Abstract.
Septo-optic dysplasia (SOD) is a congenital anomaly in which agenesis of the septum pellucidum and optic nerve hypoplasia are accompanied by hypopituitarism. Typically, the symptoms develop in 3 organs, the brain, eyes, and pituitary, and approximately one third of the patients present with all of the three cardinal features. The diagnostic criteria for SOD were established in Japan in 2015. The purpose of this study is to review clinical features regarding SOD patients with hypopituitarism in Japan. In this study, 21 patients with SOD were identified by a questionnaire survey for congenital central hypothyroidism. All 3 symptoms of SOD, agenesis of the septum pellucidum, optic nerve hypoplasia, and endocrine abnormalities, were noted in 8 of the 21 patients. Various combinations of pituitary hormone deficiencies were observed in patients with SOD, although SOD is a rare, heterogeneous, and phenotypically variable disorder, some patients develop hypoglycemia and convulsions after birth, and early intervention with hormone replacement is necessary in severe cases. In addition, 14 cases were complicated by both developmental delay and epilepsy, and 16 cases involved eye abnormalities. Therefore, in addition to an early endocrinological diagnosis and hormone replacement, consultation with both pediatric neurologists and pediatric ophthalmologists is necessary.
Keywords: septo-optic dysplasia, combined pituitary hormone deficiency, optic nerve hypoplasia, agenesis of the septum pellucidum, congenital central hypothyroidism
Introduction
Septo-optic dysplasia (SOD) is a congenital anomaly in which agenesis of the septum pellucidum and optic nerve hypoplasia are accompanied by hypopituitarism. According to a survey conducted in England, the annual incidence of SOD was estimated to be 1 in 10,000 births or lower, and the male : female ratio was 1:1 (1–3), however the frequency of occurrence in Japan is not known. The etiology of SOD is unclear in several cases, although an association with childbearing at a young age and drug addiction of pregnant women has been suggested. Although the largely sporadic occurrence of SOD remains unexplained, viral infections and other environmental causes have been implicated (1). Gene mutations associated with SOD, in transcriptional factors involved in the development of the pituitary, such as HESX1, SOX2, and OTX2 have been identified, although such mutations are very rare (1,2,3).
Typically, patients with SOD develop symptoms in 3 organs, the brain, eyes, and pituitary, and approximately one third of the patients present with all the three cardinal features of the disease. The disease is difficult to manage owing to visual disturbances, epileptic seizures, and cerebral palsy; the intellectual disturbances vary from normal to severe (1,2,3,4). Dysfunction of both, the anterior and posterior pituitary hormones, occurs but the severity and combinations of deficiency of the hormones vary among the patients (1,2,3). Early diagnosis of TSH, GH, ACTH, and AVP deficiencies and early treatment with hormone replacement therapy are very important (1, 2, 5)
A nationwide questionnaire survey was carried out among the councilors of the Japanese Society for Pediatric Endocrinology to investigate the current state of treatment for congenital central hypothyroidism (CCH) throughout Japan. A total of 21 patients with SOD were identified. We report here on the endocrine characteristics, neurologic manifestations, eye symptoms, and MRI findings of the brain and pituitary of these patients with SOD. The purpose of this study is to review clinical features regarding SOD patients with hypopituitarism in Japan.
Methods
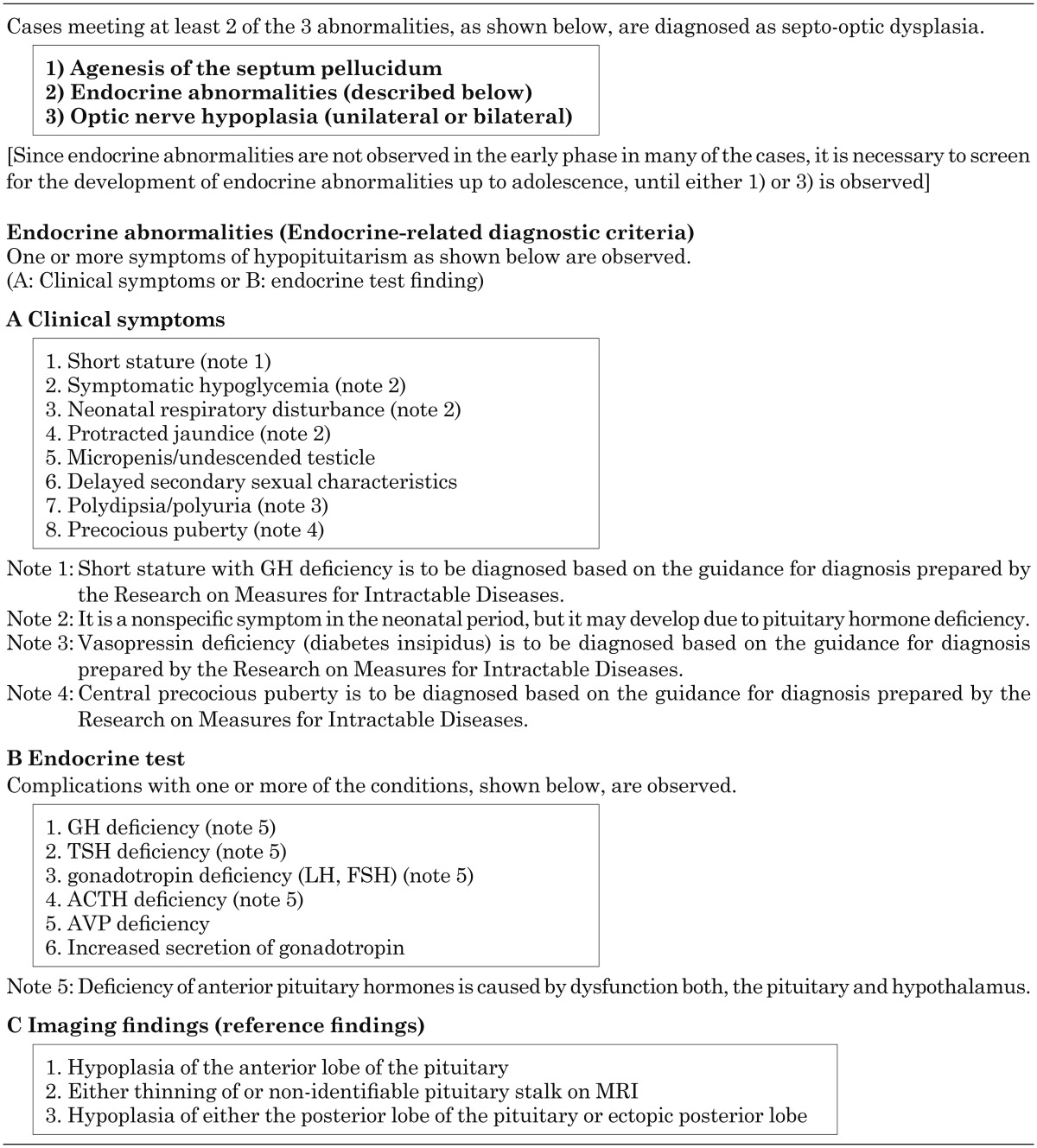
SOD was diagnosed according to the guidelines of the Japan Intractable Diseases Information Center septo-optic dysplasia/De Morsier syndrome (specified intractable disease 134) (6) (Table 1). The subjects were patients who were diagnosed with CCH between April 2004 and March 2014. An epidemiological survey was conducted among pediatric endocrinologists (councilors of the Japanese Society for Pediatric Endocrinology) throughout Japan who were likely to be involved in the management of patients with CCH. As a primary survey, 191 councilors of the Japanese Society for Pediatric Endocrinology were queried about whether they were treating patients with CCH, including suspected cases, between December 2014 and January 2015. The request for this information was made through an e-mail in association with the Society (primary survey). The secondary survey form was sent to the institutions identified in the primary survey that reported to treating the particular patients, and clinical information was collected (July 2015–March 2016). The details of the methods and subjects were previously reported (7).
Table 1. Diagnostic criteria of septo-optic dysplasia.
This survey was performed after approval by the Ethics Committee of Niigata University School of Medicine, and an outline of the study was published on the homepage (http://jspe.umin.jp/medical/research/CongenitalCH/index.html).
Results
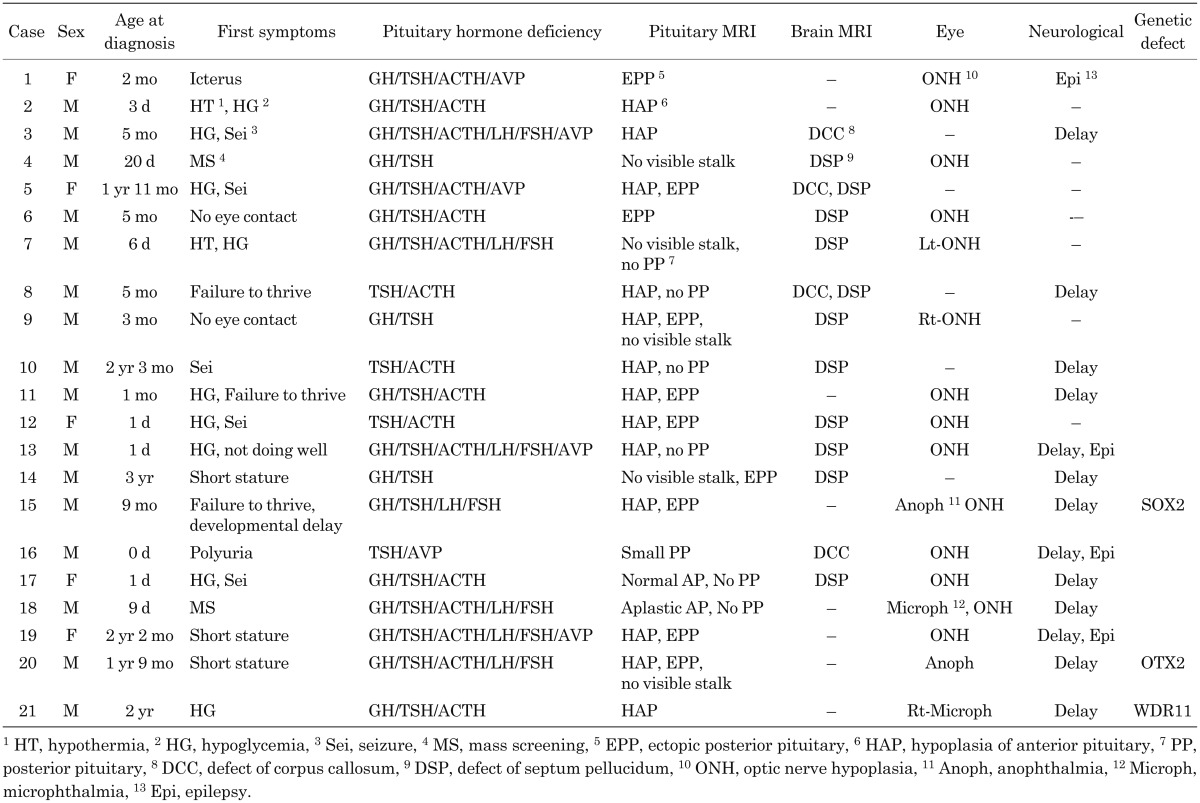
The age, specific findings leading to the SOD diagnosis, endocrine-related findings, MRIs findings of the pituitary and brain, ophthalmologic findings, neurologic manifestations, and genetic abnormalities of the study subjects are summarized in Table 2.
Table 2. Characteristics of patients with SOD.
Of the 21 patients with SOD (16 men and 5 women), 8 met the diagnostic criteria with respect to the three main symptoms: agenesis of the septum pellucidum, eye abnormalities, and endocrine disorders, 9 patients developed endocrine and eye abnormalities, and 4 patients developed endocrine disorder and agenesis of the septum pellucidum.
The age at the time of diagnosis ranged from after birth to 2 yr and 3 mo. The findings that led to the diagnosis were neonatal hypoglycemia, convulsions, protracted jaundice, polyuria immediately after birth, and growth disturbances. The disease was diagnosed upon finding the absence of pursuit eye movements in 2 patients. The disease was identified on neonatal mass screening to detect CCH, by measuring free thyroxine (FT4), in 2 patients. The thyroid function tests at initial diagnosis were FT4 0.66 ng/dl / TSH 4.8 µU/ml at the age of 20 d and FT4 0.11 ng/dl / TSH 1.2 µU/ml at the age of 9 d. Both of them are before attendance at school, and the degree of the development is unknown.
As the survey was focus on CCH, TSH deficiency was observed in all the patients. Other than TSH, the anterior pituitary function was evaluated in 20 patients, and GH, ACTH, LH/FSH, and AVP deficiencies were noted in 17, 16, 7, and 6 patients, respectively. Dysplasia of the pituitary was noted in 20 of the 21 patients. In Case 17, the anterior lobe of the pituitary was normal, but the posterior lobe could not be identified on MRI. In Case 16, TSH deficiency and diabetes insipidus were observed, and the anterior lobe of the pituitary was normal, but the posterior lobe was hypoplastic.
Developmental delay and epilepsy were observed in 15 and 4 patients, respectively. Eye symptoms were noted in 16 patients. Unilateral optic nerve hypoplasia and microphthalmia were observed in 3 patients. Anophthalmia was noted in 2 patients.
Mutations were identified in SOX2 and OTX2 genes in the patients with anophthalmia, and a WDR11 gene abnormality was identified in a patient with right microphthalmia.
Discussion
The endocrine-related characteristics of SOD were identified, and it was found that specific hormone deficiencies varied among the cases. Symptoms developed within one week after birth in 6 of the 21 patients, and diabetes insipidus was found in 1 of these patients. The symptoms were hypoglycemia and hypothermia in the other 5 patients, and GH and ACTH deficiencies were present in addition to TSH deficiency. These are serious complications of congenital hypopituitarism (5, 8) that correlate with the findings that some cases of SOD develop severe hypopituitarism early after birth. Hormone replacement to treat hormone deficiencies is very important to improve the morbidity of patients with SOD, for which early endocrinological diagnosis is important.
The etiology of SOD is unclear, as described above, and reportedly, genetic and environmental factors are involved (1,2,3). SOD may be diagnosed when at least 2 of the 3 main symptoms are observed. Accordingly, very heterogeneous diseases may be included in SOD, and the causes are also diverse; HESX1, SOX2, SOX3, and OTX2 gene aberrations have been reported (1, 9,10,11), although these genetic abnormalities are rare, and development of SOD due to a KAL1 gene aberration in Kallmann syndrome has recently been reported (12). In the present survey, a SOX2 gene deletion and an OTX2 gene mutation were present in the patients with anophthalmia. A SOX2 gene aberration was initially reported as a cause of anophthalmia and microphthalmia, but it was subsequently found to induce a wide range of symptoms, such as hypogonadotropic hypogonadism, pituitary hypoplasia, combined pituitary hormone deficiency (CPHD), morphological abnormality of the hippocampus, agenesis of the septum pellucidum, and sensorineural deafness (1, 10). An OTX2 gene aberration also manifests as anophthalmia and microphthalmia, but development of pituitary hypoplasia and CPHD have also been reported, which may cause SOD (1, 5, 11). In addition, a WDR11 mutation was identified in 1 patient with microphthalmia. A WDR11 aberration, particularly 4 missense mutations, has been identified as a cause of hypogonadotropic hypogonadism, similar to a SOX2 aberration (13). At present, the association of these mutations with CPHD, pituitary formation, eye development, and the optic nerve is unclear.
There are several limitations of this study. Since the focus was on SOD in the survey of endocrine-related symptoms, particularly CCH, the endocrine-related pathology of patients without TSH deficiency was unclear. Moreover, the pathology of patients with agenesis of the septum pellucidum and eye symptoms without endocrine-related symptoms was unclear. The clinical characteristics of SOD patients will be further clarified with the registration of intractable disease patients with SOD in the future. Although there are several limitations, the present study helps to understand the endocrine-related characteristics and severity of the disease based on the analysis of a reasonable number (21) of SOD cases.
Conclusions
Various combinations of pituitary hormone deficiencies occur in patients with SOD.
Although SOD is a rare, heterogeneous and phenotypically variable disorder, some patients develop hypoglycemia and convulsions after birth, and early intervention with hormone replacement is necessary for the severe cases.
Since the disease is accompanied by serious neurologic manifestations and eye abnormalities, communication with pediatric neurologists and pediatric ophthalmologists is necessary.
Conflicts of interest: The authors declare no conflict of interest.
Acknowledgments
We are grateful to Dr. Mitsuhiro Kato, Department of Pediatrics Showa University School of Medicine, Dr. Miho Sato, Department of Ophthalmology Hamamatsu University School of Medicine, and Dr. Takashi Kawamura, Kyoto University Health Service, the representatives of Study Group for survey of the actual state of septo-optic dysplasia and preparation of diagnostic criteria·severity classification in Research project for Intractable Disease Measures, for giving us valuable advice related to this study.
This study was partially supported by the Health and Labour Sciences Research Grants, Research on Intractable Diseases, Research Committee on Septo-Optic Dysplasia of the Ministry of Health, Labour, and Welfare, Japan (H27-7).
References
- 1.McCabe MJ, Alatzoglou KS, Dattani MT. Septo-optic dysplasia and other midline defects: the role of transcription factors: HESX1 and beyond. Best Pract Res Clin Endocrinol Metab 2011;25: 115–24. doi: 10.1016/j.beem.2010.06.008 [DOI] [PubMed] [Google Scholar]
- 2.Cemeroglu AP, Coulas T, Kleis L. Spectrum of clinical presentations and endocrinological findings of patients with septo-optic dysplasia: a retrospective study. J Pediatr Endocrinol Metab 2015;28: 1057–63. doi: 10.1515/jpem-2015-0008 [DOI] [PubMed] [Google Scholar]
- 3.Ryabets-Lienhard A, Stewart C, Borchert M, Geffner ME. The optic nerve hypoplasia spectrum: review of the literature and clinical guidelines. Adv Pediatr 2016;63: 127–46. doi: 10.1016/j.yapd.2016.04.009 [DOI] [PubMed] [Google Scholar]
- 4.Signorini SG, Decio A, Fedeli C, Luparia A, Antonini M, Bertone C, et al. Septo-optic dysplasia in childhood: the neurological, cognitive and neuro-ophthalmological perspective. Dev Med Child Neurol 2012;54: 1018–24. doi: 10.1111/j.1469-8749.2012.04404.x [DOI] [PubMed] [Google Scholar]
- 5.Tajima T, Ishizu K, Nakamura A. Molecular and clinical findings in patients with LHX4 and OTX2 mutations. Clin Pediatr Endocrinol 2013;22: 15–23. doi: 10.1297/cpe.22.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.http://www.nanbyou.or.jp/entry/4403 diagnostic criteria (In Japanese).
- 7.Nagasaki K, Kubota T, Kobayashi H, Sawada H, Numakura C, Harada S, et al. National survey for congenital central hypothyroidism in Japan. Jpn J Mass Screening 2017;27: 9–14(in Japanese). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Takanashi K, Suzuki Y, Noro A, Sugiyama M, Nakanishi M, Nagashima T, et al. Three Japanese patients with congenital pituitary hormone deficiency and ophthalmological anomalies. Pediatr Rep 2011;3: e20. doi: 10.4081/pr.2011.e20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tajima T, Hattorri T, Nakajima T, Okuhara K, Sato K, Abe S, et al. Sporadic heterozygous frameshift mutation of HESX1 causing pituitary and optic nerve hypoplasia and combined pituitary hormone deficiency in a Japanese patient. J Clin Endocrinol Metab 2003;88: 45–50. doi: 10.1210/jc.2002-020818 [DOI] [PubMed] [Google Scholar]
- 10.Kelberman D, Rizzoti K, Avilion A, Bitner-Glindzicz M, Cianfarani S, Collins J, et al. Mutations within Sox2/SOX2 are associated with abnormalities in the hypothalamo-pituitary-gonadal axis in mice and humans. J Clin Invest 2006;116: 2442–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tajima T, Ohtake A, Hoshino M, Amemiya S, Sasaki N, Ishizu K, et al. OTX2 loss of function mutation causes anophthalmia and combined pituitary hormone deficiency with a small anterior and ectopic posterior pituitary. J Clin Endocrinol Metab 2009;94: 314–9. doi: 10.1210/jc.2008-1219 [DOI] [PubMed] [Google Scholar]
- 12.McCabe MJ, Hu Y, Gregory LC, Gaston-Massuet C, Alatzoglou KS, Saldanha JW, et al. Novel application of luciferase assay for the in vitro functional assessment of KAL1 variants in three females with septo-optic dysplasia (SOD). Mol Cell Endocrinol 2015;417: 63–72. doi: 10.1016/j.mce.2015.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim HG, Ahn JW, Kurth I, Ullmann R, Kim HT, Kulharya A, et al. WDR11, a WD protein that interacts with transcription factor EMX1, is mutated in idiopathic hypogonadotropic hypogonadism and Kallmann syndrome. Am J Hum Genet 2010;87: 465–79. doi: 10.1016/j.ajhg.2010.08.018 [DOI] [PMC free article] [PubMed] [Google Scholar]