Abstract
The aim of this study was to analyze the correlation between high-intensity zone (HIZ) on magnetic resonance imaging (MRI) of a lumbar disc and positive pain response assessed by discography for the diagnosis and treatment of discogenic low back pain (LBP). Thirty-seven patients aged 21 to 59 years with chronic LBP but without any neurological symptoms or lumbar disc herniation who underwent MRI and subsequent discography were included in this study. During discography, concordant pain was regarded as positive, whereas discordant pain and no pain were regarded as negative. X-ray and computed tomography (CT) after discography with positive pain response were analyzed to correlate with HIZ on MRI. A total of 98 discs underwent discography in 37 patients; 21 discs presented positive pain response, including 10 with HIZ (47.6%). Seventy-seven discs presented negative pain response, including 29 with HIZ (37.6%). The high grade of annular disruption group shows a high proportion of HIZ on MRI. A positive correlation between HIZ and degree of annular disruption was observed. However, no correlation between HIZ and positive pain response was established on discography. The findings confirm that the presence of HIZ on MRI is only a suggestive and screening iconography indication for the diagnosis of discogenic LBP and cannot replace the gold standard of the discography. MRI should be closely integrated with those of discography, and thus, they play a crucial role in selecting operative segments of multilevel lumbar degenerative disk disease.
Keywords: diagnosis, high-intensity zone (HIZ), low back pain (LBP), lumbar discography
1. Introduction
Low back pain (LBP) associated with functional decline or disability is a common medical and social problem, also casting a cost-burden.[1–4] Several large and well-designed previous studies suggested that a history of LBP could serve as a robust predictor of future, severe LBP.[5,6] Discography as a pain provocation test is considered as the sole method to indicate a radiographic image of the patient's pain directly. From an empirical perspective, a discography is an optimal tool for evaluating discogenic LBP.[7–9] However, owing to its invasiveness, radiation exposure, and infectious risk, discography has continually been controversial.[10–12]
Magnetic resonance imaging (MRI) can accurately detect the morphological abnormalities of the degenerative discs. Although MRI was found to be sensitive in the identification of degenerative discs, it was unreliable in the case of the symptomatic disc. Some early studies have attempted to correlate the MRI features of disc degeneration with pain reproduction on discography; however, the results were controversial.[13–20]
The high-intensity zone (HIZ) was first described by Aprill and Bogduk[15] in lumbar spine MRI studies. HIZ is a high-intensity focal signal on T2-weighted sequences in the posterior annulus fibrosus with a considerably brighter signal intensity than nucleus pulposus that is distinctly dissociated.[16,19] Some investigators suggested that the presence of HIZ could be used as an indicator of annular tears and discogenic LBP on the image.[14–18,21] However, some other researchers speculated that the value of HIZ is limited to the diagnosis of discogenic LBP.[22–25] Therefore, in this study, we attempted to identify HIZ as an effective iconographic marker of annular tears and discogenic LBP. Also, whether HIZ can determine the discs of the proposed fusion segment that are symptomatic before fusion was investigated.
2. Methods
2.1. Patient population
This study was approved by the ethics statement of our hospital (First Affiliated Hospital of PLA General Hospital, Beijing). MRI and discography were performed on 37 chronic LBP patients who did not exhibit any typical symptoms, signs of radiculopathy, or protrusion of intervertebral disc on CT, as assessed by the same group of surgeons from October 2012 to December 2014. The cohort was composed of 26 males and 11 females, aged 21 to 59 (average 37.8) years, with constant LBP over 4 months before the discography and without satisfactory therapeutic response to conservative therapy. The intervertebral discs to be examined with discography were selected on the basis of MRI; these included 5 cases with a single segment of intervertebral disc degeneration, 8 with 2 segments of intervertebral disc degeneration, 19 with 3 segments of intervertebral disc degeneration, and 5 with 4 segments of intervertebral disc degeneration. Discography was performed on a total of 98 segments of intervertebral discs. Depressant administration and iodine allergy test were performed before the operation. The patients were placed in a prone position, and C-arm X-ray machine was used for the localization of discs. Under local anesthesia, a 22-gauge double-casing piped needle (15 cm) was punctured into the disc through anterolateral approach 8 to 10 cm off the spinous process. Nonionic contrast medium (Omnipaque; GE Healthcare) was used as a contrast agent that was administered under fluoroscopy. The injection of the contrast agent was terminated if the injection into the involved disc induced original pain in the patient or if it could not be injected due to resistance. The puncture needle was maintained stationary for 1 minute under sufficient pressure after the contrast agent was injected; then, the needle was extracted. Simultaneously, during the operation, silence was maintained in the operational environment, along with gentle actions, and the mental status of the patient was monitored. The discograms of adjacent 1 to 2 discs served as negative controls. The surgical procedure was consistent in all operations. The X-ray of the anteroposterior and lateral view of the lumbar vertebra was acquired and CT scan performed using GE Medical System Hi-speed NX/I-CT (USA) 1 hour after the discography. Imaging conditions were as follows: thickness 3 mm and slice spacing 0.5 mm. The patient could leave the bed immediately after the discography.
2.2. Evaluation standards
The negative indications are no pain or no specific pain, and the pain is caused by injection and varies from the clinical symptoms. The positive indications are concordant pain, and the pain is similar to normal LBP or the reproduction of normal LBP or referred pain. The grade of annular tears was divided into 4 grades on the basis of Dallas CT discography classification system [26]; Grade 0: contrast agent was limited to the nucleus pulposus, Grade 1: contrast agent flowed into the internal annulus along the fissure but the compactness was < 10% annulus, Grade 2: contrast agent flowed into the external annulus, and the compactness was 10% to 50% annulus, and Grade 3: contrast agent outflowed into the external annulus, also into the cavum epidurale and the compactness was >50% annulus. Grades 0 and 1 are categorized as normal, and Grades 2 and 3 represent annular tears.
2.3. Statistical analyses
Statistical Package for Social Sciences software for Windows (Version 17.0; SPSS Inc., Chicago, IL) was used for the analysis. The relationships between HIZ on MRI and the grade of annular tears and between the grade of annular tears or provocative discography were analyzed using Ridit (Reference IDentical unit). The relationship between HIZ on MRI and provocative discography was analyzed by Kappa consistency check. P values < .05 were considered significant for a 2-tailed probability.
3. Results
3.1. Clinical outcomes
The segments that underwent discography included a total 98 discs: 3 at L2/3, 31 at L3/4, 37 at L4/5, and 27 at L5/S1, of which 21 discs from 11 patients (21.4%) presented concordant pain. These 11 patients received operative treatment constituting posterior approach interbody fusion in 8 cases and anterior approach prosthetic disc nucleus replacement in 3 cases. All patients were followed up for a mean of 2.2 years. As a result, all patients experienced a satisfactory relief from LBP. Visual analog scales (VAS) were 7.9 ± 0.4 before the operation and 1.1 ± 0.3 after the operation, which was a significant improvement (t = 45.11, P < .01); Oswestry disability index (ODI) was 61.7 ± 5.5 before operation and 22.8 ± 4.4 after the operation, significantly improved (t = 18.32, P < .01). Nevertheless, no complications or worsening of symptoms were observed.
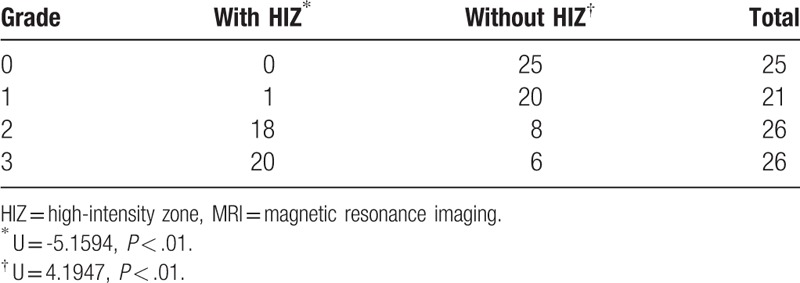
3.2. The relationship between HIZ on MRI and the grade of annular tears
Of the 98 discs that underwent discography, 39 discs (7 at L3/4, 21 at L4/5, and 11 at L5/S1) showed HIZ on MRI, accounting for 39.8%. Most of these 39 discs with HIZ on MRI showed Grade 2 or above annular disruption on contrast CT. The higher the grade of annular disruption, the higher the incidence of HIZ on MRI. The grade of annular disruption was higher in the disc with HIZ than in the disc without HIZ with statistical significance (U = 5.1594 and 4.1947, P < .01, Table 1).
Table 1.
HIZ on MRI and grade of annular disruption.
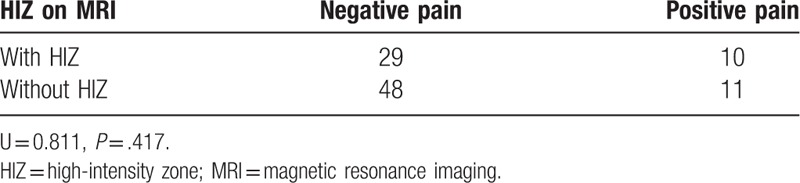
3.3. The relationship between HIZ on MR and provocative discography
On discography, 10 of 39 (25.6%) discs with HIZ on MRI showed concordant pain. Of the 59 discs without HIZ on MRI, only 11 discs showed concordant pain, accounting for 18.6%. However, no significant correlation was established between HIZ on MRI and concordant pain on discography (U = 0.8110, P > .05, Table 2).
Table 2.
HIZ on MRI and discographic pain.
3.4. The relationship between the grade annular disruption and discographic pain
Out of the 21 discs of Dallas grade 1, 6 had positive pain, accounting for 28.6%, 8 of 26 discs of Dallas grade 2 had positive pain (30.8%), and 6 of 26 (23.1%) discs of Dallas grade 3 presented positive pain. A significant correlation was not established between the grade of annular disruption and discographic pain (U = 0.7393 and -1.4157, P > .05, Table 3). A typical case was illustrated in Fig. 1.
Table 3.
Grade of annular disruption and discographic pain.
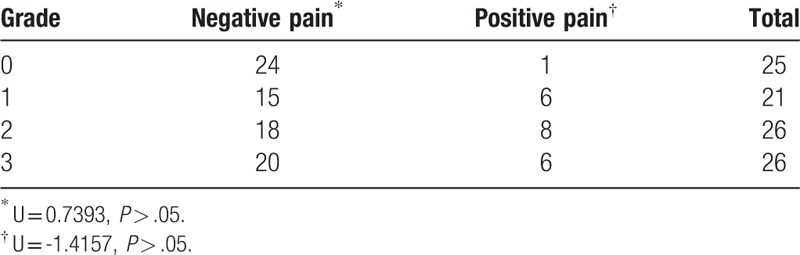
Figure 1.
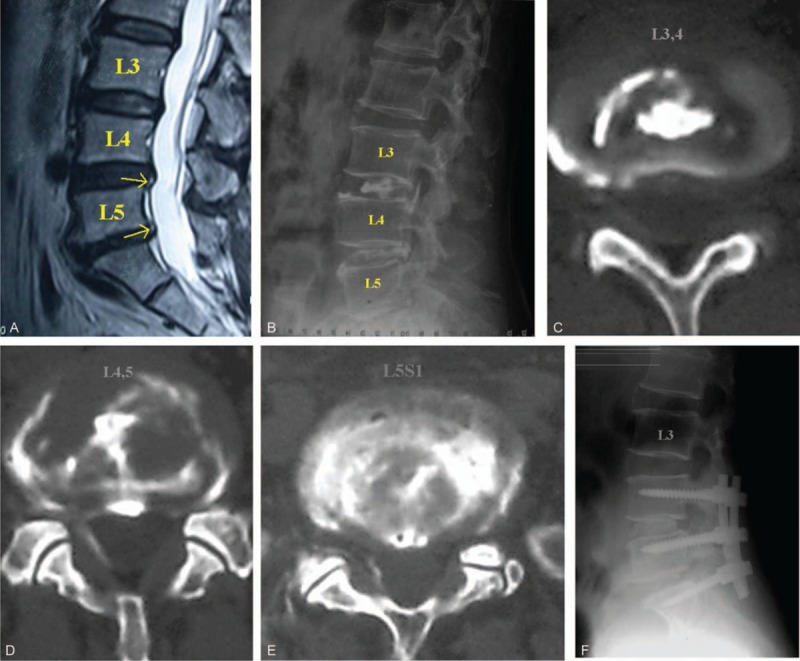
(A) Female patient, 55-year-old, suffering from chronic low back pain for 2 years, HIZ in 2 segments (L3/4, L4/5, and L5/S1) on MRI. (B) Lateral view of X-ray after discography showed that the contrast agent entered into the outer annulus and some into the outer layer of annulus, also into the epidural space. (C–E) CT following discography showed that the annulus in 3 intervertebral discs underwent tears, L4/5 (D) and L5/S1 (E) intervertebral discs had positive pain response, L3/4 (C) intervertebral discs had negative pain response. (F) Internal fixation and fusion of L4/5 and L5/S1 intervertebral discs were performed without interfering with L3/4 intervertebral discs and low back pain released completely after the operation.
4. Discussion
Some studies found HIZ as the inflammation of annulus fibrosus and speculated a correlation between the presence of HIZ within the posterior annulus of lumbar intervertebral disc on MRI and the pain response following discography in LBP patients.[14–16,18]. Schellhas et al[14] postulated HIZ as the indication of Grade 3 to 4 annular tears and that it represented the accumulation of mucoid fluid within the fissure of the annulus. After studying the pathogenesis of discogenic LBP, Peng et al[16] proposed that the band region of granulation tissue widely distributed in HIZ was the original area of discographic pain and discogenic LBP. The presence of HIZ as an image indication of annular tears and discogenic LBP is yet controversial.[14–18,22–24] Carragee et al[22] reported that the occurrence of HIZ in asymptomatic population was 24% and 59% in LBP patients. In the patients exhibiting symptoms, 30% intervertebral discs with HIZ were negative, and 24% intervertebral discs without HIZ were positive on discography. After comparing the results of various examinations including discography between the LBP and control groups, HIZ was considered as an unreliable marker of symptomatic intervertebral discs. Presently, the reproduction of discographic concordant pain is the gold standard for the diagnosis of discogenic LBP. Our study showed that the positive incidence of discographic concordant pain in the discs appeared in HIZ was not high, thereby indicating that HIZ was not a high specific diagnostic index for discogenic LBP. In a clinical setting, the disc in which HIZ appeared on MRI was not necessarily the disc that caused pain. The pain depended on the grade of the inner annular disruption and pathological type. HIZ is only a suggestive iconographic sign and cannot replace discography in discogenic LBP diagnosis.
Yu et al[27] found that high-resolution MRI could detect various signals of annular tears, which were indicated as nonconsecutive HIZ based on the signals of nucleus pulposus in MRI T2-weighted image. However, this change could also be detected in some asymptomatic individuals. The accuracy of MRI in diagnosing annular tears is low. Ito et al[24] showed that the signs of annular disruption on MRI could not reliably predict the incidence of inducing pain; however, they could predict the pain in a relative manner only when disruption occurred in the outer layer of the annulus. The disadvantage of MRI is that the segments of intervertebral space that cause the symptoms cannot be localized specifically when disc degeneration or protrusion involves several intervertebral spaces.
LBP is a common condition in the general population. A typically overlooked source of LBP in the general population is the consequence of internal disc disruption. This condition was described by Crock[28] in 1970 and continues to be a diagnostic and therapeutic challenge to physicians. CT scanning following discography allows us to accurately study the anatomical position of annular tears and aids in localization during operation, as well as selecting the operation approach and preventing operation on the nonpain disc. Resnick et al[29] speculated that only when MRI is closely integrated with the discography, it can provide reliable information for decision-making with respect to lumbar surgery. In this study, 10 of 39 discs with HIZ on MRI presented concordant pain response and the symptom of LBP in the patients released completely after operative treatment of these intervertebral spaces.
The relationship between HIZ and LBP can be arbitrated on the basis of the discographic pain. However, not all discs with HIZ presented symptoms. In the current group of patients, out of the 39 discs with HIZ, only 10 had concordant pain response. Therefore, we speculated that HIZ cannot reliably prompt the actual source of LBP, and although it is sensitive, the specificity is not high.[16,30] In the diagnosis and treatment of discogenic LBP, if HIZ appears within the posterior annulus of the patient lumbar disc on MRI, it indicates annular tears. If discography induces concordant pain response at the corresponding segment simultaneously same time, the pathological changes of the disc are potentially the actual source of pain and the possibility of symptom release after the operation would increase greatly. If the positive discographic pain does not appear during discography and only HIZ appears on MRI, the rate of relief from symptoms and the satisfaction of the patients after the operation will be lower than that of the patients positive in both concordant pain and HIZ. Thus, operative treatment is not recommended in these patients. The present study shows that the higher the grade of annular tears, the higher the incidence of HIZ on MRI; the grade of annular tears is higher in the discs with HIZ than in the discs without HIZ, and there is no obvious consistency between HIZ and discographic pain. MRI results should be closely integrated with those of discography, and thus, they play a crucial role in selecting operative segments only in this situation.
Nevertheless, the limitation of this study was its retrospective nature as an unrandomized case–control study, and the sample size constituting the number of patients was small. Therefore, further large-scale prospective randomized studies are essential to overcome these limitations and confirm that the presence of HIZ on MRI is only a suggestive and screening iconography sign for the diagnosis of discogenic LBP and that it cannot replace the gold-standard of the discography.
Footnotes
Abbreviations: HIZ = high-intensity zone, LBP = low back pain, MRI = magnetic resonance imaging, ODI = Oswestry Disability Index, VAS = visual analog scales.
HW, CZ, and ZL contributed equally to the manuscript and should be considered cofirst authors.
All authors state that there is no actual or potential of conflicts of interest in relation to this article. All authors declare that there are no financial and personal relationships with other people or organizations that could inappropriately influence (bias) our work.
References
- [1].Allan DB, Waddell G. An historical perspective on low back pain and disability. Acta Orthop Scand Suppl 1989;234:1–23. [DOI] [PubMed] [Google Scholar]
- [2].Rihn JA, Radcliff K, Norvell DC, et al. Comparative effectiveness of treatments for chronic low back pain: a multiple treatment comparison analysis. Clin Spine Surg 2017;30:204–25. [DOI] [PubMed] [Google Scholar]
- [3].Triebel J, Snellman G, Sandén B, et al. Women do not fare worse than men after lumbar fusion surgery: Two-year follow-up results from 4,780 prospectively collected patients in the Swedish National Spine Register with lumbar degenerative disc disease and chronic low back pain. Spine J 2017;17:656–62. [DOI] [PubMed] [Google Scholar]
- [4].Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet 2017;389:736–47. [DOI] [PubMed] [Google Scholar]
- [5].Adams MA, Mannion AF, Dolan P. Personal risk factors for first-time low back pain. Spine (Phila Pa 1976) 1999;24:2497–505. [DOI] [PubMed] [Google Scholar]
- [6].Bigos SJ, Battie MC, Spengler DM, et al. A prospective study of work perceptions and psychosocial factors affecting the report of back injury. Spine (Phila Pa 1976) 1991;16:1–6. [DOI] [PubMed] [Google Scholar]
- [7].Yrjama M, Tervonen O, Vanharanta H. Ultrasonic imaging of lumbar discs combined with vibration pain provocation compared with discography in the diagnosis of internal anular fissures of the lumbar spine. Spine (Phila Pa 1976) 1996;21:571–5. [DOI] [PubMed] [Google Scholar]
- [8].McCutcheon ME, Thompson WC3rd. CT scanning of lumbar discography. A useful diagnostic adjunct. Spine (Phila Pa 1976) 1986;11:257–9. [DOI] [PubMed] [Google Scholar]
- [9].Zhang X, Hao J, Hu Z, et al. Clinical evaluation and magnetic resonance imaging assessment of intradiscal methylene blue injection for the treatment of discogenic low back pain. Pain Phys 2016;19:E1189–95. [PubMed] [Google Scholar]
- [10].Manchikanti L, Hirsch JA. An update on the management of chronic lumbar discogenic pain. Pain Manag 2015;5:373–86. [DOI] [PubMed] [Google Scholar]
- [11].Reeves RS, Furman MB. Discography's role in low back pain management. Pain Manag 2012;2:151–7. [DOI] [PubMed] [Google Scholar]
- [12].Kim D, Wadley R. Variability in techniques and patient safety protocols in discography: a national multispecialty survey of International Spine Intervention Society members. J Spinal Disord Tech 2010;23:431–8. [DOI] [PubMed] [Google Scholar]
- [13].Carragee EJ, Alamin TF, Miller JL, et al. Discographic, MRI and psychosocial determinants of low back pain disability and remission: a prospective study in subjects with benign persistent back pain. Spine J 2005;5:24–35. [DOI] [PubMed] [Google Scholar]
- [14].Schellhas KP, Pollei SR, Gundry CR, et al. Lumbar disc high-intensity zone. Correlation of magnetic resonance imaging and discography. Spine (Phila Pa 1976) 1996;21:79–86. [DOI] [PubMed] [Google Scholar]
- [15].Aprill C, Bogduk N. High-intensity zone: a diagnostic sign of painful lumbar disc on magnetic resonance imaging. Br J Radiol 1992;65:361–9. [DOI] [PubMed] [Google Scholar]
- [16].Peng B, Hou S, Wu W, et al. The pathogenesis and clinical significance of a high-intensity zone (HIZ) of lumbar intervertebral disc on MR imaging in the patient with discogenic low back pain. Eur Spine J 2006;15:583–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Saifuddin A, Braithwaite I, White J, et al. The value of lumbar spine magnetic resonance imaging in the demonstration of anular tears. Spine (Phila Pa 1976) 1998;23:453–7. [DOI] [PubMed] [Google Scholar]
- [18].Walsh TR, Weinstein JN, Spratt KF, et al. Lumbar discography in normal subjects. A controlled, prospective study. J Bone Joint Surg Am 1990;72:1081–8. [PubMed] [Google Scholar]
- [19].Khan I, Hargunani R, Saifuddin A. The lumbar high-intensity zone: 20 years on. Clin Radiol 2014;69:551–8. [DOI] [PubMed] [Google Scholar]
- [20].Tonosu J, Oka H, Matsudaira K, et al. The relationship between findings on magnetic resonance imaging and previous history of low back pain. J Pain Res 2017;10:47–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Wang ZX, Hu YG. High-intensity zone (HIZ) of lumbar intervertebral disc on T2-weighted magnetic resonance images: spatial distribution, and correlation of distribution with low back pain (LBP). Eur Spine J 2012;21:1311–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Carragee EJ, Paragioudakis SJ, Khurana S. 2000 Volvo Award winner in clinical studies: lumbar high-intensity zone and discography in subjects without low back problems. Spine (Phila Pa 1976) 2000;25:2987–92. [DOI] [PubMed] [Google Scholar]
- [23].Lee KS, Doh JW, Bae HG, et al. Diagnostic criteria for the clinical syndrome of internal disc disruption: are they reliable? Br J Neurosurg 2003;17:19–23. [PubMed] [Google Scholar]
- [24].Ito M, Incorvaia KM, Yu SF, et al. Predictive signs of discogenic lumbar pain on magnetic resonance imaging with discography correlation. Spine (Phila Pa 1976) 1998;23:1252–8. discussion 1259-1260. [DOI] [PubMed] [Google Scholar]
- [25].Teraguchi M, Yoshimura N, Hashizume H, et al. The association of combination of disc degeneration, end plate signal change, and Schmorl node with low back pain in a large population study: the Wakayama Spine Study. Spine J 2015;15:622–8. [DOI] [PubMed] [Google Scholar]
- [26].Sachs BL, Vanharanta H, Spivey MA, et al. Dallas discogram description. A new classification of CT/discography in low-back disorders. Spine (Phila Pa 1976) 1987;12:287–94. [DOI] [PubMed] [Google Scholar]
- [27].Yu SW, Haughton VM, Sether LA, et al. Comparison of MR and diskography in detecting radial tears of the anulus: a postmortem study. AJNR Am J Neuroradiol 1989;10:1077–81. [PMC free article] [PubMed] [Google Scholar]
- [28].Crock HV. Internal disc disruption. A challenge to disc prolapse fifty years on. Spine (Phila Pa 1976) 1986;11:650–3. [PubMed] [Google Scholar]
- [29].Resnick DK, Choudhri TF, Dailey AT, et al. Guidelines for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 6: magnetic resonance imaging and discography for patient selection for lumbar fusion. J Neurosurg Spine 2005;2:662–9. [DOI] [PubMed] [Google Scholar]
- [30].Jha SC, Higashino K, Sakai T, et al. Clinical significance of high-intensity zone for discogenic low back pain: a review. J Med Invest 2016;63:1–7. [DOI] [PubMed] [Google Scholar]


