Abstract
Objective
To describe the proportion and characteristics of patients with late stage cancer that are and are not receptive to receiving rehabilitation services, as well as the rationale for their level of interest.
Setting
A comprehensive cancer center in a Northcentral US quaternary medical center
Design
A prospective mixed methods study
Participants
311 adults with Stage IIIC or IV non-small cell or extensive stage small cell lung cancer.
Interventions
Not applicable
Main Outcome Measures
Telephone acquired responses to the administration of: 1) the Activity Measure for Post Acute Care Computer Adaptive Test (AM-PAC-CAT); 2) Numerical rating scales for pain, dyspnea, fatigue, general emotional distress, and distress associated with functional limitations; 3) a query regarding receptivity to receipt of rehabilitation services, and 4) a query about rationale for non-receptivity.
Results
Overall 99 (31.8%) of the study’s 311 participants expressed interest in receiving rehabilitation services; 38 at the time of enrollment and an additional 61 during at least one subsequent contact. Participants expressing interest were more likely to have a child as primary caregiver (18.18% vs. 9.91%, p = 0.04) and a musculoskeletal comorbidity (42.4% vs. 31.6%, p = 0.05). Function-related distress was highly associated with receptivity, as were lower AM-PAC-CAT scores. Reasons provided for lack of interest in receiving services included a perception of their limited benefit, being too busy, and prioritization below more pressing tasks/concerns.
Conclusions
One-third of patients with late stage lung cancer are likely to be interested in receiving rehabilitation services despite high levels of disability and related distress. These findings suggest that patient misperception of the role of rehabilitation services may be a barrier to improved function and quality of life. Efforts to educate patients on the benefits of rehabilitation and to more formally integrate rehabilitation as part of comprehensive care may curb these missed opportunities.
The benefits of exercise and rehabilitation in improving the quality of life (QOL), function, and health of people with chronic diseases is well established and accepted by both the lay and medical communities.1,2 Although not as well appreciated, these benefits extend even to individuals with disease, including late stage cancer, with numerous studies finding that the initiation of an exercise program can lessen fatigue, dyspnea, and anxiety.3,4,5,6 The provision of rehabilitation services may also improve QOL and reduce healthcare utilization among patients with late stage cancer.7
Despite these findings, the use of exercise and rehabilitation services among chronically ill populations is far below the levels that would be the most beneficial for the individual as well as for society.8 This is particularly true in cancer where research shows that fewer than a third of remediable physical impairments are actually addressed with appropriate rehabilitation services and that the subject of exercise is rarely broached by oncological clinicians.9,10 This situation is likely to only worsen as current treatment trends indicate that cancer patients, in the future, will be older with higher levels of functional morbidity.11
Researchers have explored the reasons for low rates of exercise and rehabilitation service utilization among cancer populations. Some are systematic in nature and relate to the treating physician’s (in this case the oncologist’s) focus on disease assessment and treatment.12 Even when physical impairments are noted, there is seldom an easy way for their severity to be assessed or for the patient to be referred for appropriate rehabilitation services.13
The patient’s interest in receiving rehabilitation services is an important concern. Investigators have paid limited attention to this issue in cancer rehabilitation. However, low participation in cardiac and pulmonary rehabilitation programs, as well as adherence challenges in cancer exercise trials, suggest that the issue is not a trivial one.14,15 Qualitative work by our group demonstrated that patients have limited insight into the potential positive impact of therapeutic exercise on outcomes that they value.10 Though this work helped to elucidate patients’ beliefs about the utility of exercise in cancer, it was only a preliminary effort and did not examine their attitudes towards the broader interventions possible with rehabilitation services which extend well beyond exercise to encompass diverse modalities.
Our current lack of insight into patients’ willingness to utilize rehabilitation services is likely to contribute to the continued lack of emphasis on rehabilitation in comprehensive cancer care. To address this gap, we conducted a mixed methods study embedded within a longitudinal cohort study of patients with late stage lung cancer. The study aims included: 1) Estimating the proportion of patients with functional limitations and associated distress that were receptive to rehabilitation; 2) Identifying patient characteristics associated with receptivity to rehabilitation services; and, 3) Qualitatively describing why disabled and/or distressed patients were not interested in receiving rehabilitation services.
Methods
Subjects
A sample of 313 patients with Stage IIIB or IV non-small cell lung cancer (NSCLC) or extensive stage SCLC who were followed for two years as part of a longitudinal study on functional monitoring comprised the study sample. Recruitment, screening, and enrollment procedures have been previously described.16 All subjects were required to be fluent in English, able to converse on the telephone, and have an intact mental status (defined as a Folstein Mini-Mental examination score ≥ 25). Participants were consecutively enrolled regardless of cancer treatment status and followed until dropout, death, or study closure. The Mayo Clinic Institutional Review Board approved the study and participants provided verbal informed consent.
Data collection
Participant demographics and cancer-related information were abstracted from medical records, including data to calculate Charlson comorbidity indices.17 Patient reported outcome (PRO) data were collected every 3–4 weeks via telephone by one of four research assistants or the principal investigator (AC). Subsequent contacts were initiated 21 days after a previous contact with daily attempts at different times of the day for two weeks. All interviews were scripted, and the PRO instruments were administered in a fixed order: 1) Activity Measure for Post-Acute Care Basic Mobility Computer Adaptive Test (AM-PAC CAT), 2) Symptom numerical rating scales (NRS), 3) NRSs for emotional distress and distress at limitations in physical functioning, 4) Willingness to receive rehabilitation services, and 5) Rationale for lack of interest in rehabilitation services among participants rating their function-related distress ≥4/10. Proxy responses from caregivers were not permitted, however participants were permitted to solicit assistance or corroboration from caregivers.
Outcome Measures
AM-PAC-CAT
The AM-PAC-CAT is derived from a traditional fixed-length measure, the AM-PAC, which demonstrates excellent reliability and validity in diverse populations, including those with complex medical conditions.18–20 The AM-PAC-CAT retains its psychometric properties when the item response theory (IRT) calibrated AM-PAC banks are administered via a CAT platform.21 The validity of the Basic Mobility domain utilized in this study established through factor, modified parallel and Rasch analyses.19,22
More specifically, the AM-PAC-CAT Basic Mobility item bank of 101 items queries how much difficulty one has with performing physical activities, such as climbing steps. Response options include “none,” “a little,” “a lot,” and “unable. The AM-PAC-CAT questions and responses were read to participants over the phone. Testing continued until an AM-PAC-CAT session standard error (SE) fell below 2.0 or until a participant had answered 10 questions.
Symptom numerical rating scales (NRS)
Single-item PRO assessments for describing symptoms are valuable23 and, whether presented verbally or in a printed format, have been extensively validated in patients with cancer.24,25 Participants rated their pain and fatigue over the last 7 days with an 11 -point NRS - 0 (none) to 10 (as bad as it can be).
Distress numerical rating scales (NRS)
The use of an 11-point NRS, anchored with “none” and “as bad as it can be,” is a valid means of assessing distress among cancer populations with accuracy comparable to the 15-item Hospital Anxiety and Depression Scale.26 Two distress NRS were used. One to assess emotional distress and a second to assess distress specifically associated with functional limitations.
Interest in rehabilitation services
All patients, irrespective of their AM-PAC-CAT or functional distress scores, were asked “Would you be interested in receiving physical or occupational therapy, or visiting with a physician specialized in rehabilitation medicine in order to improve your functioning?” Similar items have been validate and used to assess patients’ receptivity to receiving a range of health care services.27,28 Participants were provided four response options; 1) No, 2) Yes, 3) Currently receiving rehabilitation services, and 4) Previously received rehabilitation services for current limitations.
Rationale for lack of interest in rehabilitation services
Participants with distress associated with functional limitations ≥ 4/10 who responded “no” when queried about interest in rehabilitation services were then asked, “Can you please help me to understand why you are not interested since you are distressed by your functional limitations?” No limitations were imposed on their responses which were transcribed verbatim.
Referral for rehabilitation services
When a participant expressed interest in receiving rehabilitation services, the study PI (AC) alerted their medical oncologist, and provided a list of local physical and occupational therapists and Physical Medicine and Rehabilitation physicians.
Ascertainment of Vital Status
Vital status was verified through death certificates, the Mayo Clinic EMR, next-of-kin reports, the Mayo Clinic Tumor Registry and the Social Security Death Index website.
Statistical Analyses
Descriptive statistics
Means and standard deviations for continuous variables and proportions for binary variables were used to summarize subject characteristics.
Logistic models, with the participant as the unit of analysis, were constructed to estimate associations between participants’ time-invariant characteristics and their receptivity to receiving rehabilitation services at any point during follow up. Since the total number of data points collected from a participant was correlated with their eventual interest in rehabilitation services, models were adjusted for total data points per participant.
Logistical mixed models were used to estimate associations between time varying covariates; sociodemographics, symptom and distress NRS scores, AM-PAC scores and receptivity to rehabilitation services, the binary dependent variable in all models. Univariate models were constructed initially, followed by multivariate models in a stepwise fashion. Variable entry in the multivariate models was based on an inclusion threshold using a coefficient Wald test p value ≤0.10, however, the criterion for retention was a p value of ≤ 0.05.29 Conventional model diagnostics were performed. All analyses were performed with STATA v.13.0.a
Qualitative Analyses
Open-ended responses regarding a lack of interest in receiving rehabilitation services were reviewed in their entirety to gain an overall impression of their content. Content analysis was used in an iterative process for coding data.30,31 Responses were assigned category codes for unique concepts or ideas. Data were then further grouped into sub-themes and assigned second-level codes. Transcripts were coded separately by two researchers to identify differences in coding.30,31 A consensus process incorporating the coders and the research team was used to resolve discrepancies. Integrity of the study data and processes were assured through: 1) the systematic use of scripted questions; 2) coding in small units to capture unique concepts; 3) review of response codes by a second investigator; and 4) final verification of the coding scheme through the evaluation of the exemplar quotations associated with each category or subcategory.
Results
Subjects
Overall 99 (31.8%) of the study’s 311 participants expressed an interest in receiving rehabilitation services; 38 at the time of their initial enrollment and an additional 61 during at least one of their subsequent contacts. Table 1 lists the baseline characteristics of all participants and subgroups that did, or did not, indicate an interest in rehabilitation services. Participants were 66 years old on average and just over half were male. Those expressing interest tended to have slightly higher Charlson indices (8.95 versus 8.54, p = 0.08), and were more likely to have a child as primary caregiver (18.18% versus 9.91%, p = 0.04) and a musculoskeletal comorbidity at the time of enrollment (42.4% versus 31.6%, p = 0.05).
Table 1.
Baseline characteristics of the total study cohort and subgroups defined by receptivity to rehabilitation services at baseline or follow-up
| All | Never | Ever | p value* | ||||
|---|---|---|---|---|---|---|---|
| Age, mean SD | 65.84 | 10.89 | 65.26 | 11.07 | 67.06 | 10.45 | 0.162 |
| Female, N % | 153 | 49.20% | 103 | 48.58% | 50 | 50.51% | 0.972 |
| Charlson index, mean SD | 8.67 | 2.53 | 8.54 | 2.51 | 8.95 | 2.56 | 0.078 |
| Principal caregiver, N % | |||||||
| Spouse† | 238 | 76.53% | 169 | 79.72% | 69 | 69.7% | |
| Child | 39 | 12.54% | 21 | 9.91% | 18 | 18.18% | 0.044 |
| Parent | 7 | 2.25% | 6 | 2.83% | 1 | 1.01 % | 0.438 |
| Sibling | 8 | 2.57% | 5 | 2.36% | 3 | 3.03% | 0.664 |
| Friend | 1 | 0.32% | 1 | .47% | 0 | ||
| Other | 18 | 5.79% | 10 | 4.72% | 8 | 8.08% | 0.202 |
| Comorbidities, N % | |||||||
| CAD | 69 | 22.19% | 44 | 20.75% | 25 | 25.25% | 0.246 |
| COPD | 101 | 32.48% | 66 | 31.13% | 35 | 35.35% | 0.327 |
| Musculoskeletal | 109 | 35.05% | 67 | 31.6% | 42 | 42.42% | 0.049 |
| Neurological | 32 | 10.29% | 20 | 9.43% | 12 | 12.12% | 0.354 |
p values were derived from logistic regression models adjusted for the number of data points collected for each participant
Spousal caregiver was the comparator.
Time-varying participant characteristics
A total of 2543 telephone interviews were conducted with an average of 8.18 interviews (SD 5.79) per participant. In 83.9% (n=2133) of interviews participants expressed that they were not interested in receiving rehabilitation services. In 7.7% of interviews participants expressed interest, and in 5.8% they reported having already received a rehabilitation service, and not being interested in further services. Table 2 lists AM-PAC-CAT, symptom, and distress scores among all participants as well as those that were or were not interested in receiving rehabilitation services at the time that the scores were collected. Symptom and distress scores were consistently higher, while AM-PAC-CAT scores were lower among participants interested in rehabilitation services. Figure 1 illustrates the proportions of receptive and non-receptive participants, as well as those who had previously received rehabilitation services in the following AM-PAC score strata. 1) Limited bed mobility and basic transfers (0–34), 2) Limited household mobility (35–52), 3) Limited community mobility (53–66), 4) Limited in moderate-strenuous activities (67–84), 5) Able to perform strenuous activity (≥85).32 The overwhelming majority of participants with limited community and household mobility were not interested in rehabilitation services.
Table 2.
Time varying characteristics among the study sample and participants who were and were not receptive to receiving rehabilitation services when the AM-PAC-CAT, and symptom and distress numerical rating scales were administered
| Odds Ratio | Standard Error | p value | Confidence Interval | ||
|---|---|---|---|---|---|
| Lower Limit | Upper Limit | ||||
| Univariate models | |||||
| APC BM score | 0.94 | 0.01 | <0.001 | 0.92 | 0.97 |
| Pain | 1.17 | 0.05 | <0.001 | 1.07 | 1.27 |
| Dyspnea | 1.08 | 0.04 | 0.067 | 0.99 | 1.17 |
| Fatigue | 1.09 | 0.04 | 0.022 | 1.01 | 1.18 |
| Functional distress | 1.33 | 0.05 | 0 | 1.23 | 1.43 |
| Proxy assisted | 2.54 | 0.98 | 0.016 | 1.19 | 5.42 |
| Multivariate model | |||||
| APC BM score | 0.97 | 0.01 | 0.006 | 0.95 | 0.99 |
| Functional distress | 1.27 | 0.05 | <0.001 | 1.17 | 1.38 |
Standard errors and p values allow for intragroup correlation,.
Figure 1.
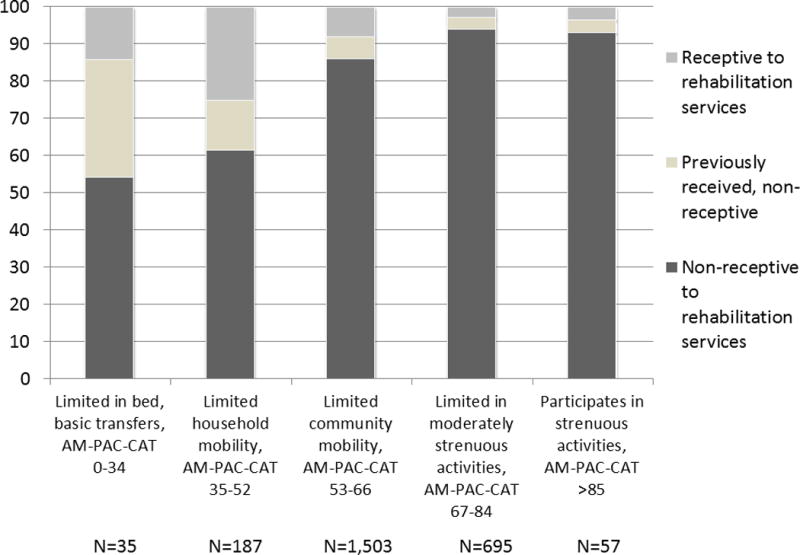
Bar chart of the proportions of participants who were receptive and non-receptive to rehabilitation services, and those who had previously received rehabilitation services among subgroups defined by AM-PAC-CAT score strata.
Uni- and multivariate models of time-varying characteristics, response-level data
Table 3 presents results of the logistic mixed models used to identify participant characteristics associated with receptivity to rehabilitation services at each data collection point. The need for caregiver assistance in answering questions was significantly associated with interest in rehabilitation (OR 2.54, p = 0.02), but did not meet criteria for retention in the multivariate model as the magnitude of the coefficient dropped to 0.84 with a p value of 0.69. Similarly, no symptom NRS score met criteria for inclusion in the multivariate model. In contrast, increased distress regarding functional limitations was highly associated with receptivity to rehabilitation services in both uni- and multivariate models, as were lower AM-PAC-CAT scores. In the final multivariate model, a 1-point increase in a participant’s functional distress rating increased the probability of rehabilitation receptivity by 27%, p <0.001, and a 1-point increase in AM-PAC-CAT score lessened the probability by 3%, p = 0.006. Neither age nor gender was significantly associated with receptivity; however the β coefficient for age in the univariate model was 1.03 with a p-value of 0.07, suggesting a weak potential association.
Table 3.
Results of the logistic mixed models used to identify participant characteristics associated with receptivity to rehabilitation services at each data collection point
| All N = 2541 |
Not receptive N = 2131 |
Receptive N = 196 |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| mean | SD | min | max | mean | SD | min | max | mean | SD | min | max | p value* | |
| AM-PAC | 62.93 | 9.68 | 4.20 | 95.84 | 63.82 | 9.09 | 4.20 | 95.84 | 57.39 | 9.82 | 4.20 | 87.85 | < 0.001 |
| Pain | 1.98 | 2.31 | 0 | 10 | 1.87 | 2.24 | 0 | 10 | 2.91 | 2.60 | 0 | 10 | < 0.001 |
| Fatigue | 3.95 | 2.85 | 0 | 10 | 3.86 | 2.84 | 0 | 10 | 4.95 | 2.77 | 0 | 10 | <0.001 |
| Dyspnea | 2.96 | 2.74 | 0 | 10 | 2.95 | 2.71 | 0 | 10 | 3.55 | 3.03 | 0 | 10 | <0.001 |
| Emotional distress | 1.33 | 2.38 | 0 | 10 | 1.17 | 2.21 | 0 | 10 | 2.70 | 3.19 | 0 | 10 | < 0.001 |
| Functional distress | 2.03 | 2.65 | 0 | 10 | 1.77 | 2.47 | 0 | 10 | 4.23 | 3.10 | 0 | 10 | < 0.001 |
Qualitative Results
The following five themes were identified using content analysis: (1) feeling “too busy” to consider rehabilitation services, and the perceptions that (2) rehabilitation is unnecessary; (3) a process must occur or reach completion (e.g., test results, cancer treatment) before considering rehabilitation; (4) rehabilitation would not be beneficial; and (5) participation would be burdensome. A final category was coded as “Miscellaneous”. Table 4 lists each of the themes and subthemes with exemplar quotations.
Table 4.
Exemplar quotes illustrating the 5 broad attitudinal barriers to receptivity to rehabilitation services identified in the qualitative analyses
| TOO BUSY |
| Fighting cancer: chemo/radiation |
| I have too much stuff going on. I get that chemotherapy. I think I’m doing pretty well. I am on radiation and chemo right now. I don’t think I will be able to do much now. Maybe later on |
| Appointments |
| All the other appointments with doctors I nave Well I have to many other things going at Mayo. I have many days of testing. |
| Other things to worry about-problems/complications/worries |
| Not yet. I have so many things that I have to do. I have cancer, diabetes, a bad back & other things It’s Christmas. I have enough going on. I know what to do for therapy. I don’t always do it. |
| UNNECESSARY |
| Don’t need it: have plenty of help |
| Because I have neighbors and friends who help me out all the time. I have my husband here. He helps a lot. |
| Receiving hospice, home health, nursing home care |
| I have Hospice and they do everything I need. I am going to a nursing home maybe they will have something there |
| Doing exercises |
| I have more physical activity because it is summer now, more lawn mowing, a lot more to do. I have been in therapy and I am doing some at home. I am doing what I can do. |
| Don’t think I need it |
| I don’t know why. Once I am off and moving around a bit I do o.k. I just have to be careful. I kind of like being on my own. I don’t want anyone to teach me how to do things. I can cope. |
| Not that bad off |
| I just don’t think I am to the point where I need any help yet I don’t think I am that bad off right now. Maybe down the road if things get worse. |
| Can take care of myself |
| I can regain my strength on my own. I can work through this on my own. If I feel like I need it in the future I might do it. |
| I am active |
| I am very active as it is. I feel like I am getting better and stronger with my normal activities I exercise and walk on my own. I’m a very active person. |
| WAITING |
| Recovery from/end of chemo/radiation/surgery |
| I just finished my radiation and they want to see how it will effect my pain and activity level. |
| Symptoms will improve |
| I am going to wait and see how my back feels. |
| Test results |
| I am going in for an MRI this Saturday. Let’s see what the problem is. |
| Treatment to work |
| I am being treated for this. I think that’s having some effect. While doing that there’s no point in therapy |
| Until I need it |
| I don’t want any until I have to have it. |
| NOT BENEFICIAL |
| Already tried therapy |
| I don’t know. I had it when I first came home. I had it right after my chemotherapy |
| I don’t think pt would help me at all. I try to do the best that I can. |
| Wouldn’t do any good/nothing would change |
| It isn’t going to change things. The arthritis is so bad it won’t help. I feel like I can do about what I can and it wouldn’t make a difference |
| Nothing else to do |
| I know I am dying and I don’t want to - it is a hopeless case |
| BURDENSOME |
| Symptoms |
| It is hard for me to breath. I have shortness of breath I get pretty tired. I get a sore back fairly easily. I’m pretty much limited in physical activity I’m in so much pain I don’t know if I could go through it |
| Related to something else |
| I have part of a lung removed and that is why I have shortness of breath. That is why I can’t do it and I accept that. I have one lung so in reality I’m probably doing better than most people. It’s not going to be bet |
| Travel |
| I would except I don’t have transportation. I can’t afford to hire someone |
| Cost |
| It costs too much money. I don’t want to get dumped by my insurance company |
| MISC |
| Therapy might make it worse |
| I have pain which has increased in my back. Therapy might aggravate it. |
Too Busy for Rehabilitation
Thirty-one respondents described feeling “too busy” with the competing demands of active cancer treatment being cited most frequently, n=13. Eight respondents identified conflicts with their medical appointments, and 10 reported a range of other issues.
Rehabilitation is unnecessary
Subthemes included that the patient: 1) had the help they needed to compensate for their functional limitations (n=27); 2) believed they were able to manage on their own (n=36); 3) had previously received therapy or remained physically active (n=18); 4) had shifted their care to an alternative setting (n=13), e.g., hospice; 5) things were not that “bad” (n=8); and 6) had no rehabilitation needs (n=25).
Waiting
Thirty-eight respondents identified that they were waiting for something to occur or reach completion: recovery from chemotherapy or radiation (n=17), symptom improvement (n=4), test results (n=6), a treatment response (n=4), worsening of their condition (n=2). Five had been given physical therapy (PT) prescriptions but had not followed up on them due to a range of issues including winter weather and the flu season.
Rehabilitation Services would not be beneficial
Eighty-four respondents indicated that rehabilitation services would not be beneficial. The most common response was some variant on the theme that they had already tried rehabilitation (n=36). For example, one respondent with a high level of functional distress offered that “I have had PT in the past and it was not helpful.” However, others shared that they had positive experiences with rehabilitation and confidence in self-management as supported by this illustrative comment: “I have already gone through physical therapy. I know what I need to know.” Twenty-eight did not believe that rehabilitation services would offer benefit. Others expressed fatalism related to the status of their cancer or treatment, (n=20) as illustrated by this remark, “My cancer is pretty active. I don’t know how much time I have left.”
Rehabilitation Services are Burdensome
A fifth barrier identified by 58 respondents reflected the perception that rehabilitation services impose extra burden. Symptoms due to cancer and/or its treatment were the most frequently reported reason for this attitude as illustrated by this response (n=29): “I’m in so much pain I don’t know if I could go through it.” Practical issues, such as transportation (n=12) and affordability (n=5) emerged as additional barriers, as did the perception that “it is too hard” (n=2). Ten participants identified physical limitations, e.g. prior lung resection, foot amputation, arthritis, as the reason that receipt of rehabilitation services would be burdensome.
Discussion
To the best of our knowledge, this is the first report of low receptivity and patients’ perceived barriers to receipt of rehabilitation services in a cancer population. Our findings suggest that patients’ attitudes and beliefs regarding rehabilitation services are important and previously unrecognized barriers to functional preservation among patients with cancer. Only one third of study participants were ever interested in receiving services despite their established benefits,33 and participants’ high levels of mobility limitations and related distress.
Low uptake of rehabilitation services, particularly in the outpatient setting, has been consistently reported among cancer populations for over four decades.34 This pattern has typically been attributed to low rates of impairment detection and referral for rehabilitation services by oncologists.12 For example, medical oncologists document functional limitations, at best, only a quarter of the time when patients endorse their presence.13 Our findings, however, suggest and begin to quantify the fact that patient attitudes and beliefs may also contribute to low rehabilitation uptake. Whether their beliefs arise, in part, from a prioritization of disease-directed treatments to the point of a neglect of function-directed care, as some reports have suggested,35 remains poorly studied and conjectural. Regardless, it appears that the reasons for low uptake of rehabilitation services are complex and require further study if this problem is to be overcome.
Our mixed methods results extend the health care barriers literature by quantifying participants’ limited receptivity to rehabilitation, revealing prevalent attitudinal barriers, and elucidating the scope of participants’ underlying beliefs. The health care barriers literature has historically focused on provider- and system-related barriers; e.g., proximity to hospitals, access to specialist care, and insurance coverage,36 however participants in this study invoked barriers more akin to those reported in exercise studies, such as being too busy or waiting for symptoms to improve.37 However, unlike exercise, the most prevalent barrier to rehabilitation was the perception that it is not needed – held even by those with marked mobility limitations and reporting the highest levels of function-related distress. Our findings suggest the need to consider a new focus on patient perception of the role of rehabilitation services as part of their comprehensive cancer care.
In addition, unlike the majority of patients receiving treatment for conventional rehabilitation diagnoses, patients with cancer face the extensive and competing demands of their cancer-directed therapies. Since being too busy with other appointments and travel were commonly cited barriers, improved integration of rehabilitation services into scheduled treatments, diagnostics, and appointments could potentially lessen perceived burden. Adverse symptoms, or the possibility of increased symptom intensity, also diminished participants’ interest. Therefore, modulating rehabilitation efforts (e.g., reducing exercise intensity following chemo- or radiation therapies) to anticipate increases in symptom burden and fatigue may also warrant consideration.
Rehabilitation services are well-integrated into the in- and outpatient management of patients with predictable (e.g. total joint replacement) and unpredictable (e.g., stroke and spinal cord injury) sources of disablement.38–40 Our findings suggest that this same approach could fill the gaps in cancer care identified in this study. Setting expectations with patients that rehabilitation is part of comprehensive care and not an “opt-out part of care may curb ambivalence.41
Study Limitations
A limitation of our study is its sample’s homogeneity – the majority of participants were Caucasian and all had advanced stage lung cancer. Further, they were recruited from a National Cancer Institute-designated comprehensive cancer center - an environment that differs from the community settings where most patients receive their cancer care. Whether demographic and/or clinical characteristics impact a patient’s receptivity to rehabilitation is not known. Future research exploring receptivity to rehabilitation appears to be warranted across diverse cancer populations and settings.
An additional limitation is the potential lack of congruence between the single item used to assess receptivity in this study and the type of “real-life” patient-clinician communication that would ideally create an individualized context for rehabilitation referrals. In theory, such communication would link the referral to patient-specific benefits rather than the generic possibility of improved function. While it is likely that such communication would increase receptivity, it is somewhat moot as reports consistently suggest that scant attention is paid to either the detection or treatment of functional limitations among cancer populations, even at National Cancer Institute-designated centers with established cancer rehabilitation programs9,10,12,13,42 Although similar items have been validated across a range of health care services,27,28 none have been specifically vetted to assess attitudes towards function-directed care. Nevertheless, we believe that participants’ responses are informative and accurately reflect their attitudes for several reasons. First, administration of the receptivity item was preceded by detailed questioning about participants’ functional abilities via the AM-PAC-CAT, as well as by an NRS querying their distress over functional limitations. This created a highly individualized functional context for posing the receptivity item. Second, participants’ qualitative responses indicate that they understood the item and answered in a manner aligned with their priorities and preferences. Last, if functional screening for emerging disablement were imbedded in oncology care as a basis for rehabilitation referrals, patients would be afforded little more promise of benefits other than improved function. Therefore, it is likely that our findings accurately reflect the attitudes of patients offered rehabilitation services after routine, systematic functional screening but, admittedly, cannot predict the outcome of more individually tailored clinician-patient communication.
Conclusion
A majority of patients with late stage lung cancer are limitedly receptive to receiving rehabilitative services despite prevalent disablement and high levels of associated distress. This finding suggests that patients may approach related clinical discussions with ambivalence, and that measures such as targeted education to acknowledge and address the sources of ambivalence are needed.
Glossary
- AM-PAC-CAT
Activity Measure for Post Acute Care Computer Adaptive Test
- EMR
Electronic medical record
- IRT
Item response theory
- NSCLC
Non-small cell lung cancer
- NRS
Numerical rating scales
- OR
Odds ratio
- PRO
Patient reported outcome
- PT
Physical therapy
- QOL
Quality of life
- SCLC
Small cell lung cancer
- SD
Standard deviation
- SE
Standard error
References
- 1.Taylor RS, Brown A, Ebrahim S, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116:682–92. doi: 10.1016/j.amjmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 2.Mereles D, Ehlken N, Kreuscher S, et al. Exercise and respiratory training improve exercise capacity and quality of life in patients with severe chronic pulmonary hypertension. Circulation. 2006;114:1482–9. doi: 10.1161/CIRCULATIONAHA.106.618397. [DOI] [PubMed] [Google Scholar]
- 3.Lahart IM, Metsios GS, Nevill AM, Carmichael AR. Physical activity, risk of death and recurrence in breast cancer survivors: A systematic review and meta-analysis of epidemiological studies. Acta Oncol. 2015;54:635–54. doi: 10.3109/0284186X.2014.998275. [DOI] [PubMed] [Google Scholar]
- 4.Ballard-Barbash R, Friedenreich CM, Courneya KS, Siddiqi SM, McTiernan A, Alfano CM. Physical activity, biomarkers, and disease outcomes in cancer survivors: a systematic review. J Natl Cancer Inst. 2012;104:815–40. doi: 10.1093/jnci/djs207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mishra SI, Scherer RW, Snyder C, Geigle P, Gotay C. Are exercise programs effective for improving health-related quality of life among cancer survivors? A systematic review and meta-analysis. Oncol Nurs Forum. 2014;41:E326–42. doi: 10.1188/14.ONF.E326-E342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tian L, Lu HJ, Lin L, Hu Y. Effects of aerobic exercise on cancer-related fatigue: a meta-analysis of randomized controlled trials. Support Care Cancer. 2015 doi: 10.1007/s00520-015-2953-9. [DOI] [PubMed] [Google Scholar]
- 7.Cheville AL, Alberts SR, Rummans TA, et al. Improving Adherence to Cancer Treatment by Addressing Quality of Life in Patients With Advanced Gastrointestinal Cancers. J Pain Symptom Manage. 2015;50:321–7. doi: 10.1016/j.jpainsymman.2015.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheville AL, Kornblith AB, Basford JR. An examination of the causes for the underutilization of rehabilitation services among people with advanced cancer. Am J Phys Med Rehabil. 2011;90:S27–37. doi: 10.1097/PHM.0b013e31820be3be. [DOI] [PubMed] [Google Scholar]
- 9.Cheville AL, Troxel AB, Basford JR, Kornblith AB. Prevalence and treatment patterns of physical impairments in patients with metastatic breast cancer. J Clin Oncol. 2008;26:2621–9. doi: 10.1200/JCO.2007.12.3075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheville AL, Dose AM, Basford JR, Rhudy LM. Insights into the reluctance of patients with late-stage cancer to adopt exercise as a means to reduce their symptoms and improve their function. J Pain Symptom Manage. 2012;44:84–94. doi: 10.1016/j.jpainsymman.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 11.Weir HK, Thompson TD, Soman A, Moller B, Leadbetter S. The past, present, and future of cancer incidence in the United States: 1975 through 2020. Cancer. 2015;121:1827–37. doi: 10.1002/cncr.29258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheville A, Kornblith A, Basford J. An Examination of the Causes for the Underutilization of Rehabilitation Services Among People with Advanced Cancer. American Journal of Physical Medicine and Rehabilitation. 2011 doi: 10.1097/PHM.0b013e31820be3be. In Press. [DOI] [PubMed] [Google Scholar]
- 13.Cheville AL, Beck LA, Petersen TL, Marks RS, Gamble GL. The detection and treatment of cancer-related functional problems in an outpatient setting. Support Care Cancer. 2009;17:61–7. doi: 10.1007/s00520-008-0461-x. [DOI] [PubMed] [Google Scholar]
- 14.Karmali KN, Davies P, Taylor F, Beswick A, Martin N, Ebrahim S. Promoting patient uptake and adherence in cardiac rehabilitation. Cochrane Database Syst Rev. 2014;6:CD007131. doi: 10.1002/14651858.CD007131.pub3. [DOI] [PubMed] [Google Scholar]
- 15.McCahon D, Daley AJ, Jones J, et al. Enhancing adherence in trials promoting change in diet and physical activity in individuals with a diagnosis of colorectal adenoma; a systematic review of behavioural intervention approaches. BMC cancer. 2015;15:505. doi: 10.1186/s12885-015-1502-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cheville AL, Yost KJ, Larson DR, et al. Performance of an item response theory-based computer adaptive test in identifying functional decline. Archives of physical medicine and rehabilitation. 2012;93:1153–60. doi: 10.1016/j.apmr.2012.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 18.Coster WJ, Haley SM, Andres PL, Ludlow LH, Bond TL, Ni PS. Refining the conceptual basis for rehabilitation outcome measurement: personal care and instrumental activities domain. Med Care. 2004;42:162–72. doi: 10.1097/01.mlr.0000103521.84103.21. [DOI] [PubMed] [Google Scholar]
- 19.Haley SM, Coster WJ, Andres PL, et al. Activity outcome measurement for postacute care. Med Care. 2004;42:149–61. doi: 10.1097/01.mlr.0000103520.43902.6c. [DOI] [PubMed] [Google Scholar]
- 20.Siebens H, Andres PL, Pengsheng N, Coster WJ, Haley SM. Measuring physical function in patients with complex medical and postsurgical conditions: a computer adaptive approach. Am J Phys Med Rehabil. 2005;84:741–8. doi: 10.1097/01.phm.0000186274.08468.35. [DOI] [PubMed] [Google Scholar]
- 21.Haley SM, Fragala-Pinkham M, Ni P. Sensitivity of a computer adaptive assessment for measuring functional mobility changes in children enrolled in a community fitness programme. Clin Rehabil. 2006;20:616–22. doi: 10.1191/0269215506cr967oa. [DOI] [PubMed] [Google Scholar]
- 22.Jette AM, Haley SM, Tao W, et al. Prospective evaluation of the AM-PAC-CAT in outpatient rehabilitation settings. Phys Ther. 2007;87:385–98. doi: 10.2522/ptj.20060121. [DOI] [PubMed] [Google Scholar]
- 23.Cleeland CS, Mendoza TR, Wang XS, et al. Assessing symptom distress in cancer patients: the M.D. Anderson Symptom Inventory. Cancer. 2000;89:1634–46. doi: 10.1002/1097-0142(20001001)89:7<1634::aid-cncr29>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 24.Buchanan DR, O’Mara AM, Kelaghan JW, Minasian LM. Quality-of-life assessment in the symptom management trials of the National Cancer Institute-supported Community Clinical Oncology Program. J Clin Oncol. 2005;23:591–8. doi: 10.1200/JCO.2005.12.181. [DOI] [PubMed] [Google Scholar]
- 25.Paice JA, Cohen FL. Validity of a verbally administered numeric rating scale to measure cancer pain intensity. Cancer Nurs. 1997;20:88–93. doi: 10.1097/00002820-199704000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Mitchell AJ. Short screening tools for cancer-related distress: a review and diagnostic validity meta-analysis. J Natl Compr Canc Netw. 2010;8:487–94. doi: 10.6004/jnccn.2010.0035. [DOI] [PubMed] [Google Scholar]
- 27.Birndorf CA, Madden A, Portera L, Leon AC. Psychiatric symptoms, functional impairment, and receptivity toward mental health treatment among obstetrical patients. Int J Psychiatry Med. 2001;31:355–65. doi: 10.2190/5VPD-WGL1-MTWN-6JA6. [DOI] [PubMed] [Google Scholar]
- 28.Howell LA, Brockman TA, Sinicrope PS, et al. Receptivity and Preferences in Cancer Risk Reduction Lifestyle Programs: A Survey of Colorectal Cancer Family Members. J Behav Health. 2013;2:279–90. doi: 10.5455/jbh.20130921013627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Burnham K, Andersson D. Model selection and multimodel inference; a practical information-theoretic approach. 2nd. New York: Springer-Verlag; 1998. Model selection methods; pp. 35–7. [Google Scholar]
- 30.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2003;24:105–12. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 31.Krippendorff K. Content analysis: An introduction to its methodology. Second. Thousand Oaks, CA: Sage; 2004. [Google Scholar]
- 32.Tao W, Haley SM, Coster WJ, Ni P, Jette AM. An exploratory analysis of functional staging using an item response theory approach. Arch Phys Med Rehabil. 2008;89:1046–53. doi: 10.1016/j.apmr.2007.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Granger CL, McDonald CF, Berney S, Chao C, Denehy L. Exercise intervention to improve exercise capacity and health related quality of life for patients with Non-small cell lung cancer: a systematic review. Lung Cancer. 2011;72:139–53. doi: 10.1016/j.lungcan.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 34.Lehmann JF, DeLisa JA, Warren CG, deLateur BJ, Bryant PL, Nicholson CG. Cancer rehabilitation: assessment of need, development, and evaluation of a model of care. Arch Phys Med Rehabil. 1978;59:410–9. [PubMed] [Google Scholar]
- 35.Takeuchi EE, Keding A, Awad N, et al. Impact of patient-reported outcomes in oncology: a longitudinal analysis of patient-physician communication. J Clin Oncol. 2011;29:2910–7. doi: 10.1200/JCO.2010.32.2453. [DOI] [PubMed] [Google Scholar]
- 36.Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19:127–40. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- 37.Ajzen I. From intentions to actions: A theory of planned behavior. In: Kuhl J, Beckman J, editors. Action-control: From cognition to behavior. Heidelberg: Springer; 1985. pp. 11–39. [Google Scholar]
- 38.Cibulka MT, White DM, Woehrle J, et al. Hip pain and mobility deficits–hip osteoarthritis: clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2009;39:A1–25. doi: 10.2519/jospt.2009.0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mertes SC, Raut S, Khanduja V. Integrated care pathways in lower-limb arthroplasty: are they effective in reducing length of hospital stay? Int Orthop. 2013;37:1157–63. doi: 10.1007/s00264-013-1829-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Starks I, Wainwright TW, Lewis J, Lloyd J, Middleton RG. Older patients have the most to gam from orthopaedic enhanced recovery programmes. Age Ageing. 2014;43:642–8. doi: 10.1093/ageing/afu014. [DOI] [PubMed] [Google Scholar]
- 41.Hewitt G, Sims S, Greenwood N, Jones F, Ross F, Harris R. Interprofessional teamwork in stroke care: Is it visible or important to patients and carers? J Interprof Care. 2015;29:331–9. doi: 10.3109/13561820.2014.950727. [DOI] [PubMed] [Google Scholar]
- 42.Cheville AL, Shen T, Chang M, Basford JR. Appropriateness of the treatment of fatigued patients with stage IV cancer. Support Care Cancer. 2012;21:229–33. doi: 10.1007/s00520-012-1515-7. [DOI] [PubMed] [Google Scholar]
- a.StataCorp. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP; 2013. [Google Scholar]


