM MF but not S were significantly higher in LPMC compared with PBMC. This was the case in both Ty21a-vaccinated and unvaccinated volunteers (Figure 10C). However, no significant differences were observed in the frequencies of CD8+ TNF-α+ TEM S between LPMC and PBMC regardless of Ty21a immunization (Figure 10C). A similar analysis for S Typhi–specific production of IL2 and MIP-1β (Figure 10E and F) revealed significantly higher frequencies of CD8+ IL2+ TEM MF in LPMC than in PBMC obtained from unvaccinated volunteers, whereas only a trend was noted in Ty21a-vaccinees (Figure 10E). No significant differences were observed in CD8+ IL2+ TEM S between LPMC and PBMC in either group of volunteers (Figure 10E). Interestingly, the frequencies of CD8+ MIP-1β+ TEM MF were significantly higher in LPMC than PBMC in only Ty21a-vaccinated volunteers (Figure 10F). Finally, of importance, we also assessed IL17A associated responses for LPMC and PBMC CD8+ TEM in both groups. In unvaccinated volunteers, we observed that both in S and MF CD8+ IL17A+ TEM frequencies were significantly higher in TI-LPMC than in PBMC (Figure 10D). However, in Ty21a-vaccinated volunteers, significantly higher frequencies of CD8+ IL17A+ TEM MF, but not S, were recorded in LPMC than in PBMC (Figure 10D). In sum, these data demonstrate that mucosal cytokine/cytotoxic effectors are different in magnitude and characteristics from their PBMC counterparts.
Figure 10.
MF- and single-expressing S Typhi–specific cytokine-producing or CD107a-expressing cells in the terminal ileum and peripheral blood in Ty21a-vaccinated and unvaccinated volunteers. Net S Typhi–specific CD8+ TEM MF and S cells responses were evaluated and compared between TI-LPMC and PBMC obtained from Ty21a-vaccinated (n = 13; red symbols) and unvaccinated volunteers (n = 22; black symbols) as shown for (A) CD107a+, (B) INF-γ+, (C) TNF-α+, (D) IL17A+, (E) IL2+, and (F) MIP-1β+ with significant differences indicated (*P < .05; **P < .005). Horizontal black bars represent median values.
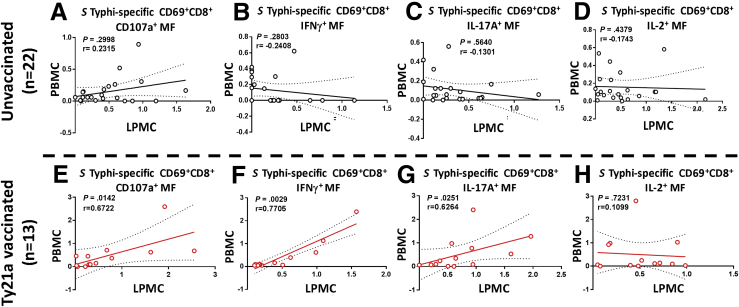
Mucosal MF S Typhi–Specific CD8+TEM Responses Correlate With Their Systemic Counterparts
We next explored the relationship between the generation of S Typhi–specific immune responses between TI-LPMC and PBMC in an individual by individual basis. We performed Spearman correlation tests on CD8+ TEM S and MF responses in both Ty21a-vaccinated and unvaccinated volunteers. We observed that in unvaccinated volunteers, the frequencies of peripheral CD8+ TEM MF (CD107a, IFN-γ, IL17A, and IL2) responses were not correlated to their LPMC counterparts (Figure 11; Table 2). However, following Ty21a vaccination, the frequencies of peripheral CD8+ TEM MF (CD107a, IFN-γ, and IL17A, but not IL2) responses were significantly correlated to their TI mucosal counterparts (Figure 11; Table 2). In addition, as shown in Table 2, only peripheral CD8+ TEM MF responses were significantly correlated to TI-LPMC CD8+ TEM MF but not CD8+ TEM S. Thus these data demonstrate that mucosal cytokines/cytotoxic MF effectors, but not single positive cells, correlate significantly to their systemic counterparts.
Figure 11.
Correlation of S Typhi–specific multifunctional CD69+CD8+-TEM responses between terminal ileum LPMC and peripheral blood (PBMC) in Ty21a-vaccinated and unvaccinated volunteers. Net S Typhi–specific CD8+-TEM responses were calculated using the FCOM function of Winlist and stratified into MF cells following stimulation with S Typhi-infected and uninfected EBV-B targets. Spearman correlation analysis was performed on (A) CD107a+ MF, (B) IFN-γ+ MF, (C) IL17A+ MF, and (D) IL2+ MF S Typhi–specific CD69+CD8+-TEM in unvaccinated volunteers (n = 22). The same correlation analysis were performed on (E) CD107a+ MF, (F) IFN-γ+ MF, (G) IL17A+ MF, and (H) IL2+ MF S Typhi–specific CD69+CD8+-TEM in Ty21a-vaccinated volunteers (n = 13). Spearman r values and P values are shown in each plot. P < .05 represent statistically significant differences.
Table 2.
Spearman Correlation Analysis of Mucosal and Systemic S Typhi–Specific CD8+ TEM Responses in Unvaccinated and Ty21a-Vaccinated Volunteers
| Terminal Ileum vs Peripheral Blood (Spearman r) |
||||
|---|---|---|---|---|
| Unvaccinated |
Ty21a vaccinated |
|||
| CD8+ TEM- S | CD8+ TEM- MF | CD8+ TEM- S | CD8+ TEM- MF | |
| CD107a | -0.151 | 0.232 | -0.281 | 0.672a |
| IFNγ | 0.060 | -0.241 | 0.432 | 0.771b |
| TNFα | -0.248 | -0.182 | -0.078 | 0.622a |
| IL-17A | 0.177 | -0.130 | -0.027 | 0.626a |
| IL-2 | -0.266 | -0.174 | 0.450 | 0.110 |
| MIP1β | 0.002 | 0.182 | -0.035 | 0.713b |
NOTE. Values were not significant unless where indicated.
P < .05.
P < .005.
Discussion
Following ingestion, some enteric pathogens (eg, S Typhi) actively invade the intestinal epithelium at the site of infection (eg, TI). Most of the knowledge of wt S Typhi infection or Ty21a immunization in human is based solely on data derived from peripheral blood. Virtually no information is available on TI immune responses. Therefore, we addressed this critical gap by characterizing in depth, for the first time, S Typhi–specific LPMC CD8+-T cell immune responses in TI following Ty21a immunization and contrasting these responses with those observed in peripheral blood.
Here, we provide direct evidence that oral Ty21a immunization elicits significant S Typhi–specific LPMC CD8+ T cell responses (IFN-γ, TNF-α, IL17A, and CD107a) in TI obtained from healthy volunteers. The TI is the preferred site of S Typhi active invasion because it contains the highest number of Peyer patches and M cells (important in S Typhi pathogenesis).3, 4, 5 Interestingly, human duodenum CD8+ T cells were recently shown to be responsive to Ty21a killed bacteria, whereas human colon T cells were unresponsive following Ty21a immunization.6 Taken together, these data indicate that human intestinal responses to oral Ty21a immunization are compartmentalized. However, differences in the magnitude and characteristics of specific responses have been noted among TI, duodenum, and colon. The magnitude of CD8+-T responses in the TI seem higher than in the duodenum and colon based on the frequencies of S Typhi–responsive CD8+ T cells from both studies. In addition, following Ty21a immunization, we show that TI-LPMC CD8+-TM responses are mostly MF, whereas the duodenum CD8+-T responses were largely attributed to single cytokine producing cells.6 Thus oral Ty21a immunization elicited local TI-LPMC CD8+-TM cells that differentiate specifically into MF Tc1 (IFN-γ and TNF-α), S and MF Tc17 (IL17A), and S and MF cytotoxic (CD107a+) CD8+T effector cells, a set of effector cells well suited for protection against intracellular pathogens. These S Typhi–responsive CD8+ T effector phenotypes are also elicited in peripheral blood but at a lower magnitude and exclusively as MF. In contrast, duodenal CD8+ T S Typhi–responsive phenotype were mostly single producing (S) Tc1 (IFN-γ, TNF-α, and IL2) CD8+ T effector cells. However, it is unclear whether these discrepancies are the result of differences in the antigens used to stimulate cells isolated from colon, duodenal, and TI biopsies. For example, it is possible that the use of Ty21a-killed bacteria, instead of S Typhi–infected autologous targets used here, favored the detection of other T-cell subsets over CD8+-T responses in the duodenum.6 In addition, other differential factors, such as microbiota composition and distribution of lymphoid structures (eg, Peyer patches, isolated lymphoid follicles, M cells; reviewed in Refs.33, 34) among colon, duodenum, and TI, might also play an important role in the differences observed between both studies.6 Moreover, the volunteers in Pennington et al6 were mostly young adults (23–24 years old), whereas the volunteers in the current studies were older adults (>49 years old). Differences in immune responses between young and older adults have been documented previously.35 Further studies are required to fully understand the factors responsible for the observed differences.
Interestingly, although LPMC CD8+-T cells displayed no significant differences in the expression of integrin α4β7, CCR9, and CCR6 homing markers, we noted that integrin α4β7+CCR9+CD8+ LPMC T cells are recruited and retained in significantly higher numbers in the TI mucosa following Ty21a vaccination. This observation argues in favor of the recruitment and retention of specific CD8+-TM at the mucosa. Remarkably, CCR9+ homing cells have been reported to play an important role in generating of antigen-specific lymphocytes in the small intestine but not in the colon.36 Our observations together with data supporting the induction of S Typhi–specific responses in the TI and duodenum but not the colon following Ty21a immunization suggest that integrin α4β7+CCR9+ cells may play a crucial role in the generation of S Typhi–specific cells in the human small intestine.
In this study we demonstrate that all major CD8+ TM subsets (TEM, TCM, and TEMRA) are elicited in the TI mucosa and display unique response profiles, but, as previously described in blood,12, 16 S Typhi–specific CD8+-TEM are the predominant phenotype. Interestingly, all major CD8+-TM subsets (TEM, TCM, and TEMRA) elicited by Ty21a immunization responded (cytotoxic CD107a expression and/or cytokines production) and were significantly higher in TI LPMC as compared with PBMC except for the chemokine MIP-1β response. Of note, the frequencies of TCM producing IL2 (required for the control of expansion of antigen-specific CD8+ T-cell populations37 and maintenance of regulatory T cells38, 39) and/or TNF-α are significantly higher following Ty21a immunization. These data suggest that local mechanisms present in the mucosa strongly activate CD8+-TM subsets following oral vaccination and/or there is an accumulation of distinct S Typhi–specific CD8+ memory and effector cells in the mucosa originating from circulation that might also change characteristics once they take residence in the mucosa.
Our results also indicate that the frequency of S Typhi–specific responsive CD8+ TEM is higher in magnitude and predominantly MF in the local intestinal mucosa, likely caused by the constant exposure to a myriad of microorganisms. However, the characteristic of these responses observed in unvaccinated versus vaccinated individuals is not the same. For example, the TI cytotoxic (CD107a+) CD8+ TEM responses are unique compared with blood with a shift from CD107a+ MF in unvaccinated to S predominant in Ty21a-vaccinated volunteers. Of note, following Ty21a immunization, the frequencies of LPMC CD8+ IL17A+ TEM MF expand significantly, whereas LPMC CD8+ TEM S producing IL17A remains constant suggesting various subsets of CD8+ TEM IL17A producing cells at the mucosa, a finding not observed in blood. Taken together, our data provide unique insights into the S Typhi–specific responses elicited in the TI mucosa and suggest that these responses are the result of local immunomodulatory mechanisms capable of influencing T cells activation, expansion, and differentiation, resulting in unique phenotypes and perhaps specificities than those in the systemic compartment. This is an important observation because most human studies relied on data obtained from peripheral blood and largely assumed that the responses obtained in the systemic compartment have a direct and proportional relationship with those present in the mucosal compartment.28
Interestingly, a positive relationship between TI mucosa and blood is noted exclusively within the CD8+ TEM MF responses (CD107a, IFN-γ, TNF-α, IL17A, and MIP1β), which showed significant correlations between the 2 compartments following Ty21a vaccination. These results suggest that CD8+ TEM MF S Typhi responsive cells may shuttle between mucosa and the periphery, and likely accumulate and/or expand locally, as evidenced by the qualitatively stronger MF responses observed in LPMC. This observation adds additional support to our recent report that S Typhi–specific CD8+ MF responses correlate with protection against typhoid and delayed disease onset in humans challenged with wt S Typhi.32 Taken together, we hypothesized that MF S Typhi–specific responses at the site of infection could be a major determinant in protection against typhoid disease. Thus, development of a highly efficacious salmonella vaccine may need to prioritize the induction of MF CD8+ TEM cells at the mucosa. These observations also provide novel insights to advance the development of oral vaccines for enteric pathogens other than S Typhi.
Conclusions
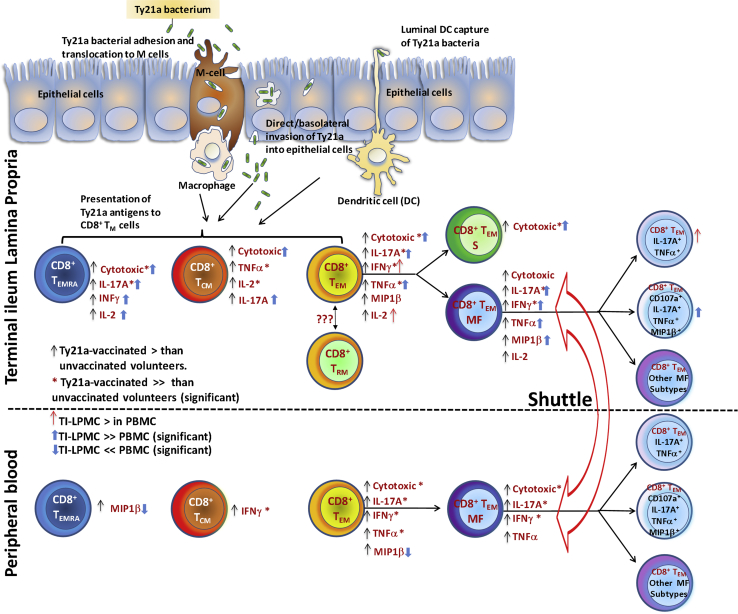
We have demonstrated that oral Ty21a immunization elicits S Typhi–specific CD8+ T-cell responses in the human TI mucosa through distinct effector functions (Figure 12). Additionally, we provided evidence that TI-LPMC CD8+-TM cell responses are unique, overlapping only partially with those observed in the systemic compartment. This study also offers new insights that are likely to contribute to the development of new or improved oral vaccines and may lead to the identification of functional correlates of protection.
Figure 12.
Drawing depicting S Typhi–specific responses elicited in the TI mucosa and peripheral blood (PBMC) following Ty21a immunization in humans. Following oral immunization with the attenuated vaccine strain Ty21a, these bacteria enter the host by various mechanisms (eg, M-cell adhesion, epithelial invasion, and dendritic cells luminal capture) and are presented by antigen-presenting cells (ie, macrophages, dendritic cells) to immune cells (ie, CD8+-TM) in the lamina propria (LP) compartment or draining mesenteric lymph nodes. CD8+-TM are subsequently activated to produce higher levels of cytokines/chemokines (IFNγ, TNFα, IL-2, IL-17A, and MIP1β) and increased cytotoxicity (upregulation of CD107a). Following Ty21a immunization each major CD8+-TM (TEM, TCM and, TEMRA) subset acquires unique characteristics in the TI LP. CD8+-TEM responses include S and MF cells. LP cytotoxic responses (CD107+) were observed both as S and MF cells, whereas the other responses were observed largely as MF cells. The relationship between mucosal and systemic immunity focused on CD8+-TEM responses are also depicted in this drawing. Following Ty21a immunization, PBMC CD8+-TEM are modulated to produce cytokines/chemokines and upregulate cytotoxic responses. However, peripheral blood CD8+-TEM responses elicited are induced mostly as MF cells rather than single producing cells. Of note, significant correlations were observed between LPMC and PBMC for all tested MF CD8+-TEM responses except for IL2. These results suggest that CD8+-TEM MF effectors elicited by immunization are the main populations with the capacity to shuttle between the TI mucosa and peripheral blood. CD8+-TEM in the terminal ileum can be composed of various subsets including tissue-resident memory T cells (TRM) and other CD8+ T cell subsets. Additionally, CD8+ TEM MF represent 64 different combinations of effector subtypes defined by the expression of CD107a, IFN-γ, IL-17A, TNF-α, IL-2, and/or MIP-1β, including doublet to sextuplet subtypes. This adds another layer of complexity in defining effector responses. This is illustrated in the figure by showing, for example, CD8+ TEM MF quadruplets (subset CD107a+, IL17A+, TNF-α+, and MIP-1β+), which exhibited significantly higher responses in terminal ileum LPMC than in PBMC following Ty21a immunization. Trends toward Ty21a vaccinees exhibiting higher responses than unvaccinated volunteers are denoted with black arrows. Significantly higher responses in Ty21a vaccinees than in unvaccinated volunteers are denoted with a red asterisk. Trends toward TI-LPMC showing higher responses than PBMC are denoted with red arrows. Significantly higher responses in TI-LPMC compared with PBMC are denoted with blue upward arrows. Significantly lower responses in TI-LPMC compared with PBMC are denoted with blue downward arrows.
Acknowledgments
The authors are indebted to the volunteers who allowed us to perform this study. They thank the staff from the Recruiting Section of Center for Vaccine Development for their help in collecting TI biopsies and blood specimens, Mr. Jeffery Floyd for isolating PBMC, and Ms. Regina Harley and Catherine Storrer for excellent technical assistance in the performance of the flow cytometric determinations.
Footnotes
Author contributions J.S.B. performed the experiments, contributed to study design, acquisition of data, and analysis and drafting of the manuscript. R.B. contributed to patient recruitment, collection of peripheral blood mononuclear cells and terminal ileum biopsies, and reviewed the manuscript. S.A.P. and L.G. performed endoscopies, obtained terminal ileum biopsies, and reviewed the manuscript. C.M.F. and A.F. participated in the design of the experiments and reviewed the manuscript. B.D.G. performed endoscopies, obtained terminal ileum biopsies, and reviewed the manuscript. M.B.S. designed the study, supervised the work, and drafted the manuscript.
Conflicts of interest The authors disclose no conflicts.
Funding This work was funded by National Institute of Allergy and Infectious Diseases, National Institutes of Health, DHHS grants R01-AI036525, U19-AI082655 (Cooperative Center for Human Immunology), and U19-AI109776 (Center of Excellence for Translational Research). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Allergy and Infectious Diseases or the National Institutes of Health.
References
- 1.Crump J.A., Mintz E.D. Global trends in typhoid and paratyphoid fever. Clin Infect Dis. 2010;50:241–246. doi: 10.1086/649541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Buckle G.C., Walker C.L., Black R.E. Typhoid fever and paratyphoid fever: systematic review to estimate global morbidity and mortality for 2010. J Glob Health. 2012;2:010401. doi: 10.7189/jogh.02.010401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parry C.M., Hien T.T., Dougan G., White N.J., Farrar J.J. Typhoid fever. N Engl J Med. 2002;347:1770–1782. doi: 10.1056/NEJMra020201. [DOI] [PubMed] [Google Scholar]
- 4.Sprinz H., Gangarosa E.J., Williams M., Hornick R.B., Woodward T.E. Histopathology of the upper small intestines in typhoid fever. Biopsy study of experimental disease in man. Am J Dig Dis. 1966;11:615–624. doi: 10.1007/BF02233509. [DOI] [PubMed] [Google Scholar]
- 5.Cornes J.S. Number, size, and distribution of Peyer's patches in the human small intestine. Part I: the development of Peyer's patches. Gut. 1965;6:225–259. doi: 10.1136/gut.6.3.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pennington S.H., Thompson A.L., Wright A.K., Ferreira D.M., Jambo K.C., Wright A.D., Faragher B., Gilmour J.W., Gordon S.B., Gordon M.A. Oral typhoid vaccination with live-attenuated Salmonella Typhi strain Ty21a generates Ty21a-responsive and heterologous influenza virus-responsive CD4+ and CD8+ T cells at the human intestinal mucosa. J Infect Dis. 2016;213:1809–1819. doi: 10.1093/infdis/jiw030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lundin B.S., Johansson C., Svennerholm A.M. Oral immunization with a Salmonella enterica serovar Typhi vaccine induces specific circulating mucosa-homing CD4(+) and CD8(+) T cells in humans. Infect Immun. 2002;70:5622–5627. doi: 10.1128/IAI.70.10.5622-5627.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levine M.M., Ferreccio C., Abrego P., Martin O.S., Ortiz E., Cryz S. Duration of efficacy of Ty21a, attenuated Salmonella typhi live oral vaccine. Vaccine. 1999;17(Suppl 2):S22–S27. doi: 10.1016/s0264-410x(99)00231-5. [DOI] [PubMed] [Google Scholar]
- 9.Sur D., Ochiai R.L., Bhattacharya S.K., Ganguly N.K., Ali M., Manna B., Dutta S., Donner A., Kanungo S., Park J.K., Puri M.K., Kim D.R., Dutta D., Bhaduri B., Acosta C.J., Clemens J.D. A cluster-randomized effectiveness trial of Vi typhoid vaccine in India. N Engl J Med. 2009;361:335–344. doi: 10.1056/NEJMoa0807521. [DOI] [PubMed] [Google Scholar]
- 10.Ferreccio C., Levine M.M., Rodriguez H., Contreras R. Comparative efficacy of two, three, or four doses of TY21a live oral typhoid vaccine in enteric-coated capsules: a field trial in an endemic area. J Infect Dis. 1989;159:766–769. doi: 10.1093/infdis/159.4.766. [DOI] [PubMed] [Google Scholar]
- 11.Guzman C.A., Borsutzky S., Griot-Wenk M., Metcalfe I.C., Pearman J., Collioud A., Favre D., Dietrich G. Vaccines against typhoid fever. Vaccine. 2006;24:3804–3811. doi: 10.1016/j.vaccine.2005.07.111. [DOI] [PubMed] [Google Scholar]
- 12.Sztein M.B., Salerno-Goncalves R., McArthur M.A. Complex adaptive immunity to enteric fevers in humans: lessons learned and the path forward. Front Immunol. 2014;5:516. doi: 10.3389/fimmu.2014.00516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Salerno-Goncalves R., Pasetti M.F., Sztein M.B. Characterization of CD8(+) effector T cell responses in volunteers immunized with Salmonella enterica serovar Typhi strain Ty21a typhoid vaccine. J Immunol. 2002;169:2196–2203. doi: 10.4049/jimmunol.169.4.2196. [DOI] [PubMed] [Google Scholar]
- 14.Salerno-Goncalves R., Fernandez-Vina M., Lewinsohn D.M., Sztein M.B. Identification of a human HLA-E-restricted CD8+ T cell subset in volunteers immunized with Salmonella enterica serovar Typhi strain Ty21a typhoid vaccine. J Immunol. 2004;173:5852–5862. doi: 10.4049/jimmunol.173.9.5852. [DOI] [PubMed] [Google Scholar]
- 15.Salerno-Goncalves R., Wahid R., Sztein M.B. Immunization of volunteers with Salmonella enterica serovar Typhi strain Ty21a elicits the oligoclonal expansion of CD8+ T cells with predominant Vbeta repertoires. Infect Immun. 2005;73:3521–3530. doi: 10.1128/IAI.73.6.3521-3530.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salerno-Goncalves R., Wahid R., Sztein M.B. Ex Vivo kinetics of early and long-term multifunctional human leukocyte antigen E-specific CD8+ cells in volunteers immunized with the Ty21a typhoid vaccine. Clin Vaccine Immunol. 2010;17:1305–1314. doi: 10.1128/CVI.00234-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kantele A. Antibody-secreting cells in the evaluation of the immunogenicity of an oral vaccine. Vaccine. 1990;8:321–326. doi: 10.1016/0264-410x(90)90088-4. [DOI] [PubMed] [Google Scholar]
- 18.McArthur M.A., Sztein M.B. Heterogeneity of multifunctional IL-17A producing S. Typhi-specific CD8+ T cells in volunteers following Ty21a typhoid immunization. PLoS One. 2012;7:e38408. doi: 10.1371/journal.pone.0038408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lindow J.C., Fimlaid K.A., Bunn J.Y., Kirkpatrick B.D. Antibodies in action: role of human opsonins in killing Salmonella enterica serovar Typhi. Infect Immun. 2011;79:3188–3194. doi: 10.1128/IAI.05081-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salerno-Goncalves R., Wyant T.L., Pasetti M.F., Fernandez-Vina M., Tacket C.O., Levine M.M., Sztein M.B. Concomitant induction of CD4+ and CD8+ T cell responses in volunteers immunized with Salmonella enterica serovar typhi strain CVD 908-htrA. J Immunol. 2003;170:2734–2741. doi: 10.4049/jimmunol.170.5.2734. [DOI] [PubMed] [Google Scholar]
- 21.Sztein M.B., Tanner M.K., Polotsky Y., Orenstein J.M., Levine M.M. Cytotoxic T lymphocytes after oral immunization with attenuated vaccine strains of Salmonella typhi in humans. J Immunol. 1995;155:3987–3993. [PubMed] [Google Scholar]
- 22.Wahid R., Fresnay S., Levine M.M., Sztein M.B. Cross-reactive multifunctional CD4+ T cell responses against Salmonella enterica serovars Typhi, Paratyphi A and Paratyphi B in humans following immunization with live oral typhoid vaccine Ty21a. Clin Immunol. 2016;173:87–95. doi: 10.1016/j.clim.2016.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wahid R., Fresnay S., Levine M.M., Sztein M.B. Immunization with Ty21a live oral typhoid vaccine elicits crossreactive multifunctional CD8+ T-cell responses against Salmonella enterica serovar Typhi, S. Paratyphi A, and S. Paratyphi B in humans. Mucosal Immunol. 2015;8:1349–1359. doi: 10.1038/mi.2015.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Booth J.S., Toapanta F.R., Salerno-Goncalves R., Patil S., Kader H.A., Safta A.M., Czinn S.J., Greenwald B.D., Sztein M.B. Characterization and functional properties of gastric tissue-resident memory T cells from children, adults, and the elderly. Front Immunol. 2014;5:294. doi: 10.3389/fimmu.2014.00294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Booth J.S., Salerno-Goncalves R., Blanchard T.G., Patil S.A., Kader H.A., Safta A.M., Morningstar L.M., Czinn S.J., Greenwald B.D., Sztein M.B. Mucosal-associated invariant T Cells in the human gastric mucosa and blood: role in Helicobacter pylori infection. Front Immunol. 2015;6:466. doi: 10.3389/fimmu.2015.00466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alter G., Malenfant J.M., Altfeld M. CD107a as a functional marker for the identification of natural killer cell activity. J Immunol Methods. 2004;294:15–22. doi: 10.1016/j.jim.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 27.Kantele A., Zivny J., Hakkinen M., Elson C.O., Mestecky J. Differential homing commitments of antigen-specific T cells after oral or parenteral immunization in humans. J Immunol. 1999;162:5173–5177. [PubMed] [Google Scholar]
- 28.Jozwik A., Habibi M.S., Paras A., Zhu J., Guvenel A., Dhariwal J., Almond M., Wong E.H., Sykes A., Maybeno M., Del Rosario J., Trujillo-Torralbo M.B., Mallia P., Sidney J., Peters B., Kon O.M., Sette A., Johnston S.L., Openshaw P.J., Chiu C. RSV-specific airway resident memory CD8+ T cells and differential disease severity after experimental human infection. Nat Commun. 2015;6:10224. doi: 10.1038/ncomms10224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang O.O., Ibarrondo F.J., Price C., Hultin L.E., Elliott J., Hultin P.M., Shih R., Hausner M.A., Ng H.L., Hoffman J., Jamieson B.D., Anton P.A. Differential blood and mucosal immune responses against an HIV-1 vaccine administered via inguinal or deltoid injection. PLoS One. 2014;9:e88621. doi: 10.1371/journal.pone.0088621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Omahony S., Arranz E., Barton J.R., Ferguson A. Dissociation between systemic and mucosal humoral immune-responses in celiac-disease. Gut. 1991;32:29–35. doi: 10.1136/gut.32.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wilkinson T.M., Li C.K., Chui C.S., Huang A.K., Perkins M., Liebner J.C., Lambkin-Williams R., Gilbert A., Oxford J., Nicholas B., Staples K.J., Dong T., Douek D.C., McMichael A.J., Xu X.N. Preexisting influenza-specific CD4+ T cells correlate with disease protection against influenza challenge in humans. Nat Med. 2012;18:274–280. doi: 10.1038/nm.2612. [DOI] [PubMed] [Google Scholar]
- 32.Fresnay S., McArthur M.A., Magder L., Darton T.C., Jones C., Waddington C.S., Blohmke C.J., Angus B., Levine M.M., Pollard A.J., Sztein M.B. Salmonella Typhi-specific multifunctional CD8+ T cells play a dominant role in protection from typhoid fever in humans. J Transl Med. 2016;14:62. doi: 10.1186/s12967-016-0819-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mowat A.M., Agace W.W. Regional specialization within the intestinal immune system. Nat Rev Immunol. 2014;14:667–685. doi: 10.1038/nri3738. [DOI] [PubMed] [Google Scholar]
- 34.Ohland C.L., Jobin C. Microbial activities and intestinal homeostasis: a delicate balance between health and disease. Cell Mol Gastroenterol Hepatol. 2015;1:28–40. doi: 10.1016/j.jcmgh.2014.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pinti M., Appay V., Campisi J., Frasca D., Fulop T., Sauce D., Larbi A., Weinberger B., Cossarizza A. Aging of the immune system: focus on inflammation and vaccination. Eur J Immunol. 2016;46:2286–2301. doi: 10.1002/eji.201546178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kunkel E.J., Campbell J.J., Haraldsen G., Pan J., Boisvert J., Roberts A.I., Ebert E.C., Vierra M.A., Goodman S.B., Genovese M.C., Wardlaw A.J., Greenberg H.B., Parker C.M., Butcher E.C., Andrew D.P., Agace W.W. Lymphocyte CC chemokine receptor 9 and epithelial thymus-expressed chemokine (TECK) expression distinguish the small intestinal immune compartment: epithelial expression of tissue-specific chemokines as an organizing principle in regional immunity. J Exp Med. 2000;192:761–768. doi: 10.1084/jem.192.5.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Boyman O., Sprent J. The role of interleukin-2 during homeostasis and activation of the immune system. Nat Rev Immunol. 2012;12:180–190. doi: 10.1038/nri3156. [DOI] [PubMed] [Google Scholar]
- 38.Geem D., Ngo V., Harusato A., Chassaing B., Gewirtz A.T., Newberry R.D., Denning T.L. Contribution of mesenteric lymph nodes and GALT to the intestinal Foxp3+ regulatory T-cell compartment. Cell Mol Gastroenterol Hepatol. 2016;2:274–280. doi: 10.1016/j.jcmgh.2015.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McArthur M.A., Fresnay S., Magder L.S., Darton T.C., Jones C., Waddington C.S., Blohmke C.J., Dougan G., Angus B., Levine M.M., Pollard A.J., Sztein M.B. Activation of Salmonella Typhi-specific regulatory T cells in typhoid disease in a wild-type S. Typhi challenge model. PLoS Pathog. 2015;11:e1004914. doi: 10.1371/journal.ppat.1004914. [DOI] [PMC free article] [PubMed] [Google Scholar]