Abstract
The metabolic syndrome (MS) is a multi-factorial disorder which includes a main risk factors associated with the development of cardiovascular, neurologic, renal and endocrine diseases, especially type 2 diabetes. This study has been conducted to estimate the prevalence of the MS in patients undergoing continuous ambulatory peritoneal dialysis (CAPD) and its association with cardiovascular morbidity. The study included 37 patients (25 type 2 diabetic patients and 12 non-diabetic patients), who had been on peritoneal dialysis for > 3 months. At the beginning of CAPD treatment (baseline) and at the end of follow-up, we measured: body mass index (BMI), blood pressure, fasting blood glucose, triglycerides and high-density lipoprotein cholesterol (HDLC) and defined the prevalence of the MS using the modified National Cholesterol Education Program (NCEP; Adult Treatment Panel III) for peritoneal dialysis patients. The overall prevalence of the MS was 89,2%. The metabolic syndrome was estimated in all (100%) type 2 diabetic patients (vs. 60% patients on the beginning of CAPD treatment). In non-diabetic peritoneal patients, the MS was estimated in 50% cases, according to 33,3% at the beginning CAPD treatment. Development of the MS was significantly higher in the type 2 diabetic patients in compared with non-diabetic patients until the end of follow-up examination (p=0,0005). The prevalence of LVH in type 2 diabetic patients with the MS was significantly higher (p=0,002) than in non-diabetic peritoneal patients with the MS. We didn’t found statistical significantly difference in the prevalence of ischemic heart disease between this two category of peritoneal dialysis patients (p=0,076). The results indicate that the metabolic syndrome is presented in high percentage in peritoneal dialysis patients, and it’s also important risk factor of high cardiovascular morbidity rate in these patients, especially in type 2 diabetic patients.
Keywords: peritoneal dialysis, metabolic syndrome, cardiovascular morbidity
INTRODUCTION
The metabolic syndrome (MS) is rapidly becoming a primary cause of morbidity and mortality in the general population (1). This syndrome is characterized by the variable coexistence of hyperinsulinemia, obesity, dyslipidemia, hyperglycemia and hypertension. Other conditions associated with the syndrome include microalbuminuria, inflammation, a protrombotic state and fatty liver. Subjects with the metabolic syndrome are, at essentially, with double risk to develop cardiovascular disease compared with those without the syndrome (2). It further raises the risk for type 2 diabetes by about 5-fold (3). Cardiovascular morbidity and mortality are common in peritoneal dialysis patients. The prevalence of the MS in peritoneal dialysis patients is a subject of recent studies (4,5). Although, some of the MS component are strongly associated with cardiovascular morbidity and mortality (6,7), association of the metabolic syndrome with cardiovascular morbidity and mortality in peritoneal dialysis patients is nor clearly establishment. Aim of this study was to estimate the prevalence of the MS in patients undergoing continuous ambulatory peritoneal dialysis (CAPD) and its association with cardiovascular morbidity.
MATERIALS AND METHODS
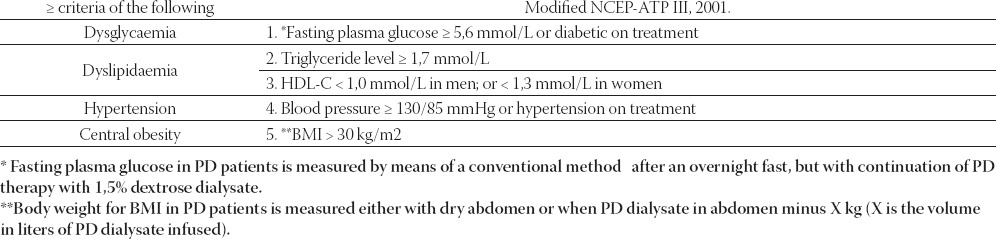
The study included 37 patients, which had been on peritoneal dialysis for more than 3 months. Twenty five patients were type 2 diabetic patients aged 46-64 years and 12 non-diabetic patients aged 30-65 years. At the beginning of CAPD treatment (baseline) and at the end of follow-up, we measured: body mass index (BMI), blood pressure, fasting blood glucose, triglycerides and high-density lipoprotein cholesterol (HDL-C) due to defined the prevalence of the MS and its associated with cardiovascular morbidity. The definition of the MS is based on the co-occurrence of the three or more risk factors using the Modified National Cholesterol Education Program (NCEP; Adult Treatment Panel III) for peritoneal dialysis patients (8), (Table 1). Left ventricular hypertrophy (LVH) was estimated by echocardiography examination. Left ventricle hypertrophy was defined by a left ventricular mass index (LVMI) of over 131 g/m2 in man or >100 g/m2 in a woman according to recommendations of the American Society of Echocardiography. Ischemic heart disease was determinated by electrocardiographic examination, antecedents of angina or myocardial infarction.
TABLE 1.
Diagnostic criteria of the metabolic syndrome in peritoneal dialysis patients
Statistical analysis
Categorial data were presented as percentages. Differences in categorial data were compared with the chisquare (χ2) test. The p-value < 0,05 was considered significant.
RESULTS
At the beginning of peritoneal dialysis treatment, 10 of 25 type 2 diabetic patients (40%) didn’t have any elements of the MS. Six (12%) patients in this group had 3 risk factors, 8 patients were with 4 risk factors (32%), and one of them (4%) had all of five risk factors of the MS (Table 2). In non-diabetic patients group 66,7% cases had no criteria of the MS at the beginning of peritoneal dialysis treatment. It was not determined the significant difference in presence of the MS comparing that two groups of patients at the beginning of CAPD treatment (χ2=2,308, p=0,315). At the end of follow-up, the metabolic syndrome was estimated in all type 2 diabetic patients (100%). In the same group 52% patients had five risk factors, 36% patients had four risk factors and only 12% patients had three risk factors of the MS. The prevalence of the MS in type 2 diabetic patients undergoing peritoneal dialysis was significantly higher than at the beginning of renal replacement therapy (χ2=12,5; p=0,001).
TABLE 2.
Distribution of the metabolic syndrome in peritoneal dialysis patients
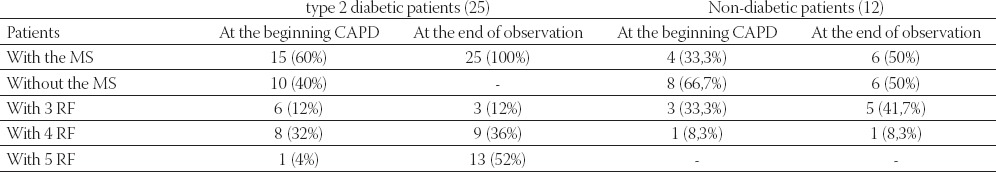
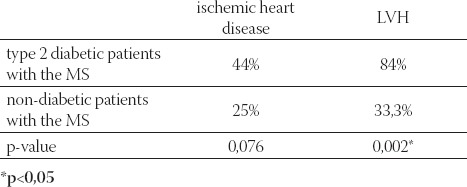
At the end of follow-up, the MS was estimated in 50% of non-diabetic peritoneal patients, more of them with three risk factors (41,7%). Significant difference in the prevalence of the MS in this category of peritoneal dialysis patients was not found between beginning and follow-up period (χ2=0,686, p=0,709). Development of the MS was significantly higher in the type 2 diabetic patients compared with non-diabetic patients until the end of follow-up examination (χ2=14,919, p=0,0005), (Table 3). The overall prevalence of the MS in peritoneal dialysis patients was 89,2%. Ischemic heart disease was manifested in 14/25 (44%) type 2 diabetic patients with the MS presenting with 4-5 risk factors. Blood pressure elevation (90,3%) and blood glucose abnormalities (87,1%) were the most frequent, while lower value of HDL-C was the least frequent component (58,1%). The prevalence of LVH was 84% (21/25) in the group of type 2 diabetic patients with the MS. All cardiovascular mortality was 16% in the same group of patients. In non-diabetic peritoneal patients with the MS, ischemic heart disease was presented in 25% patients, LVH in 33,3% patients, while 41,7% patients didn’t have electrocardiographic and echocardiographic changes. The prevalence of LVH in type 2 diabetic patients with the MS was significantly higher (p=0,002) than in non-diabetic peritoneal patients with the MS (Table 4). There was no difference in the prevalence of ischemic heart disease between this two category of peritoneal dialysis patients (p=0,076).
TABLE 3.
The metabolic syndrome in peritoneal dialysis patients
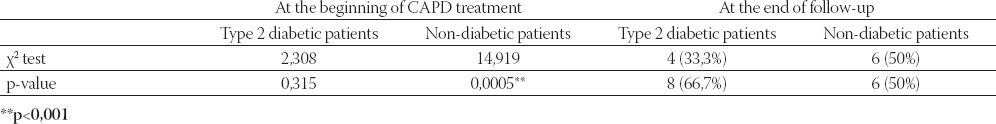
TABLE 4.
The prevalence of cardiovascular diseases in peritoneal dialysis patients
DISCUSSION
The metabolic syndrome represents a clustering of metabolic risk factors for development of cardiovascular disease. The available evidence indicates that between 15 to 25% of the world’s general population have features of metabolic syndrome (9). Because of this relatively high prevalence, the metabolic syndrome accounts for an increasing proportion of cardiovascular risk worldwide. Despite its high prevalence, little is known of the prospective association of the metabolic syndrome with cardiovascular morbidity and mortality in peritoneal dialysis patients. Chronic ambulatory peritoneal dialysis is associated with a number of metabolic abnormalities. These include lipid abnormalities, especially hypertriglyceridemia, carbohydrate abnormalities resulting of the large glucose absorption from peritoneal dialysate, protein depletion, obesity etc. (10). Although some of these metabolic abnormalities are separately strong cardiovascular risk factor, links among different conditions and components appear to be an independent and aggravating risk factor for cardiovascular diseases. The dialysis population has a much higher risk of cardiovascular mortality compared with the general population (11). The patients with chronic kidney disease stages 4 and 5 with the metabolic syndrome have a significantly higher risk mortality compared to those without the metabolic syndrome (12). In a study by a Johnson’s group (12), the prevalence of the MS was highest among those on peritoneal dialysis (50%). Patients on peritoneal dialysis compared with those on haemodialysis might be more at risk for the MS due to impaired glucose regulation. It is known that peritoneal dialysis solutions contain large quantities of glucose and 6-8% of the glucose installed into the peritoneal cavity is absorbed, corresponding to 100-300 g of glucose per day (13). That should be alert to the development of the MS among patients undergoing peritoneal dialysis. Young et al. (14) examined the prevalence of the MS at the time of renal replacement therapy initiation in a group of 202 incident dialysis patients (94% haemodialysis and 6% peritoneal dialysis) using NCEP criteria and found that the overall prevalence of the MS was 69,3% in that population. Another recent study showed the prevalence of the MS of 53,3% among cohort of 212 peritoneal dialysis patients (15). The prevalence of the MS in our study was highly 89,2%. At the beginning of continuous ambulatory peritoneal dialysis treatment, the prevalence of the MS was higher in type 2 diabetic patients than in non-diabetic peritoneal patients, but without significant difference (p=0,315). During to follow-up, the MS has been noted significantly more in the type 2 diabetic patients than in non-diabetic patients (p=0,0005). The results of a large number of cross-sectional and longitudinal studies confirmed the unfavorable impact of the metabolic syndrome on cardiovascular risk profile and associated of the metabolic syndrome with an increased risk of cardiovascular disease and death in general population (16, 17). Kwan et al. found that the 8-year cardiovascular survival for patients on peritoneal dialysis with and without the metabolic syndrome was 64% and 73,8% (15). A considerable number of studies have demonstrated that modifications of the left ventricular structure take place in a considerable proportion of patients with the metabolic syndrome (18). We found that 84% of type 2 diabetic peritoneal dialysis patients with the MS and 33,3% of non-diabetic peritoneal dialysis patients with the MS showed left ventricular hypertrophy. The prevalence of LVH was significantly higher in type 2 diabetic patients with the MS (p=0,002). This finding emphasizes that the metabolic syndrome in peritoneal dialysis patients is important factor for the development or progression of cardiac organ damage. The increased cardiovascular risk profile of the metabolic syndrome might be interplayed between metabolic factors (such as hyperglycemia, hyperinsulinaemia) and other non-metabolic factors (haemodynamic and non-haemodynamic). Ischemic heart disease was found in 44% of type 2 diabetic peritoneal dialysis patients with the MS and 25% of non-diabetic peritoneal dialysis patients with the MS, but without significantly difference (p=0,076). Therefore, there is a strong reason for intensive risk factor modification of the metabolic syndrome in peritoneal dialysis patients and intervention programme for multiple risk factors.
CONCLUSION
- The metabolic syndrome is common in peritoneal dialysis patients with the prevalence of 89,2%.
- The prevalence of the metabolic syndrome significantly increases in type 2 diabetic patients undergoing CAPD treatment.
- Left ventricular remodeling is much higher in type 2 diabetic patients with the metabolic syndrome undergoing peritoneal dialysis than in non-diabetic peritoneal dialysis patients.
- The metabolic syndrome has important contribution to the risk of high cardiovascular morbidity rate in these patients.
REFERENCES
- 1.Wilkin TJ, Voss L.D. Metabolic syndrome: Maladaptation to a modern world. J. R. So.c Med. 2004;97(11):511–520. doi: 10.1258/jrsm.97.11.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grundy S.M. Metabolic syndrome pandemic. Arterioscler. Thromb. Vasc. Biol. 2008;86:629–636. doi: 10.1161/ATVBAHA.107.151092. [DOI] [PubMed] [Google Scholar]
- 3.Malik S, Wong N.D. Metabolic syndrome, cardiovascular risk and screening for subclinical atherosclerosis. Expert Res. Cardiovasc. Ther. 2009;7(3):272–280. doi: 10.1586/14779072.7.3.273. [DOI] [PubMed] [Google Scholar]
- 4.Li P.K.-T, Kwan B.C.-H, Szeto C.C, Ko G.T.-C. Metabolic syndrome in peritoneal dialysis patients. Nephrol. Dial. Transplant. 2008;1(4):206–214. doi: 10.1093/ndtplus/sfn073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McDonald S.P, Collins J.F, Johnsson D.W. Obesity is associated with worse peritoneal dialysis outcomes in the Australia and New Zealand Patients populations. J. Am. Soc. Nephrol. 2003;14:2894–2901. doi: 10.1097/01.asn.0000091587.55159.5f. [DOI] [PubMed] [Google Scholar]
- 6.Peterson G.E, de Backer T, Gabriel A, Ilic V, Vagaonescu T, Appel L.J, Contreras G, Kendrick C, Rostand S, Phillips R.A. African American Study of Kidney Disease Investigators. Prevalence and correlates of left ventricular hypertrophy in the African American Study of Kidney Disease Cohort Study. Hypertension. 2007;50:1033–1039. doi: 10.1161/HYPERTENSIONAHA.107.090613. [DOI] [PubMed] [Google Scholar]
- 7.Bestermann W, Houston M.C, Basile J, Egan B, Ferrario C.M, Lackland D, Hawkins R.G, Reed J, Rogers P, Wise D, Moore M.A. Addressing the global cardiovascular risk of hypertensive, dislipidemia, diabetes mellitus and the metabolic syndrome in the southeastern United States. Am. J. Med. Sci. 2005;329:292–305. doi: 10.1097/00000441-200506000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Park S.H, Lindholm B. Definition of metabolic syndrome in peritoneal dialysis. Perit. Dial. Int. 2009;29(Suppl 2):S137–S144. [PubMed] [Google Scholar]
- 9.Eckel R.H, Grundy S.M, Zimmet P.Z. The metabolic syndrome. Lancet. 2005;365:1415–1428. doi: 10.1016/S0140-6736(05)66378-7. [DOI] [PubMed] [Google Scholar]
- 10.Morrison G. Metabolic effects of continuous ambulatory peritoneal dialysis. Ann. Rev. Med. 1989;40:163–172. doi: 10.1146/annurev.me.40.020189.001115. [DOI] [PubMed] [Google Scholar]
- 11.i P.K, Chow K.M. The clinical and epidemiological aspects of vascular mortality in chronic peritoneal dialysis patients. Perit. Dial. Int. 2005;25(Suppl 3):S112–S119. [PubMed] [Google Scholar]
- 12.Johnson D.W, Armstrong K, Campbell S.B, Mudge D.W, Hawley C.M, Coombes J.S, Prins J.B, Isbel N.M. Metabolic syndrome in severe chronic kidney disease: prevalence, predictors, prognostic significance and effects of risk factors modification. Nephrology (Carlton) 2007;12:391–398. doi: 10.1111/j.1440-1797.2007.00804.x. [DOI] [PubMed] [Google Scholar]
- 13.Holmes C.J, Shockley T.R. Strategies to reduce glucose exposure in peritoneal dialysis patients. Perit. Dial. Int. 2000;20(Suppl 2):S37–S41. [PubMed] [Google Scholar]
- 14.Young D.O, Lund R.J, Haynatzki G, Dunlay R.W. Prevalence of the metabolic syndrome in an incident dialysis population. Hemodial. Int. 2007;11:86–95. doi: 10.1111/j.1542-4758.2007.00158.x. [DOI] [PubMed] [Google Scholar]
- 15.Kwan B.C, Szeto C, Ckow 1С, Leung C, Li P.K. Metabolic syndrome and cardiovascular mortality in Chinese PD patients. Abstracts from the 12th Congress of the International Society for Peritoneal Dialysis, Istanbul 2008. Peritoneal Dialysis International. 2008;28(Suppl 4):560. [Google Scholar]
- 16.Lindsay R.S, Howard B.V. Cardiovascular risk associated with the metabolic syndrome. Curr. Diab. Rep. 2004;4:63–68. doi: 10.1007/s11892-004-0013-9. [DOI] [PubMed] [Google Scholar]
- 17.Dekker J.M, Girman C, Rhodes T, Nijpels G, Stehouher C.D, Bouter L.M, Heine R.J. Metabolic syndrome and 10-year cardiovascular disease risk in the Hoorn Study. Circulation. 2005;112:666–673. doi: 10.1161/CIRCULATIONAHA.104.516948. [DOI] [PubMed] [Google Scholar]
- 18.Chinali M, Devereux R.B, Howard B.V, Roman M.J, Bella J.N, Liu J.E, Resnick H.E, Lee E.T, Best L.G, de Simone G. Comparison of cardiac structure and function in American Indians with and without the metabolic syndrome (the Strong Heart Study) Am. J. Cardiol. 2004;93:40–41. doi: 10.1016/j.amjcard.2003.09.009. [DOI] [PubMed] [Google Scholar]


