Abstract
Cardiovascular diseases (CVD) are a major cause of morbidity and leading cause of mortality in almost 50% of patients (pts) with chronic kidney disease (CKD), including kidney transplant recipients. Left ventricular hypertrophy (LVH) is the most common structural alteration and powerful risk factor for cardiovascular complications in the uremic patients.
The aim of this study is to analyze predictors of the left ventricular remodelling in the first year after kidney transplantation based on comparison of echocardiographic findings, which had been done before and twelve months after transplantation. In five years retrospective study, we followed up 30 kidney transplant patients in the first post-transplant year. All patients data - blood pressure, BMI, ECG, blood haemoglobin, serum protein, calcium, phosphorus, product of calcium and phosphorus, the values of parathyroid hormone, serum creatinine and creatinine clearance were recorded just before kidney transplantation and in one month interval after transplantation in the first post-transplant year. Echocardiographic examination was done before transplantation and one year after kidney transplantation.
Before transplantation, 33% of patients had normal echocardiographic finding and 67% of patients had echocardiographic signs of left ventricular hypertrophy. After first post-transplant year, 63% of patients showed normal echocardiographic finding of LV, while 37% of patients remained with LV hypertrophy. Diastolic dysfunction of LV until the end of study had been reduced in 40% of pts compared to 70% pts at the beginning of the study. The positive echocardiographic remodelling of LV significantly correlated with rising values of haemoglobin (p<0,05), creatinine clearance (p=0,039) and with the reduction of the serum creatinine values (p=0,047), as well as values of parathyroid hormone (p=0,022). These results confirmed positive relationship between echocardiographic remodelling of left ventricular hypertrophy and elimination uraemia-related risk factors after successful renal transplantation.
Keywords: kidney transplantation, left ventricular remodelling, echocardiography
INTRODUCTION
Uraemic cardiomyopathy, defined as left ventricular hypertrophy (LVH), left ventricular dilatation or left ventricular systolic dysfunction, is reported to be a predictor of cardiovascular morbidity and mortality in patients with end-stage of renal disease. Left ventricular hypertrophy, as an adaptive response to volume and pressure overload, remains the prevalent form of cardiomyopathy in the patients with end-stage renal disease, including renal transplant patients (50-70%) (1,2).
Cardiovascular disease is major limitation of life expectancy of renal transplant recipients. A large number of traditional and non-traditional uraemia related risk factors independently predict the risk of cardiovascular outcome, even among the patients with less degrees of renal failure (3). The certain interplay between kidney and cardiovascular disease suggests synergistic effect whereby advancing kidney failure promotes cardiovascular complications and vice versa in bi-direction relationship. Some recently published studies emphasize that the identification of modifiable cardiovascular risk factors may enable reduction risk of cardiovascular morbidity in renal transplant recipient also (4).
We hypothesized that some risk factors could independently predict the course and outcome of left ventricular remodelling in the first post-transplant year. The objective of this study was to determine the prevalence of LVH and prognostic impact of follow-up risk factors on LV remodelling in the first year after transplantation. Investigation was made by the comparison of echocardiographic findings made before and twelve months after transplantation.
MATERIALS AND METHODS
The five years retrospective clinical study on left ventricular remodelling in renal transplant patients in the first post-transplant year and the influence of risk factors was undertaken at Clinic of Nephrology, Clinical Centre University of Sarajevo. We followed up 30 patients (pts) with renal allograft in the first post-transplant year. Two of them received cadaveric and 28 living related kidney grafts. Gender and age ratio was 19 males with mean age 37,8±19,9 years vs. 11 females with mean age 35,5±11 years. All evaluated patients were on haemodialysis treatment before renal transplantation / males with average duration of 27 months and females with average duration of 36 months. Following patients were excluded from the study: ones with acute renal rejection, chronic allograft nephropathy with progressively decreased renal function in the first three post-transplant months, ones with heart failure and older than 55 years. All patients data were recorded just before kidney transplantation and in one month interval after transplantation in the first post-transplant year and included control of blood pressure, BMI, ECG, blood haemoglobin, serum protein, calcium, phosphorus, product of calcium and phosphorus, the values of parathyroid hormone, serum creatinine and creatinine clearance. Echocardiographic examination was done just before transplantation and one year after kidney transplantation at Clinic of cardiology, Clinical Centre University of Sarajevo. Ehocardiographic analysis was performed by use of M mod, two-dimensional and pulse Doppler apparatus. The criterion accepted for left ventricular hypertrophy was left ventricular mass index (LVMI) for males >131 g/m2, and for females LVMI>100g/m2. Systolic left ventricular function was estimated by ejection function (EF), and systolic dysfunction was defined as EF < 50%. Left ventricular diastolic dysfunction was defined as E/A (relationship between early and late atrial phase of rapid left ventricular filling) <1,0. The same immunosuppressants/cyclosporine, mycophenolate mofetil, prednisone/for all patients were given by accepted protocol and shown non toxic effects of the drugs during follow up. All patients where with controllable blood pressure during evaluated period.
Statistical analysis
The data were analyzed by using the descriptive statistics for each parameter that was followed up. Student’s t-test was used to compare arithmetic means of numeric variables of each parameter, with the acceptance of statistical significance at the level of p<0,05. Logistical regression was used to test the independent relationship between left ventricular mass index and potential predictors: blood haemoglobin, serum protein, calcium, phosphorus, product of calcium and phosphorus, the values of parathyroid hormone, serum creatinine and creatinine clearance.
RESULTS
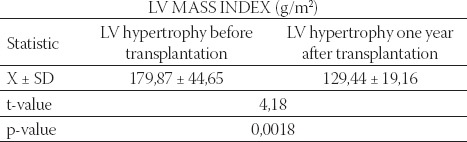
Before kidney transplantation, in the group of all patients, 10 of them (33%) showed normal echocardiographic findings and 67% of patients had echocardiographic signs of left ventricular hypertrophy. Among patients with LVH, 47% (14 pts) of them had concentric and 20% had eccentric LV hypertrophy. In the beginning of the study 20% of patients had normal function of left ventricle, while 80% had left ventricular dysfunction, out of which 70% had diastolic and 10% had systolic-diastolic LV dysfunction. All patients with normal mass index in the beginning of this study remained with normal LV mass index until the end of this study, while nine of twenty patients (9/20) with LVH in the beginning had reached normal echocardiography finding at the end of the study. Patients with left ventricular hypertrophy in the end of the study had significantly lower LV mass index compared with the start values (p=0,0018), as it is shown in Table 1.
TABLE 1.
Left ventricular mass index in the group with LVH at the beginning and at the end of the study
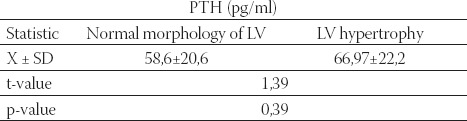
Normal function at the end of this study had been observed in 57% of patients. Diastolic dysfunction of LV until the end of study had been reduced in 40% of patients compared to 70% at the beginning of the study. Before kidney transplantation, renal anaemia was detected in the both tested groups (Table 2). The group with normal LV mass index had significantly higher values of haemoglobin compared with LV hypertrophy group (96,4 ±11,74 vs. 86,97±13,18, p=0,019). By the end of the first post-transplant year mean level of haemoglobin was increased evidently for 32% in group with normal mass index (Hgb 137,14±16,6 g/L) and for 35% in group with LV hypertrophy (Hgb 128,55±9,033 g/L). At the end of this study the value of parathormon was lower for 12,5% in the group of patients with normal LV mass compared to the group with LV hypertrophy (Table 3). In respect of LV functional status, significantly higher values of PTH were detected in the group of patients with diastolic dysfunction compared to the patients with normal LV function (p=0,029). Our results did not show any significant difference in average Ca x P product between the two tested groups.
TABLE 2.
Inter group relationship between mean values of haemoglobin compared to morphology status of LV before transplantation
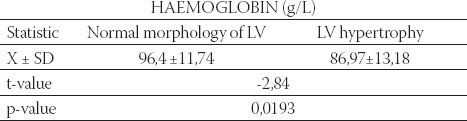
TABLE 3.
Inter group relationship between mean values of parathyroid hormone compared to morphology status of LV at the end of follow up
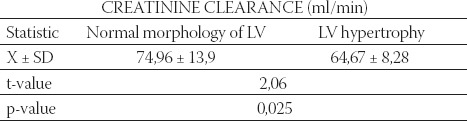
At the end of the first post-transplant year, the group with normal morphology of LV reached higher values of creatinine clearance (74,96 ± 13,9) compared to LV hypertrophy group (64,67 ± 8,28), p=0,025. The group of patients with normal LV function had significantly higher creatinine clearance (p=0,015) compared to the group of patients with diastolic dysfunction of LV (76,4 ml/min ±13,3 vs. 63,4 ml/min±13,9), Table 4.
TABLE 4.
Inter-group relationship between mean value of creatinine clearance and morphological status of LV at the end of follow up
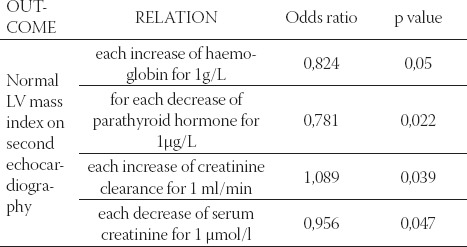
The logistical regression showed that positive echocardiographic remodelling of LV on second echocardiography significantly correlated with rising values of haemoglobin (p<0,05), increased values of creatinine clearance (p=0,039), decreased values of serum creatinine (p=0,047), and decreased values of parathyroid hormone (p=0,02), as it is shown in Table 5.
TABLE 5.
Predictors’ presence of normal LV appearance on follow up echocardiography
DISCUSSION
Cardiovascular disease is reported to be a predictor of premature mortality in patients with end-stage renal disease, with mortality rate 10-20 times higher than in a general population (5,6). Renal transplanted patients compared to patients undergoing dialysis have improved survival, but cardiovascular mortality remains twice higher than in a general population (7). Cardiovascular diseases in renal transplant patients are related to both traditional and non-traditional risk factors (like anaemia, hypertension, LVH, diabetes mellitus, dyslipidaemia, homocysteine, advanced glycosylation end-products), including the others specific factors for transplant patients such as effects of renal allograft dysfunction and effects of immunosuppressive drugs (8). Left ventricular hypertrophy is a major and independent risk factor for cardiovascular morbidity and mortality. Each of LV abnormalities, such as LV hypertrophy, LV dilatation, LV systolic dysfunction, cumulatively gives worse prognosis. LVH diagnosis has been assessed conventionally by echocardiography, as clinical tool and gold standard for non-invasive and reproducible method of examination. Previous studies have suggested that the echocardiographic prevalence of LVH among dialysis patients is 50 - 90%, with left ventricular dilatation in 20-40%, and systolic dysfunction in 16% of patients (9,10). Before renal transplantation LVH was common alteration among our patients (67%). In respect of left ventricular functional status, only 20% of patients had normal LV function, while diastolic dysfunction was predominant finding in 70% of patients. Until the end of the first post-transplant year normal finding of LV had been observed in 63% of patients compared with 33% at the start. Left ventricular hypertrophy remained in 37% of patients at the end of the study, with LV mass index significantly lower compared to the start values (129,44 v.s.179,87, p=0,0018). One year after transplantation, the reduction of diastolic dysfunction was significant (40%pts v.s.70% on the start, p=0,015). Hernandez et al (2) reported that regression of left ventricular hypertrophy partially starts at the first year after transplantation, is raised up to maximum value between two years, persists between third and forth year, while long evaluations of this findings are still unknown. Anaemia occurs early in patients with chronical renal disease. It is considered as an independent risk factor for progression to renal replacement therapy and cardiovascular complications such as cardiac enlargement, LVH, congestive heart failure as well as an ischemic heart disease. The prevalence of anaemia was not only specific to advanced renal disease, but also to relatively early stage of kidney disease where 25% of patients were anaemic (11). Levin and the other researchers (12) notified that anaemia also contributed to the development of LVH and chronic heart failure for each of 0,5 g/dl decrease in Hgb concentration. It was also independently associated with 32% increase in LV hypertrophy, i.e. an increase in LV mass. The results of our study show that renal anaemia was detected in all patients before transplantation. Compared with LV morphology status, patients with normal LV before transplantation had significantly higher serum haemoglobin values compared to the patients with LVH (p=0,019). Until the end of the first post-transplant year mean level of haemoglobin was increased significantly in a group with normal mass index for 32% (96,4±11,74 vs.137,14±16,6 g/L), while in a group with LV hypertrophy was for 35% (86,97±13,18 vs.128,55 ± 9,033 g/L). Secondary hyperparathyroidism is linked to renal dysfunction, as an important condition associated with cardiovascular disease, especially with LVH. Clinical studies have confirmed experimental observation that parathyroid hormone has important role in the activation and proliferation of cardiac interstitial cells and in the genesis of cardiac fibrosis (13). At the beginning of our study parathyroid hormone values were statistically higher in the group of patients with LV hypertrophy (p=0,033). Until the end of the study the value of parathormon had been reduced in both groups, and it was 12,5% lower in the group of patients with normal LV mass. In respect of LV functional status, significantly higher value of PTH was detected in group of patients with diastolic dysfunction compared to the patients with normal LV function (p=0,029). Our results did not show any significant difference in average Ca x P product between the two tested patient groups. It has been confirmed that the high values of phosphorus, CaxP product and PTH are associated with increased risk of death. A possible mechanism could be cardiac calcifications and subsequent coronary disease (13). The renal function is measured by absolute values of serum creatinine and creatinine clearance. Epidemio- logical studies shown that about 60% of renal transplant patients had GFR lower than 60/ml and about 15% of patients <30/ml/min (14). The results of our study showed that patient with LV hypertrophy before kidney transplantation had significantly higher serum creatinine values compared to patients with normal LV (p=0,023). At the end of this study patients with LV hypertrophy had significantly lower value of creatinine clearance than patients with normal LV mass index (p=0,025). Normalization of LV on follow up echocardiography significantly interplays with decrease in values of serum creatinine and increase in creatinine clearance. These findings are in the accordance with the results of other authors. Moreso and Grinyp (15) determined that renal allograft dysfunction is a strong risk factor for occurrence and development of cardiovascular complications.
CONCLUSION
The left ventricular hypertrophy is the most frequent cardiac abnormality in the time of kidney transplantation. One year after transplantation, the reduction of LVH and diastolic dysfunction were significant. Cardiovascular remodelling within the first year after successful renal transplantation is related to better kidney function, with correction of anaemia and control of hyperparathyroidism and can explain better outcomes of patients with renal transplant over the patients on long-term dialysis.
List of Abbreviations
LV - Left ventricle
LVH - Left ventricular hypertrophy
LVMI - Left ventricular mass index
EF - Ejection function
E/A - Diastolic function
cLVH - Concentric left ventricular hypertrophy
eLVH - Eccentric Left ventricular hypertrophy
NFLV - Normal function of left ventricle
DDLV - Diastolic dysfunction of left ventricle
SDDLV - Systolic-diastolic dysfunction of left ventricle
Hgb - Haemoglobin
PTH - Parathyroid hormone
REFERENCES
- 1.Sarnak M.J, Levey A.S, Schoolwerth A.C, et al. Kidney disease as a risk factor for development of cardiovascular disease. Circulation. 2003;108:2154–2169. doi: 10.1161/01.CIR.0000095676.90936.80. [DOI] [PubMed] [Google Scholar]
- 2.Hernandez D. Left ventricular hypertrophy after renal transplantation: new approach to a deadly disorder. Nephrol. Dial. Transplant. 2004;19:1682–1686. doi: 10.1093/ndt/gfh283. [DOI] [PubMed] [Google Scholar]
- 3.Baigent C, Landray M. Which cardiovascular risk factors matter in chronic kidney disease. Nephol. Dial. Trans. 2007;22:9–11. doi: 10.1093/ndt/gfl580. [DOI] [PubMed] [Google Scholar]
- 4.Dimeny E.M. Cardiovascular disease after renal transplantation. Kidney Int. 2002; 61:78–84. doi: 10.1046/j.1523-1755.61.s80.14.x. [DOI] [PubMed] [Google Scholar]
- 5.Mark P.B, Patel R.K, Jardine A.G. Are we overestimating left ventricular abnormalities in end stage renal disease? Nephrol. Dial. Transplant. 2007;22:1815–1819. doi: 10.1093/ndt/gfm224. [DOI] [PubMed] [Google Scholar]
- 6.London G.M. Cardiovascular disease in chronic renal failure, patophysiological aspect. Emm. Dial. 2003;16(2):85–94. doi: 10.1046/j.1525-139x.2003.16023.x. [DOI] [PubMed] [Google Scholar]
- 7.Weiner D.E, Sarnak M.J. Chronic Kidney Disease and Cardiovascular Disease: A Bi-Directional Relationship? Dial. Transplant. 2007;36(3):113–118. [Google Scholar]
- 8.Callaghan C.J, Bradley J.A. Current status of renal transplantation. Methods Mol. Biol. 2006;333:1–28. doi: 10.1385/1-59745-049-9:1. [DOI] [PubMed] [Google Scholar]
- 9.Rašić S, Kulenović I, Haračić A, Ćatović A. Left ventricular hypertrophy and risk factors for its development in uraemic patients. Bosn J. Basic Med. Sci. 2004;4(1):34–40. doi: 10.17305/bjbms.2004.3458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parashur A. The 2006 K/DOQI Anaemia Guidelines for CKD: Key Updates. Dialysis et Transplantation. 2006;35:632–634. [Google Scholar]
- 11.Levin A. The relationship of haemoglobin level and survival direct or indirect effects? Nephrol. Dial. Transplant. 2001;16(Suppl 2):7–11. doi: 10.1093/ndt/17.suppl_5.8. [DOI] [PubMed] [Google Scholar]
- 12.Amann K, Wiest G, Klaus G, Ritz E, Mall G. The role of parathyroid hormone in the genesis of interstitial cell activation in uraemia. J. Am. Soc. Nephrol. 1994;4:1814–1819. doi: 10.1681/ASN.V4101814. [DOI] [PubMed] [Google Scholar]
- 13.Lasic B.L, DeVita M.V, Michelis M.F. Coronary artery calcifications and bone pathology in haemodialysis patients with lower PTH levels. Dial. Transplant. 2005;34(12):845–850. [Google Scholar]
- 14.Gill J.S, Tonelli M, Mix C.H, Pereira B.J. The changes in allograft function among long-term kidney transplant recipients. J. Am. Soc. Nephrol. 2003;14:136–142. doi: 10.1097/01.asn.0000070621.06264.86. [DOI] [PubMed] [Google Scholar]
- 15.Moreso F, Grinyp J.M. Graft dysfunction and cardiovascular riskan unholy alliance. Nephrol. Dial. Transplant. 2007;22:699–702. doi: 10.1093/ndt/gfl657. [DOI] [PubMed] [Google Scholar]


