Abstract
Objective
To evaluate improvements in otologic symptoms after endoscopic sinus surgery (ESS) in patients with chronic rhinosinusitis (CRS), and identify differences in symptoms, if any, between CRS patients with (CRSwNP) and without (CRSsNP) nasal polyposis.
Material and methods
This is a prospective multi-center observational cohort study. Adults with medically recalcitrant CRS who elected ESS were enrolled in a prospective, multi-center, observational cohort study between March, 2011 and October, 2014. Preoperative evaluation of subjects included assessment of clinical characteristics, measures of disease severity, and quality of life evaluation using the 22-item SinoNasal Outcome Test (SNOT-22). Postoperative improvement in otologic symptoms (ear fullness, dizziness, ear pain) scores were evaluated and compared between CRSwNP and CRSsNP subgroups.
Results
Three hundred and ninety-five study patients completed both preoperative and postoperative evaluations, with an average follow-up of 13.9 months after ESS. The prevalence of patients reporting at least one otologic symptom preoperatively (87%) significantly decreased after ESS (63%, P < 0.001). Significant postoperative improvement across all otologic scores was also reported (P < 0.001). Relative mean improvement in otologic symptom severity was similar for both CRSwNP and CRSsNP, except patients with CRSwNP reported significantly greater postoperative improvement in ear fullness compared to CRSsNP (54% vs. 41%, P = 0.039). A total of 61%, 44%, and 43% of patients reported experiencing improvement in “ear fullness”, “dizziness” and “ear pain”, respectively.
Conclusion
Sinus surgery significantly improves otologic symptoms associated with CRS. CRSwNP patients reported slightly greater relief of ear fullness than CRSsNP patients following ESS.
Keywords: Ear symptoms, Chronic rhinosinusitis, Endoscopic sinus surgery
Introduction
Chronic rhinosinusitis (CRS) can cause not only nasal symptoms, but also associated otologic symptoms, with negative impact on social and emotional aspects of daily life. The nasal cavity is connected anatomically and functionally to the middle ear via the eustachian tube, so that diseases of the nose and paranasal sinuses can result in middle ear disease.1 These relationships have been studied more extensively in the pediatric population, whose anatomy predisposes them to eustachian tube dysfunction (ETD) and otitis media with effusion (OME), often compounded by co-morbid adenoid hypertrophy.2 Among adults, there has been relatively less investigation into the relationship between sinonasal and otologic disease.
While otologic symptoms may be considered a minor symptom criteria in the diagnosis of CRS, the severity of otologic symptoms associated with CRS may be great. Despite this, there is very little literature to date that focuses on the effects of endoscopic sinus surgery (ESS) on otologic symptoms in adults. Studies have reported otologic symptoms as part of broader health questionnaires, or grouped them with other symptoms into domains like “ear/facial symptoms” or “oropharyngeal symptoms” for further evaluation,3, 4 but only one so far that has looked specifically at otologic outcomes after ESS for CRS.5 This retrospective study found that symptoms of “ear fullness/congestion”, “dizziness”, “ear cracking/popping” and “ear pain”, which are associated with ETD, were present in 15%–42% of patients, and that ESS had a significant positive treatment effect on all of them. The goal of this study was to evaluate post-ESS changes in otologic symptoms associated with CRS as determined by standardized patient-reported outcome measures.
Materials and methods
Study population and inclusion criteria
Adult patients with a confirmed diagnosis of CRS as defined by criteria outlined by both the European Position Paper on Rhinosinusitis and Nasal Polyps 2012 (EPOS 2012) and the American Academy of Otolaryngology,6, 7 were recruited and prospectively enrolled into a continuing, multi-center, observational, prospective cohort investigation across five academic tertiary rhinology practices in North America (Oregon Health & Science University (OHSU), Portland, OR, Stanford University, Palo Alto, CA, the Medical University of South Carolina, Charleston, SC, and the University of Calgary, Calgary, Alberta, Canada). The Institutional Review Board (IRB) at each enrollment location governed all investigational protocols and specific informed patient consent documentation. All study participants elected endoscopic sinus surgery (ESS) as the subsequent treatment option for alleviation of symptoms related to CRS after previous medical therapy including, but not limited to, at least one course (≥14 days) of broad spectrum or culture-directed antibiotics and at least one course of either topical corticosteroids (≥21 days) or a 5-day course of oral corticosteroid therapy. The extent of ESS was directed by the discretion of each enrolling physician based on an amalgamation of patient-reported symptoms and radiologic and endoscopic findings of disease severity. All surgical cases were followed with postoperative therapeutic regimens including daily nasal saline rinses and subsequent medical therapy if necessary. Preliminary findings from this investigation have been previously reported.4, 8, 9, 10, 11, 12, 13, 14, 15, 16
Study data collection and management
During each preoperative enrollment meeting, participants were asked to provide detailed demographic information, as well as social and medical history. Participants were also asked to complete an extensive battery of patient-based survey instruments chosen to evaluate quality of life (QOL) and symptom severity for the study duration, including the 22-item SinoNasal Outcome Test (SNOT-22).17 The SNOT-22 is a validated, disease-specific, patient-reported QOL questionnaire developed for evaluating sinonasal conditions, and has been used as a primary outcome measure in previous outcome studies of CRS.4, 9, 10, 11, 12, 13, 14, 15, 16, 17 The minimal clinically important difference (MCID) of this questionnaire has been shown to be 8.9 units.17 Baseline Lund–Mackay scores of computed tomography (CT) of the paranasal sinuses and Lund–Kennedy endoscopic scoring were performed by the enrolling surgeon at each site.18, 19 Participants were followed through the standard of care for up to 18 months after ESS and completed survey evaluations postoperatively at regular 6 month intervals, together with post-operative Lund–Kennedy endoscopic scoring.
Study data was de-identified at each enrollment site to ensure confidentiality before transfer to OHSU. All study data was manually entered into a relational database (Microsoft Access, Microsoft Corp., Redmond, WA.).
Exclusion criteria
Due to variations in disease etiology and potential variability in treatment study participants with recurrent acute rhinosinusitis (RARS) were excluded from final analysis. Participants were initially excluded if less than 6 months had lapsed since ESS procedures and any participant failing to provide any study related QOL evaluation within 18 months after ESS was considered lost to follow-up.
Otologic outcome measures
Otologic symptom scores were extracted from the study participants' SNOT-22 questionnaires, using the 3 discrete survey items “ear fullness”, “dizziness” and “ear pain”. Higher scores on the SNOT-22 suggest worse patient functioning or symptom severity. Individual item scores are measured using patient selected responses on a Likert scale where higher scores indicate worse symptom severity as follows: 0 = “No problem”; 1 = ”Very mild problem”; 2 = ”Mild or slight problem”; 3 = ”Moderate problem”; 4 = ”Severe problem”; 5 = ”Problem as bad as it can be”. The enrolling physician at each site was blinded to all patient-based survey responses for the study duration.
The specific otologic data extracted from the SNOT-22 questionnaires were then analyzed to describe the following four parameters: prevalence of otologic symptoms before and after ESS, degree of severity of otologic symptoms, proportion of patients with changes in otologic symptoms after ESS, and relative mean improvement of otologic symptoms after ESS. Relative mean improvement (RMI) was calculated to account for variations in preoperative scores, and was defined by the formula: [(mean preoperative score − mean postoperative score)/mean preoperative score] × 100%.
Data management and statistical analyses
Sample size estimations were completed using tests for two dependent means. A total of 27 study participants were required to detect a 1.0 difference on SNOT-22 item responses, corresponding to a discernible change in Likert scale responses for each otologic symptom score over time, using a two-tailed t-test, a 0.050 alpha level and 80% 1-β error probability, a highly conservative between group correlation of 0.300 and equal variance assumption of 1.5 units.
Statistical analyses were conducted using commercially available statistical software (SPSS v.22, IBM Corp., Armonk, NY.). Preoperative cofactors, clinical measures of disease severity, measures of surgical extent, otologic outcome scores, and days of medication use were evaluated descriptively while data normality was verified for all continuous measures using distributive analysis. Last available SNOT-22 item scores were used to operationalize each postoperative evaluation due to previously reported stability of postoperative scores between 6, 12, and 18 month follow-up.16 Preoperative and postoperative distributions were evaluated for all symptom item scores to identify potential floor or ceiling effects. Differences over time between both mean preoperative and postoperative symptom scores and ordinal responses were compared using Wilcoxon signed-rank tests for matched pairings. Significant improvement in the proportion (%) of participants reporting the presence of any otologic symptom was also compared using McNemar chi-square (χ2) testing for matched pairings and correlated bivariate proportions. Subgroup analysis was performed between CRS with (CRSwNP) and without (CRSsNP) nasal polyposis, because of the distinct clinical characteristics of these two entities, as well as between primary and revision surgery patients, to ascertain if there was any difference in otologic presentations between these groups of patients. All comparisons were conducted for the total cohort as well as subgroups, and differences in relative improvement between those subgroups were conducted using Mann–Whitney U test statistics. Two-tailed statistical differences were determined at the 0.050 level of significance.
Results
Final cohort characteristics
A total of 576 study participants completed enrollment procedures and received endoscopic sinus surgery between March, 2011 and October, 2014. A total of 395 participants were selected for final analyses after exclusions for RARS (n = 38) and removal of all subjects without available SNOT-22 follow-up evaluations (n = 143) to date. Participant characteristics and preoperative clinical measures of disease severity are described in Table 1. Participants were followed for an average of 13.9 months after endoscopic sinus surgery.
Table 1.
Cohort characteristics and preoperative clinical measures of disease severity (n = 395).
| Item | Mean [SD] | Range [LL, UL] | n (%) |
|---|---|---|---|
| Age (years) | 51.6 [15.6] | [18, 86] | |
| Male | 185 (47) | ||
| Caucasian | 334 (85) | ||
| African American | 19 (5) | ||
| Asian | 17 (4) | ||
| Hispanic/Latino | 23 (6) | ||
| Asthma | 148 (38) | ||
| Allergy (mRAST/skin prick) | 170 (43) | ||
| Nasal polyposis | 149 (38) | ||
| Aspirin sensitivity | 36 (9) | ||
| Septal deviation | 158 (40) | ||
| Turbinate hypertrophy | 62 (16) | ||
| Depression | 63 (16) | ||
| Tobacco use | 18 (5) | ||
| Alcohol consumption | 171 (43) | ||
| Ciliary dyskinesia | 12 (3) | ||
| Corticosteroid dependency | 33 (8) | ||
| Diabetes mellitus (Type I or II) | 33 (8) | ||
| Lund–Mackay CT scores | 12.2 [6.2] | [0, 24] | |
| Lund–Kennedy endoscopy scores | 6.3 [3.8] | [0, 18] |
SD, standard deviation; LL, lower limit; UL, upper limit; mRAST, modified radioallergosorbent testing; CT, computed tomography.
Prevalence of otologic symptoms
A total of 343 of the 395 study participants (87%) reported at least one otologic symptom before ESS intervention, with mixed severity, while only 247 (63%) participants reported at least one otologic symptom postoperatively (P < 0.001). Participants in both subgroups showed similar improvements, with the CRSwNP subgroup showing reduction from 86% to 57% (P < 0.001), and the CRSsNP subgroup from 87% to 66% postoperatively (P < 0.001).
Looking at the individual otologic symptoms, ear fullness had the greatest proportion of patients who reported presence of any severity of this symptom pre-operatively, compared with dizziness and ear pain (Table 2). This was found among the entire cohort, as well as in each of the subgroups analyzed. All groups had an improvement in the prevalence of each individual otologic symptom post-operatively (P < 0.001).
Table 2.
Proportion of patients reporting any severity of ear symptoms before and after endoscopic sinus surgery for whole cohort and subgroups.
| Symptom | Whole cohort (n = 395) |
CRSwNP (n = 149) |
CRSsNP (n = 246) |
Primary surgery (n = 180) |
Revision surgery (n = 215) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-operative (%) | Post-operative (%) | Pre-operative (%) | Pre-operative (%) | Post-operative (%) | Pre-operative (%) | Post-operative (%) | Post-operative (%) | Pre-operative (%) | Post-operative (%) | |
| Ear fullness | 82 | 54 | 82 | 82 | 50 | 81 | 82 | 49 | 82 | 59 |
| Dizziness | 58 | 33 | 54 | 54 | 29 | 60 | 64 | 30 | 53 | 35 |
| Ear pain | 57 | 33 | 54 | 54 | 32 | 59 | 57 | 27 | 57 | 39 |
All postoperative improvements are significant (P < 0.001); CRSwNP, chronic rhinosinusitis with nasal polyps; CRSsNP, chronic rhinosinusitis without nasal polyps.
Mean preoperative and postoperative QOL and otologic symptom scores
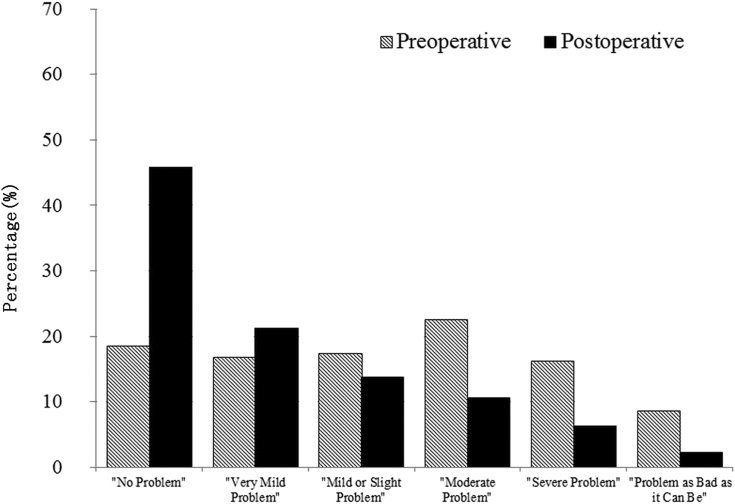
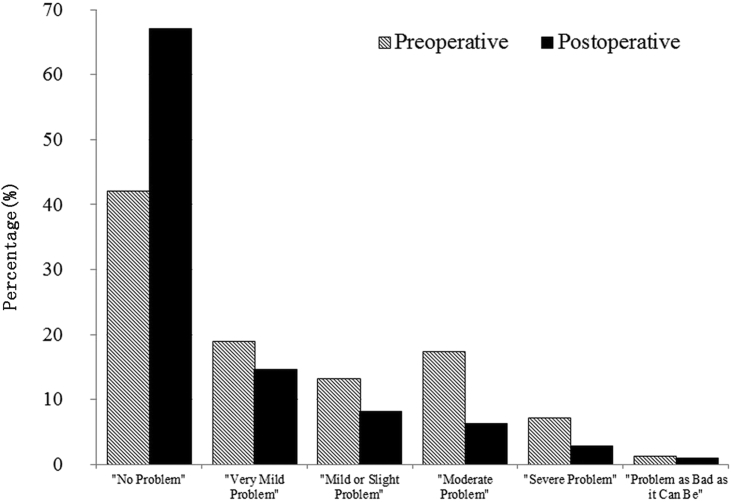
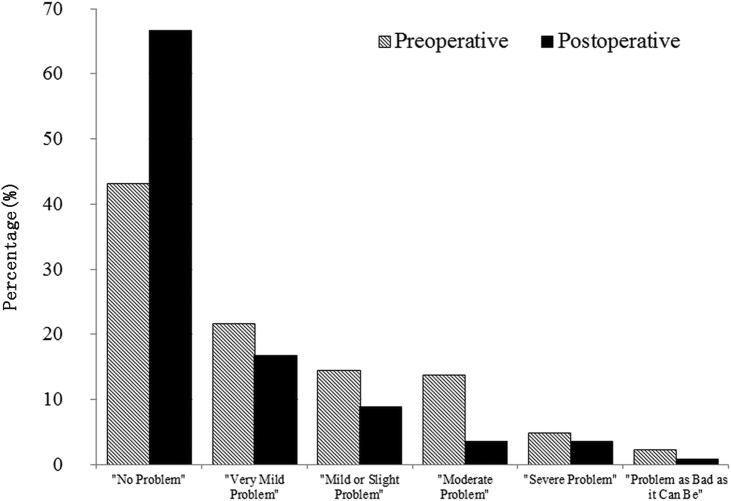
There was also improvement in the severity of otologic symptoms that were reported post-operatively. Significant postoperative improvement in mean SNOT-22 total scores and for each otologic item score of the SNOT-22 were found for the entire cohort, as well as for each of the subgroups analyzed (Table 3). Total cumulative proportions of preoperative and postoperative discrete otologic score responses are shown in Fig. 1, Fig. 2, Fig. 3, which also showed significant improvements post-operatively.
Table 3.
Pre-operative and post-operative SNOT-22 total scores and mean otologic symptom scores for whole cohort and subgroups.
| Whole cohort (n = 395) |
CRSwNP (n = 149) |
CRSsNP (n = 246) |
Primary surgery (n = 180) |
Revision surgery (n = 215) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-operative mean [SD] | Post-operative mean [SD] | Pre-operative mean [SD] | Post-operative mean [SD] | Pre-operative mean [SD] | Post-operative mean [SD] | Pre-operative mean [SD] | Post-operative mean [SD] | Pre-operative mean [SD] | Post-operative mean [SD] | |
| Total score | 53.1 [19.7] | 29.0 [21.6] | 55.0 [20.0] | 28.5 [20.8] | 52.0 [19.6] | 29.2 [22.1] | 51.4 [19.1] | 23.5 [18.4] | 54.6 [20.2] | 33.6 [23.0] |
| Ear fullness | 2.3 [1.6] | 1.2 [1.4] | 2.3 [1.6] | 1.0 [1.3] | 2.3 [1.6] | 1.3 [1.4] | 2.3 [1.6] | 0.9 [1.2] | 2.2 [1.6] | 1.4 [1.5] |
| Dizziness | 1.3 [1.4] | 0.7 [1.1] | 1.2 [1.4] | 0.6 [1.1] | 1.4 [1.4] | 0.7 [1.2] | 1.4 [1.3] | 0.6 [1.1] | 1.3 [1.5] | 0.7 [1.2] |
| Ear pain | 1.2 [1.4] | 0.6 [1.1] | 1.2 [1.4] | 0.5 [1.0] | 1.3 [1.3] | 0.9 [1.1] | 1.2 [1.3] | 0.5 [0.9] | 1.2 [1.4] | 0.8 [1.2] |
All postoperative improvements are significant (P < 0.001); CRSwNP, chronic rhinosinusitis with nasal polyps; CRSsNP, chronic rhinosinusitis without nasal polyps.
Fig. 1.
Distribution of preoperative and postoperative SNOT-22 item “ear fullness” Likert scores.
Fig. 2.
Distribution of preoperative and postoperative SNOT-22 item “dizziness” Likert scores.
Fig. 3.
Distribution of preoperative and postoperative SNOT-22 item “ear pain” Likert scores.
Relative mean improvement in symptom scores
Overall relative mean improvement for total SNOT-22 scores was found to be 42% with similar relative improvements in ear fullness (46%), dizziness (51%), and ear pain (56%). In participants with CRSwNP, relative percentage of mean improvement SNOT-22 total scores was 45%, with relative mean improvements in ear fullness (54%), dizziness (59%), and ear pain (61%). For participants with CRSsNP, relative mean improvement for total SNOT-22 scores was 40%, with relative mean improvements in ear fullness (41%), dizziness (47%), and ear pain (53%).
Relative improvement between CRSsNP and CRSwNP was found to be statistically similar for SNOT-22 total scores (P = 0.540), dizziness (P = 0.091), and ear pain (P = 0.484). However participants with CRSwNP reported significant greater improvement in ear fullness following ESS compared to CRSsNP counterparts (54% vs. 41%; P = 0.039).
Changes in status of otologic symptoms
We evaluated each individual patient to see if they experienced no change, improvement or worsening by ≥1 point of each otologic symptom after ESS, as we feel this provides more clinically relevant data for patient counselling. Overall, the percentage of patients showing improvement in ear fullness after ESS was greater than that for dizziness (P < 0.001) and ear pain (P < 0.001; Table 4). Similar findings were noted within each of the subgroups analyzed. Significantly more patients reported improvement in ear fullness (67% vs 57%; P = 0.050) and dizziness (50% vs 38%; P = 0.015) from the primary surgery subgroup compared to the revision surgery subgroup, while no significant difference was found for ear pain between these subgroups (47% vs 40%; P = 0.160). With reference to overall SNOT-22 scores, 79% of the entire cohort (n = 314)reported improvement in total SNOT-22 scores, defined as a reduction in scores by the MCID of 8.9, while 21% had either no change in or worsening of symptoms.
Table 4.
Percentages of patients who reported improvement, worsening, or no change of otologic symptoms following endoscopic sinus surgery.
| Ear fullness | Dizziness | Ear pain | |
|---|---|---|---|
| Whole cohort (n=395) | |||
| Improved | 61% | 44% | 43% |
| Worsened | 12% | 10% | 12% |
| No change | 27% | 46% | 45% |
| CRSwNP (n=149) | |||
| Improved | 66% | 42% | 42% |
| Worsened | 11% | 11% | 11% |
| No change | 23% | 47% | 46% |
| CRSsNP (n=246) | |||
| Improved | 58% | 44% | 44% |
| Worsened | 13% | 10% | 12% |
| No change | 29% | 46% | 44% |
| Primary surgery (n=180) | |||
| Improved | 67% | 50% | 47% |
| Worsened | 7% | 8% | 8% |
| No change | 27% | 42% | 45% |
| Revision surgery (n=215) | |||
| Improved | 57% | 38% | 40% |
| Worsened | 17% | 13% | 15% |
| No change | 26% | 50% | 45% |
CRSwNP, chronic rhinosinusitis with nasal polyps; CRSsNP, chronic rhinosinusitis without nasal polyps.
Discussion
The relationship between ETD and diseases of the sinonasal cavity has been well documented. Stammberger found that the normal secretory pathway of mucus flows around the eustachian tube orifice, while excessive or infected mucus may obstruct the orifice and promote ascending infections into the middle ear.1 The presence of infected mucus can cause chronic inflammation of the eustachian tube mucosa, or lead to ascending infection. A pediatric study found that 69.1% of children with CRS had altered middle ear pressure, with decreasing rates of ETD among older children.2 Unequal pressures between both middle ears may be contributory to the sensation of imbalance in ETD. In a retrospective study by Stoikes et al among adult patients with CRS who had undergone ESS, patients were asked to evaluate presence of “ear fullness and congestion”, “ear cracking and popping”, “dizziness” and “ear pain” before and after surgery.5 The prevalence of these individual otologic symptoms was up to 42% of patients, and surgery had a significant positive treatment effect on all of these symptoms. Similarly, Bhattacharyya reported that ESS provided a moderate effect size reduction in ear symptoms as evaluated from the Rhinosinusitis Symptom Inventory (RSI).3
Our study suggests that a much larger proportion of CRS patients than previously appreciated experience at least one otologic symptom (87%), with no significant difference between CRSsNP and CRSwNP subgroups. In comparison, the proportion of patients in our cohort experiencing nasal symptoms of thick nasal discharge, postnasal discharge, and nasal blockage or congestion was 92%, 93% and 96%, respectively. While our cohort may represent more complicated CRS patients presenting to tertiary centers, the findings nevertheless challenge the notion that otologic symptoms are a minor problem in patients suffering from CRS. More CRS patients experienced ear fullness (82%) than dizziness (58%) and ear pain (57%). These figures are much higher than the study by Stoikes et al, where the percentage of patients experiencing ear fullness, dizziness and ear pain preoperatively were 42%, 26% and 15% respectively.5 In both studies, ear fullness seemed to be the most common otologic symptoms reported by patients with CRS. This may be due to relief of eustachian tube obstruction by nasal polyps or postnasal discharge, or by reduction of nasopharyngeal edema.
Compared to ear fullness, dizziness and ear pain both had correspondingly larger proportions of patients with no change in symptoms postoperatively in our study. These findings corroborate results from previous studies.3, 5 While there was a group of patients whose otologic symptoms did not improve after ESS, 21% of the entire cohort also did not show postoperative improvement in total SNOT-22 scores, as defined by reduction of more than 8.9. This reflects clinical practice and experience, where not all patients may respond favorably to ESS due to a variety of factors. In addition, the non-responsiveness of otologic symptoms in some patients may also highlight the fact that otologic symptoms are nonspecific to CRS and may have other etiologies, and therefore continued workup of non-rhinogenic otologic symptoms may be warranted in some patients after ESS.
There are some caveats to consider when interpreting the findings of this study. Due to the focus of the study on CRS, we did not specifically evaluate patients preoperatively to exclude intrinsic otologic disease; ear symptoms were assumed to be due to CRS. This assumption may introduce some level of uncontrolled confounding of these results. Due to the nature of our study design, we were also unable to evaluate other aspects of otologic disease, such as otoscopic findings, audiometry and tympanometry, and their response to sinus surgery. As this was not a randomized placebo-controlled trial, we could not evaluate and compare the effect of medical management alone versus ESS on otologic symptoms associated with CRS. We also did not exclude patients with any preoperative otologic symptom score of 0 (“No problem”) to account for potential floor effect due to the fact that it would bias all estimates towards greater magnitudes of improvement and not account for those patients who did not improve or who reported worse otologic symptoms following ESS. While the overall SNOT-22 questionnaire has been validated as a patient-reported QOL assessment of CRS, the individual item scores may not be adequately discriminative of otologic symptoms. We thus analyzed the data in different approaches, all of which showed improvement in otologic symptoms after ESS. Our analysis did not consider other clinical phenotypes besides CRSsNP and CRSwNP, potentially missing nuances of otologic symptom presentation and response to ESS in other clinical subgroups. While our study is multi-institutional, the patients that are seen in our tertiary centers may not be externally generalizable to all patients with CRS undergoing ESS. Further studies specifically evaluating intrinsic otologic factors that may predispose CRS patients to ear symptoms may provide us with more insight into the relationship between otologic disease and CRS. Assessing patients with otologic-specific measures, such as audiometry and tympanometry, may help to further differentiate symptoms related to eustachian tube dysfunction from other middle ear diseases. The Cambridge Otology Quality of Life Questionnaire (COQOL), which is a new otology-specific patient-reported outcome measurement, may also be useful in evaluating treatment outcomes for these patients.20
Conclusion
Otologic symptoms, despite being minor criteria in the diagnosis of CRS, are more common among CRS patients than previously thought. ESS is effective in alleviating these symptoms, with the greatest benefit being seen in patients with ear fullness. CRSwNP patients reported greater relief of ear fullness than CRSsNP patients. For patients who still experience otologic symptoms after ESS, non-rhinogenic causes of ear disease should be sought.
Potential conflicts of interest
None to report.
Financial disclosures
Timothy L. Smith, Jess C. Mace, and Peter H. Hwang are supported by a grant for this investigation from the National Institute on Deafness and Other Communication Disorders (NIDCD), one of the National Institutes of Health, Bethesda, MD., USA (R01 DC005805; PI/PD: TL Smith). Public clinical trial registration (www.clinicaltrials.gov) ID# NCT01332136. This funding organization did not contribute to the design or conduct of this study; collection, management, analysis, or interpretation of the data; preparation, review, approval or decision to submit this manuscript for publication. There are no financial disclosures for Neville W. Teo. Peter H. Hwang is a consultant for Intersect ENT, Medtronic, Smith & Nephew, & Olympus.
Edited by Yu-Xin Fang
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Stammberger H. An endoscopic study of tubal function and the diseased ethmoid sinus. Arch Otorhinolaryngol. 1986;243:254–259. doi: 10.1007/BF00464441. [DOI] [PubMed] [Google Scholar]
- 2.Leo G., Piacentini E., Incorvaia C., Consonni D. Sinusitis and eustachian tube dysfunction in children. Pediatr Allergy Immunol. 2007;18(suppl 18):35–39. doi: 10.1111/j.1399-3038.2007.00631.x. [DOI] [PubMed] [Google Scholar]
- 3.Bhattacharyya N. Symptom outcomes after endoscopic sinus surgery for chronic rhinosinusitis. Arch Otolaryngol Head Neck Surg. 2004;130:329–333. doi: 10.1001/archotol.130.3.329. [DOI] [PubMed] [Google Scholar]
- 4.DeConde A.S., Bodner T.E., Mace J.C., Smith T.L. Response shift in quality of life after endoscopic sinus surgery for chronic rhinosinusitis. JAMA Otolaryngol Head Neck Surg. 2014;140:712–719. doi: 10.1001/jamaoto.2014.1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stoikes N.F., Dutton J.M. The effect of endoscopic sinus surgery on symptoms of eustachian tube dysfunction. Am J Rhinol. 2005;19:199–202. [PubMed] [Google Scholar]
- 6.Fokkens W.J., Lund V.J., Mullol J. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology. 2012;50:1–12. doi: 10.4193/Rhino12.000. [DOI] [PubMed] [Google Scholar]
- 7.Rosenfeld R.M., Andes D., Bhattacharyya N. Clinical practice guideline: adult sinusitis. Otolaryngol Head Neck Surg. 2007;137:S1–S31. doi: 10.1016/j.otohns.2007.06.726. [DOI] [PubMed] [Google Scholar]
- 8.Soler Z.M., Mace J., Smith T.L. Symptom-based presentation of chronic rhinosinusitis and symptom-specific outcomes after endoscopic sinus surgery. Am J Rhinol. 2008;22:297–301. doi: 10.2500/ajr.2008.22.3172. [DOI] [PubMed] [Google Scholar]
- 9.Alt J.A., Smith T.L., Schlosser R.J., Mace J.C., Soler Z.M. Sleep and quality of life improvements after endoscopic sinus surgery in patients with chronic rhinosinusitis. Int Forum Allergy Rhinol. 2014;4:693–701. doi: 10.1002/alr.21364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Soler Z.M., Rudmik L., Hwang P.H., Mace J.C., Schlosser R.J., Smith T.L. Patient-centered decision making in the treatment of chronic rhinosinusitis. Laryngoscope. 2013;123:2341–2346. doi: 10.1002/lary.24027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alt J.A., Smith T.L., Mace J.C., Soler Z.M. Sleep quality and disease severity in patients with chronic rhinosinusitis. Laryngoscope. 2013;123:2364–2370. doi: 10.1002/lary.24040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alt J.A., Mace J.C., Buniel M.C., Soler Z.M., Smith T.L. Predictors of olfactory dysfunction in rhinosinusitis using the brief smell identification test. Laryngoscope. 2014;124:E259–E266. doi: 10.1002/lary.24587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DeConde A.S., Mace J.C., Alt J.A., Schlosser R.J., Smith T.L., Soler Z.M. Comparative effectiveness of medical and surgical therapy on olfaction in chronic rhinosinusitis: a prospective, multi-institutional study. Int Forum Allergy Rhinol. 2014;4:725–733. doi: 10.1002/alr.21350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DeConde A.S., Mace J.C., Alt J.A., Soler Z.M., Orlandi R.R., Smith T.L. Investigation of change in cardinal symptoms of chronic rhinosinusitis after surgical or ongoing medical management. Int Forum Allergy Rhinol. 2015;5:36–45. doi: 10.1002/alr.21410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DeConde A.S., Barton M.D., Mace J.C., Smith T.L. Can sinus anatomy predict quality of life outcomes and operative times of endoscopic frontal sinus surgery? Am J Otolaryngol. 2015;36:13–19. doi: 10.1016/j.amjoto.2014.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DeConde A.S., Mace J.C., Alt J.A., Rudmik L., Soler Z.M., Smith T.L. Longitudinal improvement and stability of the SNOT-22 survey in the evaluation of surgical management for chronic rhinosinusitis. Int Forum Allergy Rhinol. 2015;5:233–239. doi: 10.1002/alr.21458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hopkins C., Gillett S., Slack R., Lund V.J., Browne J.P. Psychometric validity of the 22-item sinonasal outcome test. Clin Otolaryngol. 2009;34:447–454. doi: 10.1111/j.1749-4486.2009.01995.x. [DOI] [PubMed] [Google Scholar]
- 18.Lund V.J., Mackay I.S. Staging in rhinosinusitus. Rhinology. 1993;31:183–184. [PubMed] [Google Scholar]
- 19.Lund V.J., Kennedy D.W. Staging for rhinosinusitis. Otolaryngol Head Neck Surg. 1997;117(3 Pt 2):S35–S40. doi: 10.1016/S0194-59989770005-6. [DOI] [PubMed] [Google Scholar]
- 20.Martin T.P., Moualed D., Paul A. The Cambridge Otology Quality of Life Questionnaire: an otology-specific patient-recorded outcome measure. A paper describing the instrument design and a report of preliminary reliability and validity. Clin Otolaryngol. 2015;40:130–139. doi: 10.1111/coa.12338. [DOI] [PubMed] [Google Scholar]