Abstract
Objective
To describe promoters and barriers to implementation of an airway safety quality improvement (QI) bundle from the perspective of interdisciplinary frontline clinicians and ICU QI leaders
Design
Mixed methods
Setting
Thirteen pediatric intensive care units (ICUs) of the NEAR4KIDS network
Intervention
Remote or on-site focus groups with interdisciplinary ICU staff. Two semi-structured interviews with ICU QI leaders with quantitative and qualitative data-based feedback.
Measurements and Main Results
Bundle implementation success (compliance) was defined as ≥ 80% use for tracheal intubations for three consecutive months. ICUs were classified as early or late adopters. Focus group discussions concentrated on safety concerns, and promoters and barriers to bundle implementation. Initial semi-structured QI leader interviews assessed implementation tactics and provided recommendations. Follow-up interviews assessed degree of acceptance and changes made after initial interview. Transcripts were thematically analyzed and contrasted by early vs. late adopters.
Median duration to achieve success was 502 days (IQR: 182–781). Five sites were early (median 153 days, IQR 146–267) and eight sites late adopters (median 783 days, IQR 773–845). Focus groups identified common promoter themes: interdisciplinary approach, influential champions, and QI bundle customization and barrier themes: time constraints, competing paperwork and QI activities, and poor engagement. Semi-structured interviews with QI leaders identified effective and ineffective tactics implemented by early and late adopters. Effective tactics included interdisciplinary QI team involvement (early adopter: 5/5, 100% vs late adopter: 3/8, 38%, p=0.08); ineffective tactics included: physician-only rollouts, lack of interdisciplinary education, lack of data feedback to frontline clinicians, and misconception of bundle as research instead of QI intervention.
Conclusions
Implementation of an airway safety QI bundle with high compliance takes a long time across diverse ICUs. Both early and late adopters identified similar promotor and barrier themes. Early adopter sites customized the QI bundle and had an interdisciplinary QI team approach.
Keywords: endotracheal intubation, safety, quality improvement, checklist, pediatrics, intensive care units
INTRODUCTION
Tracheal intubation (TI) is a life-saving procedure for critically ill children in pediatric ICUs (1–2). However, TI procedures are associated with complications and poor outcomes (3–11). Specifically, our previously published studies revealed 20% of TIs are associated with adverse TI associated events (TIAEs), and 6% are associated with severe TIAEs such as hypotension requiring intervention or cardiac arrests (3, 12). Although not all adverse events in critically ill children are preventable, we have identified specific patient, clinician, and practice factors associated with the occurrence of adverse TIAEs (3–8). Importantly, these factors are potentially modifiable. With these data, the National Emergency Airway Registry for Children (NEAR4KIDS), a multicenter TI quality improvement (QI) collaborative, developed an airway QI bundle to improve safety of TIs across diverse pediatric ICUs (5).
Implementation of QI interventions is often difficult due to a combination of inherent reluctance to change strongly established practice patterns and financial and/or physical space limitations (13). Although a checklist is often used as a powerful vehicle to implement specific QI interventions, this does not negate the challenges inherent to team based interactions and complex procedures (14). Key factors of an organization such as structural characteristics, external forces, resources for management and incentive, a culture of safety, and teamwork/leadership participation can have an effect on the successful implementation of patient safety initiatives (15). However, key factors for QI success identified in the literature vary and are often content and location specific (e.g., central line associated blood stream infection) (16). Furthermore, these identified key factors have not been routinely reported for most QI projects.
In this study, we evaluated the implementation process of a multicenter NEAR4KIDS airway safety QI bundle checklist as a key QI intervention across 13 diverse pediatric ICUs in 12 institutions. We utilized a mixed methods approach with: (1) qualitative data from interdisciplinary frontline clinician focus groups, (2) semi-structured interview data from QI leaders, and (3) ICU QI bundle compliance data for all TIs to achieve comprehensive understanding (16). We sought to identify promoters and barriers and determine whether promoters/barriers and implementation approach chosen by QI leaders may be different between early and late adopter ICUs.
MATERIALS AND METHODS
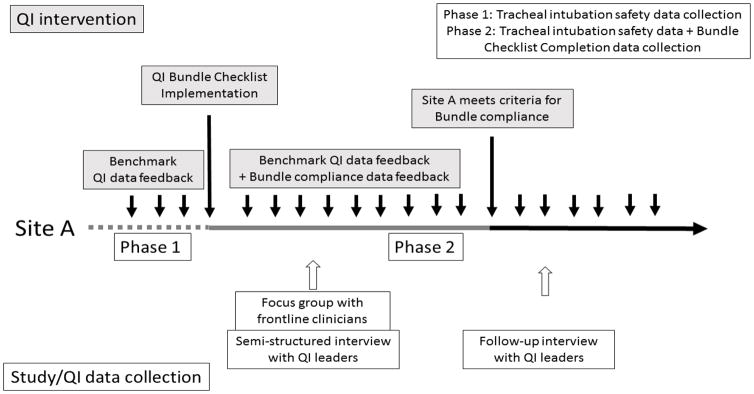
This is a prospective multicenter study with a mixed methods approach. The overall study diagram is displayed in Figure 1. The NEAR4KIDS registry is a large international multicenter QI collaborative to improve TI quality and safety in pediatric ICUs (3). Data collection for this study had been either approved or declared exempt by the Institutional Review Board (IRB) at each participating site. The patient, clinician, and practice factors, process and outcomes of each TI were prospectively collected at the time of the procedure. This procedure was monitored by a compliance plan which ensured validation of data accuracy, timely data entry, and >95% TI capture (3).
Figure 1.
Quality improvement (QI) intervention and study flow. Gray boxes indicate QI intervention, and white boxes indicate study intervention.
Airway safety QI bundle checklist development and implementation
The checklist development process has previously been described in detail (5). Briefly, a multi-center interdisciplinary QI committee was formed through the NEAR4KIDS collaborative to reduce high adverse TI associated event rates observed in baseline data from 13 pediatric ICUs (3). The committee decided to utilize a specifically developed QI bundle checklist to: 1) enforce a plan to ensure consistency, 2) provide cognitive aids, 3) ensure clinicians’ psychological safety to provide appropriate care, and 4) enhance teamwork and communication through a shared mental model across disciplines. The QI bundle checklist was developed to follow bedside workflows: preparation (risk identification and planning), pre-procedure timeout, and post-procedural debriefing (Supplemental Digital Content 1). The ICU oversight body at each institution approved this as a part of QI activity. Each ICU QI leader was also required to review and modify the QI bundle checklist to match their local bedside workflow around TI. As a part of the QI bundle, each ICU received a quarterly site benchmarking report which included a standard run chart for bundle checklist use and a control chart for the occurrence of adverse TI associated events. Each site leader was requested to review these data with their interdisciplinary frontline clinicians. An educational video which highlighted the interdisciplinary practice in using the QI bundle checklist [https://www.youtube.com/watch?v=YCGPOl6E1rc&feature=youtu.be] was provided for each site leader for staff education. Through bi-monthly teleconference calls, the QI bundle checklist implementation process was discussed with a strong emphasis on interdisciplinary involvement. Lastly, American Board of Pediatrics maintenance of certification points were offered to pediatric physician providers at each participating ICU if he/she was fully engaged in the QI activity.
Qualitative data collection
Focus groups with interdisciplinary pediatric ICU clinicians
Following IRB approval and participant consent, a focus group was held at each site within nine months after QI bundle implementation. Each ICU QI leader recruited a group of interdisciplinary pediatric ICU clinicians for a 1-hour focus group. Each group had a maximum of 10 clinicians including a maximum of three physicians to ensure interdisciplinary opinions were captured. QI leaders were not allowed to participate to ensure an open and honest discussion. Focus groups were facilitated by a moderator (KFD) either on-site (seven) or remotely (five) using video conference technology (Skype, Skype Technologies S.A., Luxembourg). The moderator had ample experience with focus group interviews and formal training in qualitative methodology. Each focus group followed a scripted introduction and set of structured questions about airway management safety in general and promoters and barriers of the QI bundle checklist implementation process (Supplemental Digital Content 2). Each focus group was audio-recorded, transcribed verbatim, and a de-identified transcript was developed.
Two authors (KFD, HB) used inductive analysis to identify common themes captured in the raw transcript content. Transcripts were read several times, coded to develop categories, and ultimately general themes emerged (17–18). Each theme was expanded or made more concise, as appropriate (19). The summary of themes was sent to focus group participants through each site leader and the participants confirmed there were no errors or misinterpretations (17). In addition, the focus group summary was provided to the QI leader to improve QI bundle implementation.
Semi-structured interviews with ICU QI leaders
Initial interview
Each site leader was interviewed by a single QI committee member (NN) using semi-structured questions. The initial interview was held concurrently at the time of the focus group or at a separate time via telephone (Figure 1). The interview focused on the implementation process of the QI bundle checklist from the site leader perspective. Semi-structured questions included presence or absence of interdisciplinary team formation for TI safety, chosen method to review and disseminate benchmarking TI safety data, and presence or absence of other TI related QI activity. During the interview, each sites’ benchmark QI data were also reviewed. Potential solutions were suggested to improve QI bundle checklist uptake and airway management safety. Site leader responses were documented by the interviewer for analysis. After the interview, each site leader received a summary of the discussion to ensure accuracy.
Follow-up interview
Each site leader was interviewed by a member of the QI committee six months after the initial interview and receipt of their institution’s focus group summary (average 6.3 months, range 4.7–8.0 months) (Figure 1). The purpose was to assess how results of the initial interview with each QI leader and the focus group summary were utilized at each ICU to improve compliance with QI bundle checklist use. Detailed notes were taken to assess changes at each site and to develop future QI implementation tactics. Qualitative inductive analyses of both interviews were performed by the same author (NN).
Quantitative data collection
QI bundle compliance
Each ICU reported the use of the QI bundle checklist for each TI encounter in addition to the required standard NEAR4KIDS data points. Specifically, the use of the QI bundle checklist was reported as either: (1) fully used (all three sections of the checklist used), (2) partially used (only one or two sections of the checklist were used), or (3) not used. We considered the TI encounter as compliant only if all three sections of the checklist were fully used. The ICU-specific compliance rate was calculated by the following formula: TIs with the fully completed checklist divided by all TI encounters for a given period.
Each ICU QI leader reported their airway bundle QI checklist go-live date to the data coordinating center. Sites were considered QI bundle compliant if their monthly compliance rate reached equal or above 80% for three consecutive months. This criterion was prospectively designated. The duration for QI bundle uptake was defined as the duration from the go-live date to the first date of the month when the ICU became compliant.
Data Analysis
We a priori defined each participating ICU in two categories: (1) early adopter defined as the sites who achieved QI bundle compliance criterion less than the median period of all sites that ultimately achieved the criterion, and (2) late adopter defined as the rest of the sites. Similarities and differences in promotors and barriers in QI bundle implementation were explored by early and late adopter sites. The QI bundle implementation tactics used at each ICU was similarly analyzed. An interdisciplinary team was defined as the leadership from more than one discipline (e.g., physicians/nurse practitioners, nurses, respiratory therapists) formed a specific team or task force to implement the QI bundle.
Statistical analyses
For quantitative data, summary statistics were described with counts, proportions (%), medians, and interquartile ranges (IQR). For categorical variables with a dichotomous outcome, a contingency table method was used with Fisher’s exact test. For a comparison of numeric variables, Wilcoxon rank-sum test was used with Stata 11.2 (College Station, TX, USA). A p<0.05 was considered significant.
RESULTS
QI bundle implementation
Thirteen pediatric ICUs from 12 institutions in the United States initiated the QI bundle implementation between January 2013 and January 2014; the bundle compliance was followed monthly until June 2015. Table 1 summarizes participating ICU characteristics. The duration from initial inception of the QI bundle checklist implementation to time achieving compliance criteria was a median of 502 days (IQR: 182–781days). The median duration to compliance was 153 days for early adopting ICUs (n=5) and 783 days for late adopting ICUs eventually meeting compliance criteria (n=5, Table 1). Three ICUs (23%) did not meet compliance criteria during the study period.
Table 1.
Participating ICU characteristics
| Site characteristics | Early adopter (n=5) | Late adopter† (n=8) | p-value |
|---|---|---|---|
| Site type n (%) |
PICU 2 (40%) CICU 1 (20%) Mixed 2 (40%) |
PICU 1 (12%) CICU 0 (0%) Mixed 7 (88%) |
0.16 |
| Total number of ICU beds (median, IQR) | 20 (20–40) | 18.5 (15–24) | 0.24 |
| Total ICU admissions per year (median, IQR) | 900 (825–2,500) | 1,125 (935–1,450) | 0.43 |
| Pediatric Residency (n, %) | Present (4, 80%) | Present (8, 100%) | 0.39 |
| Pediatric Critical Care Fellowship (n, %) | Present (4, 80%) | Present (5, 63%) | 1.00 |
| In-house attending call system (n, %) | In-house (5, 100%) | In-house (5, 63%) | 0.23 |
| Duration (days) to achieve compliance‡ (median, IQR) | 153 (146–267) | 783 (773–845) | 0.009 |
Late adopter includes both ICUs meeting the bundle compliance criteria after 502 days (n=5) or not yet meeting criteria (n=3).
CICU=cardiac intensive care unit (pediatric); IQR=interquartile range; Mixed=unit has both PICU and CICU patients; PICU=pediatric intensive care unit.
Calculated for the 5 late adopter sites that met compliance criteria by end of study period.
P-values were calculated with Fisher’s exact test for categorical values and Wilcoxon rank sum test for numeric values.
Focus groups with ICU clinicians
Twelve focus groups with interdisciplinary frontline clinicians were conducted with 13 ICUs at a median of 610 days (IQR: 533–621) after implementing the QI bundle. Two pediatric ICUs (non-cardiac and cardiac) from one institution held a combined focus group. Table 2 describes the timing of the focus group interview, method, and participants (5–10 per group) and Table 3 summarizes participant demographic information. The average ICU experience of participants was 11 years (median 8 years, IQR: 4–14).
Table 2.
Focus group characteristics
| Focus Group | Early adopter ICUs (n=4†) | Late adopter ICUs (n=8) | Total (n=12†) |
|---|---|---|---|
| Interview days after QI implementation (median, IQR) | 537 (441–585) | 617 (589–621) | 610 (533–621) |
| Focus group method (remote vs. on-site) | Remote 1 (25%) On-site 3 (75%) |
Remote 4 (50%) On-site 4 (50%) |
Remote 5 (42%) On-site 7 (58%) |
| Total number of participants (range per site) | Attending Physician 5 (0–3) Fellow 2 (0–1) Resident 0 (0) Nurse Practitioner 4 (1) Registered Nurse 7 (1–3) Respiratory Therapist 8 (1–3) Pharmacist 0 (0) |
Attending Physician 8 (0–2) Fellow 6 (0–3) Resident 1 (0–1) Nurse Practitioner 6 (0–2) Registered Nurse 15 (1–3) Respiratory Therapist 9 (0–2) Pharmacist 1 (0–1) |
Attending Physician 13 (0–3) Fellow 8 (0–3) Resident 1 (0–1) Nurse Practitioner 10 (0–2) Registered Nurse 22 (1–3) Respiratory Therapist 17 (0–3) Pharmacist 1 (0–1) |
Two early adopter sites had one combined focus group meeting (pediatric non-cardiac ICU and pediatric cardiac ICU). ICU denotes intensive care unit. QI denotes quality improvement. IQR denotes interquartile range.
Table 3.
Focus group participant demographics (total participants N=71)
| Age (years) | Gender | Pediatric ICU experience (years) | Site ICU experience (months) | Role in pediatric airway management n (%) |
Involvement in QI bundle use* n (%) |
|---|---|---|---|---|---|
| Mean 38 Median 36 (IQR: 30–46) |
Male 19 (27%) Female 52 (73%) |
Mean 11 Median 8 (IQR: 4–14) |
Mean 99 Median 84 (IQR: 33–136) |
Supervisor 4 (5%) Frontline clinician 36 (51%) Both 26 (37%) Not specified 5 (7%) |
Very involved 23 (32%) Involved 30 (42%) Somewhat involved 11 (16%) Not involved 7 (10%) |
IQR denotes Interquartile range.
Very involved - familiar with the QI bundle and use it every time I am involved with an intubation
Involved - familiar with the QI bundle and use it most of the times I am involved with an intubation
Somewhat involved - familiar with the QI bundle and use it some of the times I am involved with an intubation
Not involved - familiar with the QI bundle, but do not use it myself
All focus group participants verbalized a fundamental understanding of the purpose of the QI bundle, identified promotor and barrier themes, and thematic saturation was achieved. In all focus groups, six common themes were discussed to varying degrees, except one group who did not describe any barriers (this was a late adopting site). Promoter and barrier themes did not differ among early vs. late adopter sites.
Promoter Themes
Theme 1 - Interdisciplinary education and QI bundle completion. Participants expressed that all clinicians should be aware of, educated about, and participate in the implementation and completion of the QI bundle.
Theme 2 - Influential site champions. Participants expressed the need and benefit of having someone on the clinical staff, regardless of role, truly invested in the QI bundle implementation that was available to coach and support its use.
Theme 3 - Bundle customization. As sites had increasing experience with the QI bundle, participants expressed the desire to modify the format to better fit with their daily work flow and unit culture.
Barrier Themes
Theme 1 - Lack of time. Participants voiced concerns over not having adequate time to complete the QI bundle checklist.
Theme 2 - Competing paperwork/QI initiatives. Participants often had competing demands in terms of paperwork and projects.
Theme 3 - Clinician buy-in. Participants expressed that gaining staff buy-in from all disciplines was challenging.
Semi-structured interview with ICU QI leader
Initial interview
Three themes around implementation tactics were identified by ICU QI leaders. The themes are listed below in their ineffective form (negative). Early adopter ICUs were more likely to have introduced the QI bundle as a QI initiative rather than a research project and were more likely to have included interdisciplinary ICU staff (at least two disciplines; physicians plus nurses and/or respiratory therapists) when implementing baseline mandatory education and developing a QI team (100% vs 38%, p=0.08).
Theme 1 – Confusion about the purpose of the QI bundle. There was a lack of recognition from ICU QI physician leaders that this was a QI initiative, not a research study.
Theme 2 – Disorganized initial implementation plan. There was failure to follow standardized processes in implementing a new QI initiative in a locally accepted manner, to customize the QI bundle checklist to local needs, to integrate the QI bundle checklist into the work flow of the unit, and develop clear guidelines how to use the QI bundle checklist for patients identified “at risk for tracheal intubation”.
Theme 3 – Lack of interdisciplinary education, involvement, and data sharing. Initial education and rollout as well as TI safety data and QI bundle checklist compliance feedback was limited to physicians. Nursing and respiratory therapy were only involved at the leadership level without reaching frontline clinicians.
Follow-up interview
A follow-up semi-structured interview with site leaders was held approximately 6 months (median: 199 days, IQR: 142–405) after initial interview to follow up on the suggestions given at that time and the focus group summary. The latest TI safety data and QI bundle compliance rates were also provided. Table 4 demonstrates typical suggestions from the initial interview that were/were not carried out by QI leaders. Early adopter sites implemented more tactics suggested at the initial interview.
Table 4.
Similarities and differences in airway safety bundle implementation tactics used by ICU QI leaders at each site
| Strategy and Tactics | Early Adopter | Late Adopter |
|---|---|---|
| Initial strategies used by site QI leader | ||
| Similarities | No guidance in screening process for QI bundle use (i.e., all ICU patients vs. only at-risk patients) | |
| Differences | At least two disciplines in implementation team Staff perceived as QI intervention |
Physician only implementation team Staff perceived as research activity |
| Tactics suggested at initial interview* | ||
| Similarities | Customize and incorporate QI bundle for local workflow‡ Frontline clinician education/re-education‡ Data sharing with all interdisciplinary frontline clinicians |
|
| Differences | Include all disciplines in interdisciplinary team† Correct entry of QI bundle use data in the database by QI team‡ |
Form interdisciplinary team Use of QI bundle by frontline providers as designed (guide for each step: preparation, timeout, post-procedural debrief)‡ |
| Additional tactics implemented by site QI leader** | ||
| Similarities | Developed local guidelines for QI bundle use | |
| Differences | No need for process change in QI data entry | Processes were augmented/changed to ensure accurate QI data entry |
Item indicates the component of specific tactic was adopted by majority (>50%) of sites at time of follow-up interview
ICU: Intensive Care Unit, QI: quality improvement.
Interdisciplinary team was defined in this manuscript as the leadership from more than one discipline (e.g., physicians/nurse practitioners, nurses, respiratory therapists).
Initial interview performed by a QI committee member. Refer to Qualitative data collection under Materials and Method section.
Additional tactics implemented by site QI leader between initial and follow up interview.
DISCUSSION
This study describes our experience implementing an airway safety QI bundle intervention across diverse pediatric ICUs. We were able to use a mixed methods approach using both qualitative and quantitative data. This triangulation of data strengthens our research findings by giving a more comprehensive insight into a topic, providing both verification and validity while complementing similar data (20). Our semi-structured interview with site leaders highlighted the importance of clear message in QI intervention and utilization of accepted QI implementation process. We also identified the struggle of leaders due to limited local infrastructure for ongoing interdisciplinary education for QI at each site. These findings were further validated by the focus group promoter themes: importance of education and QI champions. We utilized quantitative data, time to achieve bundle compliance, to contrast with qualitative data obtained through QI leader semi-structured interviews and frontline clinician focus groups to obtain an inclusive picture.
The implementation of the checklist was the cornerstone of the QI bundle. This was similar to other QI bundle intervention studies which published their successful implementation (21–22). The specific function of the checklist: 1) forcing function to ensure consistency of care, 2) providing cognitive aids, 3) providing a shared mental model, and 4) streamlining teamwork and communication, was fully utilized in our process of airway safety bundle implementation. Unfortunately, having a checklist in place does not ensure its use. Therefore, we designed our QI bundle checklist to be marked for task completion at the bedside by frontline clinicians. This process provided us quantitative data to track the complete use of the QI bundle for each TI encounter.
Our study used qualitative approach to identify barriers and promoters and QI bundle implementation tactics. Frontline clinicians, while not being formally trained in QI methodology, innately identified common promoters and barriers to QI implementation during the focus groups. Interestingly and importantly, these identified promotors and barriers were similar across the diverse ICUs regardless of their speed of adoption (early vs late). Similar themes have been identified in the literature with surgical site checklist implementation (13, 23–24). Notably, frontline clinicians identified the importance of interdisciplinary involvement, site customization, and having local champions to promote QI bundle checklist use.
Semi-structured interviews with ICU QI leaders identified effective and non-effective QI bundle implementation tactics, often relating to the clinician identified promoters and barriers. There were differences between early and late adopting ICUs in using effective and non-effective tactics such as interdisciplinary team development, plan to incorporate the QI bundle into unit workflow, and a system to educate all clinicians on its use. Misperception of the QI initiative as a research activity may have introduced perceived limited involvement and responsibility by the staff. It may have also introduced thinking that this was a rigid protocol. While the staff requirement to comply with the QI bundle should be rigorous, misconception of rigid protocol with limited sense of ownership by frontline clinicians was identified as a barrier in our study, which was not previously described in the literature. This qualitative information is highly valuable for refining and improving the QI implementation process to focus on effective implementation tactics.
Customization of the QI bundle checklist for the local workflow was identified important during the focus groups, while QI leaders needed to ensure the effectiveness of the QI bundle remain unchanged. For the current study, the NEAR4KIDS QI Committee provided an oversight with a priori developed criteria: 1. A basic structure of the QI bundle checklist is maintained, 2. All minimal items on the checklist is maintained while sites are allowed to change orders within each section and add site specific items, and 3. All customized checklist requires approval before clinical use by the QI committee.
The duration from the initial inception of the QI bundle to the time meeting compliance was long (median 502 days) with a wide discrepancy between early and late adopting ICUs. Our study results suggest this may be partially explained by the lack of interdisciplinary involvement in QI bundle implementation. This likely resulted in low interdisciplinary staff buy-in and limited sense of responsibility for QI bundle completion. The long duration to implement the QI intervention may be subject to underlying practice changes and updates in practice guidelines, which will jeopardize the validity of the QI intervention since it was developed prior to these changes and updates. Therefore we should aim for minimizing the implementation phase of QI intervention (duration between implementation to full compliance). We should also ‘update’ the QI intervention to meet emerged clinical needs identified through the ongoing QI data collection.
These findings should be considered in light of inherent methodological limitations. Investigators only spoke with limited numbers of frontline clinicians during the focus groups. Participants were invited by the ICU QI leader and not randomly chosen; therefore, selection bias may have been present. The sample size was limited by the overall study design to evaluate QI bundles on TI safety outcomes; therefore, our quantitative analyses are underpowered. Frontline clinicians might have had limited levels of understanding in QI interventions in the environment where QI infrastructure and educational resources were limited. Despite these limitations, we believe that our findings are valid, particularly since the promotors and barriers, and effective and ineffective implementation tactics were strikingly similar across diverse ICUs. QI bundle implementation speed was associated with effective implementation tactics. Therefore, a set of common interventions to diminish barriers, support promoters, and teach effective implementation tactics could be useful to all pediatric ICUs regardless of size or geographic location. Finally, we did not collect data regarding organizational QI structure, institutional and unit culture for QI activities. These factors likely played a role in our TI safety QI bundle implementation process (25). Future studies should include these measures and tailor implementation tactics by utilizing existing QI paths and expertise at each unit.
Future Direction
Based on these study findings, we have further developed a new airway safety QI bundle implementation kit (Instruction document as Supplemental Content File 3) to address the themes identified through focus groups, and facilitate effective implementation tactics identified through QI leader interviews. This detailed instruction for each QI bundle implementation step was not available during the present study. The kit serves as a start-up tool for ICUs to facilitate the QI bundle implementation. The kit consists of three components; 1) introduction, 2) clinician education, and 3) QI bundle checklist tailored to ICU needs and workflow. The introduction component outlines the steps of the implementation process: presentation to frontline clinicians as a QI initiative as opposed to a research project, obtaining ICU leadership endorsement, and emphasis to develop an interdisciplinary team with leaders from each discipline. The second component includes a slide presentation to provide frontline clinician education and a link to a video which demonstrates the interdisciplinary involvement and the use of the QI bundle checklist at the bedside. The last component includes two versions of the draft QI bundle checklist and an instruction to customize to their local needs with submission for approval. This component also includes a general guidance regarding which “at risk” patients should have a QI bundle checklist started at bedside. Lastly, a teleconference with an interdisciplinary site team and NEAR4KIDS QI leader is scheduled to discuss each component and specific guidance regarding how to assess the workflow of the unit to incorporate the bundle without adding many additional steps. All new sites implementing QI bundle checklists are required to use this new airway safety QI bundle implementation kit.
CONCLUSIONS
Focus groups with frontline clinicians and semi-structured interviews with ICU QI leaders identified common promotors and barriers as well as effective and ineffective tactics for QI bundle implementation. Interdisciplinary involvement and education was critical in successful QI bundle implementation, along with influential site champions and sharing of QI bundle compliance and safety data across all disciplines. Tailoring QI bundles to local specific needs and workflow were also found important for successful implementation.
Supplementary Material
Acknowledgments
We would like to thank all site study coordinators, frontline clinicians, especially focus group participants, and QI team leaders for this study. We also thank Jessica Leffelman and Stephanie Tuttle, MBA for administrative support.
Footnotes
Financial Disclosure and Conflicts of Interest
This study was supported by Agency for Healthcare Research and Quality: AHRQ R03HS021583, R18 HS022464, R18HS024511 and Endowed Chair, Critical Care Medicine, The Children’s Hospital of Philadelphia.
Copyright form disclosure: Dr. Davis’ former institution received funding from Agency for Healthcare Research and Quality (AHRQ R03HS021583, AHRQ R18HS022464, and AHRQ 1R18HS024511-01). Dr. Napolitano received funding from board membership for Allergy and Asthma Network and American Association for Respiratory Care; she received support for article research from AHRQ R18 grant; her institution received funding from AHRQ R18 (NEAR - airway bundle development and qualitative analysis), CVS Health (development of tobacco dependence program), consulting work for product development for Actuated Medical and GeNO, and from research funding and speaking fees from Draeger Medical and Aerogen. Dr. Buffman received funding from AHRQ R18HS022464 grant, as a research coordinator for this project. Dr. Sullivan received support for article research from the National Institutes of Health. Dr. Parker received funding from Raynes McCarty. Dr. Nishisaki’s institution received funding from AHRQ R03HS021583, AHRQ R18HS022464, and AHRQ 1R18HS024511-01. The remaining authors have disclosed that they do not have any potential conflicts of interest.
References
- 1.Kleinman ME, de Caen AR, Chameides L, et al. Part 10: Pediatric basic and advanced life support: 2010 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2010;122(16 Suppl 2):S466–515. doi: 10.1161/CIRCULATIONAHA.110.971093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kleinman ME, Chameides L, Schexnayder SM, et al. Part 14: pediatric advanced life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(18 Suppl 3):S876–908. doi: 10.1161/CIRCULATIONAHA.110.971101. [DOI] [PubMed] [Google Scholar]
- 3.Nishisaki A, Turner DA, Brown CA, III, et al. A National Emergency Airway Registry for children (NEAR4KIDS): landscape of tracheal intubation in 15 pediatric intensive care units. Crit Care Med. 2013;41(3):874–85. doi: 10.1097/CCM.0b013e3182746736. [DOI] [PubMed] [Google Scholar]
- 4.Sanders R, Giuliano J, Sullivan J, et al. Level of trainee and tracheal intubation outcomes. Pediatrics. 2013;131(3):e821–8. doi: 10.1542/peds.2012-2127. [DOI] [PubMed] [Google Scholar]
- 5.Simon Li, Rehder K, Giuliano J, Apkon M, et al. Development of a quality improvement bundle to reduce tracheal intubation associated event in pediatric ICUs. Am J Med Qual. 2016;31(1):47–55. doi: 10.1177/1062860614547259. [DOI] [PubMed] [Google Scholar]
- 6.Nett ST, Emeriaud G, Jarvis JD, et al. Site-level variance for adverse tracheal intubation associated events across 15 North American Pediatric ICU’s: A report from the National Emergency Airway Registry for children (NEAR4KIDS) Pediatr Crit Care Med. 2014;15(4):306–13. doi: 10.1097/PCC.0000000000000120. [DOI] [PubMed] [Google Scholar]
- 7.Graciano AL, Tamburro R, Thompson AE, et al. Incidence and associated factors of difficult tracheal intubations in pediatric ICUs: A report from the National Emergency Airway Registry for children: NEAR4KIDS. Intensive Care Med. 2014;40(11):1659–69. doi: 10.1007/s00134-014-3407-4. [DOI] [PubMed] [Google Scholar]
- 8.Tarquinio KM, Howell JD, Montgomery V, et al. Current medication practice and tracheal intubation safety outcomes from a prospective multicenter observational cohort study. Pediatr Crit Care Med. 2015;16(3):210–8. doi: 10.1097/PCC.0000000000000319. [DOI] [PubMed] [Google Scholar]
- 9.Nishisaki A, Donoghue A, Colborn S, et al. Effect of just-in-time simulation training on tracheal intubation procedure safety in the pediatric ICU. Anesthesiology. 2010;113(1):214–23. doi: 10.1097/ALN.0b013e3181e19bf2. [DOI] [PubMed] [Google Scholar]
- 10.Nishisaki A, Nguyen J, Colborn S, et al. Evaluation of interdisciplinary simulation training on clinical performance and team behavior during tracheal intubation procedures in a pediatric intensive care unit. Pediatr Crit Care Med. 2011;12(4):406–14. doi: 10.1097/PCC.0b013e3181f52b2f. [DOI] [PubMed] [Google Scholar]
- 11.Nishisaki A, Marwaha N, Kasinathan V, et al. Airway management in pediatric patients at referring hospitals compared to a receiving tertiary pediatric ICU. Resuscitation. 2011;82(4):386–90. doi: 10.1016/j.resuscitation.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 12.Shiima Y, Berg RA, Bogner HR, et al. Cardiac arrests associated with tracheal intubations in pediatric intensive care units: A multicenter cohort study. Crit Care Med. 2016;44(9):1675–82. doi: 10.1097/CCM.0000000000001741. [DOI] [PubMed] [Google Scholar]
- 13.Conley DM, Singer SJ, Edmondson L, et al. Effective surgical safety checklist implementation. J Am Coll Surg. 2011;212(5):873–9. doi: 10.1016/j.jamcollsurg.2011.01.052. [DOI] [PubMed] [Google Scholar]
- 14.Catchpole K, Russ S. The problem with checklists. BMJ Qual Saf. 2015;24(9):545–9. doi: 10.1136/bmjqs-2015-004431. [DOI] [PubMed] [Google Scholar]
- 15.Taylor SL, Dy S, Foy R, et al. What context features might be important determinants of the effectiveness of patient safety practice interventions? BMJ Qual Saf. 2011;20(7):611–7. doi: 10.1136/bmjqs.2010.049379. [DOI] [PubMed] [Google Scholar]
- 16.Krein SL, Damschroder LJ, Kowalski CP, Forman J, Hofer TP, Saint S. The influence of organizational context on quality improvement and patient safety efforts in infection prevention: a multi-center qualitative study. Soc Sci Med. 2010;71(9):1692–701. doi: 10.1016/j.socscimed.2010.07.041. [DOI] [PubMed] [Google Scholar]
- 17.Patton MQ. Enhancing the quality and credibility of qualitative analysis. Health Serv Res. 1999;34(5 Pt 2):1189–1208. [PMC free article] [PubMed] [Google Scholar]
- 18.Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Eval. 2006;27(2):237–246. [Google Scholar]
- 19.Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15(3):398–405. doi: 10.1111/nhs.12048. [DOI] [PubMed] [Google Scholar]
- 20.Rothwell E. Analyzing focus group data: content and interaction. J Spec Pediatr Nurs. 2010;15(2):176–80. doi: 10.1111/j.1744-6155.2010.00237.x. [DOI] [PubMed] [Google Scholar]
- 21.Gillis A, Jackson W. Research for nurses: Methods and interpretation. Philadelphia, PA: F.A. Davis Company; 2002. [Google Scholar]
- 22.Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360(5):491–9. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 23.Tarrago R, Nowak JE, Leonard CS, et al. Reductions in invasive device use and care costs after institution of a daily safety checklist in a pediatric critical care unit. Jt Comm J Qual Patient Saf. 2014;40(6):270–8. doi: 10.1016/s1553-7250(14)40036-9. [DOI] [PubMed] [Google Scholar]
- 24.Bergs J, Lambrechts F, Simons P, et al. Barriers and facilitators related to the implementation of surgical safety checklists: a systematic review of the qualitative evidence. BMJ Qual Saf. 2015;24(12):776–86. doi: 10.1136/bmjqs-2015-004021. [DOI] [PubMed] [Google Scholar]
- 25.Russ SJ, Sevdalis N, Moorthy K, et al. A qualitative evaluation of the barriers and facilitators toward implementation of the WHO surgical safety checklist across hospitals in England: lessons from the “Surgical Checklist Implementation Project”. Ann Surg. 2015;261(1):81–91. doi: 10.1097/SLA.0000000000000793. [DOI] [PubMed] [Google Scholar]
- 26.Berry JC, Davis JT, Bartman T, et al. Improved safety culture and teamwork climate are associated with decreases in patient harm and hospital mortality across a hospital system. J Patient Saf. 2016 Jan 7; doi: 10.1097/PTS.0000000000000251. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.