Abstract
Background
A low ratio of utilization of healthcare services in postpartum women may contribute to maternal deaths during the postpartum period. The maternal mortality ratio is high in the Philippines. The aim of this study was to examine the current utilization of healthcare services and the effects on the health of women in the Philippines who delivered at home.
Methods
This was a cross-sectional analytical study, based on a self-administrated questionnaire, conducted from March 2015 to February 2016 in Muntinlupa, Philippines. Sixty-three postpartum women who delivered at home or at a facility were enrolled for this study. A questionnaire containing questions regarding characteristics, utilization of healthcare services, and abnormal symptoms during postpartum period was administered. To analyze the questionnaire data, the sample was divided into delivery at home and delivery at a facility. Chi-square test, Fisher’s exact test, and Mann–Whitney U test were used.
Results
There were significant differences in the type of birth attendant, area of residence, monthly income, and maternal and child health book usage between women who delivered at home and those who delivered at a facility (P<0.01). There was significant difference in the utilization of antenatal checkup (P<0.01) during pregnancy, whilst there was no significant difference in utilization of healthcare services during the postpartum period. Women who delivered at home were more likely to experience feeling of irritated eyes and headaches, and continuous abdominal pain (P<0.05).
Conclusion
Financial and environmental barriers might hinder the utilization of healthcare services by women who deliver at home in the Philippines. Low utilization of healthcare services in women who deliver at home might result in more frequent abnormal symptoms during postpartum.
Keywords: Philippines, health care services, postpartum, delivery at home, danger signs, abnormal symptoms
Background
Maternal mortality ratio (MMR) in the Philippines dropped from 170 (per 100,000 live births) in 2003 to 114 in 2015. Although this ratio has undergone a slow decrease over time, it remains unacceptably high.1–3
The major causes of maternal death in the Philippines are complications during pregnancy, delivery, and the postpartum period (ie, pregnancy-induced hypertension, postpartum hemorrhage, and puerperal infection).4,5 This indicates that many maternal deaths occur not only during pregnancy and delivery, but also during the postpartum period.6 In fact, approximately two-thirds of all maternal deaths occur during the postpartum period.7,8 In one study, the utilization of healthcare services in pregnant and postpartum women in the Philippines was observed to be 95.8% and 62.3%, respectively.9 It is possible that a lower ratio of healthcare service utilization in postpartum women may contribute to maternal deaths during the postpartum period. Furthermore, it has been reported that women who delivered at home showed a lower ratio of postpartum healthcare service utilization than women who delivered in facilities.10 A ratio of home deliveries in the Philippines had decreased from 56% in 2008 to 38% in 2013, but it remains still high.9 Therefore, the provision of health-care services to postpartum women who deliver at home might be important for reducing MMR in the Philippines. However, there are no reports regarding the outcome of utilization of healthcare services on the health condition of postpartum women who deliver at home in the Philippines. Therefore, we conducted the present study to examine the current utilization of healthcare services, and its effects on the health of women who deliver at home in the Philippines.
Methods
Participants
This was a cross-sectional analytical study based on self-administered questionnaires. Postpartum women who delivered at home or a facility were enrolled in this study, which was conducted from March 2015 to February 2016 in Muntinlupa, Philippines. Muntinlupa is located in the Luzon region and divided into 9 districts, with a total population of 504,509 in 2015.11
To increase the sample size, we chose two approaches to distribute questionnaires. During daily home visits, community health volunteers who were registered at the Muntinlupa City Health Center distributed the questionnaires to 50 postpartum women (Group A), whilst staff members of the Health Center also distributed the questionnaires to 50 postpartum women and immunized their babies at the Health Center (Group B). Women who had non-obstetrical complications and did not consent to the study were excluded. Consequently, 63 postpartum women participated in this study (Figure 1).
Figure 1.
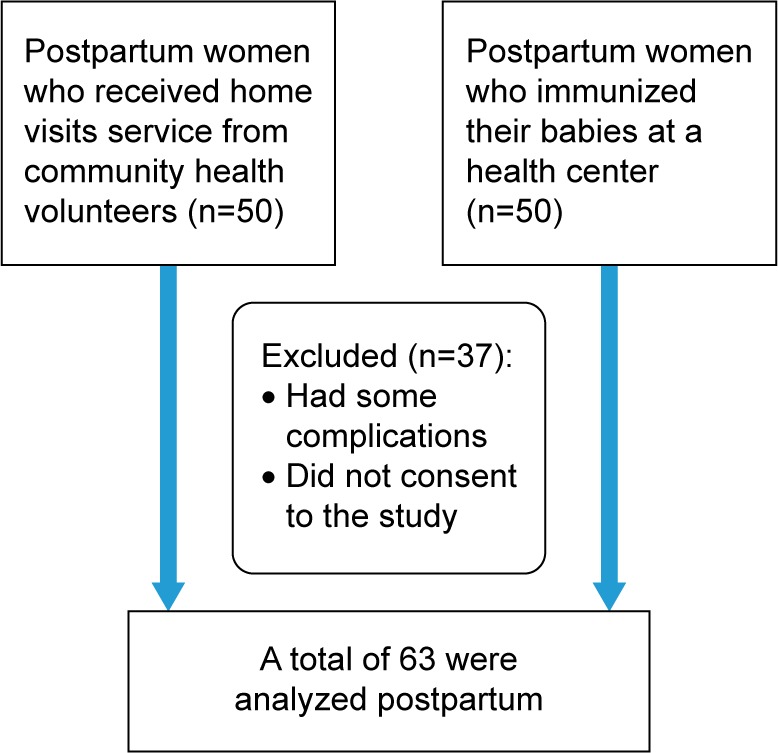
Sampling design.
Ethics approval and consent to participate
All participants provided written informed consent prior to participation in the study. The Ethical Committee of Kobe University Graduate School of Health Sciences, Japan and Muntinlupa City Health Office approved the study protocol.
Self-reported questionnaire
The questionnaire contained questions on characteristics, utilization of healthcare services, and abnormal symptoms during postpartum. The category of characteristics included questions on age, days after delivery, parity (primipara/multipara), type of birth attendant (skilled birth attendant/traditional birth attendant [TBA]), area of residence (Poblacion/Putatan), education (primary or middle school/high school/college or university), employment status of husband (unemployed/white-collar occupation [professional service, production worker] or blue-collar occupation [agricultural worker, laborer, farmer]), monthly income (<2,499 or >2,500 Philippine peso), health insurance, maternal and child health book usage, and access to health centers. The category of healthcare services during pregnancy included questions on antenatal checkup, home visiting service, vaccination of tetanus toxoid, supply of iron and folic acid, and health education (ie, danger signs and breastfeeding problems in pregnancy). The category of postpartum healthcare services included questions on postpartum checkups, home visiting service, and health education (ie, postpartum danger signs, breastfeeding problems, and family planning). The breastfeeding problems during pregnancy and postpartum periods were mastitis, insufficient breastfeeding, and cracked or sore nipples. The abnormal symptoms during postpartum period were examined with the following seven statements adapted from our previous research:10 1) fever (>38°C) for more than 2 days, 2) bad lochia odor, 3) irritated eyes and headaches, 4) continuous abdominal pain with increasing intensity, 5) pain in the breast, reddening of skin around the breast, and an observed spike in fever during the evening, 6) high blood pressure and dizziness, and 7) low mood and aversion to child-rearing or housework.12 Participants were asked to respond to each of the symptom statements by choosing one of two responses: present or absent.
Statistical analysis
Sixty-three subjects (27 and 36 women who delivered at home and a facility, respectively) were included in the data analysis. Chi-square test and Fisher’s exact test were used for analyzing categorical variables, whilst Mann–Whitney U test was used for continuous variables. To analyze the questionnaire data, the sample was divided into two: delivery at home and delivery at a facility. Analyses were two-tailed, with a P-value <0.05 considered significant. Statistical analyses were performed using the Statistical Package for the Social Sciences version 23 (IBM Inc., Chicago, IL, USA).
Results
Participant characteristics
The mean age (mean ± standard deviation) of women who delivered at home and a facility was 26.1±7.1 years and 27.2±6.4 years, respectively. The mean days after delivery in women who delivered at home and a facility was 33.3±23.1 days and 38.3±21.2 days, respectively. There were significant differences in the type of birth attendant, area of residence, monthly income, and maternal and child health book usage (P<0.01), but not parity, education, employment, health insurance, and time to a health center between women who underwent delivery at home and a facility (Table 1).
Table 1.
Characteristics of study participants
| Characteristics | Home, n=27 (%) | Facility, n=36 (%) | P-value |
|---|---|---|---|
| Age (years) | 0.45 | ||
| Mean ± SD | 26.1±7.1 | 27.2±6.4 | |
| Days after delivery | 0.47 | ||
| Mean ± SD | 33.3±23.1 | 38.3±21.2 | |
| Parity | 1.00 | ||
| Primipara | 6 (22.2) | 9 (25.0) | |
| Multipara | 21 (77.8) | 27 (75.0) | |
| Birth attendant | <0.01 | ||
| Skilled birth attendant | 9 (33.3) | 35 (97.2) | |
| Traditional birth attendant | 18 (66.7) | 1 (2.8) | |
| Area of residence | <0.01 | ||
| Poblacion | 4 (14.8) | 22 (61.1) | |
| Putatan | 23 (85.2) | 14 (38.9) | |
| Mother’s education | 0.38 | ||
| Primary or middle school | 4 (14.8) | 4 (11.1) | |
| High school | 20 (74.1) | 23 (63.9) | |
| College or university | 3 (11.1) | 9 (25.0) | |
| Father’s education | 0.34 | ||
| Primary or middle school | 4 (15.4) | 3 (8.3) | |
| High school | 20 (76.9) | 26 (72.2) | |
| College or university | 2 (7.7) | 7 (19.4) | |
| Monthly income (Philippines peso) | <0.01 | ||
| <2,499 | 22 (81.5) | 15 (41.7) | |
| >2,500 | 5 (18.5) | 21 (58.3) | |
| Health insurance | 0.22 | ||
| Have | 10 (37.0) | 18 (50.0) | |
| Do not have | 17 (63.0) | 18 (50.0) | |
| Maternal and child health book | <0.01 | ||
| Have | 9 (33.3) | 33 (91.7) | |
| Do not have | 18 (66.7) | 3 (8.3) | |
| Time to health center (minutes) | 0.97 | ||
| Mean ± SD | 24.1±18.4 | 22.2±10.1 |
Note: P-values were derived from chi-square test, Fisher’s exact test, and Mann–Whitney U test.
Abbreviation: SD, standard deviation.
Utilization of healthcare services during pregnancy
There were significant differences in the utilization of antenatal checkup (P<0.01), but not home visiting service, tetanus toxoid, iron and folic acid supply, health education on danger signs in pregnancy, and health education on breastfeeding troubles between women who delivered at home and those who did at a facility (Table 2).
Table 2.
Healthcare service utilization during pregnancy in women who delivered at home or at a facility in the Philippines
| Category | Home, n=27 (%) | Facility, n=36 (%) | P-value |
|---|---|---|---|
| Antenatal checkup | <0.01 | ||
| >4 times | 10 (37.0) | 28 (77.8) | |
| 1–3 times | 10 (37.0) | 7 (19.4) | |
| Not received | 7 (25.9) | 1 (2.8) | |
| Home visit | 0.30 | ||
| Received | 15 (55.6) | 25 (69.4) | |
| Not received | 12 (44.4) | 11 (30.6) | |
| Tetanus toxoid | 0.21 | ||
| Received | 23 (85.2) | 34 (94.4) | |
| Not received | 4 (14.8) | 2 (5.6) | |
| Iron | 0.28 | ||
| Received | 25 (92.6) | 29 (80.6) | |
| Not received | 2 (7.4) | 7 (19.4) | |
| Folic acid | 0.33 | ||
| Received | 24 (88.9) | 28 (77.8) | |
| Not received | 3 (11.1) | 8 (22.2) | |
| Health education on danger signs in pregnancy | 1.00 | ||
| Received | 21 (77.8) | 29 (80.6) | |
| Not received | 6 (22.2) | 7 (19.4) | |
| Health education on breastfeeding problems | 0.53 | ||
| Received | 20 (74.1) | 30 (83.3) | |
| Not received | 7 (25.9) | 6 (16.7) |
Note: P-values were derived from chi-square test and Fisher’s exact test.
Utilization of healthcare services during postpartum period
There were no significant differences in time of first postpartum checkup, home visiting service, health education on postpartum danger signs, health education on breastfeeding troubles, and health education on family planning between both groups of postpartum women (Table 3).
Table 3.
Healthcare service utilization during postpartum in women who delivered at home or at a facility in the Philippines
| Category | Home, n=27 (%) | Facility, n=36 (%) | P-value |
|---|---|---|---|
| Time of first postpartum checkup | 0.16 | ||
| Within 4 hours | 6 (22.2) | 5 (13.9) | |
| Within 4–24 hours | 6 (22.2) | 3 (8.3) | |
| Within 2 days | 13 (48.1) | 27 (75.0) | |
| Not received | 2 (7.4) | 1 (2.8) | |
| Home visit | 1.00 | ||
| Received | 18 (66.7) | 24 (66.7) | |
| Not received | 9 (33.3) | 12 (33.3) | |
| Health education on postpartum danger signs | 1.00 | ||
| Received | 18 (66.7) | 24 (66.7) | |
| Not received | 9 (33.3) | 12 (33.3) | |
| Health education on breastfeeding troubles | 0.43 | ||
| Received | 20 (74.1) | 23 (63.9) | |
| Not received | 7 (25.9) | 13 (36.1) | |
| Health education on family planning | 0.55 | ||
| Received | 22 (81.5) | 26 (72.2) | |
| Not received | 5 (18.5) | 10 (27.8) |
Note: P-values were derived from chi-square test and Fisher’s exact test.
Presence of abnormal symptoms during postpartum period
There were significant differences in the feeling of irritated eyes and headaches and continuous abdominal pain (P<0.05), but not fever for more than 2 days, bad lochia odor, breast pain, high blood pressure, and dizziness with a low mood state between both groups of women (Table 4).
Table 4.
Postpartum abnormal symptoms in women who delivered at home or at a facility in the Philippines
| Category | Home, n=27 (%) | Facility, n=36 (%) | P-value |
|---|---|---|---|
| Fever for >2 days | 0.31 | ||
| Present | 3 (11.1) | 1 (2.8) | |
| Absent | 24 (88.9) | 35 (97.2) | |
| Bad lochia odor | 1.00 | ||
| Present | 1 (3.7) | 2 (5.6) | |
| Absent | 26 (96.3) | 34 (94.4) | |
| Irritated eyes and headaches | 0.03 | ||
| Present | 10 (37.0) | 4 (11.1) | |
| Absent | 17 (63.0) | 32 (88.9) | |
| Continuous abdominal pain | 0.04 | ||
| Present | 6 (22.2) | 1 (2.8) | |
| Absent | 21 (77.8) | 35 (97.2) | |
| Breast pain | 0.48 | ||
| Present | 5 (18.5) | 4 (11.1) | |
| Absent | 22 (81.5) | 32 (88.9) | |
| High blood pressure and dizziness | 1.00 | ||
| Present | 1 (3.9) | 1 (2.8) | |
| Absent | 26 (96.3) | 35 (97.2) | |
| State of low mood | 1.00 | ||
| Present | 1 (3.7) | 1 (2.8) | |
| Absent | 26 (96.3) | 35 (97.2) |
Note: P-values were derived from chi-square test and Fisher’s exact test.
Discussion
In this study, we demonstrated that postpartum women who delivered at home had lower financial status, were assisted by TBA, and demonstrated lower utilization of the maternal and child health book. We also found that postpartum women who delivered at home did not have access to adequate antenatal checkups and health education during pregnancy as well as sufficient home visiting service and health education during the postpartum period. The lower utilization of healthcare services in women who delivered at home might have contributed to a high frequency of abnormal symptoms during the postpartum period.
In our study, lower financial status was significantly related to deliveries at home that were assisted by TBAs, but access to health center was not significantly related to it. Previous researchers have reported that women who delivered at home in the Philippines, Indonesia, Vietnam, India, Bangladesh, Nigeria, Nepal, Tanzania, and Kenya had social, cultural, and financial barriers.13–25 Financial status is one of the main determinants of the choice for women to deliver at home.9 However, it has been reported that the majority of women who delivered at home felt that this option was more comfortable and convenient.26–28 Therefore, the factors of deliveries at home were not only financial status and transportation, but also comfort and convenience on them. The maternal and child health book was generally distributed to women at health facilities in the Philippines. Accordingly, the women who delivered at home lacked the opportunity to access it. Yanagisawa et al reported that the maternal and child health book could be useful for maintaining good health in pregnant women.29,30 Therefore, it is important to provide this book to women who deliver at home to help improve their health.
A previous study reported that 84% of pregnant women received antenatal checkups in the Philippines.9 However, in this study, women who delivered at home did not receive sufficient antenatal checkups during pregnancy, compared to those who delivered at a facility. On the other hand, during the postpartum period, there were no differences in the utilization of healthcare services between both groups. However, health education on danger signs was not sufficient for women who delivered at home. Wilunda et al reported that financial status, knowledge, attitude, and perceived good quality of maternal health care could be positively associated with utilization of health care services.31 In addition, Choe et al demonstrated that physical, cultural, or familial influence could dissuade women from receiving healthcare services.23 Therefore, this study demonstrated that deliveries assisted by TBAs and lower maternal and child health book utilization might also contribute to a lower utilization of healthcare services during pregnancy and in the postpartum period.
According to the current findings, women who delivered at home had more abnormal symptoms related to postpartum hypertension and postpartum infection than women who delivered at a facility. Belda and Gebremariam reported that women who delivered at home were not adequately prepared for postpartum complications.32 Therefore, the lower utilization of healthcare services by these women might have resulted in higher abnormal postpartum symptoms.
Barangay Health Workers (BHWs), who are registered health volunteers at the Health Center in the Philippines, provide support to women who live in the community.33 We reported that BHWs could efficiently evaluate a woman’s physical and mental condition through their home visiting services.34 Therefore, BHWs play an important role in assessing healthcare service utilization and postpartum health conditions in women who deliver at home in the Philippines. Health education on danger signs which is provided not only by professionals, but also by BHWs, could enhance knowledge and attitudes in postpartum women, which could ultimately enrich their health in the Philippines.
Our study had several limitations. Our sample size was small and the study region was limited. However, this is the first study to evaluate the effect of healthcare service utilization on health conditions of women who deliver at home in the Philippines.
Conclusion
In conclusion, we found that financial and environmental barriers might hinder the utilization of healthcare services in women who deliver at home in the Philippines. A lower utilization of healthcare services in these women might result in higher abnormal postpartum symptoms. These symptoms may contribute to the MMR in the Philippines. In the Philippines, the provision of health education on abnormal symptoms can enhance knowledge and attitudes in postpartum women, which can ultimately enrich their health.
Acknowledgments
The authors would like to acknowledge the support of the Muntinlupa City Health Center staff and the Barangay Health Workers at the Putatan Health Center. They would also like to acknowledge all study participants and their families who kindly cooperated in this study. This work was supported by the Japan Society for the Promotion of Science KAKENHI, grant number 15K20811.
Footnotes
Author contributions
TY and HM analyzed study data and contributed materials and analytical tools. All of the authors contributed to the concept and design of this study, performed the experiments, contributed toward data analysis, drafted the manuscript, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division Trends in maternal mortality. 1990 to 2015. 2015. [Accessed 18 May, 2016]. Available from: http://apps.who.int/iris/bitstream/10665/194254/1/9789241565141_eng.pdf.
- 2.The United Nations The millennium development goals report 2015–2015. [Accessed 18 May, 2016]. Available from: http://www.un.org/millenniumgoals/2015_MDG_Report/pdf/MDG%202015%20rev%20%28July%201%29.pdf.
- 3.Republic of the Philippines, Department of Health Mortality 2013. [Accessed 9 May, 2017]. Available from: http://www.doh.gov.ph/mortality.
- 4.World Health Organization WHO recommendations for the prevention and treatment of postpartum haemorrhage. 2012. [Accessed 18 May, 2016]. Available from: http://apps.who.int/iris/bitstream/10665/75411/1/9789241548502_eng.pdf. [PubMed]
- 5.Republic of the Philippines Department of Health National Epidemiology Center Manila The 2010 Philippine health statistics. 2010. [Accessed 18 May, 2016]. Available from: http://www.doh.gov.ph/sites/default/files/publications/PHS2010_March13.compressed.pdf.
- 6.Li XF, Fortney JA, Kotelchuck M, Glover LH. The postpartum period: the key to maternal mortality. Int J Gynaecol Obstet. 1996;54(1):1–10. doi: 10.1016/0020-7292(96)02667-7. [DOI] [PubMed] [Google Scholar]
- 7.Zupan J. Perinatal mortality in developing countries. N Engl J Med. 2005;352(20):2047–2048. doi: 10.1056/NEJMp058032. [DOI] [PubMed] [Google Scholar]
- 8.Ronsmans C, Graham WJ, Lancet Maternal Survival Series steering group Maternal mortality: who, when, where, and why. Lancet. 2006;368(9542):1189–1200. doi: 10.1016/S0140-6736(06)69380-X. [DOI] [PubMed] [Google Scholar]
- 9.Philippine Statistics Authority Philippines-national demographic and health survey 2013. 2013. [Accessed 18 May, 2016]. Available from: https://dhsprogram.com/pubs/pdf/FR294/FR294.pdf.
- 10.Yamashita T, Suplido SA, Ladines-Llave C, Tanaka Y, Senba N, Matsuo H. A cross-sectional analytic study of postpartum health care service utilization in the Philippines. PLoS One. 2014;9(1):e85627. doi: 10.1371/journal.pone.0085627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Philippines Statistics Authority Highlights of the Philippine population 2015 census of population. [Accessed 5 May, 2017]. Available from: https://psa.gov.ph/content/highlights-philippine-population-2015-census-population.
- 12.World Health Organization WHO recommendations on postpartum care of the mother and newborn: a practical guide. 2013. [Accessed 5 May, 2017]. Available from: http://apps.who.int/iris/bitstream/10665/97603/1/9789241506649_eng.pdf.
- 13.Lee RB, Abellera M, Triunfante CC, Mirandilla MEL. Utilization of maternal health care services among low-income Filipino women, with special reference to Bicol region. Asia-Pacific E-Journal Health Soc Sci. 2012;1(1):1–7. [Google Scholar]
- 14.Sobel HL, Oliveros YE, Nyunt-U S. Secondary analysis of a national health survey on factors influencing women in the Philippines to deliver at home and unattended by a healthcare professional. Int J Gynaecol Obstet. 2010;111(2):157–160. doi: 10.1016/j.ijgo.2010.06.020. [DOI] [PubMed] [Google Scholar]
- 15.Titaley CR, Dibley MJ, Roberts CL. Factors associated with non-utilisation of postnatal care services in Indonesia. J Epidemiol Community Health. 2009;63(10):827–831. doi: 10.1136/jech.2008.081604. [DOI] [PubMed] [Google Scholar]
- 16.Titaley CR, Hunter CL, Dibley MJ, Heywood P. Why do some women still prefer traditional birth attendants and home delivery?: a qualitative study on delivery care services in West Java Province, Indonesia. BMC Pregnancy Childbirth. 2010;10:43. doi: 10.1186/1471-2393-10-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sepehri A, Sarma S, Simpson W, Moshiri S. How important are individual, household and commune characteristics in explaining utilization of maternal health services in Vietnam? Soc Sci Med. 2008;67(6):1009–1017. doi: 10.1016/j.socscimed.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 18.Singh A, Kumar A, Pranjali P. Utilization of maternal healthcare among adolescent mothers in urban India: evidence from DLHS-3. PeerJ. 2014;2:e592. doi: 10.7717/peerj.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taleb F, Perkins J, Ali NA, et al. Transforming maternal and newborn health social norms and practices to increase utilization of health services in rural Bangladesh: a qualitative review. BMC Pregnancy Childbirth. 2015;15:75. doi: 10.1186/s12884-015-0501-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chakraborty N, Islam MA, Chowdhury RI, Bari W, Akhter HH. Determinants of the use of maternal health services in rural Bangladesh. Health Promot Int. 2003;18(4):327–337. doi: 10.1093/heapro/dag414. [DOI] [PubMed] [Google Scholar]
- 21.Babalola S, Fatusi A. Determinants of use of maternal health services in Nigeria – looking beyond individual and household factors. BMC Pregnancy Childbirth. 2009;9:43. doi: 10.1186/1471-2393-9-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sharma SR, Poudyal AK, Devkota BM, Singh S. Factors associated with place of delivery in rural Nepal. BMC Public Health. 2014;14:306. doi: 10.1186/1471-2458-14-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Choe SA, Kim J, Kim S, Park Y, Kullaya SM, Kim CY. Do antenatal care visits always contribute to facility-based delivery in Tanzania? A study of repeated cross-sectional data. Health Policy Plan. 2016;31(3):277–284. doi: 10.1093/heapol/czv054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kitui J, Lewis S, Davey G. Factors influencing place of delivery for women in Kenya: an analysis of the Kenya demographic and health survey, 2008/2009. BMC Pregnancy Childbirth. 2013;13:40. doi: 10.1186/1471-2393-13-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Finlayson K, Downe S. Why do women not use antenatal services in low-and middle-income countries? A meta-synthesis of qualitative studies. PLoS Med. 2013;10(1):e1001373. doi: 10.1371/journal.pmed.1001373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jiang H, Qian X, Chen L, et al. Towards universal access to skilled birth attendance: the process of transforming the role of traditional birth attendants in Rural China. BMC Pregnancy Childbirth. 2016;16:58. doi: 10.1186/s12884-016-0854-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Godlonton S, Okeke EN. Does a ban on informal health providers save lives? Evidence from Malawi. J Dev Econ. 2016;118:112–132. doi: 10.1016/j.jdeveco.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim JM, Koh KW, Oak CH, Jung WH, Kim SH, Park DH. Assessment of village health worker training program in Tuguegarao, Philippine. J Prev Med Public Health. 2009;42(6):377–385. doi: 10.3961/jpmph.2009.42.6.377. [DOI] [PubMed] [Google Scholar]
- 29.Yanagisawa S, Soyano A, Igarashi H, Ura M, Nakamura Y. Effect of a maternal and child health handbook on maternal knowledge and behaviour: a community-based controlled trial in rural Cambodia. Health Policy Plan. 2015;30(9):1184–1192. doi: 10.1093/heapol/czu133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aiga H, Nguyen VD, Nguyen CD, Nguyen TT, Nguyen LT. Knowledge, attitude and practices: assessing maternal and child health care handbook intervention in Vietnam. BMC Public Health. 2016;16:129. doi: 10.1186/s12889-016-2788-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wilunda C, Quaglio G, Putoto G, et al. Determinants of utilisation of antenatal care and skilled birth attendant at delivery in South West Shoa Zone, Ethiopia: a cross sectional study. Reprod Health. 2015;12:74. doi: 10.1186/s12978-015-0067-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Belda SS, Gebremariam MB. Birth preparedness, complication readiness and other determinants of place of delivery among mothers in Goba District, Bale Zone, South East Ethiopia. BMC Pregnancy Childbirth. 2016;16:73. doi: 10.1186/s12884-016-0837-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Republic of the Philippines Republic Act 7883 – Barangay health workers’ benefits & incentives act of 1995. 1995. [Accessed 22 May, 2016]. Available from: http://www.officialgazette.gov.ph/1995/02/20/republic-act-no-7883/
- 34.Yamashita T, Suplido SA, Llave C, Tuliao MT, Tanaka Y, Matsuo H. Understanding postpartum healthcare services and exploring the challenges and motivations of maternal health service providers in the Philippines: a qualitative study. Trop Med Health. 2015;43(2):123–130. doi: 10.2149/tmh.2014-40. [DOI] [PMC free article] [PubMed] [Google Scholar]


