Abstract
Introduction
Recent advancements in imaging technology have significantly increased the diagnostic accuracy of magnetic resonance imaging for prostate cancer. However, tissue diagnosis and grading remain the gold standard for diagnosis and prognostication. Because transrectal ultrasound guided prostate biopsy performs poorly, extensive research has been conducted into biopsy techniques that are guided by magnetic resonance imaging, including direct in-bore, cognitive fusion and magnetic resonance imaging/ultrasound fusion guided biopsies.
Methods
The PubMed® database was searched from inception until January 15, 2014 for criteria pertaining to targeted prostate biopsy.
Results
Initial studies of the 3 types of targeted prostate biopsy yielded similar results. Most importantly, targeted biopsy detects a greater amount of clinically significant prostate cancer than does transrectal ultrasound guided biopsy. Magnetic resonance imaging/ultrasound fusion guided biopsy has generated the most interest, as it is an office based procedure that does not require a significant change from the current workflow of transrectal prostate biopsy. These techniques hold great promise in the areas of patient selection for definitive treatment, appropriate screening, active surveillance and focal therapy for prostate cancer.
Conclusions
Targeted prostate biopsy has the potential to significantly improve the way patients are screened, treated and monitored in the setting of prostate cancer. These techniques allow for an individualized approach to each patient, which is a substantial improvement over the current practice of effectively random prostate biopsies. Large, multicenter studies are necessary to determine whether targeted prostate biopsy will become a definitive standard of care.
Keywords: prostatic neoplasms, image-guided biopsy, magnetic resonance imaging, ultrasound, high-intensity focused, transrectal
History of Prostate Cancer Screening
Reducing the morbidity and mortality associated with prostate cancer has been the urgent goal of cancer screening programs for several decades. However, it is a goal that has been largely unmet. Since the 1940s PCa in American men has been prevalent and deadly, accounting for nearly 90% of all male genital cancers at that time and yet only 5% were detected at a stage that was still amenable to surgery.1,2 These rates illustrate the limitations associated with the use of digital rectal examination, a time-tested screening tool for prostate cancer. It is subjective, operator dependent and experience dependent, and primarily limited to large, posterior tumors. Worst of all, DRE screening studies of PCa have failed to demonstrate a reduction in cancer specific mortality in any age group.3
It is in this context that serum prostate specific antigen was introduced and approved by the Food and Drug Administration in 1986. Originally intended as a tool for monitoring previously diagnosed PCa, PSA was quickly adapted for screening in conjunction with DRE. This additional screening changed the epidemiology of PCa in 2 distinct ways. First, the overall incidence of PCa increased dramatically, as previously non-palpable and asymptomatic tumors were detected. Second, the relative incidence of higher stage disease decreased. These developments came on the heels of advances in medical imaging, which paved the way for the adoption of transrectal ultrasound. This too was originally thought to be a possible PCa screening tool, although initial reports demonstrated limited accuracy.4 Nonetheless, in 1989 Hodge et al reported that systematic TRUS guided biopsy detected significantly more PCa than did any previously used technique.5 This biopsy scheme became the foundation for the current standard of care, with even greater cancer detection as the number of biopsy cores increased from 6 to 12 or more.6
Thus, the current paradigm for PCa screening faces several challenges. The death rate from prostate cancer remains high. In 2013 it was the most common nonskin cancer in American men, as well as the second most common cause of cancer related death.7 PSA, DRE and TRUS guided biopsy still perform poorly in culling those patients with clinically significant disease for whom definitive therapy would render a survival benefit.8 It is becoming increasingly apparent that the screening process itself carries inherent risks, including infectious complications, many of which are now caused by antibiotic resistant organisms.9 These limitations all played a role in the decision by the USPSTF (U.S. Preventive Services Task Force) to recommend against routine PSA based screening for PCa.
MRI as a Diagnostic Modality for Prostate Cancer
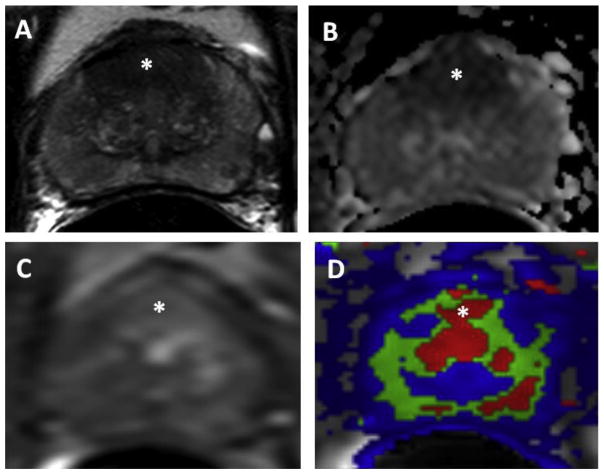
Magnetic resonance imaging was introduced in the 1990s as a tool with the potential to improve the preoperative staging of PCa. It was initially limited to this role, as early techniques had a high resolution for T3 disease but a poor sensitivity for intraprostatic lesions.10 However, MRI technology quickly improved, which became most readily apparent after the recent advent of MP-MRI, a technique that combines traditional T1 and T2-weighted images with other MRI sequences such as diffusion weighted imaging, MR spectroscopy and dynamic contrast enhancement (fig. 1). MP-MRI, in conjunction with endorectal coils and high field strength magnets, significantly improves PCa detection and localization,11,12 which has led to a recent consensus among radiologists endorsing its use for prostate imaging.13
Figure 1.
Patient is 53-year-old man with family history of prostate cancer (PSA 6.1 ng/dl) and multiple prior negative 12-core biopsies. A, axial T2-weighted MRI demonstrates lesion in midline apical-base anterior transitional zone (asterisk). B, apparent diffusion coefficient maps of diffusion weighted MRI show restricted diffusion corresponding to hypointense signal intensity within lesion (asterisk). C, raw dynamic contrast enhanced MRI. D, ktrans map derived from dynamic contrast enhanced MRI confirms hypervascularity within anterior midline transitional zone lesion (asterisk). MRI/TRUS fusion guided biopsy revealed high volume Gleason 8 PCa in multiple targeted cores of this anterior lesion.
MRI Guided Biopsy
Despite the invaluable anatomical information provided by MRI, tissue diagnosis and grading remain the gold standard for the diagnosis and prognostication of PCa. Thus, a variety of prostate biopsy techniques that are MRI guided have been developed, including direct in-bore, cognitive fusion and MRI/ultrasound fusion guided biopsy.
Direct in-Bore MRI Guided Biopsy
An option for obtaining MRI guidance of a prostate biopsy is to perform the biopsy within the MRI gantry itself. A patient with clinical suspicion of PCa first undergoes a diagnostic MRI. If suspicious lesions are identified, he then returns for a repeat MRI to re-localize these lesions immediately before biopsy. The biopsy is then performed within the MRI gantry, with further MRI scans obtained throughout the biopsy session to track needle placement. The primary advantage of this technique is that it allows for precise targeting of MRI suspicious lesions, many of which are clinically relevant.12 However, the technique also suffers from significant limitations from the perspectives of the patient, physician and hospital.
The procedure is lengthy and physically uncomfortable, often requiring sedation with general anesthesia. The magnetic environment, with its requirement for nonmagnetic needles and other supplies, and the long duration of serial MRI scanning are practical challenges to the physician performing the biopsy. The technique produces high opportunity costs from time spent within MRI facilities. All of these limitations have spurred the development of other techniques for using MRI data for biopsies performed outside the MRI gantry. Published detection rates vary but a recent prospective comparative study demonstrated that MRI guided biopsy was superior to TRUS guided biopsy for PCa detection (see table).14
Table.
Representative studies of direct in-bore, cognitive fusion and MRI/US fusion guided biopsies
| No. all PCa Detected/Total No. (%) | No. Clinically Significant PCa Detected/Total No. (%) | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Biopsy System | Primary Comparison | Targeted Biopsy | Standard Biopsy | Targeted Biopsy Standard Biopsy | Notes | |
| Direct in-gantry MRI guided biopsy: | ||||||
| Charité MRI devices, Daum custom device (Beyersdorff et al: Radiology 2005; 234: 576) | Not applicable | 5/12 (42) | Not applicable | Not recorded | Not recorded | Feasibility study |
| Modified MRI devices, Daum custom device (Engelhard et al: Eur Radiol 2006; 16: 1237) | Not applicable | 14/37 (38) | Not applicable | Not recorded | Not recorded | Modified feasibility study |
| Invivo, Schwerin, Germany14 | MRI guided vs TRUS | 34/34 (100) | 64/64 (100) | Highest Gleason grade 4 (91) | Highest Gleason grade 4 (46) | MRI guided and TRUS guided biopsy predicted radical prostatectomy pathology in 88% and 55% of cases, respectively (p=0.001, statistically significant) |
| Cognitive fusion guided biopsy: | ||||||
| 1.5 T MRI without endorectal coil32 | Cognitive fusion vs TRUS | 290/302 (96) | 236/302 (78) | 236/249 (95) | 237/249 (95) | Targeted biopsy alone would have avoided diagnosis of clinically insignificant PCa in 53/302 pts |
| 3 T MRI without endorectal coil (Park et al: AJR Am J Roentgenol 2011; 197: W876) | Cognitive fusion vs TRUS | 13/44 (30) | 4/41 (10) | Not recorded | Not recorded | MRI guided and TRUS guided biopsy groups had positive core rates of 10% and 2.5%, respectively (p=0.00, statistically significant) |
| eiNav/Artemis15 | Cognitive fusion vs MRI/US fusion | 27% vs 32% | Not applicable | 15% vs 20% | Not applicable | Trend toward statistical significance in favor of MRI/US fusion guided biopsy, standard 12-core biopsy detected more highest Gleason grade 6 disease than did targeted biopsy |
| MRI/US fusion guided biopsy: | ||||||
| UroNav17 | MRI/US fusion vs TRUS | 53/105 (51) | 51/105 (49) | 47/105 (45) | 34/105 (32) | External validation study of Pinto et al20 |
| Esaote, Koelis22 | MRI/US fusion (rigid, elastic) vs cognitive fusion vs TRUS* | |||||
| BiopSee23 | MRI/US fusion vs TRUS | 30% of cores | 8% of cores | Not recorded | Not recorded | Transperineal approach |
Cancer detection rates reported using logistic regression. The 2 MRI/US fusion platforms performed significantly better than TRUS (p=0.0065, p=0.0016), while cognitive fusion did not (p=0.66).
Cognitive Fusion Guided Biopsy
A second option for combining prostate MRI with the gold standard of biopsy is “cognitive fusion.” This term essentially describes the process of evaluating a diagnostic prostate MRI before performing a TRUS guided biopsy. During the TRUS guided biopsy the urologist then estimates where the MRI positive lesions are on real-time TRUS, allowing for increased sampling density in these areas. This technique is appealing for 2 reasons. First, it is immediately available to all urologists, as no special biopsy equipment is necessary, and second, cognitive fusion does not incur the time and opportunity costs of in-gantry MRI guided biopsy. However, cognitive fusion is a low-tech solution to a complex problem and thus introduces its own set of limitations.
The technique is highly operator dependent. Even if cognitive fusion is reliable in expert hands, it may not be reproducible outside of centers of excellence with the most extensive MRI and US experience. Cognitive fusion requires a difficult mental anatomical transformation from 2-dimensional TRUS images to 3-dimensional MRI and vice versa. This is a likely aspect of MRI guided biopsy that could be better automated by computer software. Finally, unlike other fusion techniques, cognitive fusion does not allow for the ability to record the precise locations of each biopsy, which makes it less appealing in the setting of active surveillance, for example when urologists may be especially interested in resampling specific biopsy locations at a later date. Nonetheless, recent studies have shown cognitive fusion to perform significantly better than TRUS guided biopsy, including in a prospective, blinded comparison (see table).15
MRI/US Fusion Guided Biopsy
General Principles
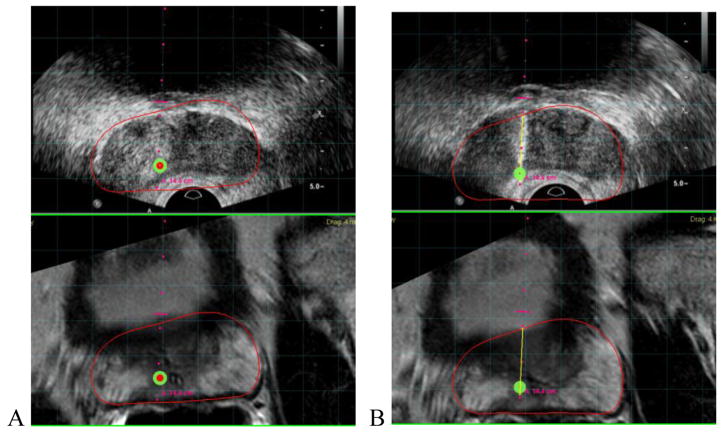
The third option for obtaining MRI guidance is MRI/US fusion guided biopsy, a process by which diagnostic magnetic resonance images are fused to TRUS images by software platforms. This technique was developed in an attempt to combine the most appealing aspects of direct in-bore and cognitive fusion MRI guided biopsies. Like the former, MRI/US fusion guided biopsy allows the operator to visualize and target suspicious lesions in real time (fig. 2). The software platforms can also record the locations of all biopsies, allowing for later resampling (figs. 3 and 4). Like the latter, MRI/US fusion guided biopsy is an office based biopsy platform that is practical for community urologists and comfortable for patients.
Figure 2.
Representative screenshots demonstrate fusion of MRI and real-time TRUS imaging before (A) and after (B) acquisition of targeted biopsy core
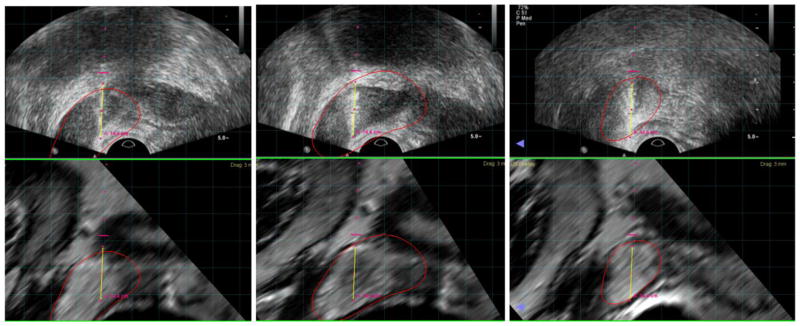
Figure 3.
Representative extended sextant biopsies using MRI/US fusion software, which allows for precise recording of all biopsy locations in 3D space
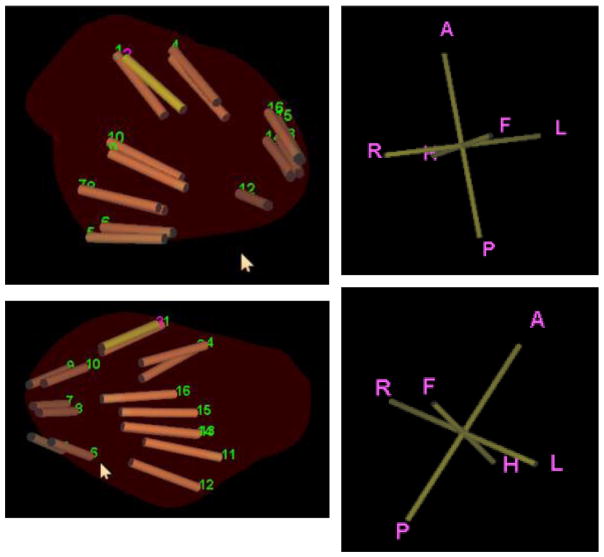
Figure 4.
Post-procedure 3D mapping of targeted and 12-core extended sextant needle biopsy locations
As with the other techniques, MRI/US fusion guided biopsy first requires a diagnostic MRI. A radiologist then identifies areas of suspicion, which are marked and loaded into the fusion software. The prostate gland is also segmented so that the shape of the prostate on MRI can be fused to the shape of the prostate on TRUS. If a biopsy is deemed necessary, the urologist begins by performing real-time TRUS. At the beginning of this session, the segmented MR and US prostate volumes are co-registered by the fusion software. The urologist then performs a TRUS guided biopsy, which now contains visible targets based on the diagnostic MRI. This is a general work-flow that holds true across different “flavors” of fusion guided biopsy platforms. However, it is not universal.
Each step in the fusion guided biopsy process offers opportunities for fusion platform manufacturers to differentiate their products from existing models. The greatest variation exists in how the MR and US images are fused, and how the fusion platform guides and tracks the biopsy. The fusion platforms currently used with the greatest amount of clinical evidence include UroNav (Philips/Invivo, Gainesville, Florida), Artemis® (Eigen, Grass Valley, California), Urostation (Koelis, Grenoble, France), BiopSee® (Pi Medical, Athens, Greece), Virtual Navigator (Esaote, Genoa, Italy) and Hitachi Real-time Virtual Sonography (Hitachi Medical Systems America, Twinsburg, Ohio).
Fusion of Diagnostic Images
One of the greatest challenges of performing accurate MRI/US fusion guided biopsy is the initial co-registration of MR and US images. Although fusion software offers the promise of a significant computational benefit over cognitive fusion, the algorithm that best achieves this result is still being determined. The 2 general strategies that have been developed are rigid registration and elastic registration. In the former the TRUS and MR images undergo rotational and translational adjustments such that they become as congruent as possible. In the latter deformation and warping are added to the rotation and translation in an attempt to create images that match even more closely. These registration techniques vary among MRI/US fusion platforms, with no clear advantage to either option.
However, a recent preclinical study demonstrated the feasibility of an appealing third option.16 In that study the current model of a single rigid or elastic registration was replaced with continuous, automatic registrations and adjustments by the fusion software. If replicated in clinical studies this improvement could help simplify MRI/US fusion even further. It could also lead to a clearer favorite among fusion platforms, as the current lack of comparative studies among platforms precludes meaningful conclusions as to which is best.
Biopsy Guidance
Whereas image co-registration is largely a challenge of software development, the more immediately obvious difference among various fusion biopsy platforms is the equipment itself. Each system uses a unique mechanism to guide and track biopsies, ranging from inconspicuous TRUS probe position detectors to larger robotic arms. UroNav provides an example of the former as the biopsy guidance system uses a sensor that is directly attached to a freehand TRUS probe. The sensor is then monitored by a small electromagnetic field generator nearby, allowing the urologist to perform targeted biopsies in a manner similar to the current standard practice (fig. 5). In contrast, the Artemis system incorporates a mechanical localizer in the form of a robotic arm that positions, monitors and controls all of the biopsy devices. This system has the advantage of removing a source of possible operator input, which may otherwise limit biopsy accuracy. For example, with a freehand device, the operator may inadvertently move the TRUS probe after a target has been localized but before the biopsy gun has fired. With a robotic arm, the entire unit may be immobilized. However, this advantage involves trade-offs in efficiency. The robotic arm is relatively bulky and somewhat limited in its access to all parts of the prostate, and the entire biopsy process involves a greater deviation from existing office based practices with which the urology community is well acquainted.
Figure 5.
Examples of equipment necessary for MRI/US fusion guided biopsy using UroNav platform. A, UroNav console. B, ultrasound probe with encoder. C, electromagnetic field generator. D, ultrasound cart.
Other MRI/US fusion guided biopsy platforms involve more subtle variations of these 2 extremes. For example, Urostation incorporates a freehand TRUS probe but generates continuous 3D images of the prostate that are fused to the MRI. The BiopSee system also uses standard freehand TRUS. However, it typically requires biopsies to be performed transperineally. Other systems like the Virtual Navigator and Hitachi Real-time Virtual Sonography differ primarily in their original intended use. These 2 fusion platforms were originally designed for a wider range of interventional procedures and thus have the capability to combine computerized tomography or MR images with US. Their use in the setting of prostate cancer is more limited, with some platforms still not commercially available in the United States.
Results
UroNav was the first MRI/US fusion guided biopsy system to be developed and thus has the greatest amount of data supporting its use. It was created by the urology and radiology departments at the National Institutes of Health in a research collaboration with Royal Philips. The NIH group began enrolling patients in a prospective study of MRI/US fusion guided prostate biopsy in 2004. UroNav has been shown to detect significantly more PCa per core than a standard 12-core biopsy, to detect more clinically significant disease and to have particular usefulness for highly suspicious lesions on MRI.17–20 Consistently similar results have been reported by numerous other institutions using the Artemis,21 Urostation,22 BiopSee,23 Virtual Navigator22 and Hitachi Real-time Virtual Sonography24 devices. Detailed results of these studies have been described in depth in recent reviews of MRI/US fusion guided biopsy and are summarized in the table.25,26
Advantages of MRI/US Fusion Guided Biopsy
Because research supporting MRI/US fusion guided biopsy is still relatively new, many of the potential advantages of this technique have yet to be definitively proven in large, prospective studies. However, the likely advantages are many. MRI/US fusion guided biopsy may result in lower prostate specific mortality, as fewer cases of high grade but localized disease are missed. Existing studies of nearly every MRI/US fusion guided biopsy platform have shown an increase in the amount of high grade PCa that can be detected. The epidemiological significance of this finding should be examined prospectively once MRI/US fusion guided biopsy is deployed on a wider scale.
Fusion biopsy has the potential to decrease what is now recognized as pervasive overtreatment of low risk PCa. This possible reduction is based on the finding that MRI characteristics correlate with the D’Amico risk score and the biopsy Gleason grade.19,27 If MRI/US fusion guided biopsy is shown to accurately depict prostate pathology in large, prospective studies, urologists may become more comfortable using this technology to monitor patients with low risk disease.
MRI/US fusion guided biopsy offers a more rational approach to active surveillance. Other than cognitive fusion, nearly all fusion platforms allow for resampling of sites that have been targeted in the past. Perhaps beginning with this context, targeted biopsies may begin to replace random systematic biopsies altogether. Eventually, active surveillance protocols could even incorporate MRI instead of biopsy at certain followup intervals, which is not only appealing to patients, but could reduce the prevalence of post-biopsy infection as well.28 Finally, MRI/US fusion guided biopsy not only improves our ability to identify patients who are candidates for focal therapy, but also allows us to effectively monitor treatment response. This potential role for fusion biopsy was recently strongly endorsed by a consensus panel.29
Conclusions
Advancements in modern imaging have led MP-MRI to become the gold standard for the noninvasive detection of PCa. This powerful technology can be used for direct in-bore MRI guided biopsy, cognitive fusion with TRUS and MRI/US fusion guided biopsy. This last technique has generated significant interest, leading to a recent proliferation of various MRI/US fusion platforms. The initial studies of nearly all of these platforms are consistent in that MRI/US fusion guided biopsy detects a larger amount of clinically significant PCa than the current standard of care TRUS guided biopsy. These developments have exciting implications for patient selection for definitive treatment, appropriate PCa screening, active surveillance and focal therapy.
Further research in 3 key areas will lead to an even wider adoption of targeted biopsy. 1) The radiology community must develop a robust, uniform grading and reporting system for PCa on MP-MRI. Current reporting systems are useful but their wide variability precludes meaningful comparisons among centers.30 2) Prospective, randomized studies are needed to compare fusion platforms. Although comparative studies exist, they generally contain heterogeneous groups of patients, present conflicting results or include small sample sizes with trends toward statistical significance that could be better assessed in larger studies.15,22,31 3) Existing models for PCa prognostication based on the results of random biopsies may need to be revisited. For example, now that targeted cores almost uniformly contain a greater percentage of PCa, it is possible that this criterion for deciding which PCa is clinically significant may no longer be meaningful.32,33 Total tumor volume has been proposed as a better criterion, although disagreement exists as to how this should be measured and implemented.
Improvements in these 3 areas have the potential to truly make the combination of MP-MRI and targeted biopsy, such as MRI/US fusion guided biopsy, the new standard of care for men with PCa. For many years the prostate has been the last example of a solid organ randomly sampled in patients with a suspicion of cancer. Targeted prostate biopsy has the potential to finally change this practice.
Acknowledgments
This research was supported by the Intramural Research Program of the National Institutes of Health, National Cancer Institute, Center for Cancer Research and the Center for Interventional Oncology. NIH and Philips Healthcare have a cooperative research and development agreement. NIH and Philips Healthcare share intellectual property in the field. This research was also made possible through the NIH Medical Research Scholars Program, a public-private partnership supported jointly by the NIH and generous contributions to the Foundation for the NIH from Pfizer Inc., the Doris Duke Charitable Foundation, Alexandria Real Estate Equities, Inc. and Mr. and Mrs. Joel S. Marcus, and the Howard Hughes Medical Institute, as well as other private donors. For a complete list, please visit the Foundation website at http://fnih.org/work/education-training-0/medical-research-scholars-program.
Abbreviations and Acronyms
- 3D
3-dimensional
- DRE
digital rectal examination
- MP
multiparametric prostate
- MR
magnetic resonance
- MRI
magnetic resonance imaging
- NIH
National Institutes of Health
- PCa
prostate cancer
- PSA
prostate specific antigen
- TRUS
transrectal ultrasound
- US
ultrasound
References
- 1.Kaufman JJ, Rosenthal M, Goodwin WE. Needle biopsy in diagnosis of prostatic cancer. Calif Med. 1954;81:308. [PMC free article] [PubMed] [Google Scholar]
- 2.Colston JA. Carcinoma of the prostate. JAMA. 1943;122:781. [Google Scholar]
- 3.Krahn MD, Mahoney JE, Eckman MH, et al. Screening for prostate cancer. A decision analytic view. JAMA. 1994;272:773. [PubMed] [Google Scholar]
- 4.Watanabe H, Igari D, Tanahasi Y, et al. Development and application of new equipment for transrectal ultrasonography. J Clin Ultrasound. 1974;2:91. doi: 10.1002/jcu.1870020203. [DOI] [PubMed] [Google Scholar]
- 5.Hodge KK, McNeal JE, Terris MK, et al. Random systematic versus directed ultrasound guided transrectal core biopsies of the prostate. J Urol. 1989;142:71. doi: 10.1016/s0022-5347(17)38664-0. [DOI] [PubMed] [Google Scholar]
- 6.Yeo L, Patel D, Bach C, et al. The development of the modern prostate biopsy. In: Bissada NK, editor. Prostate Biopsy. Rijeka, Croatia: InTech; 2011. pp. 1–19. Available at www.intechopen.com/books/prostate-biopsy/the-development-of-the-modern-prostate-biopsy. [Google Scholar]
- 7.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63:11. doi: 10.3322/caac.21166. [DOI] [PubMed] [Google Scholar]
- 8.Presti JC, Jr, O’Dowd GJ, Miller MC, et al. Extended peripheral zone biopsy schemes increase cancer detection rates and minimize variance in prostate specific antigen and age related cancer rates: results of a community multi-practice study. J Urol. 2003;169:125. doi: 10.1016/S0022-5347(05)64051-7. [DOI] [PubMed] [Google Scholar]
- 9.Loeb S, Carter HB, Berndt SI, et al. Complications after prostate biopsy: data from SEER-Medicare. J Urol. 2011;186:1830. doi: 10.1016/j.juro.2011.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.D’Amico AV, Schnall M, Whittington R, et al. Endorectal coil magnetic resonance imaging identifies locally advanced prostate cancer in select patients with clinically localized disease. Urology. 1998;51:449. doi: 10.1016/s0090-4295(97)00630-4. [DOI] [PubMed] [Google Scholar]
- 11.Turkbey B, Merino MJ, Gallardo EC, et al. Comparison of endorectal coil and nonendorectal coil T2W and diffusion-weighted MRI at 3 Tesla for localizing prostate cancer: correlation with whole-mount histopathology. J Magn Reson Imaging. 2013 doi: 10.1002/jmri.24317. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Turkbey B, Mani H, Shah V, et al. Multiparametric 3T prostate magnetic resonance imaging to detect cancer: histopathological correlation using prostatectomy specimens processed in customized magnetic resonance imaging based molds. J Urol. 2011;186:1818. doi: 10.1016/j.juro.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoeks CM, Barentsz JO, Hambrock T, et al. Prostate cancer: multi-parametric MR imaging for detection, localization, and staging. Radiology. 2011;261:46. doi: 10.1148/radiol.11091822. [DOI] [PubMed] [Google Scholar]
- 14.Hambrock T, Hoeks C, Hulsbergen-van de Kaa C, et al. Prospective assessment of prostate cancer aggressiveness using 3-T diffusion-weighted magnetic resonance imaging-guided biopsies versus a systematic 10-core transrectal ultrasound prostate biopsy cohort. Eur Urol. 2012;61:177. doi: 10.1016/j.eururo.2011.08.042. [DOI] [PubMed] [Google Scholar]
- 15.Wysock JS, Rosenkrantz AB, Huang WC, et al. A prospective, blinded comparison of magnetic resonance (MR) imaging-ultrasound fusion and visual estimation in the performance of MR-targeted prostate biopsy: the PROFUS trial. Eur Urol. 2013 doi: 10.1016/j.eururo.2013.10.048. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 16.Sparks R, Bloch BN, Feleppa E, et al. Fully automated prostate magnetic resonance imaging and transrectal ultrasound fusion via a probabilistic registration metric. Proc Soc Photo Opt Instrum Eng. 2013;8671:1. doi: 10.1117/12.2007610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rastinehad AR, Turkbey B, Salami SS, et al. Improving detection of clinically significant prostate cancer: MRI/TRUS fusion-guided prostate biopsy. J Urol. 2013 doi: 10.1016/j.juro.2013.12.007. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siddiqui MM, Rais-Bahrami S, Truong H, et al. Magnetic resonance imaging/ultrasound-fusion biopsy significantly upgrades prostate cancer versus systematic 12-core transrectal ultrasound biopsy. Eur Urol. 2013;64:713. doi: 10.1016/j.eururo.2013.05.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rais-Bahrami S, Siddiqui MM, Turkbey B, et al. Utility of multiparametric magnetic resonance imaging suspicion levels for detecting prostate cancer. J Urol. 2013;190:1721. doi: 10.1016/j.juro.2013.05.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pinto PA, Chung PH, Rastinehad AR, et al. Magnetic resonance imaging/ultrasound fusion guided prostate biopsy improves cancer detection following transrectal ultrasound biopsy and correlates with multiparametric magnetic resonance imaging. J Urol. 2011;186:1281. doi: 10.1016/j.juro.2011.05.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sonn GA, Natarajan S, Margolis DJ, et al. Targeted biopsy in the detection of prostate cancer using an office based magnetic resonance ultrasound fusion device. J Urol. 2013;189:86. doi: 10.1016/j.juro.2012.08.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Delongchamps NB, Peyromaure M, Schull A, et al. Prebiopsy magnetic resonance imaging and prostate cancer detection: comparison of random and targeted biopsies. J Urol. 2013;189:493. doi: 10.1016/j.juro.2012.08.195. [DOI] [PubMed] [Google Scholar]
- 23.Kuru TH, Roethke MC, Seidenader J, et al. Critical evaluation of magnetic resonance imaging targeted, transrectal ultrasound guided trans-perineal fusion biopsy for detection of prostate cancer. J Urol. 2013;190:1380. doi: 10.1016/j.juro.2013.04.043. [DOI] [PubMed] [Google Scholar]
- 24.Miyagawa T, Ishikawa S, Kimura T, et al. Real-time virtual sonography for navigation during targeted prostate biopsy using magnetic resonance imaging data. Int J Urol. 2010;17:855. doi: 10.1111/j.1442-2042.2010.02612.x. [DOI] [PubMed] [Google Scholar]
- 25.Moore CM, Robertson NL, Arsanious N, et al. Image-guided prostate biopsy using magnetic resonance imaging-derived targets: a systematic review. Eur Urol. 2013;63:125. doi: 10.1016/j.eururo.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 26.Logan JK, Rais-Bahrami S, Turkbey B, et al. Current status of MRI and ultrasound fusion software platforms for guidance of prostate biopsies. BJU Int. 2013 doi: 10.1111/bju.12593. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rastinehad AR, Baccala AA, Jr, Chung PH, et al. D’Amico risk stratification correlates with degree of suspicion of prostate cancer on multi-parametric magnetic resonance imaging. J Urol. 2011;185:815. doi: 10.1016/j.juro.2010.10.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stamatakis L, Siddiqui MM, Nix JW, et al. Accuracy of multiparametric magnetic resonance imaging in confirming eligibility for active surveillance for men with prostate cancer. Cancer. 2013;119:3359. doi: 10.1002/cncr.28216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Muller BG, Fütterer JJ, Gupta RT, et al. The role of magnetic resonance imaging in focal therapy for prostate cancer: recommendations from a consensus panel. BJU Int. 2013 doi: 10.1111/bju.12243. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dickinson L, Ahmed HU, Allen C, et al. Scoring systems used for the interpretation and reporting of multiparametric MRI for prostate cancer detection, localization, and characterization: could standardization lead to improved utilization of imaging within the diagnostic pathway? J Magn Reson Imaging. 2013;37:48. doi: 10.1002/jmri.23689. [DOI] [PubMed] [Google Scholar]
- 31.Puech P, Rouvière O, Renard-Penna R, et al. Prostate cancer diagnosis: multiparametric MR-targeted biopsy with cognitive and transrectal US-MR fusion guidance versus systematic biopsy–prospective multicenter study. Radiology. 2013;268:461. doi: 10.1148/radiol.13121501. [DOI] [PubMed] [Google Scholar]
- 32.Haffner J, Lemaitre L, Puech P, et al. Role of magnetic resonance imaging before initial biopsy: comparison of magnetic resonance imaging-targeted and systematic biopsy for significant prostate cancer detection. BJU Int. 2011;108:E171. doi: 10.1111/j.1464-410X.2011.10112.x. [DOI] [PubMed] [Google Scholar]
- 33.Robertson NL, Hu Y, Ahmed HU, et al. Prostate cancer risk inflation as a consequence of image-targeted biopsy of the prostate: a computer simulation study. Eur Urol. 2014;65:628. doi: 10.1016/j.eururo.2012.12.057. [DOI] [PMC free article] [PubMed] [Google Scholar]