Summary
The World Health Organization has defined ‘elderly’ as 65 years or older. Age is a known major prognostic factor after burn injury. The objective of this study is to establish whether epidemiologic differences in the elderly contribute to higher mortality compared to younger patients. Patients admitted to the burn unit between 2011 and 2014 (229 patients) were included: 159 were under 65 years old and 70 (30.6%) were 65 or over. The elderly group had a higher mortality rate, 24.6% versus 8.2% (p=0.002). Patients over 65 presented more pre-existing co-morbidities (1.7 ± 1.1) than patients under 65 (1.1 ± 1.0), p<0.001, and COPD was significantly associated with higher mortality rate (p=0.014). Patients over and under 65 suffered similar TBSA, 15.7 versus 14.1, p=0.720. Regarding burn depth, deeper burns were significantly more prevalent in the over 65 group (17.1% vs. 5.0%, p=0.003). Patients over 65 developed more complications (0.9 ± 1.1) than the under 65s (0.5 ± 0.9), p=0.009, and sepsis was significantly associated with higher mortality rate (p=0.042). Over-65-year-old burn victims have a higher mortality risk than the under 65s. Elderly patients generally have more pre-existing comorbidities and develop more complications during hospital stay, which increase the mortality risk. Apparently, history of COPD or sepsis complication during hospital stay are independent risk factors for death in the elderly group. Although over-65-year-olds presented similar TBSA to the younger patients, the proportion of deep burns was higher, which suggests that burns might be more aggressive in the elderly
Keywords: burns, aged, complications, comorbidity
Abstract
L’OMS a défini la vieillesse comme l’âge supérieur ou égal à 65 ans. L’âge est un facteur pronostic majeur reconnu chez les brûlés. Le but de cette étude est d’évaluer si des variables épidémiologiques contribuent à la plus grande mortalité des sujets âgés (SA). Les patients (229) admis dans l’unité entre 2011 et 2014 ont été inclus. Cent cinquante neuf avaient moins de 66 ans, 70 (30,6%) 65 ans ou plus. La mortalité des SA était significativement plus élévée (24,6 VS 8,2%, p = 0,002). Les SA avaient plus de comorbités que les plus jeunes (1,7 ± 1,1 VS 1,1 ± 1; p< 0,001) et les BPCO étaient sigificativement à risque de surmortalité (p = 0,014). La surface brûlée des SA (15,7%) était comparable à celle des sujets plus jeunes (14,1%; p = 0,72). Les brûlures étaient plus fréquemment profondes chez les SA (17,1 VS 5%, p = 0,003). Les SA ont eu plus de complications que les plus jeunes (0,9 ± 1,1 VS 0,5 ± 0,9; p = 0,009) et le sepsis est associé à une surmortalité (p = 0,04). Les SA brûlés ont plus de comorbités, développent plus de complications et meurent plus que les sujets plus jeunes. Il semble que l’existence d’une BPCO et la survenue d’un sepsis soient des facteurs indépendants de risque de mortalité chez le sujet âgé. Bien que les surfaces brûlées soient comprables, la proportion de brûlures profondes est plus importante chez les SA, rendant les brûlures du SA plus graves.
Introduction
The World Health Organization (WHO) and the National Institutes of Health (NIH) have defined ‘elderly’ as 65 years or older.1 The proportion of elderly people has been rising in developed countries. Accordingly, in Portugal, the elderly population increased from 8.0% in 1960 to more than double (16.4%) in 2001 and to 19% in 2011.2 An increasingly ageing population will have considerable repercussions on health care systems, including burn care provision.3
The literature demonstrates that age is a major prognostic factor after burn injury. The best outcomes are found in children, followed by adults and, lastly, the elderly.3,4 The elderly are particularly susceptible to trauma and burn injuries due to impairments in judgement, coordination, balance and reaction times together with reduced ability to escape from harm.5 In general, they have thinning skin,6 impaired sensation, decreased metabolic reserves,7 mental alterations and pre-existing medical conditions,8-10 which together with immune response impairment11 contribute to worsened outcomes after burn injuries. Moreover, during hospital stay, elderly patients who survive a burn injury have significantly increased morbidity, particularly from infectious complications.12 They are more prone to longer hospital stays and to needing post-hospitalization resources.13,14
The primary objective of this study is to establish whether epidemiologic differences in elderly burned patients may contribute to higher mortality compared to younger patients. The secondary objective is to analyse whether number or type of comorbidities and complications in this population influence mortality.
Material and methods
Study design and patient selection
A retrospective, single-centre trial at the burn unit of Prelada Hospital was conducted. Patients admitted to the burn unit between January 2011 and December 2014 were included: those who were hospitalized for less than 24 hours were excluded. The following data were retrieved from patient files: demographic data, co-morbidities, characteristics of the injury scene, aetiology and characteristics of the burn, major complications, length of hospitalization and mortality.
Statistics and data analysis
Data were analysed using Microsoft Excel and IBM SPSS 22 software. Descriptive analysis was presented with absolute frequency (n) and percentage (%) or mean (χ) ± standard deviation (σ) and median (m). A multivariate analysis was performed to evaluate how the variables related to mortality. A value of p < 0,05 was considered statistically significant.
Results
During the 48-month study period, 233 patients were admitted to our burn unit. However, 4 patients who were hospitalized for less than 24 hours were excluded. A total of 229 patients were included in the study: 159 were under 65 years old and 70 were 65 or over, elderly people accounting for 30.6% of the patient population.
In the under 65 group 73% of the patients were male. In the over 65 group, the gender proportion was more balanced, with 47% male. This difference was statistically significant (p<0.001).
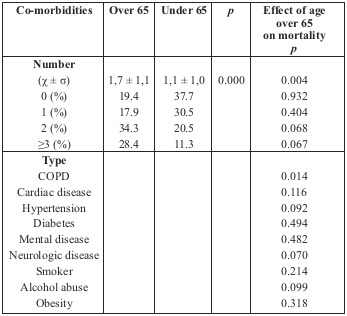
As shown in Table I, patients over 65 presented more preexisting co-morbidities (1.7 ± 1.1) than patients under 65 (1.1 ± 1.0), p<0.001. In addition, patients who died had a mean of 1.8 co-morbidities and those who survived had 1.2 co-morbidities, p=0.004. Regarding patients previously diagnosed with Chronic Obstructive Pulmonary Disease (COPD), being older than 65 significantly increases mortality (p=0.014). However, for patients with a history of cardiac disease, hypertension, diabetes, mental or neurologic disease, tobacco or alcohol abuse and obesity, being over 65 does not influence the risk of mortality (p > 0.05). There were not enough patients with a past history of asthma, drug addiction or immunodeficiency diseases to perform statistical tests.
Table I.
In the elderly group, 95.8% of admissions were due to home incidents. In the younger group the proportion was more distributed, with 51% of injuries occurring in the home and 40% in the workplace. For the elderly group, most accidents occurred in a closed space (78.4%), while in the younger group, accidents equally occurred in a closed or open space (50%), p=0.001.
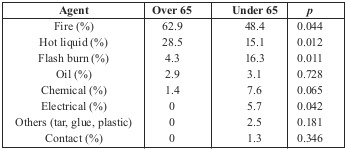
The leading causes of burn in the over 65 group were fire (62.9%) and scalding (22.5%). In the under 65 group, the proportion of each cause was more diluted. Therefore, fire (62.9 vs. 48.4%, p=0.004) and scalding (22.5% vs. 15.1%, p=0.012) were significantly less frequent causes in the younger burn patients (Table II).
Table II.
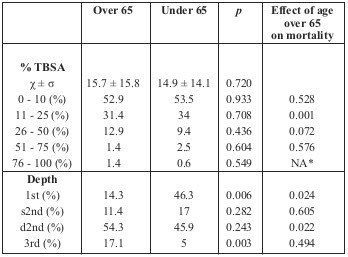
According to Table III, patients over and under 65 suffered similar TBSA, 15.7 versus 14.1, p=0.720. When TBSA is rearranged into categories, it turns out that age over 65 significantly increases mortality only for patients with 11-25% TBSA burns. Regarding burn depth, deeper burns are significantly more prevalent in the over 65 group (17.1% vs. 5.0%, p=0.003) and more superficial burns are significantly more prevalent in the under 65 group (14.3 vs. 46.3, p=0.006). Additionally, being older increases the risk of mortality only for patients with predominantly 1st or deep 2nd degree burns.
Table III.
Face burn, inhalation injury and endotracheal intubation (ETI) were more prevalent in younger patients. However, among patients with face burns and those who underwent ETI, age over 65 significantly increased the mortality risk (respectively, p=0.001 and p=0.013). For patients with inhalation injury, being older than 65 did not influence mortality rate (p=0.052).
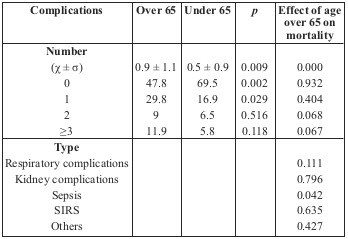
As shown in Table IV, patients over 65 generally developed more complications (0.9 ± 1.1) than patients under 65 (0.5 ± 0.9), p=0.009. In addition, patients who died had developed a mean of 2.2 complications and those who survived 0.3 complications, p<0.001. Regarding patients who developed sepsis during hospital stay, being older than 65 significantly increases mortality risk (p=0.042). However, age over 65 does not influence the risk of mortality in patients with other complications (p > 0.05).
Table IV.
The number of surgical operations performed to recover the cutaneous barrier was higher in the older group, 2.1 vs. 1.3 (p = 0.002).
The elderly group had a higher mortality rate, 24.6% vs. 8.2% (p=0.002) and longer hospital stays, 35.1 vs. 23.1 (p<0.001).
Discussion
The 65 years and older age group represents the fastest growing segment of populations in Europe and the USA.15 Since this demographic group remains vulnerable to trauma injuries including burns,5,16 a growing number of elderly patients are being admitted to burn units. In our sample, 30.6% of admissions belonged to the elderly population, which is in accordance with recent studies from other countries.6
A higher mortality rate among elderly burn victims compared to younger people was detected in this study, but this is not a novel issue.6,17-20 The literature reports that mortality among elderly burn patients ranges from 7.4 to 66%, averaging around 30% in most of them.17,19,20-22 Consistent with these reports, the mortality rate in our elderly group was 24.6%.
Our analysis detected a significant relation between age over 65 and the presence of more co-morbidities, and between mortality and the presence of more co-morbidities. However, among patients with the same number of co-morbidities, age over 65 did not significantly increase mortality rate. Therefore, age increases mortality, apparently indirectly due to its association with a higher number of comorbidities. Analysing the impact of each comorbidity, only COPD appears to increase the risk of mortality in the elderly group, which also supports the previous conclusion.
The majority of the patients got burned at home (95.8%), in a closed space (78.4%) with fire (62.9%) or hot liquids (28.5%), concordant with the literature.19,20,22 Elderly people who suffer burn injuries usually live alone and have an impaired social support network.21 Improving education, establishing prevention measures and reinforcing social support networks might be important in reducing the occurrence of these incidents.
Several studies have reported that elderly patients with a similar TBSA are more likely to die than younger patients.23 However, in our results age over 65 significantly increased mortality only for patients with 11-25% TBSA. Therefore, only for burns of intermediate extension might age be a prognostic factor. For less extensive burns, mortality is very low even in the elderly group. For more extensive burns, mortality should rely on other factors than just age.
Even though patients aged over 65 got burned with similar TBSA compared to younger patients, the proportion of deep burns was higher, which suggests that burns might be more aggressive in the elderly. This relationship has already been suggested in previous studies.6
In our sample, among patients with face burns and those who underwent ETI, age over 65 significantly increased mortality risk. According to previous studies, face burns are positively associated with early ETI, presence of inhalation injury and higher TBSAs, which appear to increase respiratory complications and mortality. Inhalation injury and TBSA are independent variables. Therefore, intubation is the remaining risk factor that, being a dependent variable, can be controlled by health care providers. Early intubation, before the patient enters the burn unit, might be life saving. However, unnecessary intubation, particularly in elderly patients, may increase morbidity and mortality.24
Our study detected a significant relationship between age over 65 and the development of more complications, and between more complications and mortality. However, among patients with the same number of complications, age over 65 did not significantly increase mortality rate. Therefore, age is associated with a higher mortality rate, apparently indirectly due to its association with the development of more complications. Analysing the impact of each complication, only sepsis appears to increase the risk of mortality in the elderly group, which also supports the previous conclusion.
In the literature, mean surgical procedures performed to recover the cutaneous barrier in elderly burned patients ranged from 1.6 to 4.1. 6,17,22,23 Accordingly, in our report, patients over 65 years underwent an average of 2.1 operations.
In the last few decades, significant advances have been made regarding the outcome of burned patients, in every age category, but improvements in the elderly were subtler.3,4 Furthermore, the elderly population requires more rehabilitation and social support to achieve an acceptable reintegration. With an increasingly ageing population, this is a concern to take into account in health systems and in the development of prevention policies and social support measures.
Conclusion
Burn victims aged over 65 years have a higher mortality risk than those under 65 years old. Elderly patients generally have more pre-existing comorbidities and develop more complications during hospital stay, which increase mortality risk. Apparently, history of COPD or sepsis complication during hospital stay are independent risk factors for death in the elderly group.
Even though patients over 65 presented similar TBSA to younger patients, the proportion of deep burns was higher, which suggests that burns might be more aggressive in the elderly.
Patients over 65 are intubated less frequently than the younger ones. However, when intubated they have a significantly higher risk of morbidity and mortality. Therefore, the decision to intubate a patient, especially an older patient, should be given careful consideration.
The majority of these patients got burned at home, in a closed space. In fact, elderly burn victims usually live alone and have an impaired social support network, which should alert the community and the authorities to reinforcing the social support network for the elderly.
References
- 1. www.who.int/ healthinfo/survey/ageingdefnolder/en/ [Google Scholar]
- 2. http://censos.ine.pt/ [Google Scholar]
- 3.Wearn C. Outcomes of burns in the elderly: revised estimates from the Birmingham Burn Centre. Burns. 2015;41(6):1161–1168. doi: 10.1016/j.burns.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 4.Pereira CT. Age-dependent differences in survival after severe burns: a unicentric review of 1,674 patients and 179 autopsies over 15 years. J Am Coll Surg. 2006;202(3):536–548. doi: 10.1016/j.jamcollsurg.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Peck MD. Epidemiology of burns throughout the world. Part I: Distribution and risk factors. Burns. 2011;37:1087–1100. doi: 10.1016/j.burns.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 6.Albornoz CR. Burns are more aggressive in the elderly: proportion of deep burn area/total burn area might have a role in mortality. Burns. 2011;37(6):1058–1061. doi: 10.1016/j.burns.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 7.Grimble RF. Inflammatory response in the elderly. Curr Opin Clin Nutr Metab Care. 2003;6(1):21–29. doi: 10.1097/00075197-200301000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Gerstein AD, Phillips TJ, Rogers GS, Gilchrest BA. Wound healing and aging. Dermatol Clin. 1993;11(4):749–757. [PubMed] [Google Scholar]
- 9.Lundgren RS. Influence of comorbidities and age on outcome following burn injury in older adults. J Burn Care Res. 2009;30(2):307–314. doi: 10.1097/BCR.0b013e318198a416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pham TN. Epidemiology and outcomes of older adults with burn injury: an analysis of the National Burn Repository. J Burn Care Res. 2009;30(1):30–36. doi: 10.1097/BCR.0b013e3181921efc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rani M, Schwacha MG. Aging and the pathogenic response to burn. Aging Dis. 2012;3(2):171–180. [PMC free article] [PubMed] [Google Scholar]
- 12.Pham TN. Risk factors for the development of pneumonia in older adults with burn injury. J Burn Care Res. 2010;31:105–110. doi: 10.1097/BCR.0b013e3181cb8c5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pham TN. Epidemiology and outcomes of older adults with burn injury: an analysis of the National Burn Repository. J Burn Care Res. 2009;30:30–36. doi: 10.1097/BCR.0b013e3181921efc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Richards WT. Predicting resource utilization of elderly burn patients in the baby boomer era. Am J Surg. 2013;205:29–34. doi: 10.1016/j.amjsurg.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Department of Economic and Social Affairs. World population ageing: 1950–2050. United Nations, New York. 2002 [Google Scholar]
- 16.Anous MM, Heimback DM. Causes of death and predictors in burned patients more than 60 years of age. J Trauma. 1986;26(2):135–139. doi: 10.1097/00005373-198602000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Khadim MF. Mortality estimates in the elderly burn patients: the Northern Ireland experience. Burns. 2009;35(1):107–113. doi: 10.1016/j.burns.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 18.Rao K. Aetiology and outcome of burns in the elderly. Burns. 2006;32(7):802–805. doi: 10.1016/j.burns.2006.03.024. [DOI] [PubMed] [Google Scholar]
- 19.Lumenta DB. Mortality and morbidity among elderly people with burns -evaluation of data on admission. Burns. 2008;34(7):965–974. doi: 10.1016/j.burns.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 20.Wibbenmeyer LA. Predicting survival in an elderly burn patient population. Burns. 2001;27(6):583–590. doi: 10.1016/s0305-4179(01)00009-2. [DOI] [PubMed] [Google Scholar]
- 21.Mahar P. Clinical factors affecting mortality in elderly burn patients admitted to a burns service. Burns. 2008;34(5):629–636. doi: 10.1016/j.burns.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 22.Wong P. Elderly burn prevention: a novel epidemiological approach. Burns. 2007;33(8):995–1000. doi: 10.1016/j.burns.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 23.Chang EJ. Gender influences on burn outcomes in the elderly. Burns. 2005;31(1):31–35. doi: 10.1016/j.burns.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 24.Santos DC, Barros F, Gomes N, Guedes T, Maia M. Face and/or neck burns: a risk factor for respiratory infection? Ann Burns Fire Disasters. 2016;40(3):97–102. [PMC free article] [PubMed] [Google Scholar]


