Abstract
Objective
The purpose of this study was to investigate the distribution of chronic illness and associated disability, out-of-pocket payment (OOPP), and other related factors using survey data from Bangladesh.
Methods
This study analyzed Bangladesh Household Income and Expenditure Survey data that include socio-economic and demographic data, such as consumption, expenditures, and assets, along with information regarding chronic illness and disability. Multiple linear regression models were used to identify factors significantly associated with OOPP. Furthermore, a binary Logistic regression model was employed to assess the association of the explanatory variables with disability status.
Results
A higher prevalence of chronic illness was found for those with chronic gastritis (18.70%), and 41.92% of the population had at least one side disability. The average OOPP healthcare expenditure for chronic illness was estimated to be US$7.59. Higher OOPP was found among the upper 2 wealth quintiles. Overall OOPP health expenditure was significantly higher among individuals with an associated disability (P < 0.001). The likelihood of having an associated disability was higher among those individuals with a lower education level (OR = 2.36, 95% CI: 1.95–4.06), those who not earning an income (OR = 2.85, 95% CI: 2.53–3.21), those who did not seek care (OR = 1.73, 95% CI: 1.57–1.90), those who sought care from a pharmacy (OR = 8.91, 95% CI: 7.38–10.74), and those in the lowest wealth quintile (OR = 7.21, 95% CI: 6.41–8.12).
Conclusions
The high OOPP illustrates the necessity of financial risk protection for the population at low socio-economic status. Therefore, we recommend that the government strengthen the healthcare system with appropriate support directed to the rural and elderly populations.
Keywords: Chronic illness, Disability, Out-of-pocket payments, Burden, Bangladesh
Introduction
The burden of chronic illness is increasing and is a significant cause of mortality and morbidity worldwide.1 According to the 2015 Global Burden of Disease (GBD) study, non-communicable diseases (NCDs) caused 71.3% of global deaths in 2015, equivalent to approximately 39.8 million deaths. Total deaths attributable to NCDs rose by 14.3%, an increase of 5 million deaths since 20152; approximately 80% of these deaths occurred in low- and middle-income countries (LMICs).3 The rapidly increasing rates of chronic illness constitute a major public health challenge, undermining social and economic development.4 In the latest GBD study, the leading causes of NCD deaths were cardiovascular disease (17.9 million) and cancers (8.8 million), though the global death due to cancers increased by 17.0% since 2005.2 Chronic illnesses, including heart disease, stroke, cancer, chronic respiratory disease, and diabetes, account for half of annual mortality (54%) and the burden of illness (47%) in the Southeast Asian Region.5 Chronic illnesses are expected to exceed communicable, puerperal, prenatal, and food diseases on the list of leading causes of death in all countries by 2020.1 According to the comprehensive estimates in the GBD study, deaths from chronic NCDs are expected to increase up to 77% from 1990 to 2020, and chronic NCDs are the cause of disability in 68% of people living with disability worldwide and 84% in LMICs.6, 7 Bangladesh is presently in the middle of the epidemiologic transition, characterized by a shift in burden of disease as primarily attributable to infectious and deficiency diseases to mostly attributable to non-communicable chronic illnesses.8, 9 Recent evidence suggests that chronic illnesses are responsible for almost half of the annual mortality (51%) and burden of disease (41%) in Bangladesh.8 Chronic illnesses are not only responsible for premature death, but also have major adverse effects on quality of life and contribute to substantial economic costs on households, communities, and society.2 The high prevalence and duration of chronic conditions often require long-lasting continuing care that contributes to an increase in the disability burden.10, 11 The most difficult outcome for individuals with a chronic illness and disability is prevention of working, performing normal daily tasks, and socializing, which necessitate help from a caregiver and thus increases economic burden for the individual, household, and the country. Further, patients with chronic conditions usually incur high level of out-of-pocket payment (OOPP) for healthcare that leads to income deficiencies for other necessities, and impedes access to healthcare, therefore reducing quality of life.10, 12 OOPP may be a severe hardship if it consumes a large proportion of income, particularly for people with multiple chronic conditions, along with disability, who require regular health service for the management of their illness.
Chronic illnesses with or without a disability are usually related to high economic burden. Similar to many LMICs, Bangladesh is also facing the burden of disease where OOPP remains the most substantial support for healthcare, and health insurance is almost nonexistent, with the exception of small scale non-governmental organization-financed schemes.13, 14 Private health expenditure constitutes a significant share of total healthcare (63.3%) in Bangladesh, of which 97.4% is covered through OOPP.15 The increasing prevalence of multiple chronic conditions will contribute to increasing healthcare utilization and increasing costs.16 Moreover, individuals with chronic disease and associated disabilities have poorer health, and the healthcare costs for the disabled present a severe financial hardship that may be catastrophic to financial well-being.17 It has already been demonstrated that households with at least one member with chronic conditions face higher financial risks than other households18, 19, 20; financial risk might increase with associated disability. Studies have shown that as the need for OOPP health expenditure increases, there is a corresponding decrease in the use of health services in LMICs.21, 22 Reliance on OOPP results in catastrophic health expenditure and impoverishment in LMICs, including Bangladesh.22, 23 A study in Bangladesh reported that incidence of catastrophic health expenditure among households with members having chronic conditions is significantly greater, and the financial risk of the lowest income households was about 3 times higher than the highest income households.24 While there is accumulated evidence showing a rapid rise in chronic disease, literature on the extent to which households experience financial burden related to OOPP due to chronic disease and disabilities is limited. The objective of this study was to observe the distribution of chronic illness with associated disability, and to assess the financial burden of households due to chronic conditions and associated disabilities using nationwide survey data.
Material and methods
Data source
This study used data from a large nationally representative survey, the Bangladesh Household Income and Expenditure Survey (HIES) 2010, conducted by the Bangladesh Bureau of Statistics (BBS), an apex organization of Bangladesh's Ministry of Planning. The survey objectives, sampling technique, survey design, survey instruments, measuring system, and quality control have been described elsewhere.25 In brief, a 2-stage stratified random sampling technique was employed for drawing the sample of HIES 2010, under the framework of Integrated Multipurpose Sample (IMPS) design, developed on the basis of the sampling frame for the Population and Housing Census 2001. The IMPS design consisted of 1000 Primary Sampling Units (PSUs), with 640 from rural and 360 from urban PSUs included in the sample throughout the country. Each PSU comprised approximately 200 households and was selected from 16 different strata. In the second stage, 20 households were selected from each of the rural PSUs and PSUs located in the municipal areas. Data collection was performed between February 1, 2010 and January 31, 2011.
A total of 12,240 households were selected, with 7840 from rural areas and 4400 from urban areas. Among the selected households, a total of 55,580 individuals were interviewed, 35,894 from rural areas and the remainder from urban areas. The survey collected socio-economic data at the household level, such as family earnings, consumption, and expenditures, assets, housing conditions, as well as individual level data on demographic structure (age, gender, marital status), education, employment, health, and disability. This analysis considered both household and individual level data. The wealth quintile was constructed using household characteristics from household level data and, then, values of wealth quintile were allocated to all individuals based on household. However, 74 cases were dropped due to missing values for the wealth index. Finally, data from 39,245 (70.61%) individuals with any type of chronic illness were analyzed. In order to estimate OOPP, data from 12,400 (31.60%) individuals with chronic disease were considered, based on any type of healthcare utilization and associated expense in the 30 days preceding the survey. Individuals of any age range with chronic illness were included in the analysis.
Study variables
Outcome variable
The World Health Organization (WHO) developed the International Classification of Functioning, Disability, and Health (ICFDH) to provide a framework for conceptualizing disability. Functionalizing an ICF-based strategy for disability has required the advancement of new measurement models for conducting both censuses and surveys. The Washington Group had developed and adopted a small set of 6 disability-related questions suitable for use in national censuses and surveys.26 The HIES-2010 used this set of questions for the disability components to be consistent with the ICFDH.26 The disability module included 6 functional domains or basic actions: (1) vision, (2) hearing, (3) walking and climbing, (4) remembering and concentrating, (5) self-care, and (6) speaking and communicating. To estimate disabilities for the above 6 functions, a set of questions for the disability components were included in the HIES-2010 survey and every individual of the household was requested to provide information about the presence of any disability and the severity of the disability. Each question had 4 response levels: (a) no difficulty; (b) yes, some difficulty; (c) yes, severe difficulty; or (d) yes, can't see/hear/walk/remember/self-care/communicate at all. For analysis, we recoded the presence of disability into 2 groups: ‘0’ denoted for “no difficulty” or ‘1’ for “any level of difficulty”.17, 26, 27 Furthermore, to create an outcome variable reflecting the presence of a disability, defined as having at least one of the above six disabilities, we created a measure with 2 values, ‘1’ denoting “at least one side disability,” and a value of ‘0’ denoting “no disability”. For the other outcome measurement, OOPP for healthcare was derived by summing up direct medical costs, including hospital outpatient fees, medicine, admission or registration fees, physician fees, diagnostic fees, and any other associated medical supplies and direct non-medical costs, including transportation and conveyance, lodging, tips, and other associated costs.25 Indirect costs such as loss of productivity, opportunity costs, and other intangible costs, such as pain and suffering, were not captured in the survey.
Independent variables
OOPP healthcare expenditure was regressed onto explanatory variables, such as demographics (sex, age, marital status, education, employment), type of chronic disease (chronic fever, injuries, chronic heart disease, asthma, gastritis or ulcer, hypertension, arthritis, diabetes, chronic dysentery, eczema, cancer, leprosy, paralysis, epilepsy, or others), type of healthcare provider (public, private, pharmacy/dispensary, traditional, or other), and economic status (lowest 20%, second 20%, middle 20%, fourth 20%, or highest 20%). Age was divided into 5 groups: childhood (0–19 years), young adulthood (20–39 years), middle-aged (40–64 years), senior (65–84 years), or old senior (>84 years).28 Marital status was categorized into 3 groups: unmarried, married, or other (widowed, divorced, or separated). Educational level was categorized as: no education, primary education, secondary education, higher secondary, or higher education and earning status.
Statistical analysis
Descriptive statistics were employed to summarize the data about the different variables (Table 1). Status of disability (“1” denoted the presence of at least one disability with chronic illness and “0” denoted no associated disability) and OOPP healthcare expenditure were considered the outcome variables. OOPP data was characterized by a large cluster of data at zero, and the right-skewed distribution of the remaining observations; however, the 76 zeros have been deleted for the current analysis. The natural log of OOPP healthcare expenditure was used to reduce the effects of the skewed nature of the OOPP healthcare expenditure variable. Multiple linear regression models were used to evaluate the explanatory variables influencing OOPP. Furthermore, a binary Logistic regression model was used to assess the effect of disability status on the explanatory variables. Data cleaning, validation, and all statistical analyses were performed by using the STATA 13.0 software (Stata Corp LLC, Texas, USA).
Table 1.
Background characteristics of study population.
| Characteristics | n | % |
|---|---|---|
| Sex | ||
| Male | 17,511 | 44.62 |
| Female | 21,734 | 55.38 |
| Age group | ||
| Childhood (≤19 years) | 746 | 1.90 |
| Young adult (20–39 years) | 8564 | 21.82 |
| Middle aged (40–64 years) | 21,691 | 55.27 |
| Senior aged (65–84 years) | 7010 | 17.86 |
| Old senior aged (≥85 years) | 1234 | 3.14 |
| Marital status | ||
| Unmarried | 2140 | 5.45 |
| Married | 27,202 | 69.31 |
| Other | 9903 | 25.23 |
| Education level | ||
| No education | 23,668 | 60.31 |
| Primary | 8492 | 21.64 |
| Secondary | 5496 | 14.00 |
| Higher secondary | 278 | 0.71 |
| Higher | 1311 | 3.34 |
| Income earner | ||
| No | 11,529 | 29.38 |
| Yes | 27,716 | 70.62 |
| Chronic illness with at least one side disability | ||
| No disability | 22,795 | 58.08 |
| Any disability | 16,450 | 41.92 |
| Sought medical treatment | ||
| Yes | 12,400 | 31.60 |
| No | 26,845 | 68.40 |
| Treatment from healthcare provider's | ||
| Public | 27,405 | 69.83 |
| Private | 7515 | 19.15 |
| Pharmacy/Dispensary | 3567 | 9.09 |
| Traditional | 1,34 | 0.34 |
| Other | 624 | 1.59 |
| Residence | ||
| Rural | 25,601 | 65.23 |
| Urban | 13,644 | 34.77 |
| Wealth quintile | ||
| Lowest 20% | 7154 | 18.23 |
| 2nd | 8358 | 21.30 |
| 3rd | 8243 | 21.00 |
| 4th | 6023 | 15.35 |
| Upper 20% | 9467 | 24.12 |
Ethical considerations
The Ethics Committee at Bangladesh Bureau of Statistics (BBS) approved a waiver from ethical approval for this retrospective study. As the de-identified data for this study came from secondary sources, this study did not require ethical approval.
Results
Description of study population
Table 1 demonstrates descriptive information about the study population. The percentage of the female population (55.38%) was higher than the male population (44.62%). More than half (55.27%) of the study population was middle-aged (40–64 years), followed by young adult (21.82%) where a higher number of persons were married (69.31%). Regarding education level, about 60% of study population were illiterate, followed by 21.64% of the study population have a primary school education. Among the study sample, approximately 70% of persons were income earners although more than 65% were living in rural communities. Regarding the duration of self-reported chronic illness, the mean duration of illness was 8.33 (standard deviation (SD): 9.84) years while a higher percentage (68.40%) of persons did not receive any healthcare in last 30 days. Furthermore, about 41.92% persons reported having at least one disability along with the chronic illness. Most of the persons received healthcare from a public provider (69.83%); in contrast, only 19.15% of persons received healthcare from private providers.
Distribution of chronic disease, duration, and disability
The frequency distribution of the sample population according to self-reported chronic illnesses is shown in Table 2. A high prevalence of chronic gastritis or ulcer (18.70%), arthritis (17.54%), chronic heart disease (8.52%), asthma (7.54%), paralysis (7.08%) was found. The mean duration of illness was highest for asthma (23.07 ± 16.34 years), followed by gastritis or ulcer (9.21 ± 9.22 years), leprosy (8.99 ± 13.44 years), epilepsy (12.90 ± 14.19 years), and diabetes (8.57 ± 6.14 years). Considering chronic illness with at least one disability, the higher prevalence was observed for paralysis (98.85%), asthma (59.56%), arthritis (56.00%), chronic fever (52.14%) and gastritis or ulcer (45.37%).
Table 2.
Distribution of chronic illness, duration and at least one side disabilities.
| Chronic illness | n (%) | Duration of illness in years |
At least one side disability with chronic illness, n (%) | |
|---|---|---|---|---|
| Mean ± SD | 95% CI | |||
| Chronic fever | 2480 (6.32) | 1.13 ± 1.82 | (1.06, 1.20) | 1293 (52.14) |
| Injuries | 1702 (4.34) | 1.85 ± 4.57 | (1.63, 2.07) | 140 (8.23) |
| Chronic heart disease | 3342 (8.52) | 6.46 ± 5.21 | (6.28, 6.64) | 177 (5.30) |
| Asthma | 2960 (7.54) | 23.07 ± 16.34 | (22.48, 23.66) | 1763 (59.56) |
| Gastric or ulcer | 7339 (18.70) | 9.21 ± 9.22 | (9.00, 9.42) | 3330 (45.37) |
| Hypertension | 5116 (13.04) | 3.93 ± 3.53 | (3.84, 4.03) | 1285 (25.12) |
| Arthritis | 6882 (17.54) | 7.47 ± 4.28 | (7.37, 7.58) | 3854 (56.00) |
| Diabetes | 875 (2.23) | 8.57 ± 6.14 | (8.17, 8.98) | 145 (16.57) |
| Chronic dysentery | 112 (0.29) | 6.94 ± 8.27 | (5.39, 8.49) | 28 (25.00) |
| Eczema | 123 (0.31) | 8.11 ± 8.83 | (6.54, 9.69) | 20 (16.26) |
| Cancer | 79 (0.20) | 4.02 ± 8.64 | (2.09, 5.96) | 57 (72.15) |
| Leprosy | 31 (0.08) | 8.99 ± 13.44 | (4.07, 13.92) | 7 (22.58) |
| Paralysis | 2779 (7.08) | 2.42 ± 3.14 | (2.30, 2.54) | 2747 (98.85) |
| Epilepsy | 35 (0.09) | 12.9 ± 14.19 | (8.03, 17.77) | 9 (25.71) |
| Others | 5390 (13.73) | 13.86 ± 11.72 | (13.55, 14.17) | 1595 (29.59) |
| Total | 39,245 (100.0) | 8.33 ± 9.84 | (8.23, 8.42) | 16,450 (41.92) |
SD: standard deviation.
Distribution of OOPP
The average OOPP healthcare expenditure for chronic illness in last 30 days was US$ 23.78; female patients spent more than male patients (US$ 28.75 vs. US$ 15.33) (Table 3). Regarding age, the highest amount of OOPP were reported in the middle-aged group (US$ 32.73), followed by old senior (US$ 22.9) and young adult (US$ 13.71) age groups. Moreover, compared to other chronic illnesses, higher OOPP was observed for cancer (US$ 106.04), chronic heart disease (US$ 54.38), gastritis or ulcer (US$ 36.88), injuries (US$ 24.11), chronic fever (24.11) and diabetes (US$ 20.99). Overall OOPP was higher for receiving healthcare from public providers (US$ 47.71), followed by local pharmacy or dispensary (US$ 33.45) as well as private providers (US$ 19.8) and traditional providers (US$ 7.99) (such as kabiraj, traditional healers, and so on). According to residence setting, those who lived in urban areas spent more money (US$ 32.42) compared to rural residents (US$ 18.56). Furthermore, households within 4th wealth quintiles spent more (US$ 57.45), followed by the highest (5th) wealth quintile (US$ 29.4).
Table 3.
Distribution of out-of-pocket payment (in USD) in the last 30 days.
| Components | Out-of-pocket payment USD in last 30 days |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Without disability |
With disability |
Overall out-of-pocket payment |
|||||||
| n | Mean ± SD | Median (IQR) | n | Mean ± SD | Median (IQR) | n | Mean ± SD | Median (IQR) | |
| Gender | |||||||||
| Male | 2628 | 17.09 ± 30.06 | 9.13 (14.78) | 1961 | 12.98 ± 65.46 | 7.25 (2.35) | 6586 | 15.33 ± 50.53 | 7.25 (16.67) |
| Female | 3958 | 24.74 ± 46.31 | 14.49 (54.78) | 3853 | 32.87 ± 39.53 | 6.52 (73.12) | 5814 | 28.75 ± 43.29 | 7.25 (54.78) |
| Age group | |||||||||
| Childhood (≤19 years) | 1477 | 11.16 ± 24.14 | 4.06 (7.25) | 128 | 16.63 ± 28.25 | 5.80 (17.46) | 1605 | 11.74 ± 24.61 | 4.35 (7.54) |
| Young adult (20–39 years) | 245 | 13.37 ± 61.96 | 9.13 (3.91) | 29 | 17.62 ± 42.96 | 4.35 (9.75) | 274 | 13.71 ± 60.67 | 9.13 (4.78) |
| Middle aged (40–64 years) | 3541 | 32.08 ± 31.11 | 23.91 (43.48) | 3800 | 33.34 ± 39.61 | 6.52 (73.12) | 7341 | 32.73 ± 35.77 | 23.91 (53.91) |
| Senior aged (65–84 years) | 1310 | 5.06 ± 25.30 | 3.19 (1.25) | 1813 | 11.84 ± 71.26 | 7.25 (4.52) | 3123 | 9.00 ± 31.54 | 7.25 (4.06) |
| Old senior aged (≥85 years) | 13 | 7.75 ± 7.96 | 5.80 (13.77) | 44 | 27.38 ± 75.70 | 7.90 (18.66) | 57 | 22.90 ± 66.96 | 7.25 (15.45) |
| Type of chronic illness | |||||||||
| Chronic fever | 1075 | 24.09 ± 23.01 | 23.91 (4.75) | 21 | 25.21 ± 81.22 | 6.59 (11.74) | 1096 | 24.11 ± 25.29 | 23.91 (12.32) |
| Injuries | 51 | 21.88 ± 58.07 | 4.35 (13.04) | 61 | 32.12 ± 64.32 | 6.88 (22.46) | 112 | 27.45 ± 61.49 | 5.29 (20.85) |
| Chronic heart disease | 1316 | 55.08 ± 60.38 | 57.97 (6.59) | 73 | 41.78 ± 144.22 | 5.8 (17.68) | 1389 | 54.38 ± 67.40 | 57.97 (10.20) |
| Asthma | 804 | 15.26 ± 18.86 | 14.49 (3.21) | 619 | 7.52 ± 10.16 | 6.52 (2.26) | 1423 | 11.89 ± 16.14 | 6.52 (7.97) |
| Gastric or ulcer | 1626 | 5.06 ± 12.83 | 3.19 (2.16) | 1764 | 66.21 ± 21.69 | 73.91 (4.52) | 3390 | 36.88 ± 35.46 | 10.07 (70.72) |
| Hypertension | 1005 | 9.82 ± 13.68 | 9.13 (4.98) | 93 | 88.82 ± 754.27 | 4.35 (9.13) | 1098 | 16.51 ± 219.93 | 9.13 (4.65) |
| Arthritis | 193 | 16.82 ± 60.93 | 3.91 (10.43) | 175 | 10.35 ± 21.65 | 4.35 (10.58) | 368 | 13.74 ± 46.64 | 4.06 (10.66) |
| Diabetes | 93 | 25.41 ± 98.05 | 7.83 (18.12) | 45 | 11.87 ± 18.56 | 4.35 (13.62) | 138 | 20.99 ± 81.29 | 7.25 (17.39) |
| Chronic dysentery | 30 | 6.30 ± 11.69 | 1.96 (3.77) | 9 | 4.22 ± 3.68 | 3.62 (5.22) | 39 | 5.82 ± 10.39 | 2.17 (4.06) |
| Eczema | 29 | 6.94 ± 9.94 | 4.35 (5.65) | 9 | 7.75 ± 9.42 | 3.62 (7.97) | 38 | 7.13 ± 9.70 | 4.20 (5.80) |
| Cancer | 5 | 124.90 ± 168.46 | 39.13 (186.09) | 1 | 11.74 ± (–) | 11.74 (–) | 6 | 106.04 ± 157.60 | 25.43 (186.09) |
| Leprosy | 9 | 8.50 ± 16.78 | 1.59 (6.67) | 2 | 10.33 ± 3.43 | 10.33 (4.86) | 11 | 8.83 ± 15.07 | 2.61 (10.29) |
| Paralysis | 3 | 130.53 ± 210.95 | 17.39 (373.62) | 1562 | 7.42 ± 4.30 | 7.25 (3.72) | 1565 | 7.66 ± 10.22 | 7.25 (4.58) |
| Epilepsy | 11 | 7.81 ± 7.01 | 5.8 (9.42) | 3 | 5.85 ± 5.22 | 5.65 (10.43) | 14 | 7.39 ± 6.53 | 5.72 (8.26) |
| Others | 336 | 17.16 ± 44.12 | 5.51 (11.00) | 1377 | 2.02 ± 9.01 | 0.80 (0.12) | 1713 | 4.99 ± 21.96 | 0.80 (0.20) |
| Healthcare provider | |||||||||
| Private | 5691 | 23.16 ± 31.23 | 14.49 (20.72) | 2024 | 10.33 ± 31.04 | 7.25 (4.25) | 7715 | 19.8 ± 31.68 | 9.13 (16.67) |
| Public | 242 | 30.57 ± 145.60 | 8.26 (15.94) | 131 | 79.37 ± 636.26 | 8.99 (18.12) | 373 | 47.71 ± 394.65 | 8.41 (16.23) |
| Pharmacy/Dispensary | 514 | 4.75 ± 9.38 | 2.46 (4.20) | 3050 | 38.29 ± 36.34 | 73.91 (73.12) | 3564 | 33.45 ± 35.80 | 4.35 (73.12) |
| Traditional | 78 | 7.81 ± 13.73 | 3.26 (6.64) | 47 | 8.28 ± 23.37 | 2.90 (5.51) | 125 | 7.99 ± 17.88 | 2.90 (5.91) |
| Other | 61 | 8.66 ± 22.03 | 2.17 (5.07) | 562 | 6.48 ± 2.55 | 6.52 (2.40) | 623 | 6.69 ± 7.29 | 6.52 (4.20) |
| Communities | |||||||||
| Rural | 3871 | 26.02 ± 45.24 | 23.91 (24.93) | 3855 | 11.06 ± 120.10 | 6.52 (6.45) | 7726 | 18.56 ± 90.98 | 7.25 (21.01) |
| Urban | 2715 | 15.50 ± 32.42 | 3.19 (11.30) | 1959 | 55.88 ± 31.90 | 73.91 (57.97) | 4674 | 32.42 ± 37.87 | 14.49 (70.72) |
| Economics status | |||||||||
| Lowest 20% | 468 | 14.03 ± 42.07 | 4.35 (8.64) | 795 | 8.97 ± 19.96 | 7.25 (6.45) | 1263 | 10.85 ± 30.19 | 7.25 (6.09) |
| 2nd | 1300 | 11.71 ± 21.81 | 9.13 (4.62) | 2135 | 6.28 ± 16.04 | 7.25 (6.45) | 3435 | 8.33 ± 18.62 | 7.25 (8.33) |
| 3rd | 1489 | 18.25 ± 13.60 | 14.49 (9.42) | 615 | 22.46 ± 56.11 | 0.80 (26.74) | 2104 | 19.48 ± 32.46 | 14.49 (20.72) |
| 4th | 400 | 17.46 ± 38.77 | 7.54 (11.59) | 1276 | 69.99 ± 203.49 | 73.91 (0) | 1676 | 57.45 ± 179.94 | 73.91 (59.49) |
| Upper 20% | 2929 | 29.66 ± 53.13 | 23.91 (54.78) | 993 | 28.66 ± 32.62 | 6.52 (67.39) | 3922 | 29.40 ± 48.75 | 7.25 (54.78) |
| Total | 6586 | 21.68 ± 40.78 | 9.71 (20.72) | 5814 | 26.16 ± 101.76 | 7.25 (73.12) | 12,400 | 23.78 ± 75.78 | 7.25 (22.75) |
USD: United States Dollar; IQR: interquartile range; SD: standard deviation.
Regarding chronic illness with an associated disability, overall OOPP health expenditure was significantly higher for disabled people (US$ 26.16) compared to non-disabled people (US$ 21.68) (P < 0.001); females (US$ 32.87) spent more than males (US$ 12.98). Furthermore, a significant variation of OOPP health expenditure was observed between females with associated disability (US$ 32.87) and those with no disability (US$ 24.74) (P < 0.001). It was also noted that senior and old senior aged people with associated disability spent significantly higher compared to non-disabled persons; however, all age group with associated disability spent higher than that of non-disabled. It is found that the people without associated disability suffered from chronic heart disease, diabetes, arthritis, and cancer, and spent more than persons with disability. Regarding healthcare provider, the people with an associated disability had higher expenditure when they sought care from any provider (public or traditional) than non-disabled persons except private provider. Persons with an associated disability from urban communities experienced significantly greater OOPP compared to non-disabled persons; however, the reverse association was found in the case of rural communities. Across the economic status, the people with associated disability who belonged to middle and/or upper middle (3rd and 4th) wealth quintiles significantly spent more than that of non-disabled persons. However, people having a chronic illness without disability from richest wealth quintiles spent higher than persons with an associated disability.
Factors influencing disability with chronic diseases and out-of-pocket payment
Table 4 presents results of Logistic regression that predict the odds of having a disability with chronic illness and ordinary least squares (OLS) estimation of regression analysis to find out the influencing factors on OOPP health expenditure among the study population. The odds of having a disability increased significantly with increased in age as well as a long time suffering from the disease. Senior aged (65–84 years) was 3 times more likely to report having a disability with suffering from some of the chronic diseases than young aged (20–39 years). We found that married persons were more likely to report having a disability than unmarried; unemployed or the people who had no income sources, were more likely to have a disability than employed people; and those who were living in urban communities more likely to have a disability than persons from rural. The lower 2 wealth quintiles of household's member had more likelihood of reporting disabilities compared with those in the rich category; people who did not receive any healthcare for chronic disease were more like to report having a disability compared with those received any healthcare. OOPP among those who reported expenditure were likely to be higher for persons who were relatively female; child and elderly; married; illiterate and primary level education; long disease duration; received any healthcare from an informal healthcare provider as well as living in urban communities.
Table 4.
Influencing factors on chronic illness with disability and out-of-pocket payment.
| Variables | Model-I |
Model-II |
|---|---|---|
| Chronic illness with disability vs. without disability |
Out-of-pocket payment |
|
| OR (95% CI) | Co-efficient (95% CI) | |
| Constant | 2.07a (1.05–3.23) | 3.16a (2.8–3.51) |
| Gender | ||
| Female vs. male | 1.87a (1.06–2.18) | 1.56a (1.10–1.81) |
| Age group | ||
| <20 vs. 20–39 years | 0.64b (0.41–0.98) | 1.22a (1.13–2.35) |
| 40–64 vs. 20–39 years | 3.74c (3.27–4.28) | 2.40 (1.74–3.06) |
| 65–84 vs. 20–39 years | 3.24a (2.74–3.85) | 3.96a (1.82–5.10) |
| >85 years vs. 20–39 years | 0.17a (0.13–0.23) | 1.50a (1.09–5.51) |
| Marital status | ||
| Married vs. Unmarried | 2.13a (1.49–3.04) | 5.60a (2.25–6.94) |
| Other vs. Unmarried | 4.54 (3.13–6.59) | 1.41a (1.39–1.54) |
| Education level | ||
| No education vs. Higher | 2.36a (1.95–4.06) | 1.95a (1.64–5.25) |
| Primary vs. Higher | 4.46b (3.19–6.23) | 1.18a (1.15–9.27) |
| Secondary vs. Higher | 1.12 (0.80–1.56) | 3.09 (0.30–5.89) |
| Higher secondary vs. Higher | 1.81 (1.11–2.96) | −1.17a (−2.67–1.67) |
| Income earner | ||
| No vs. Yes | 2.85a (2.53–3.21) | −3.12a (−4.80–1.57) |
| Illness duration in years | 1.07a (1.06–1.07) | 2.15a (1.12–3.16) |
| Sought medical treatment | ||
| No vs. Yes | 1.73a (1.57–1.90) | 2.92a (1.16–6.68) |
| Treatment from healthcare provider's | ||
| Public vs. Private | 2.27 (1.66–3.09) | −3.00c (−4.66–1.52) |
| Pharmacy/Dispensary vs. Private | 8.91a (7.38–10.74) | 1.27b (1.06–1.48) |
| Traditional vs. Private | 3.23a (1.91–5.47) | 8.20a (5.31–9.10) |
| Other vs. Private | 8.48a (5.80–12.42) | 2.18 (2.04–3.23) |
| Residence | ||
| Urban vs. Rural | 1.31a (1.20–1.42) | 0.16b (−0.87–1.19) |
| Wealth quintile | ||
| Lowest quintile vs. upper quintile | 7.21a (6.41–8.12) | −5.43a (−6.97–(−3.9)) |
| 2nd vs. upper quintile | 5.26a (4.66–5.92) | −8.62a (−10.05–(−7.19)) |
| 3rd vs. upper quintile | 0.16 (0.14–0.18) | −1.87 (−3.25–(−0.49)) |
| 4th vs. upper quintile | 5.40 (4.81–6.06) | 4.62 (3.15–6.09) |
| n | 39,245 | 12,324 |
| R-square | 45.65 | |
| F-value (Prob > F) | 220.64 (0.000) | |
| Root MSE | 41.457 | |
| Mean VIF (Max) | 3.36 (3.85) | |
| Breusch–Pagan/Cook–Weisberg test (P > chi2) | 152.23 (0.001) | |
| Ramsey RESET, F (P > F) | 681.91 (0.005) | |
MSE: mean squared error; VIF: variance inflation factor.
a,b and c denote 1%, 5% and 10% significance level, respectively.
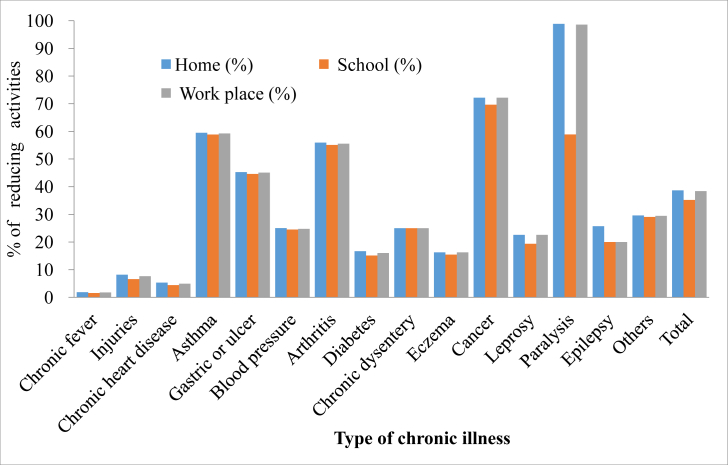
Distribution of reducing activities due to chronic disease with disabilities
Fig. 1 shows that distribution of reducing daily activities in the home, school, or working environment was associated with having a disability, as well as suffering from some of the chronic diseases. Persons who had been suffering from asthma and arthritis, more than half of the reported that they had reduced their daily activities at home, school or working environment. All persons who experienced paralysis had to reduce their day-to-day operations in the household and/or at their work place. Among the cancer patients with associated disability, about 72% of persons reported reduced household and/or workplace activities, and 69% reduced their academic activities as well.
Fig. 1.
Distribution of reducing activities due to chronic disease with at least one disabilities.
Discussion
This study reports findings based on nationally representative data on the distribution of OOPP healthcare spending and its association at the household level with chronic illness and disabilities in Bangladesh. Chronic diseases with associated co-morbidity are increasing globally with a growing concern for assessment of the disease burden and health system efficiency.29 However, limited research has been conducted in LMICs, where 80% of the NCDs burden falls.30 We examined the relationship between combinations of chronic illness with/without disability on OOPP healthcare expenditure and between different socio-economic characteristics. In this study, overall, a high prevalence of self-reported chronic illness was observed where nearly 40% of populations were affected by an associated disability. Cardiovascular disease, arthritis, and gastritis have found to be highly prevalent and contributed around 50% of total chronic illnesses. NCDs in Bangladesh have already affected a large population which also be reported in other studies.2, 8, 9 However, several studies conducted in other Asian countries documented the on-going epidemiologic transition and also found high economic burden associated with chronic illness.21, 24
The prevalence of chronic disease was higher among women in our study while other studies are also indicating a higher prevalence among women than men.31, 32, 33 Unlike earlier studies, this study demonstrated that the prevalence was higher in rural areas compared to urban areas34 and people >40 years of age experience higher rates of chronic illness. Earlier studies also reported that chronic illness conferred a heightened risk of disability, especially among older adults.11, 35 Also, other studies revealed that women and the population from rural areas were particularly affected by disability and suggested to conduct further research focusing on these groups since they were often excluded or under-sampled in previous research.35, 36 However, consistent with the earlier study, our regression model found that probability of experiencing chronic illness and associated disabilities was highest among the lowest 2 wealth quintiles and in older age.35 The study also revealed that men are more likely to report chronic illness with associated disability than women, and the population from urban areas was more likely to experience associated disabilities. This might be explained by the variability of health behavior practices, as well as factors affecting the urban and rural areas. Our study findings suggest that further research would be necessary to understand the underlying reasons for these variations.
Our study showed that people with chronic illness prefer to seek care from public hospitals. Bangladesh is a LMIC, and most of the population is relatively poor; however, seeking care from a private hospital might be associated with a higher level of expenditures, such as consultation fees, the cost for bed/days, and costs for diagnostic tests. Therefore, most of the people with poor income status might not be able to afford care from the private hospital. However, the need for inpatient care might be associated with the high rate of public service utilization. Evidence from health system perspective also showed that the patients with chronic illness need more inpatient care.37 OOPP healthcare expenditure for any chronic illness was reported highest for people 40–64 years old and those with cancer and chronic heart disease, which is similar to the findings of studies conducted in Australia.10 However, all people with chronic illness had OOPP healthcare expenditure irrespective of economic status reflects the need for social and health protection schemes from aspect. Policy efforts need to focus on the elderly population particularly in lowest income quintiles with chronic illness to reduce OOPP healthcare expenditure and to relieve the economic burden of chronic disease.
This study analyzed the differences in OOPP healthcare expenditure between people with chronic illness with and without disability and found that chronic illness with a disability was associated with a significantly higher healthcare expenditure; females were more likely to have higher OOPP healthcare expenditure than males. Middle aged with disability spent significantly more than persons in other age groups. The highest 2 wealth quintile was associated with high OOPP healthcare expenditure, which is consistent with the findings of an earlier study that showed that people with relatively high income have a tendency to take better care and are more likely to report high OOPP healthcare expenditure.10 Our findings revealed that chronic illness itself is a burden for any household and causes increased expenditure on health services; this becomes higher when it is associated with disability, which forces persons to use more health services. As a consequence, the household has to spend more of its OOPP money on health care. In this study, higher overall OOPP healthcare expenditure for associated disability might be explained by the substantially higher levels of healthcare utilization, such as more use of both outpatient and inpatient services. These findings are consistent with those of previous studies that have identified a positive correlation between multi-morbidity with OOPP and the health care utilization.29, 38, 39, 40 Findings showed that chronic illness with associated disability is a significant determinant of OOPP expenditure, which may lead to the heavy financial burden for the households. For example, evidence from a Scottish study showed persons with multi-morbidity were six times more likely to have an unplanned hospital admission.41 This could be a result of more consultations, diagnostic tests, medications, and frequent hospitalization. Health care professionals treating people with chronic illness and associated disability need to be aware of these potential financial pressures while proposing treatments, and policy makers need to be aware of the growing pressures on both personal and government budgets.
Some limitations should be considered while interpreting the results of the study. Since the HIES data is cross-sectional in nature, there was limited opportunity to make inferences about the causal relationship between chronic illnesses with/without disability and other associated factors. Further, our findings are based on self-reported illness, utilization, and expenditure, which might cause recall bias. However, the relatively short recall period (last 30 days) of HIES strives to reduce this potential bias. Additionally, reliance on self-reported expenditure might be associated with measurement error.42 We evaluated the incidence and the associated OOPP expenditure of chronic illness and for at least one associated disability but did not take into account the multi-morbidity or the expenses associated with more than one disability. However, study findings can be generalized at the national level as the study gathered data from a nationally representative household income and expenditure survey.
Conclusions
The results demonstrated that chronic illness with associated disability imposes a financial burden on households, in particular for the low-income households. The OOPP healthcare expenditure for receiving care imposes intractable barriers to healthcare to some households. This illustrates the necessity of financial risk protection of healthcare expenditures in LMIC settings like Bangladesh and also express the urgency of accounting for chronic illness especially for persons with associated disability. Social and private health insurance can be experimented with, which can help to finance health services that are currently limited in Bangladesh. Furthermore, more attention needs to be directed toward the rural, and the elderly population with chronic illness with associated disability since their households is at the greatest risk of experiencing higher OOPP. Therefore, the government can take the effort to strengthen the healthcare system with appropriate settings for these patients to be managed and further optimize health programs to further protect the population with chronic illness.
Conflicts of interest
The authors declare that they have no conflicts of interests.
Authors' contributions
All authors contributed to the writing of the manuscript. All authors agree with the manuscript's results and conclusions. All authors have read, and confirm that they meet, ICMJE criteria for authorship. All authors have read and approved the final manuscript for publication.
Acknowledgments
International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b) gratefully acknowledges the donors who provide unrestricted support: Government of the People's Republic of Bangladesh; the Department of Foreign Affairs, Trade and Development (DFATD), Canada; Swedish International Development Cooperation Agency (Sida) and the Department for International Development, (UK Aid).
Edited by Wei-Zhu Liu
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Kankeu H.T., Saksena P., Xu K., Evans D.B. The financial burden from non-communicable diseases in low-and middle-income countries: a literature review. BMC Heal Res Policy Syst. 2013;11:31. doi: 10.1186/1478-4505-11-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2015 Mortality and Causes of Death Collaborators Global, regional, and national life expectancy, all-cause mortality, and cause-specifi c mortality for 249 causes of death, 1980 – 2015: a systematic analysis for the Global Burden of Disease Study 2015. 2016;388:1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO . 2011. Global Status Report on Non-communicable Diseases 2010.http://www.who.int/nmh/publications/ncd_report_full_en.pdf?ua=1 Geneva, Switzerland. Available at: [Google Scholar]
- 4.Islam A., Biswas T. Chronic non-communicable diseases and the healthcare system in Bangladesh: current status and way forward. Chronic Dis Int. 2014;1:1–6. [Google Scholar]
- 5.Plianbangchang S, Narain JP. Health situation in the South-East Asia Region: challenges for the next decade. WHO South East Asia J Public Health. http://www.searo.who.int/LinkFiles/SEAJPH_SEAJPH-1-1.pdf. Published 2012. [DOI] [PubMed]
- 6.Murray C.J.L., Lopez A.D. Estimating causes of death: new methods and global and regional application for 1990. In: Murray C.J.L., Lopez A.D., editors. Global Burden of Disease and Injury Series. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Harvard School of Public Health, on behalf of the World Health Organization and the World Bank; Boston: 1996. pp. 117–200. [Google Scholar]
- 7.Sousa R.M., Ferri C.P., Acosta D. Contribution of chronic diseases to disability in elderly people in countries with low and middle incomes: a 10/66 Dementia Research Group population-based survey. Lancet. 2009;374:1821–1830. doi: 10.1016/S0140-6736(09)61829-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bleich S.N., Koehlmoos T.L., Rashid M., Peters D.H., Anderson G. Noncommunicable chronic disease in Bangladesh: overview of existing programs and priorities going forward. Health Policy (New York) 2011;100:282–289. doi: 10.1016/j.healthpol.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karar Z.A., Alam N., Streatfield P.K. Epidemiological transition in rural Bangladesh, 1986-2006. Glob Health Action. 2009;2:1–9. doi: 10.3402/gha.v2i0.1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Islam M.M., Yen L., Valderas J.M., McRae I. Out-of-pocket expenditure by Australian seniors with chronic disease: the effect of specific diseases and morbidity clusters. BMC Public Health. 2014;14(1):1008. doi: 10.1186/1471-2458-14-1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yokota R.T., Van der Heyden J., Nusselder W.J. Impact of chronic conditions and multimorbidity on the disability burden in the older population in Belgium. J Gerontol A Biol Sci Med Sci. 2016;71:903–909. doi: 10.1093/gerona/glv234. [DOI] [PubMed] [Google Scholar]
- 12.Hwang W., Weller W., Ireys H., Anderson G. Out-of-pocket medical spending for care of chronic conditions. Health Aff. 2001;20:267–278. doi: 10.1377/hlthaff.20.6.267. [DOI] [PubMed] [Google Scholar]
- 13.Rahman M.M., Gilmour S., Saito E., Sultana P., Shibuya K. Health-related financial catastrophe, inequality and chronic illness in Bangladesh. PLoS One. 2013;8(2):e56873. doi: 10.1371/journal.pone.0056873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. WHO Global Health Expenditure Atlas. Geneva, Switzerland 2014. Available at: http://www.who.int/health-accounts/atlas2014.pdf.
- 15.MOHFW . Health Economics Unit, Ministry of Health and Family Welfare, Government of the People’s Republic of Bangladesh; Dhaka, Bangladesh: 2012. Expanding Social Protection for Health: Towards Universal Coverage, Health Care Financing Strategy 2012–2032. [Google Scholar]
- 16.Zhong W., Finnie D.M., Shah N.D. Effect of multiple chronic diseases on health care expenditures in childhood. J Prim Care Community Health. 2015;6:2–9. doi: 10.1177/2150131914540916. [DOI] [PubMed] [Google Scholar]
- 17.Tareque M.I., Begum S., Saito Y. Inequality in disability in Bangladesh. PLoS One. 2014;9:e103681. doi: 10.1371/journal.pone.0103681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Helmchen L.A., Lo Sasso A.T. How sensitive is physician performance to alternative compensation schedules? Evidence from a large network of primary care clinics. Health Econ. 2010;19(11):1300–1317. doi: 10.1002/hec.1551. [DOI] [PubMed] [Google Scholar]
- 19.Onoka C.A., Onwujekwe O.E., Hanson K., Uzochukwu B.S. Examining catastrophic health expenditures at variable thresholds using household consumption expenditure diaries. Trop Med Int Heal. 2011;16:1334–1341. doi: 10.1111/j.1365-3156.2011.02836.x. [DOI] [PubMed] [Google Scholar]
- 20.Wang Q., Fu A.Z., Brenner S., Kalmus O., Banda H.T., De Allegri M. Out-of-pocket expenditure on chronic non-communicable diseases in Sub-Saharan Africa: the case of Rural Malawi. PLoS One. 2015;10(1):e0116897. doi: 10.1371/journal.pone.0116897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brinda E.M., Kowal P., Attermann J., Enemark U. Health service use, out-of-pocket payments and catastrophic health expenditure among older people in India: the WHO Study on global AGEing and adult health (SAGE) J Epidemiol Community Health. 2015;69:489–494. doi: 10.1136/jech-2014-204960. [DOI] [PubMed] [Google Scholar]
- 22.Van Doorslaer E., O'Donnell O., Rannan-Eliya R.P. Effect of payments for health care on poverty estimates in 11 countries in Asia: an analysis of household survey data. Lancet. 2006;368:1357–1364. doi: 10.1016/S0140-6736(06)69560-3. [DOI] [PubMed] [Google Scholar]
- 23.Van Doorslaer E., O'Donnell O., Rannan-Eliya R.P. Catastrophic payments for health care in Asia. Health Econ. 2007;16:1159–1184. doi: 10.1002/hec.1209. [DOI] [PubMed] [Google Scholar]
- 24.Wang Z., Li X., Chen M. Catastrophic health expenditures and its inequality in elderly households with chronic disease patients in China. Int J Equity Health. 2015;14:8. doi: 10.1186/s12939-015-0134-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.BBS (Bangladesh Bureau of Statistics) 2011. Bangladesh Household Income and Expenditure Survey 2010. Statistics Division, Ministry of Planning. Government of the People's Republic of Bangladesh: New Panama Printing Press. Available at: http://203.112.218.65/WebTestApplication/userfiles/Image/LatestReports/HIES-10.pdf. Accessed 20 January 2017. [Google Scholar]
- 26.Madans J.H., Loeb M.E., Altman B.M. Measuring disability and monitoring the UN Convention on the Rights of Persons with Disabilities: the work of the Washington Group on Disability Statistics. BMC Public Health. 2011;11(suppl 4):1–8. doi: 10.1186/1471-2458-11-S4-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tareque M.I., Begum S., Saito Y. Gender differences in disability-free life expectancy at old ages in Bangladesh. J Aging Health. 2013;25:1299–1312. doi: 10.1177/0898264313501388. [DOI] [PubMed] [Google Scholar]
- 28.Sarker A.R., Mahumud R.A., Sultana M., Ahmed S., Ahmed W., Khan J.A. The impact of age and sex on healthcare expenditure of households in Bangladesh. Springerplus. 2014,14;3:435. doi: 10.1186/2193-1801-3-435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pati S., Agrawal S., Swain S. Non communicable disease multimorbidity and associated health care utilization and expenditures in India: cross-sectional study. BMC Health Serv Res. 2014;14:451. doi: 10.1186/1472-6963-14-451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.WHO . 2014. Global Status Report on Noncommunicable Diseases 2014. Geneva, Switzerland. Available at: http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf. [Google Scholar]
- 31.Purty A.J., Bazroy J., Kar M., Vasudevan K., Veliath A.P.P. Morbidity pattern among the elderly population in the Rural Area of Tamilnadu, India. Turk Jr Med Sci. 2006;36:45–50. [Google Scholar]
- 32.Joshi K., Kumar R., Avasthi A. Morbidity profile and its relationship with disability and pyschological distress among elderly people in Northern India. Int J Epidemiol. 2003;32:978–987. doi: 10.1093/ije/dyg204. [DOI] [PubMed] [Google Scholar]
- 33.Britt H.C., Harrison C.M., Miller G.C., Knox S.A. Prevalence and patterns of multimorbidity in Australia. Med J Aust. 2008;189:72–77. doi: 10.5694/j.1326-5377.2008.tb01919.x. [DOI] [PubMed] [Google Scholar]
- 34.Lee J.T., Hamid F., Pati S., Atun R., Millett C. Impact of noncommunicable disease multimorbidity on healthcare utilisation and out-of-pocket expenditures in middle-income countries: cross sectional analysis. PLoS One. 2015;10:e0127199. doi: 10.1371/journal.pone.0127199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Basu S., King A.C. Disability and chronic disease among older adults in India: detecting vulnerable populations through the WHO SAGE Study. Am J Epidemiol. 2013;178:1620–1628. doi: 10.1093/aje/kwt191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stuckler D., Siegel K. Oxford University Press; Oxford: 2013. Sick Societies: Responding to the Global Challenge of Chronic Disease. [Google Scholar]
- 37.Nolte E.E., McKee M. Caring for people with chronic conditions: a health system perspective. Int J Integr Care. 2009;9:e08. [Google Scholar]
- 38.Schäfer I., Hansen H., Schön G. The influence of age, gender and socio-economic status on multimorbidity patterns in primary care. first results from the multicare cohort study. BMC Health Serv Res. 2012;12:89. doi: 10.1186/1472-6963-12-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Glynn L.G., Valderas J.M., Healy P. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Fam Pract. 2011;28:516–523. doi: 10.1093/fampra/cmr013. [DOI] [PubMed] [Google Scholar]
- 40.Huntley A.L., Johnson R., Purdy S., Valderas J.M., Salisbury C. Measures of multimorbidity and morbidity burden for use in primary care and commu-nity settings: a systematic review and guide. Ann Fam Med. 2012;10:134–141. doi: 10.1370/afm.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mbchb R.A.P., Abel G.A., Mbbchir B.G., Mbchb S.W.M. Admissions to hospital: a retrospective cohort study. 2013;185(5):1–8. doi: 10.1503/cmaj.121349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Murphy A., Mahal A., Richardson E., Moran A.E. The economic burden of chronic disease care faced by households in Ukraine: a cross-sectional matching study of angina patients. Int J Equity Health. 2013;12:38. doi: 10.1186/1475-9276-12-38. [DOI] [PMC free article] [PubMed] [Google Scholar]