Abstract
Objectives
In-hospital cardiac arrest (CA) occurs in 2.6%–6% of children with cardiac disease and is associated with significant morbidity and mortality. Much remains unknown about CA in pediatric cardiac intensive care units (CICU), therefore we aimed to describe CA epidemiology in a contemporary multicenter CICU cohort.
Design
Retrospective analysis within the Pediatric Cardiac Critical Care Consortium (PC4) clinical registry.
Setting
CICUs within 23 North American hospitals
Patients
All cardiac medical and surgical patients admitted from 8/2014–7/2016
Interventions
None
Measurements and Main Results
There were 15,908 CICU encounters (6498 medical, 9410 surgical). 3.1% had CA; rate was 4.8 CA/1000 CICU days. Medical encounters had 50% higher rate of CA compared to surgical encounters. Observed (unadjusted) CICU CA prevalence varied from 1–5.5% among the 23 centers; CA/1000 CICU days varied from 1.1 to 10.4. Over half CA occur within 48hrs of admission. On multivariable analysis, prematurity, neonatal age, any Society of Thoracic Surgeons preoperative risk factor, and STS-European Association for Cardiothoracic Surgery mortality category 4,5 had strongest association with surgical encounter CA. In medical encounters independent CA risk factors were acute heart failure, prematurity, lactic acidosis >3mmol/dL, and invasive ventilation 1hr after admission. Median cardiopulmonary resuscitation (CPR) duration was ten minutes, return of spontaneous circulation occurred in 64.5%, extracorporeal CPR in 27.2%. Unadjusted survival was 53.2% in encounters with CA vs. 98.2% without. Medical encounters had lower survival after CA (37.7%) vs. surgical encounters (62.5%); Norwood patients had less than half the survival after CA (35.6%) compared to all others. Unadjusted survival after CA varied greatly among 23 centers.
Conclusions
We provide contemporary epidemiologic and outcome data for CA occurring in the CICU from a multicenter clinical registry. As detailed above, we highlight high-risk patient cohorts and periods of time that may serve as targets for research and QI initiatives aimed at CA prevention.
Keywords: cardiac arrest, pediatrics, cardiac intensive care unit, mortality, congenital heart disease, epidemiology
Introduction
Cardiac arrest (CA) occurs more frequently in hospitalized children with acquired and congenital cardiac disease compared to any other disease type (1, 2). CA is always a clinically important event with potential for significant morbidity or mortality. Children with cardiac disease suffer CA at rates of 2.6% to 6%, with corresponding survival ranging from 32–50.6% (1–6). The most recent multi-institutional data from the Society of Thoracic Surgeons (STS) Congenital Heart Surgery database suggests a 2.6% CA rate for postoperative patients, and a survival rate of 50.6% among those having CA (6). As more hospitals develop dedicated cardiac intensive care units (CICUs) to optimize the care of this complex patient population, practitioners must continue to advance their understanding of CA to improve quality of care and clinical outcomes (7).
Much remains unknown about the epidemiology of CA in cardiac patients cared for in the CICU. Several existing data sources lack important details crucial for characterizing cardiac patients and CA events in this highly specialized clinical setting; only two single-center studies describe the epidemiology of CA occurring exclusively in a pediatric CICU (3, 8). Critical knowledge gaps remain regarding modifiable patient factors, timing of events, therapies for, and outcomes after CA. Previous literature identifies younger age, prematurity, genetic syndromes, preoperative co-morbid conditions, and increased surgical complexity as risk factors for CA in postoperative cardiac surgery patients (4, 6, 9). However, the epidemiology and risk factors in non-surgical cardiac patients have not been thoroughly elucidated, though medical cardiac patients may be at higher risk for mortality after CA compared to surgical patients (5, 10). Deficiencies in CICU-specific CA data prevents accurate benchmarking across hospitals and represents a major barrier to potential quality improvement (QI) efforts aimed at reducing the rates of CA and its associated sequelae.
In this context, we performed an analysis within the Pediatric Cardiac Critical Care Consortium (PC4) clinical registry. We aimed to describe CA epidemiology in a contemporary patient cohort - event characteristics, frequency, and outcome data - from the CICUs in North America contributing data to PC4. Identification of independent risk factors for CA in both surgical and non-surgical CICU encounters could be used in subsequent risk adjustment models to better characterize metrics of CA prevention and treatment. We viewed this study as a crucial initial step in a process to improve CA-related care in the pediatric CICU.
Materials and Methods
Data Source
PC4 is a voluntary QI collaborative for pediatric CICUs at 30 participating hospitals across North America. This analysis includes data from the 23 hospitals actively submitting data at the time of analysis. The PC4 dataset provides information across the full spectrum of cardiovascular disease regarding patient characteristics, diagnoses, procedures and outcomes during the entire CICU encounter. We have previously described the components of the PC4 clinical registry and architecture of the collaborative (11). Briefly, every CICU encounter at each participating hospital is submitted to the database, and over 90% of the variables are mandatory for case submission, thus ensuring complete data collection on all variables necessary for risk-adjusted outcome reporting. The rate of missing variables for this analysis was <1%. We have previously demonstrated excellent accuracy and completeness of the data in the clinical registry (12). PC4 data collection qualifies as QI activity at the data coordinating center and participating hospitals, and is therefore not subject to ongoing institutional review board (IRB) oversight. The data coordinating center IRB at the University of Michigan provided a waiver of informed consent to conduct this study.
Inclusion and exclusion criteria
We considered all hospitalizations and each CICU encounter of patients admitted to PC4 hospitals between August 2014 and July 2016. We performed both hospitalization and encounter-level descriptive analyses. For all inferential analyses the unit of analysis was an individual CICU encounter. A surgical encounter was defined as any that included a STS index operation (operations with cardiopulmonary bypass or cardiovascular surgery without bypass) immediately before or during the CICU encounter. When analyzing surgical encounters, we excluded those encounters of patients <2.5kg undergoing isolated patent ductus arteriosus repair, undergoing index operations that could not be classified into one of the STS-European Association for Cardiothoracic Surgery (STAT) mortality categories (13), and those who did not receive postoperative care in the CICU. Non-surgical, or medical encounters, included all encounters not meeting the above criteria; this included those patients admitted for planned cardiac surgery that did not occur (medical encounter, preoperative cardiovascular surgery) and patients admitted postoperatively after general surgery procedures and cardiovascular surgeries that were not STS index operations (i.e. extracorporeal membrane oxygenation (ECMO) cannulation, thoracic duct ligations, diaphragm plication, etc.).
Definitions of outcomes and independent variables
We used the following registry definition of CA as the primary outcome for all analyses: (1) cardiopulmonary arrest requiring chest compressions and/or defibrillation for pulseless ventricular tachycardia, or (2) acute respiratory compromise requiring emergency assisted ventilation leading to cardiopulmonary arrest requiring chest compressions and/or defibrillation. All events must also elicit a resuscitation response by facility personnel and have a resuscitation record completed.
This CA event definition is consistent with the American Heart Association’s Get with the Guidelines – Resuscitation (GWTG-R) registry (14). All complications and clinical events in the registry – including CA – are timed and dated. Time to arrest was calculated from the start time of the CICU encounter. Sequence of events, complications, and procedures was determined from these time stamps. Where possible, we reported our results to be consistent with the Utstein template of reporting CA and resuscitation outcomes (15). As such, successful resuscitation was defined as cardiopulmonary resuscitation (CPR) in which the patient survived without extracorporeal support. Survival was calculated based on the patient’s first CA during a CICU encounter.
Cardiac diagnoses and operative procedures are defined according to the International Pediatric and Congenital Cardiac Code (16). As previously described, PC4 data collection on surgical encounters is harmonized by sharing variables submitted to the STS Congenital Heart Surgery Database locally by the participant hospital (12). For medical encounters, we grouped cardiomyopathy, acute myocarditis, and acute decompensated heart failure diagnoses into a single exposure variable of “acute heart failure.” Primary reason for CICU admission is classified into mutually exclusive groups: 1. medical condition (cardiac, respiratory, infectious, neurologic, other); 2. preoperative for planned cardiothoracic surgery; 3. postoperative non-cardiothoracic surgery; 4. Post-cardiac catheterization; 5. evaluation of structural heart disease (patient admitted with known or suspected congenital/structural heart disease for the purpose of a diagnostic/therapeutic trial to determine if intervention is needed). Prematurity was defined as gestational age <37 weeks. Underweight was defined as CICU encounters where patient weight is at least two standard deviations below average weight for age category as defined by World Health Organization and Center for Disease Control. These and all other variables studied are defined in the PC4 data definitions manual [pc4quality.org].
Statistical analysis
We describe overall and stratified unadjusted CA rates as events per encounter (%) and events per 1000 CICU days; any portion of a patient day in the CICU contributed one day to the denominator of CICU days. Univariate and multivariate analyses were performed to determine the association between independent variables and CA during an encounter within the surgical and medical strata. Our approach was similar for each subgroup. We utilized the Chi-square and Fisher’s Exact tests as appropriate for univariate comparisons. Variables associated with CA at p<0.1 on univariate analysis were included in a multivariable logistic regression model with generalized estimating equations to account for clustering within hospitals. Our goal was to define predictors of CA that could be used in the future for a case-mix adjustment model to compare hospitals. In our primary analysis of surgical encounter CA events, we considered all CA whether they occurred preoperatively or at any time postoperatively. In this first model, we only included patient factors, complexity of surgical disease, and pre-arrest complications. In a complementary analysis, we analyzed postoperative CA events occurring >2 hours after the patient’s index cardiovascular surgery. This allowed us to include all of the factors in the first model, as well as illness-severity variables from the first two post-operative hours. In this analysis 67 CA (16.4%) were excluded because they occurred before the end of the two hour window for postoperative risk factor variable collection (n=65), or because there was missing postoperative variable data (n=2).
After analyzing the frequency of CA within the first hour of medical CICU encounters (~20%), we decided for two reasons to change the dependent variable for the medical encounter model to include only CA occurring after the first hour. First, this better reflects CICU quality in preventing arrests; arrests on admission or shortly after are less likely attributable to the quality of care provided by the CICU team. Second, some of the independent variables are recorded within the first two hours of the encounter, so our approach helps to prevent misclassification of post-arrest variables as risk factors for CA. Independent variables associated with the outcome at p<0.05 in surgical and medical models were considered statistically significant predictors of CA.
After determining the final models for CA in both surgical and medical encounters, we performed bootstrap resampling (1000 samples) to empirically derive bias-corrected 95% confidence intervals around the odds ratio for each predictor. The final model was comprised of those variables where the 95% confidence interval did not include one. We then calculated a bias-corrected C-statistic to assess model discrimination, and tested calibration using the Hosmer-Lemeshow test. All analyses were performed using SAS Version 9.4 (SAS Institute, Cary, NC) or STATA Version 14 (Stata Corp, College Station, TX.
Results
Patient characteristics and Cardiac Arrest prevalence
The study cohort included hospitalizations and CICU encounters from 23 hospitals; there were 14,522 hospitalizations and 15,908 CICU encounters (6,498 medical and 9,410 surgical). Overall and stratified CA rates are presented in Table 1.
Table 1.
CICU Encounter Cardiac Arrest Rates
| Cohort | CICU Encounters (n) | Cardiac Arrest n (%) |
CA/1000 CICU days |
|---|---|---|---|
| All | 15908 | 492 (3.1) | 4.79 |
| Age | |||
| Neonate, 0–30 days | 2808 | 186 (6.6) | 5.12 |
| Infant, 31–365 days | 5007 | 166 (3.3) | 4.83 |
| Child, 1–18 years | 6896 | 118 (1.7) | 4.25 |
| Adult, >18 years | 1197 | 22 (1.8) | 5.25 |
| Medical | 6498 | 183 (2.8) | 6.24 |
| Surgical | 9410 | 309 (3.3) | 4.18 |
| Pre-operative | 2214 | 45 (2.0) | 3.32 |
| Post-operative | 9410 | 272 (2.9) | 3.72 |
| STAT category | |||
| 1 | 2692 | 23 (0.85) | 2.36 |
| 2 | 3046 | 56 (1.8) | 3.31 |
| 3 | 1162 | 25 (2.2) | 3.00 |
| 4 | 1983 | 143 (7.2) | 5.06 |
| 5 | 361 | 58 (16.1) | 7.00 |
| None | 166 | 4 (2.4) | 2.48 |
CA, cardiac arrest; CICU, cardiac intensive care unit; STAT, Society of Thoracic Surgeons - European Association for Cardio-Thoracic Surgery Congenital Heart Surgery Mortality Categories
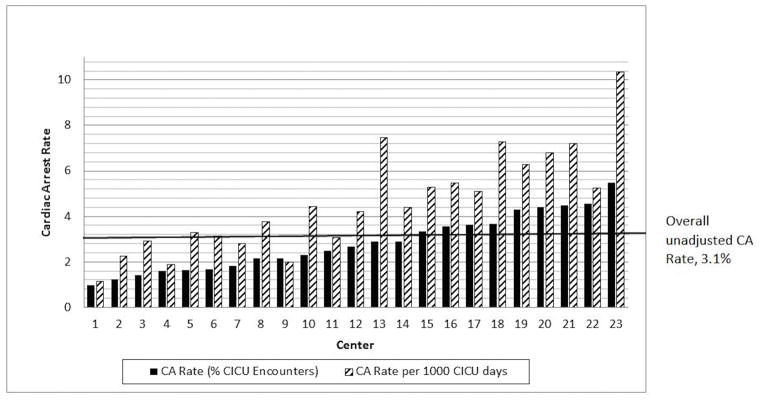
CA occurred in 3.3% (n=485) of hospitalizations and 3.1% (n=492) of CICU encounters. Of the 492 CICU encounters with CA, 79.5% (n=391) had only one CA, while 20.5% (n=101) of the encounters had more than one CA. There were 642 total CA episodes, resulting in 4.8 CA per 1000 CICU days. The prevalence of CA in medical encounters per 1000 CICU days was 50% greater when compared to surgical encounters (Table 1). The frequency of CA was higher in younger age subgroups; patients < 1 year of age incur 71.5% (n=352) of CA despite representing only 49% of all CICU encounters. Neonates had double the prevalence of CA compared to infants. Figure 1 demonstrates that the overall observed (unadjusted) CICU CA rates among the 23 centers varied from 1% to 5.5%, and the rate of CA/1000 CICU days varies from 1.1 to 10.4.
Figure 1.
Center variation in observed (unadjusted) cardiac arrest (CA) rates shown as a percentage of cardiac intensive care unit (CICU) encounters and per 1000 CICU days
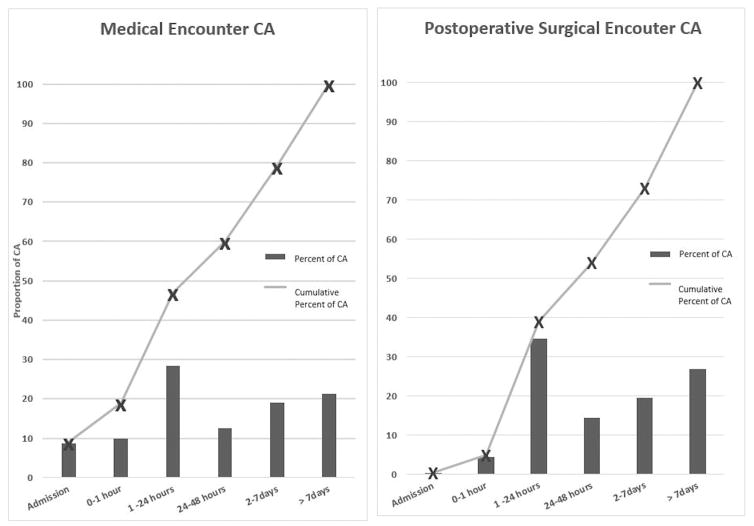
Timing of Cardiac Arrest
Figure 2 demonstrates the timing of the first CA during medical encounters and the first postoperative CA in surgical encounters. Greater than half of the CA events occur within the first 48 hours of CICU admission in both encounter types, while about 1/4 occurred >1 week after admission. Of the 2,214 surgical encounters where the patient was admitted to the CICU preoperatively, 2% (n=45) included a preoperative CA, 25% of which occurred within the first hour of admission. 207/642 (32.2%) of CA occurred at night (23:00 – 06:59); while 165/642 (25.8%) occurred on the weekend (Friday 23:00 – Monday 06:59). Weekend CA were evenly distributed between the day and night. However, 352 (73.8%) of the 477 weekday CA occurred during the day.
Figure 2.
Timing of cardiac arrest (CA) occurrence in relation to cardiac intensive care unit (CICU) admission for medical and postoperative surgical encounters
Risk factors for surgical encounter CA
Surgical patients account for 63% (309/492) of the total encounters with CA. Surgical CA rates stratified by STS benchmark operation and surgical procedure category are shown in supplemental Table 1. Encounters with greater surgical complexity and/or single ventricle palliation of any type had a disproportionately greater prevalence of CA.
Supplemental Table 2 includes the results from univariate analysis of variables associated with CA in surgical encounters. Preoperative variables including younger age, lower weight, genetic abnormality, syndrome, extra cardiac anomaly, higher STAT category, and presence of any STS preoperative risk factor were associated with CA, all p<0.0001. Pre-arrest ECMO, pulmonary hypertension, arrhythmia, CICU readmission, previous CA, and listing for heart transplant were also significantly associated with CA.
In our primary analysis of surgical encounter CA, multivariable logistic regression (including only patient and pre-arrest variables) showed that prematurity, neonatal age, presence of any STS preoperative risk factor, and STAT category 4 or 5 had the strongest association with CA (Table 2). In our complementary analysis of postoperative cardiac arrest (>2 hours after the index surgery), ECMO within two hours of CICU admission, open sternum, mechanical ventilation at 2 hours, and maximum vasoactive inotropic score (17) were all associated with postoperative CA; preoperative predictors of CA previously identified remained independently associated with CA in this model (Supplemental Table 3).
Table 2.
Multivariate Logistic Regression Model of Preoperative Risk Factors Associated with CA in Surgical Encounters
| Risk Factor | Odds Ratio | 95% CI | P Value |
|---|---|---|---|
| Age at encounter start* | |||
| Premature neonate, <31 days | 5.04 | 2.98, 8.54 | <0.001 |
| Term neonate, <31 days | 3.77 | 2.54, 5.60 | <0.001 |
| Infant, 31–365 days | 2.48 | 1.69, 3.63 | <0.001 |
| Underweight vs. other | 1.56 | 1.17, 2.08 | 0.003 |
| Any chromosomal abnormality | 1.36 | 1.04, 1.78 | 0.027 |
| Any STS preoperative risk factor | 2.14 | 1.68, 2.74 | <0.001 |
| STAT category 4 or 5 vs. other | 3.92 | 2.94, 5.22 | <0.001 |
Reference group Child, 1–18years
CA, cardiac arrest; CI, confidence interval; STAT, Society of Thoracic Surgeons - European Association for Cardio-Thoracic Surgery Congenital Heart Surgery Mortality Categories; STS, Society of Thoracic Surgeons
Risk factors for medical encounter CA
Patient characteristics, clinical variables, and comorbidities that were associated with CA >1 hour after CICU admission during a medical encounter are presented in Supplemental Table 4. Prematurity, younger age group, extra cardiac anomaly, admission for medical diagnosis, listed for heart transplant, arrhythmia, pulmonary hypertension, acute heart failure, systemic atrioventricular regurgitation, lactic acidosis within two hours of admission, and mechanical ventilation at one hour after CICU admission were some of the important univariate risk factors for CA. After multivariable logistic regression, five variables emerged as independent risk factors for CA in medical encounters; all p<0.001 (Table 3).
Table 3.
Multivariate Logistic Regression Model of Patient Characteristics Associated with CA in Medical Encounters
| Risk Factor | Odds Ratio | 95% CI | P value |
|---|---|---|---|
| Premature neonate | 3.15 | 1.54, 5.37 | <0.001 |
| Admission for Medical Condition vs. all others* | 2.20 | 1.56, 3.34 | <0.001 |
| Acute heart failure vs. all other diagnoses* | 2.23 | 1.47, 3.19 | <0.001 |
| Lactate > 3mmol/dL within 2 hours of CICU admission | 3.00 | 1.86, 4.86 | <0.001 |
| Mechanical ventilation 1 hour post CICU admission | 2.61 | 1.70, 3.82 | <0.001 |
CA, Cardiac Arrest; CI, confidence interval; CICU, Cardiac Intensive Care Unit; *see methods and supplemental Table 3 for details
Resuscitation characteristics
Twenty-nine percent of patients were not intubated at CPR initiation; 36% of these patients had been extubated during the previous 24-hour period. Median CPR duration for all CA was ten minutes (IQR 3, 31). Successful resuscitation occurred in 64.5% (n=313); with CPR ending in death in 8.2% (n=40) and ECPR in 27.2% (n=132). Median CPR duration in ECPR patients was 44 min (IQR 24, 65). Hospital survival in ECPR patients was 38.6% (n=51).
Epidemiology of survival after cardiac arrest
Overall observed survival occurred in 53.2% (262/492) of CICU encounters with CA vs. 98.2% without, p<0.0001. Stratified unadjusted survival rates at the CICU encounter level are shown in Table 4 and supplemental Table 1. Survival after CA is low across all strata evaluated compared to those without CA. In age strata, survival after CA was highest in infants. Medical encounters had lower survival after CA (37.7%) compared to all surgical encounters (62.5%), p<0.0001. Surgical encounters that included CA in the postoperative period had a 77% survival rate. Patients undergoing the Norwood operation had half the survival rate after CA (35.6%) compared to any other surgical procedure (supplemental Table 1). The survival rate in CICU encounters with >1 CA episode was 38.6% vs. 57% (p=0.001) in those with only one episode. Time to mortality data was available for 215/230 patients: 18.6% (n=40) of patients died during their resuscitation, 41.4% (n=89) died within 24 hours, and 47.9% (n=103) died >72 hours after CA. Unadjusted survival rate after CA varied among the 23 centers (12.5% to 75.8%).
Table 4.
CICU Encounter Stratified Unadjusted Survival Rates
| Cohort | CICU Encounters (n) | Cardiac Arrest n (%) |
Survival, Yes CA n (%) |
Survival, No CA n (%) |
|---|---|---|---|---|
| All | 15908 | 492 (3.1) | 262 (53.3) | 15136 (98.2) |
| Neonate, 0–30 days | 2808 | 186 (6.6) | 90 (48.4) | 2501 (95.4) |
| Infant, 31–365 days | 5007 | 166 (3.3) | 108 (65.1) | 4769 (98.5) |
| Child, 1–18 years | 6896 | 118 (1.7) | 56 (47.5) | 6778 (99.0) |
| Adult, >18 years | 1197 | 22 (1.8) | 8 (36.4) | 1155 (98.3) |
| Medical | 6498 | 183 (2.8) | 69 (37.7) | 6150 (97.4) |
| Surgical | 9410 | 309 (3.3) | 193 (62.5) | 8986 (98.7) |
| Pre-operative | 2214 | 45 (2.0) | 24 (53.3) | 2093 (96.5) |
| Post-operative | 7407 | 272 (2.9) | 243 (89.3) | 7090 (99.4) |
| STAT category | ||||
| 1 | 2692 | 23 (0.85) | 18 (78.3) | 2668 (99.96) |
| 2 | 3046 | 56 (1.8) | 39 (69.6) | 2970 (99.3) |
| 3 | 1162 | 25 (2.2) | 18 (72) | 1121 (98.6) |
| 4 | 1983 | 143 (7.2) | 89 (62.2) | 1788 (97.2) |
| 5 | 361 | 58 (16.1) | 27 (46.6) | 280 (92.4) |
| None | 166 | 4 (2.4) | 2 (50.0) | 159 (98.1) |
CA, cardiac arrest; CICU, cardiac intensive care unit; STAT, Society of Thoracic Surgeons – European Association for Cardio-Thoracic Surgery Congenital Heart Surgery Mortality Categories
Discussion
This study represents the first multi-institutional analysis reporting CA epidemiology for all medical and surgical patients that suffer CA while receiving specialized care exclusively by a pediatric CICU care team. We established contemporary benchmarks for CA prevalence and rate: CA occurs in 3.1% of CICU encounters and 4.8/1000 CICU patient days across our cohort. The majority of existing pediatric CA literature focuses on CPR metrics and risk factors for morbidity/mortality after CA. Our data is the precursor for quality improvement initiatives for CA prevention, thus we focus on identification of risk factors contributing to CA incidence. We present independent risk factors for CA in both medical and surgical encounters, which lays the foundation for calculating risk-adjusted CA rates at individual centers. Given the high morbidity and mortality associated with CA (1–6), it is paramount that clinicians and researchers investigate methods to mitigate harm related to CA. Our hope is that the data from this study will be the first step in a multi-institutional initiative aimed at decreasing the prevalence of CA in pediatric CICUs.
Children with cardiac disease are at significantly higher risk for in-hospital CA compared to those admitted without cardiac disease (1, 2, 5, 10). Previous studies report the prevalence of CA in patients with congenital or acquired heart disease to range from 2.6% to 6% depending on the characteristics and locations of the patients analyzed (1–6). Our CA prevalence was lower than the other two historical studies inclusive of all admissions to a single pediatric CICU, in which the CA prevalence were 4.1% (9.3 CA/1000 CICU days) [n=786] (3) and 4.6% (n=2230) (8). However, the CA rates in both these single-center studies do fall within the wide range of CA rates seen across the 23 individual centers in our cohort (1% to 5.5%).
The risk factors for CA in CICU patients have not been completely investigated (1, 6). In a retrospective analysis of the administrative Kid’s Inpatient Database (which included CA in all hospital locations), children <1 year of age, heart failure, myocarditis, single ventricle physiology, and coronary artery pathology were associated with increased risk of CA on multivariate analysis, while patients undergoing cardiac surgery had decreased risk of CA (1). Many of these risk factors are confirmed in our analyses, including our findings that medical patients suffer more CA per 1000 patient days than surgical patients, and CA occurs more frequently in younger age groups and those diagnosed with acute heart failure. However, our study was unique in that we also evaluated severity of illness measures (biomarkers and therapies) on admission to the CICU for non-surgical encounters to determine associations with subsequent CA. The novel findings were that mild lactic acidosis (>3 mMol) and/or invasive mechanical ventilation shortly after CICU admission were independent risk factors for CA during a medical CICU encounter.
Our analysis also confirms many of the univariate risk factors for postoperative CA reported by the STS database study (6). We took the next step and performed the first comprehensive multivariate analysis to identify risk factors for CA in pediatric cardiac surgical patients from our multicenter cohort. Younger age groups, presence of any STS preoperative risk factor, chromosomal abnormality, underweight patient, and high complexity surgery (STAT 4 and 5) were all independent risk factors for CA in surgical encounters. When considering specific risk factors for postoperative arrest, including postoperative measures of illness severity and markers of physiologic derangement – ECMO, open sternum, mechanical ventilation, and higher vasoactive support – all had strong association with CA. Prematurity, which is known to be associated with worse outcomes after cardiac surgery, (18) was the strongest and the only independent risk factor for CA identified in both surgical and medical encounters.
The granularity of the PC4 dataset enables us to make some novel observations about the timing of CA. About 60% of CA occur within the first 48 hours for both medical and post-surgical admissions. In a recent analysis from the Collaborative Pediatric Critical Care Research Network (CPCCRN), 27% of CA in their cardiac patient cohort occurred in the first 24 hours, compared to 43% in our study (2). The first 24–48 hours often represents the period of time during which the patient’s physiology is most tenuous, and thus at highest risk for cardiovascular collapse. Additionally, over 1/3 of the CA that occur in non-intubated children occur during the first 24 hours after extubation. This suggests the transition from invasive ventilation may be a vulnerable period for these children with limited cardiac output reserve - possibly due to increases in afterload of the systemic ventricle and cardiac output demand from the respiratory muscles – increasing risk for CA (7). These revelations provide relatively short time intervals during which quality initiatives, protocols, practice guidelines, and interventions aimed at CA prevention might be focused for maximal impact on overall CA rates. Night shift and weekends, however, did not seem to portend an increased risk of CA as seen in other studies (8). Recording etiology of CA and preceding events in the next iteration of CA data collection may help identify modifiable risk factors occurring during this period of time to further focus CA prevention initiatives.
Observed hospital survival after CA in cardiac patients in the PC4 registry (53%) is higher than post-CA survival reported in other databases, including that in GWTG-R database (35%) (14), Kid’s Inpatient Database (44%) (1), and CPCCRN (44%) (2). The recent analysis of the STS database demonstrated an overall survival rate of 51% in postoperative CA patients (18) vs. 77% survival after postoperative CA in PC4. The reasons for apparently improved post-CA survival in our study are unclear and should be the focus of future study. All CPR and post-resuscitation management occurs in the CICU for CA recorded in the PC4 registry. We speculate that patient management/interventions in place at time of the arrest (frequent central venous and arterial access, improved cardiac monitoring, etc.) and/or presence of team members experienced with the unique considerations of resuscitation of the cardiac patient may contribute to improved survival after CA when CPR occurs in the CICU (7). In adult patients, CA location in a general ward or telemetry unit is associated with decreased survival relative to intensive care settings, and intensive monitoring (including arterial line, independent of hospital location) also confers a survival benefit (19). Additionally, specialized CA processes and post arrest management, including easier access to ECPR, may improve survival after CA when it occurs in the CICU (7, 20, 21).
Though most of our data focuses on CICU CA rates and associated risk factors, we can make some general comments about CPR for these CICUs in comparison to the studies from the GWTG-R registry (5, 10). Despite the same definition of CA, the duration of CPR in our study was much shorter (median ten minutes) than that demonstrated in pediatric cardiac surgical (n=711, median 25 minutes) and medical (n=572, median 23 minutes) patients from the GWTG-R database (14). Specialized care provided in the CICU may have contributed to this difference; compared to 100% of CA episodes receiving CPR in the CICU for our PC4 cohort, only 75% of CA occurred in either a pediatric ICU or CICU from the GWTG-R population. In the CPCCRN multicenter CA study, 42% of cardiac patients had CPR duration less than median ten minutes; the majority of these patients were treated in a pediatric CICU (2). Despite the difference in CPR duration, return of spontaneous circulation was approximately 60% for all three studies, though, as above, we did observe higher survival rate in the PC4 cohort. Perhaps not surprising given the predilection for ECPR in pediatric CICUs, ECPR occurs more frequently in our registry (27%) compared to the GWTG-R (14%) and CPCCRN (12%).
We report observed (unadjusted) prevalence and rates for CA at each of our 23 individual centers. Although the hospital rates are not adjusted for patient factors or severity of illness, the observed variation in CA rates across centers suggests differential performance with respect to CA prevention. The next key step to understand true center variation in CA rates requires determination of risk-adjusted CA rates at each site; these analyses are underway within PC4.
The limitations of our study are inherent of any observational analysis using clinical registry data. Although the data integrity of the PC4 database has previously been demonstrated as excellent (12), the possibility remains for ascertainment bias resulting from inadvertent exclusion of some CA episodes or misclassification of CA related data points such as stop and start times of CPR. Further, we were only able to analyze the variables included in the registry, and there may be other important associations between predictors and the outcome that we could not assess. We do not include preceding events, rhythm and other CA metrics such as time to epinephrine, defibrillation and quality of CPR. Additionally, we do not present risk factors associated with survival after CA or risk-adjusted survival rates across centers; future analyses to investigate these outcomes are underway. A strategy of linking PC4 data to a registry such as GTWG-R would enable evaluation of the interaction of CA risk factors and compliance with standard CPR processes in comprehensive risk adjusted mortality and survival with favorable neurologic outcome models. Finally, this analysis only includes 23 North American centers, all of whom have dedicated pediatric CICUs, and thus may not be generalizable to other hospitals or care settings; the findings are not applicable to pediatric cardiac patients that suffer CA outside the CICU.
Conclusion
These analyses describe, for the first time, the granular clinical epidemiology of CA in dedicated pediatric CICUs, a unique setting and patient population when considering CA. In contemporary pediatric CICUs, 3.1% of encounters suffered CA with an event rate of 4.8 CA/1000 CICU days. We identified high-risk patient cohorts and time periods in a patient’s clinical course that may serve as strategic targets for research and QI initiatives to determine if prevention and treatment outcomes from CA can be improved. This study lays the groundwork for development of risk-adjustment models such that we can explore true variation in CA rates across pediatric CICUs and identify high-performing CICUs with respect to CA prevention and CA rescue. This analysis represents an important and necessary first step for a planned multicenter QI initiative aimed at decreasing the prevalence of CA in the pediatric CICU.
Supplementary Material
Acknowledgments
Financial support for this study was provided through departmental funds
We acknowledge data collection teams at all of the participating centers, and the generous donors to the University of Michigan Congenital Heart Center and CHAMPS for Mott for their support of PC4.
Footnotes
Reprints will not be ordered
Copyright form disclosure: Wenying Zhang disclosed work for hire. Dr. Gaies’ institution received funding from the National Institutes of Health (NIH)/National Heart, Lung, and Blood Institute, and he received support for article research from the NIH. The remaining authors have disclosed that they do not have any potential conflicts of interest.
References
- 1.Lowery AW, Knudson JD, Cabrera AG, et al. Cardiopulmonary resuscitation in hospitalized children with cardiovascular disease: estimated prevalence and outcomes from the kids inpatient database. Pediatric Crit Care Med. 2013;14(3):248–255. doi: 10.1097/PCC.0b013e3182713329. [DOI] [PubMed] [Google Scholar]
- 2.Berg RA, Nadkarni VM, Clark AE, et al. Incidence and outcomes of cardiopulmonary resuscitation in pediatric intensive care units. Crit Care Med. 2016;44:798–808. doi: 10.1097/CCM.0000000000001484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parra DA, Totapally BR, Zahn E, et al. Outcome of cardiopulmonary resuscitation in a pediatric cardiac intensive care unit. Crit Care Med. 2000;28(9):3296–3300. doi: 10.1097/00003246-200009000-00030. [DOI] [PubMed] [Google Scholar]
- 4.Rhodes JF, Blaufox AD, Seiden HS, et al. Cardiac arrest in infants after congenital heart surgery. Circulation. 1999;100(19SUppl):II194–199. doi: 10.1161/01.cir.100.suppl_2.ii-194. [DOI] [PubMed] [Google Scholar]
- 5.Ortmann L, Prodham P, Gossett J, et al. Outcomes after in-hospital cardiac arrest in children with cardiac disease: a report from Get with the Guidelines-Resuscitation. Circulation. 2011;124(21):2329–2337. doi: 10.1161/CIRCULATIONAHA.110.013466. [DOI] [PubMed] [Google Scholar]
- 6.Gupta P, Jacobs JP, Pasquali SK, Hill KD, Gaynor JW, O’Brien SM, He M, Sheng S, Schnexnayder Sm, Berg RA, Nadkarni WM, Imamura M, Jacobs ML. Epidemiology and outcomes after in-hospital cardiac arrest after pediatric cardiac surgery. Ann Thorac Surg. 2014;98(6):2138–2143. doi: 10.106/j.athoracsur.2014.06.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peddy SB, Hazinski MF, Laussen PC, et al. Cardiopulmonary resuscitation: Special considerations for infants and children with cardiac disease. Cardiol Young. 2007;(Suppl 2):116–126. doi: 10.1017/S1047951107001229. [DOI] [PubMed] [Google Scholar]
- 8.Gaies MG, Clarke NS, Donohue JE, et al. Personnel and unit factors impacting outcome after cardiac arrest in a dedicated pediatric cardiac intensive care unit. Ped Crit Care Med. 2012;13(5):583–588. doi: 10.1097/PCC.0b013e318238b272. [DOI] [PubMed] [Google Scholar]
- 9.Suominen P, Palo R, Sairanen H, et al. Perioperative determinants and outcome of cardiopulmonary arrests in children after heart surgery. Eur J Cardiothorac Surg. 2001;19(2):127–134. doi: 10.1016/s1010-7940(00)00650-3. [DOI] [PubMed] [Google Scholar]
- 10.Matos RI, Watson RS, Nadkarni VM, et al. Duration of cardiopulmonary resuscitation and illness category impact survival and neurologic outcomes for in-hospital pediatric cardiac arrests. Circulation. 2013;127(4):442–451. doi: 10.1161/CIRCULATIONAHA.112.125625. [DOI] [PubMed] [Google Scholar]
- 11.Gaies M, Cooper DS, Tabbutt S, et al. Collaborative quality improvement in the cardiac intensive care unit: development of the Pediatric Cardiac Critical Care Consortium (PC4) Cardiol Young. 2015;25(5):951–957. doi: 10.1017/S1047951114001450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gaies M, Donohue JW, Willis GM, et al. Data integrity of the Pediatric Cardiac Critical Care Consortium (PC4) clinical registry. Cardiol Young. 2016;26(6):1090–1096. doi: 10.1017/S1047951115001833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O’Brien SM, Clarke, Jacobs JP, et al. An empirically based tool for analyzing mortality associated with congenital heart surgery. J Thorac Cardiovasc Surg. 2009;138(5):1139–1153. doi: 10.1016/j.jtcvs.2009.03.071. [DOI] [PubMed] [Google Scholar]
- 14.American Heart Association. [Accessed January 31, 2017];Get with the guidelines-resuscitation web page. Available at: https://www.heart.org/HEARTORG/HealthcareResearch/GetWithTheGuidelines/GetWithTheGuidelines-Resuscitation/Get-With-The-Guidelines-Resuscitation_UCM_314496_SubHomePage.jsp.
- 15.Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries. A statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa) Resuscitation. 2004;63(3):233–249. doi: 10.1016/j.resuscitation.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 16.International Society for Nomenclature of Paediatric and Congenital Heart Disease. [Accessed January 31, 2017];International paediatric and congenital cardiac code web page. Available at www.ipcc.net.
- 17.Gaies MG, Gurney JG, Yen AH, et al. Vasoactive-inotrope score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr Crit Care Med. 2010;11(2):234–238. doi: 10.1097/PCC.0b013e3181b806fc. [DOI] [PubMed] [Google Scholar]
- 18.Costello JM, Pasquali SK, Jacobs JP, et al. Gestational age at birth and outcomes after neonatal cardiac surgery: an analysis of the Society of Thoracic Surgeons Congenital Heart Surgery Database. Circulation. 2014;129(24):2511–2517. doi: 10.1161/CIRCULATIONAHA.113.005864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Larkin GL, Copes WS, Nathanson BH, Kaye W. Pre-resuscitation factors associated with mortality in 49,130 cases of in-hospital cardiac arrest: a report from the national registry for cardiopulmonary resuscitation. Resuscitation. 2010;81(3):302, 311. doi: 10.1016/j.resuscitation.2009.11.021. [DOI] [PubMed] [Google Scholar]
- 20.Lasa JJ, Rogers RS, Localio R, et al. Extracorporeal cardiopulmonary resuscitation (E-CPR) during pediatric in-hospital cardiopulmonary arrest is associated with improved survival to discharge: A report from the American Heart Association’s Get With the Guidelines-Resuscitation (GWTG-R) Registry. Circulation. 2016;133(2):165–176. doi: 10.1161/CIRCULATIONAHA.115.016082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Raymond TT, Cunnyngham CB, Thompson MT, et al. Outcomes among neonates, infants, and children after extracorporeal cardiopulmonary resuscitation for refractory in-hospital pediatric cardiac arrest: a report from the National Registry of Cardiopulmonary Resuscitation. Pediatr Crit Care Med. 2010;11(3):362–371. doi: 10.1097/PCC.0b013e3181c0141b. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.