Abstract
Background
Cancer education is essential for improving cancer prevention and biobanking knowledge among racial-ethnic minorities, with the goal of increasing diversity and representativeness of biospecimen collections. However, little is known about the communication modalities for optimal delivery of information.
Methods
We examined feasibility of recruitment and compared communication modalities for delivering cancer prevention and biobanking education to Hispanics. Communication modalities were evaluated using participation rates and change in knowledge, attitudes, self-efficacy, intention, receptivity, and trust. Enrollment in a biobanking registry was a behavioral outcome. Community members in Ponce, Puerto Rico and Tampa, Florida were recruited. Participants (N=254) were randomized to one of three communication modalities: standard dissemination (mailed materials); enhanced dissemination (mailed materials plus follow-up call); and ‘charla’ (face-to-face group discussion). Participants completed questionnaires about their knowledge, attitudes, self-efficacy, intentions, receptivity, and trust regarding biobanking and cancer prevention pre- and post-intervention.
Results
Knowledge, attitudes, and self-efficacy were improved among all three modalities. Although the greatest increases in knowledge were observed when the information was delivered via charla, the charla had the lowest participation rate. The standard and enhanced dissemination modalities were more feasible for delivering cancer prevention and biobanking education to Hispanics.
Conclusion
Lack of differences among the three modalities suggests culturally-tailored education may be sufficient to capture the community’s intention to participate in biobanking research, regardless of the delivery method for the education.
Impact
Results from this study contribute to the limited knowledge regarding Hispanics knowledge and intentions for biospecimen collection, and in the future may improve participation in this underrepresented group.
INTRODUCTION
The geographic proximity and large Hispanic populations in Florida and Puerto Rico presented an opportunity for the development of an academic partnership between the Ponce Health Sciences University-Research Institute, formerly known as Ponce School of Medicine (PSM), and Moffitt Cancer Center (MCC). Through a National Cancer Institute (NCI)-funded cooperative agreement, the PSM-MCC Partnership is a collaboration between a minority-serving institution (PSM) and NCI-designated comprehensive cancer center (MCC) to address cancer-related health disparities among Hispanics. Results from our previous outreach activities and research [8,13,17,22,23,27] and other public health research suggest that Hispanic audiences prefer more culturally appropriate, direct interpersonal communication methods over traditional United States (US) mainland-based cancer communication channels (e.g., distribution of educational materials). Cancer health communication channels can impact receptivity to the health information, as well as knowledge, attitudes, and behavior. Even when the health information is desired, if the delivery method is unappealing or uninteresting, knowledge acquisition may be low. As such, identifying effective and preferred communication channels when introducing health concepts or information is imperative to the success of the health message [18].
The National Academy of Sciences suggests that cultural considerations have been poorly applied in the context of health communication, and that adequate regard for culture requires research beyond the traditional variables of race, ethnicity, and socioeconomic status [9]. Traditional health communication approaches, including supplying educational materials and intensive face-to-face communication modalities (e.g., charla – a Spanish term referring to a group presentation and subsequent discussion by participants led by a trained health educator), have been shown to be effective for relaying health information to Hispanics [5]. These health education modalities utilize varying levels of direct interpersonal communication. Previous studies suggest that personal, individual, and face-to-face interactions are the preferred channel for communicating health messages to Hispanic populations [11,25]. Although the necessity of face-to-face health communication (i.e., charla) for Hispanic populations is frequently expressed in the literature [7], there is a lack of direct empirical evidence testing the effectiveness of this modality as a channel for increasing knowledge and influencing health behavioral change. However, considering that face-to-face health communication is more complex to implement and more resource-intensive for the educators as well as the audience, compared to traditional approaches (e.g., printed educational materials), a need exists for empirical evidence on cancer communication modalities with respect to producing behavioral change among Hispanics [15].
One understudied area of cancer health communication involves educating the community on biobanking. Biobanks are repositories that store biospecimens for research. Healthy control samples from diverse racial-ethnic groups must be represented in biobanks to better examine genetic and environmental risk factors for diseases, such as cancer, and to expand the generalizability of basic and translational oncology research [25]. However, racial-ethnic minorities are typically underrepresented in biobanks, and recruitment for biobanking can be challenging among minority communities because of barriers, such as perceived lack of benefit, medical mistrust, concern about the physical toll of donating, and media sensationalism on biospecimen misuse [6]. Encouraging contribution of biospecimens from healthy individuals for research requires innovative and effective approaches with attention to cultural values and preferences. As such, the purpose of this study was to assess the feasibility of three communication modalities for delivering biobanking education to Hispanics. Each modality represented different points along the personal contact continuum, ranging from the traditional approach of supplying educational materials to a more intensive face-to-face education channel.
METHODS
Study Design
This pilot randomized controlled trial (RCT) assessed the feasibility of three communication modalities for delivering cancer prevention and biobanking education to Hispanics in Tampa, Florida and Ponce, Puerto Rico. Informed consent was obtained from all individual participants included in the study. All participants received a pre-intervention (baseline) questionnaire, followed by random assignment to one of the three study arms: (i) standard dissemination, (ii) enhanced dissemination, or (iii) charla. Participants in all study arms received an 6-minute culturally-tailored DVD with a companion brochure, entitled “Biobanco: Una esperanza de cura para el cancer” (Biobanking: A hope of cure for cancer) that explained the biobanking process, conveyed the need for Hispanic healthy controls in biospecimen-based research, and addressed myths and misperceptions about research involving biological samples [16]. Participants also received an American Cancer Society standard informational pamphlet about cancer prevention and screening entitled: “Tome control de su salud y reduzca su riesgo de cancer” (Take control of your health and reduce your cancer risk). Participants in the standard dissemination arm were mailed the video and print materials. Participants in the enhanced dissemination arm were also mailed the video and print materials, and a telephone call was scheduled to occur approximately 10 days after receipt of the materials to provide an opportunity for personal contact to have questions answered regarding the mailed materials. A trained health educator completed phone calls with all participants in the enhanced dissemination arm. During these calls the health educator asked participants if they watched the DVD and read the print materials. Those participants who reported watching the DVD and reading the materials received an overview of the main points presented in the educational materials and where encouraged to ask questions. Participants who reported not watching the DVD at the time of the call, where given two additional attempts to comply with study requirements.
Participants in the charla arm were scheduled to attend a charla, held in the evening or on a weekend, in a community setting. During the charla, the video was viewed and the information in the print materials was presented by a health educator. After viewing the video and receiving the cancer prevention presentation, the health educator facilitated a discussion by inviting participants to ask questions regarding the materials they had viewed/read. Also the video and print materials were disseminated after the charla so participants could take them home. For those participants who did not attend their scheduled charla, two additional attempts were made to reschedule participants to a future charla. Participants who failed to attend a total of three scheduled charlas were considered non-completers. All charlas and enhanced dissemination calls were led by a health educator trained by the investigative team. Approximately three weeks after receipt of their assigned intervention, all participants were contacted by telephone to complete the post-intervention questionnaire. Following the post-intervention assessment, participants were asked if they were interested in enrolling in a biobanking registry.
Communication Modalities
The communication modalities included: (i) standard dissemination consisting of educational materials distributed via regular mail (this was the comparison condition representing the traditional US mainland approach to health communication); (ii) enhanced dissemination consisting of educational materials distributed via regular mail, plus a follow-up telephone call with the health educator to provide an opportunity for personal contact to have questions answered; and (iii) charla condition consisting of a face-to-face group discussion (this was the most personalized and intensive approach, which has frequently been recommended as the most culturally-appropriate and effective means of communicating health information to Hispanic populations).
Participant Recruitment
After receiving Institutional Review Board (IRB) approval at both sites, Hispanic community members in Ponce, Puerto Rico and the Tampa, Florida metropolitan area were recruited through local flyers (e.g., posted at churches, markets, and other community gathering places) and Spanish-language media channels (e.g., radio talk shows, television programs, and newspapers). Interested individuals were asked to call a toll-free telephone number to learn more about the study. Scripts were developed for the research assistants to ensure uniform information was shared with potential participants. Study staff at both sites received detailed training to ensure fidelity of the recruitment strategies. Scripts were practiced by study staff and recruitment protocols were set in place. From October, 2014 through June, 2015, callers were screened for the following eligibility criteria: self-report as Hispanic and preference for Spanish language materials; age ≥ 30 years; ability to speak and read standard Spanish; no personal history of cancer other than non-melanoma skin cancer; willingness and ability to participate in the study (e.g., transportation, in case randomized to the charla condition); provide verbal informed consent; and a valid mailing address and telephone number.
For individuals meeting the eligibility criteria, a study team member at each site explained that the study would provide information about cancer prevention and the value of biobanking for personal and community benefit, and that they would receive a $25 gift card for completing questionnaires before and after receipt of the educational intervention. A verbal consent script approved by both IRBs was utilized for obtaining informed consent before study participation.
Randomization
Participants were randomized to one of the three study arms. Random assignment was pre-generated by the study statistician and distributed to each site within sealed envelopes that were opened after an individual was screened, deemed eligible, and completed the pre-intervention assessment.
Measures
For feasibility, we assessed participation and study completion rates (proportion of consented participants who received the intervention [i.e., DVD and brochures] and proportion of consented participants who completed the study in each arm). Both receipt of intervention and completion rates of at least 75% were considered sufficient evidence of feasibility.
At baseline, we collected demographic and health-related information, including gender, age, race, educational level, relationship status, employment status, household income, insurance, and blood and organ donor status.
Self-reported knowledge, attitudes, self-efficacy and intentions toward biobanking were assessed pre- and post-intervention using the Spanish Biobanking Attitudes and Knowledge Survey (BANKS-SP) [1] and the Biomedical Research Trust Scale (BRTS-SP) [2]. Cancer prevention knowledge items (related to the Spanish language cancer prevention print material) were developed by our study team. Each measure underwent a multi-step process for appropriate translation and validity based on the Brislin Model of Translation [4,10]. To ensure suitability with respect to culture and literacy level, all measures were reviewed by our Community Advisory Panels in Ponce, Puerto Rico and Tampa, Florida.
Cancer Prevention Knowledge Scale
General cancer prevention knowledge was assessed by eight factual statements about cancer prevention. The responses on the scale were “yes,” “no,” and “don’t know,” with correct answers scored 1, and incorrect or don’t know answers scored 0. The scale score was calculated by adding all item scores. Higher scores reflect greater cancer prevention knowledge.
BANKS-SP
The 43-item BANKS-SP includes three single-item measures of intention to donate a biospecimen and receptivity to learning more about biospecimen donation and biobanking, as well as three scales measuring biobanking knowledge, biobanking attitudes, and self-efficacy for donating a biospecimen [28].
BANKS-SP-Knowledge
The knowledge scale includes 16 items, and each item provides a factual statement about biospecimen donation and biobanking. The responses on the scale are “yes,” “no,” and “don’t know.”
BANKS-SP-Attitudes
The attitudes scale includes 12 items measuring attitudes towards biospecimen donation and biobanking. Each item includes either a positive or negative attitude statement, which a person would rate using a five-point Likert scale ranging from “strongly agree” to “strongly disagree.” The 12-item BANKS-SP-Attitudes scale has demonstrated adequate internal consistency (Cronbach’s α =.79) and construct validity [1].
BANKS-SP-Self-Efficacy
The self-efficacy scale includes 12 items and each queried the person’s confidence in donating a biospecimen to a biobank given different situations. The numeric rating scale ranges from 0 to 100, with 0 indicating “cannot do” and 100 indicating “highly certain I can do.” The 12-item BANKS-SP self-efficacy scale has demonstrated good internal consistency (Cronbach’s α =.91) and construct validity [1].
BANKS-SP-Intention and Receptivity
The intention and receptivity section included three items related to the participant’s intention to donate blood, intention to donate urine, and receptivity to learning more about biospecimen donation and biobanking. All items are measured on a five-point Likert scale ranging from “definitely yes” to “definitely no”.
BRTS-SP
The BRTS-SP included 10 items assessing trust in researchers and institutions associated with biomedical research. All items are measured on a 0–10 Likert scale ranging from “I do not trust” to “I completely trust.” The 10-item BRTS-SP has demonstrated strong internal consistency (Cronbach’s α =.91) and construct validity [2].
Biobanking Registration
After completing the post-intervention assessment, participants were asked if they would be willing to have their contact information stored in a biobanking registry. Participants were told if they enrolled in the registry, they were permitting a researcher from MCC or PSM to contact them to see if they qualified for and were interested in participating in future research studies that may involve the collection of biospecimens from Hispanic participants. Given the limitations of intention measures at predicting future behavior [21], this measure permitted a direct behavioral outcome, albeit still removed from actual biospecimen donation.
Data Analysis
Statistical analyses were conducted using SAS v9.4 (Cary, NC). Descriptive statistics were calculated for all variables. Site comparisons (Florida vs. Puerto Rico) were conducted to assess potential confounding factors or variables that may affect interpretation of the results. Comparisons of the three interventions were conducted using statistics most appropriate for the measure: chi-square and logistic regression for discrete measures (e.g., biobanking registration), and t-tests and general linear models for continuous variables (e.g., biobanking knowledge). Alpha was .05 for all inferential statistical tests, including follow-up analyses of significant main effects involving group (three levels) and any significant interaction.
RESULTS
Participant Characteristics
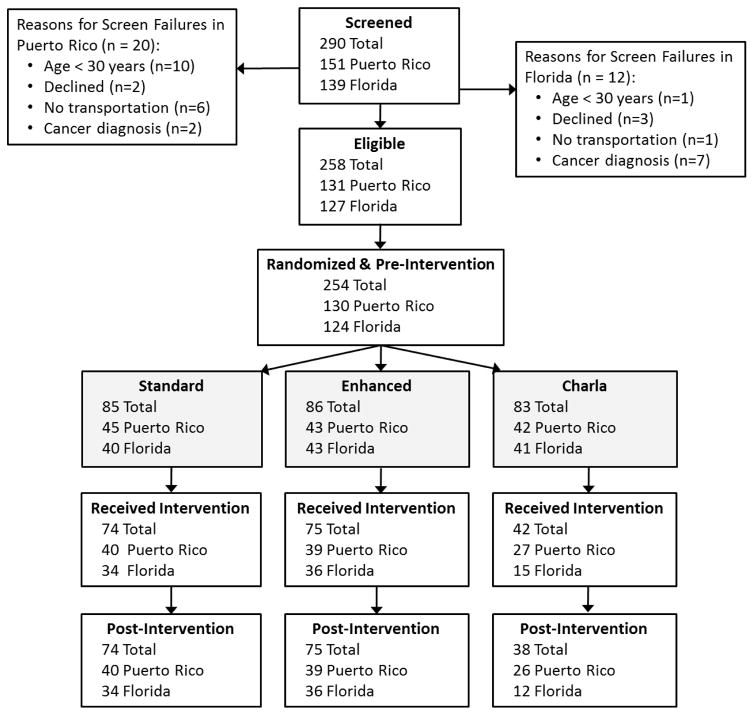
Figure 1 presents data on study recruitment, study participation, and study completion by intervention condition and site. A total of 290 Hispanic community members from Ponce, Puerto Rico (n = 151) and the Tampa Bay area, Florida (n = 139) were screened (Figure 1) over a period of 9 months. Of these individuals, 254 (130 in Puerto Rico, 124 in Florida) were eligible for study participation and randomly assigned to one of three communication modalities: standard dissemination (n = 85), enhanced dissemination (n = 86), or charla (n = 83). A total of 187 participants (74 standard dissemination, 75 enhanced dissemination, and 38 charla) completed the study.
Fig. 1.
Participant Flow Diagram
Table 1 presents descriptive statistics for participant characteristics by intervention condition for those who completed the post-intervention questionnaire. The majority of the participants were white, Hispanic, female, 40–60 years of age, had a high school diploma, and were of lower income, and insured. Chi-square and one-way analysis of variance analyses did not reveal any significant group differences. When comparing the Puerto Rico and Florida sites, chi-square and t-tests revealed several significant differences. The mean age of Florida participants (52.5 years) was significantly greater than that of Puerto Rico participants (47.8 years, P = 0.008). A significantly higher percentage of Puerto Rico participants reported an annual income less than $40,000 (93% vs. 79%, P = 0.012). However, 11% of Puerto Rico and 26% of Florida participants declined to answer this question. Among the health-related variables, participants in Puerto Rico were more likely to report having medical insurance (92% vs. 67%, P < 0.0001) and a primary care provider (83% vs. 69%, P = 0.022), whereas Florida participants were more likely to report previously donating blood (49% vs. 31%, P = 0.013) or being a registered organ donor (56% vs. 36%, P = 0.007).
Table 1.
Demographic and Health-related Variables by Group for Completers
| Variable | Standard Dissemination (N = 74) | Enhanced Dissemination (N = 75) | Charla (N = 38) |
|---|---|---|---|
|
| |||
| Site | |||
| Puerto Rico/Florida (n/n) | 40/34 | 39/36 | 26/12 |
|
| |||
| Demographic Variables | |||
| Sex, male (%) | 24.3 | 29.3 | 31.6 |
| Age in years, mean (SD) | 51.3 (12.6) | 49.2 (11.6) | 48.4 (11.3) |
| Race (%) | |||
| White | 56.2 | 72.0 | 65.8 |
| Black/African American | 12.3 | 5.3 | 7.9 |
| Native American | 6.9 | 5.3 | 0.0 |
| Other | 24.7 | 17.3 | 23.7 |
| Mixed | 0.0 | 0.0 | 2.6 |
| Preferred language, Spanish (%) | 98.7 | 98.7 | 97.4 |
| Education (%) | |||
| Less than high school diploma | 13.5 | 14.7 | 7.9 |
| High school diploma or GED | 41.9 | 32.0 | 26.3 |
| Associate degree | 20.3 | 17.3 | 21.1 |
| Bachelor degree | 16.2 | 24.0 | 36.8 |
| Master or doctorate degree | 8.1 | 12.0 | 7.9 |
| Married or living with partner (%) | 50.0 | 51.4 | 55.3 |
| Employment status (%) | |||
| Full-time | 32.4 | 37.0 | 47.4 |
| Part-time | 12.2 | 9.6 | 2.6 |
| Homemaker | 16.2 | 24.7 | 31.6 |
| Retired | 10.8 | 11.0 | 10.5 |
| Unable to work | 12.2 | 9.6 | 2.6 |
| Unemployed | 16.2 | 8.3 | 5.3 |
| Annual household income, up to $40k (%) | 91.7 | 82.3 | 87.9 |
|
| |||
| Health-related Variables | |||
| Insured (%) | 81.1 | 76.0 | 92.1 |
| Primary care physician/nurse (%) | 78.4 | 72.0 | 81.1 |
| Loved one with cancer history (%) | 67.6 | 64.0 | 76.3 |
| Previously donated blood (%) | 37.0 | 45.3 | 31.6 |
| Registered organ donor (%) | 41.9 | 52.0 | 36.8 |
Abbreviations: GED, general educational development; SD, standard deviation.
Feasibility
Of the 290 screened individuals, 151 were from Puerto Rico and 139 were from Florida. Of the 254 who were eligible and randomized in the study, 130 were from Puerto Rico and 124 were from Florida. Overall, 87.1% (86.1% in Puerto Rico, and 89.2% in Florida) of the screened individuals were eligible to participate in the study. Four additional screened and eligible individuals were not randomized because they did not provide consent.
Study completion rates were not equal across the three intervention conditions. Chi-square analyses revealed a significantly lower completion rate for the charla group (46%) compared with the standard (87%) and enhanced (87%) groups (P values < 0.0001). Within the charla group, Chi-square analyses revealed a significantly lower completion rate at the Florida site (29%) compared with the Puerto Rico site (62%; P = 0.003). Across all participants, one demographic measure predicted study completion. Non-white participants were less likely to complete the study than white participants (65% vs. 79%, P = 0.010).
Intervention Measures
Table 2 presents the pre- and post-intervention self-report measures by intervention group for those who completed the study. Primary analyses were performed using linear regression with intervention group, time (pre- vs. post-intervention), and their interaction as the predictors. Preliminary analyses found no significant differences among the three groups for any of the measures at the pre-intervention time point.
Table 2.
Intervention Measures and Biobanking Registration by Group for Completers
| Intervention Measure (range) Timepoint | Mean (SD) Scores
|
||
|---|---|---|---|
| Standard Dissemination (N = 74) | Enhanced Dissemination (N = 75) | Charla (N = 38) | |
|
| |||
| Knowledge (0–16) | |||
| Pre-intervention | 8.1 (2.4) | 7.9 (2.6) | 7.3 (2.8) |
| Post-intervention | 11.2 (2.5) | 11.6 (2.5) | 12.0 (2.1) |
|
| |||
| Receptivity (1–5) | |||
| Pre-intervention | 4.4 (0.8) | 4.5 (0.7) | 4.8 (0.4) |
| Post-intervention | 4.4 (1.0) | 4.7 (0.5) | 4.7 (0.5) |
|
| |||
| Intention to donate urine (1–5) | |||
| Pre-intervention | 4.4 (1.0) | 4.6 (0.7) | 4.6 (0.8) |
| Post-intervention | 4.3 (1.1) | 4.7 (0.5) | 4.7 (0.5) |
|
| |||
| Intention to donate blood (1–5) | |||
| Pre-intervention | 4.1 (1.2) | 4.5 (0.7) | 4.7 (0.5) |
| Post-intervention | 4.2 (1.2) | 4.5 (0.8) | 4.6 (0.5) |
|
| |||
| Attitude (12–60) | |||
| Pre-intervention | 47.0 (5.0) | 48.0 (5.9) | 47.9 (5.3) |
| Post-intervention | 49.2 (5.4) | 50.5 (6.5) | 50.7 (4.3) |
|
| |||
| Self-efficacy (0–120) | |||
| Pre-intervention | 76.1 (31.3) | 77.8 (30.6) | 76.6 (28.7) |
| Post-intervention | 84.4 (31.9) | 88.7 (29.2) | 83.6 (26.3) |
|
| |||
| Trust (0–100) | |||
| Pre-intervention | 69.2 (16.4) | 69.7 (19.7) | 68.3 (17.4) |
| Post-intervention | 69.2 (19.4) | 70.4 (21.6) | 70.7 (18.5) |
|
| |||
| Cancer prevention knowledge (0–8) | |||
| Pre-intervention | 5.4 (1.3) | 5.6 (1.5) | 6.0 (1.6) |
| Post-intervention | 5.8 (1.2) | 5.9 (1.4) | 6.5 (1.1) |
|
| |||
| Registered for donation | |||
| % of randomized | 77.7 | 80.2 | 43.4 |
|
| |||
| % of completers | 89.2 | 92.0 | 94.7 |
There was a significant increase in biobanking knowledge from pre- to post-intervention across all three modalities (P < 0.0001). This increase was modified by an interaction of time and intervention (P = 0.028). Tukey’s post-hoc comparisons of change revealed that the mean improvement in biobanking knowledge was greater for the charla group (4.7) than the standard dissemination group (3.1).
There was a significant increase in cancer prevention knowledge (P < 0.001). There was also a significant group difference (P = 0.018) with charla participants reporting a higher level of cancer prevention knowledge than those receiving standard intervention (P = 0.001). The time x intervention interaction was not significant.
Positive attitude towards and self-efficacy about biobanking also increased significantly (P values < 0.0001) across conditions. For these two variables, neither the main effect for intervention nor the time x intervention interaction was significant.
There were no significant increases over time for the following four variables: intention to provide urine to a biobank, intention to provide blood to a biobank, receptivity to learn more about biospecimen donation and biobanking, and trust in biomedical research. Their time x intervention interactions also were not significant. Although there were no significant group differences for receptivity and trust, there were significant differences for intention to donate blood and intention to donate urine to a biobank (P values < 0.008). Tukey’s post-hoc tests showed that the charla group had a higher average score than the standard dissemination group for each intention variable (P values < 0.028).
Biobanking Registration
More than 91% of study completers agreed to enroll in the biobanking registry (Table 2). Although no significant difference was found among the three groups (P = 0.53), the charla group had the highest percentage of enrollment of those who completed the study (95%). However, the charla group had the lowest percentage of registered participants relative to randomized participants (46%) because of the much lower rate of participants who received the intervention and completed the study.
To better understand registry enrollment, post-intervention measures were explored as predictors of registration. Using logistic regression, five variables were found to be significant positive predictors (P values < 0.05): receptivity, intention to bank urine, intention to bank blood, self-efficacy, and biomedical research trust. Not surprisingly, these self-report measures were significantly correlated (r values ranging from 0.21 to 0.78; P values < 0.005).
DISCUSSION
To our knowledge, this is the first RCT to examine multiple communication channels for delivering cancer prevention and biobanking education to Hispanics. The study is deemed highly feasible in terms of screening, eligibility, and randomization. Results support the effectiveness of traditional health communication methods, specifically standard dissemination, enhanced dissemination, and charla, for increasing biobanking and cancer prevention knowledge in Hispanics. In addition, positive changes in attitude and self-efficacy toward biobanking were observed across the communication methods.
Interestingly, our assessment of feasibility showed the standard and enhanced dissemination modalities may be more feasible when compared to face-to-face communication. As stated by Bowen et al, successful implementation of an intervention refers to the likelihood and manner in which an intervention can be fully executed as planned and proposed [3]. In this study, we successfully delivered the intervention to 74 participants in the standard dissemination group and 75 participants in the enhanced dissemination group; however, only 38 participants in the charla group were reached. The charla had the lowest participation and study completion rates because nearly half of the participants did not show up to receive the intervention, even when given two additional attempts to reschedule for a later date.
In addition, participants in the standard and enhanced dissemination groups reported viewing the video and reading the educational brochure that were mailed to them. Overall, participants in all three groups stated the video and brochures were interesting, and in each arm the delivery method was found to be acceptable based on participants’ feedback. Consistent with findings from a study seeking to improve colorectal cancer screenings, our study showed that culturally-tailored educational materials delivered to patients via mail (standard and enhanced dissemination) may offer a cost-effective approach to deliver effective cancer prevention education [20].
Although our findings demonstrate an overall increase in knowledge, positive attitudes, and self-efficacy across all three communication modalities, there was a notably greater increase in cancer prevention knowledge when the information was delivered in the charla setting. Face-to-face communication (such as the charla) has been recommended as the most culturally appropriate and effective means of communicating health information to a variety of populations, including Hispanics [24,25]. However, there has been a lack of data to support this approach as compared to other health education modalities. Certainly, given the differential participation rates across study arms, an alternative explanation is that the superior effects of the charla upon these variables may have reflected self-selection by the subgroup of participants who were most motivated or adherent.
Participant enrollment in the biobanking registry was very high (> 91%) across the three groups after receipt of the education. This is consistent with research demonstrating that when asked to participate in clinical trials, Latinos are willing to do so and enroll at the same rates as non-Hispanic whites [12,26]. Although the registration rate was high across all three arms, the low study completion rates in the charla group rendered this modality as the least effective overall. This study offers an improvement over traditional effort that measure behavioral intentions, as it provided an opportunity for registering in the biobank – a direct behavioral outcome. Self-efficacy for participating in biobanking increased significantly across conditions with no difference between the three modalities. Self-efficacy was found to be a significant positive predictor of biobanking registration. This suggests culturally-tailored education may be sufficient to increase a person’s confidence in donating a biospecimen, regardless of the delivery method of the education.
While culturally tailoring is an important aspect of health education interventions for Hispanics, there may be times when the communication channel is more meaningful, depending on the goal or outcome. For example, if he goal is to reach a broad group of people, to increase awareness, then standard dissemination methods may be appropriate. However, if the goal is to improve knowledge, then face-to-face communication may be warranted, although this channel is more resource intensive when compared to standard methods (e.g., staff time to schedule participant reminder calls, staff time to prepare for and deliver the charla) and likely to reach smaller groups of people.
This pilot study has several strengths. First, the randomized design limited the observed and unobserved differences in participant characteristics among the intervention groups. Second, the educational interventions were culturally and linguistically tailored to the study population, thereby eliminating a considerable barrier to the delivery of health information. Third, the inclusion of two geographically diverse Hispanic communities (Ponce, Puerto Rico and Tampa, Florida) enhanced the generalizability of the findings from this study. Finally, the inclusion of a behavioral outcome (enrollment in biobanking registry) in addition to self-reported intentions represents an additional strength of the study design.
There are, however, a number of limitations to consider when interpreting our results. Intention to donate to a biobank was used as one of the outcome measures and health behavior research suggests there is poor correlation between intentions and actual behaviors [19]. We were unable to locate previously published studies that report how well intentions to donate to biobanks predict actual behavior in donating biospecimens. Although the majority of participants enrolled in the biobanking registry, they have yet to be contacted for participation requiring a biospecimen. Future studies will examine the rate of agreement to provide biospecimens when contacted.
In conclusion, results from this study contribute to the limited knowledge base regarding Hispanics and biospecimen collection, particularly since this group is vulnerable to underrepresentation in cancer research [14]. Further research to build upon these findings will help broaden our understanding of the impact of health education/communication on biobanking and cancer prevention knowledge in the Hispanic population. Future research is needed to better understand barriers to charla attendance and strategies for overcoming those and could incorporate a cost-effectiveness approach or include technology-mediated communication that mimics a charla but could be done from home. In addition, future research will explore the impact of the cultural tailoring on improving Hispanics participation in research as a healthy control and in screening and other cancer prevention initiatives. It is also important to explore the role of sub-ethnicities in Hispanic research and not treat the group as homogenous. Our future studies will continue to explore sub-ethnic similarities and differences to identify the extent to which culturally tailored materials need adaptation to accommodate.
Acknowledgments
We would like to acknowledge the assistance of Wendy Rojas. This work was supported by the National Cancer Institute’s Center to Reduce Cancer Health Disparities of the National Institutes of Health, for the Ponce School of Medicine-Moffitt Cancer Center Partnership [U54 CA163068 and U54 CA163071]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This work has been supported in part by the Survey Methods Core and Biostatistics Core Facilities at the H. Lee Moffitt Cancer Center & Research Institute; an NCI designated Comprehensive Cancer Center (P30-CA076292).
References
- 1.Arevalo M, Jacobsen PB, Gwede CK, Meade CD, Quinn GP, Luque JS, San Miguel G, Watson D, Wells KJ. Development and validation of the Biobanking Attitudes and Knowledge Survey-Spanish (BANKS-SP) Journal of Community Genetics (under review) 2016 doi: 10.1007/s12687-016-0280-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baik SH, Arevalo M, Gwede Cl, Meade CD, Jacobsen PB, Quinn GP, Wells KJ. Development and validation of the Biomedical Research Trust Scale (BRTS) in English and Spanish. 2016 doi: 10.1177/1556264616668973. (under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bowen DJ, Kreuter M, Spring B, Cofta-Woerpel L, Linnan L, Weiner D, Bakken S, et al. How we design feasibility studies. Am J Prev Med. 2009;36(5):452–457. doi: 10.1016/j.amepre.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brislin. Back-translation for cross-cultural research. Journal of Cross-Cultural Psychology. 1970;1:185–216. [Google Scholar]
- 5.Cline R. Everyday interpersonal communication and health. In: Dorsey A, Thompson T, Miller K, Parrott R, editors. Handbook of Health Communication. Mahwah, NJ: Lawrence Erlbaum Associates Inc; 2003. pp. 285–318. [Google Scholar]
- 6.Dang JH, Rodriguez EM, Luque JS, Erwin DO, Meade CD, Chen MS., Jr Engaging diverse populations about biospecimen donation for cancer research. J Community Genet. 2014;5(4):313–327. doi: 10.1007/s12687-014-0186-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elder JP, Ayala GX, Parra-Medina D, Talavera GA. Health communication in the Latino community: issues and approaches. Annu Rev Public Health. 2009;30:227–251. doi: 10.1146/annurev.publhealth.031308.100300. [DOI] [PubMed] [Google Scholar]
- 8.Gwede Clement K, Castro Eida, Brandon Thomas H, McIntyre Jessica, Meade Cathy D, Munoz-Antonia Teresita, Simmons Vani N, Vadaparampil Susan T, Jimenez Julio, Quinn Gwendolyn P. Developing Strategies for Reducing Cancer Disparities via Cross-Institutional Collaboration Outreach Efforts for the Partnership Between the Ponce School of Medicine and the Moffitt Cancer Center. Health promotion practice. 2012;13(6):807–815. doi: 10.1177/1524839911404227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.IOM. Institute of Medicine. Speaking of health: assessing health communication strategies for diverse populations. Washington, DC: National Academies Press; 2002. Report No. 13: 978-0-309-11061-7. [PubMed] [Google Scholar]
- 10.Jones PS, Lee JW, Phillip LR, Zhang ZE, Jaceldo KB. An adaptation of Brislin’s translational model for cross-cultural research. Nursing Research. 2001;(50):300–304. doi: 10.1097/00006199-200109000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Juarbe T. People of Puerto Rican heritage. In: Purnell LD, Paulanka BJ, editors. Transculatural health care: a culturally competent approach. 2. Philadelphia: F.A. Davis; 1998. pp. 307–326. [Google Scholar]
- 12.Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DEH. Acculturation and Latino health in the United States: A review of the literature and its sociopolitical context. Annual Review of Public Health. 2005;(26):367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Litvin EB, Rojas A, Brandon TH, Quinn G, Meade CD, Jimenez J, Castro E, Diaz Z, Simmons VN. Cultural Acceptability of a Smoking Relapse Prevention Intervention for Pregnant Women in Puerto Rico: Providers’ Feedback. Hisp Health Care Int. 2011;9(3):117–126. doi: 10.1891/1540-4153.9.3.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Loffredo Christopher A, Luta Gheorghe, Wallington Sherrie, Makgoeng Solomon B, Selsky Claire, Mandelblatt Jeanne S, Adams-Campbell Lucile L Region 1 Bio-specimen Management of Cancer Health Disparities Program. Knowledge and willingness to provide research biospecimens among foreign-born Latinos using safety-net clinics. Journal of community health. 2013;38(4):652–659. doi: 10.1007/s10900-013-9660-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Luque JS, Quinn GP, Montel-Ishino FA, Arevalo M, Bynum SA, Noel-Thomas S, Wells KJ, Gwede CK, Meade CD Partners Tampa Bay Community Cancer Network. Formative research on perceptions of biobanking: what community members think. J Cancer Educ. 2012;27(1):91–99. doi: 10.1007/s13187-011-0275-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McIntyre J, Moreno L, Jiménez J, Castro EM, Gwede CK, Meade CD, Brandon TH, Simmons VN, Vadaparampil ST, Quinn GP. Adapting Spanish-Language Educational Materials about Biobanking for Hispanics in Puerto Rico. PLOS ONE. 2016 (under review) [Google Scholar]
- 17.Quinn G, Jimenez J, Simmons VN, Castro E, Gwede C, Vadaparampil S, McIntyre J, Antonia TM, Meade C, Brandon TH. Practice Notes: Ponce School of Medicine and Moffitt Cancer Center Cancer Outreach. Health Education & Behavior. 2010;37:777–778. [Google Scholar]
- 18.Resnicow K, Braithwaite RL. Cultural sensitivity in public health. In: Braithwaite RL, Taylor S, editors. Health issues in the black community. 2. San Francisco, CA: Jossey-Bass; 2001. pp. 516–542. [Google Scholar]
- 19.Schwarzer R. Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Applied Psychology-an International Review-Psychologie Appliquee-Revue Internationale. 2008;57(1):1–29. doi: 10.1111/j.1464-0597.2007.00325.x. [DOI] [Google Scholar]
- 20.Sequist TD, Franz C, Ayanian JZ. Cost-effectiveness of patient mailings to promote colorectal cancer screening. Med Care. 2010;48(6):553–557. doi: 10.1097/MLR.0b013e3181dbd8eb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sheeran Paschal. Intention—behavior relations: A conceptual and empirical review. European review of social psychology. 2002;12(1):1–36. [Google Scholar]
- 22.Simmons Vani N, Jiménez Julio C, Castro Eida, Litvin Erika B, Gwede Clement K, Vadaparampil Susan T, McIntyre Jessica, Meade Cathy D, Brandon Thomas H, Quinn Gwendolyn P. Initial efforts in community engagement with health care providers: perceptions of barriers to care for cancer patients in Puerto Rico. Puerto Rico health sciences journal. 2011;30(1):28. [PMC free article] [PubMed] [Google Scholar]
- 23.Simmons Vani N, Quinn Gwendolyn, Litvin Erika B, Rojas Ariz, Jimenez Julio, Castro Eida, Meade Cathy D, Brandon Thomas H. Transcreation of validated smoking relapse-prevention booklets for use with Hispanic populations. Journal of Health Care for the Poor and Underserved. 2011;22(3):886. doi: 10.1353/hpu.2011.0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tong EK, Fung LC, Stewart SL, Paterniti DA, Dang JH, Chen MS., Jr Impact of a biospecimen collection seminar on willingness to donate biospecimens among Chinese Americans: results from a randomized, controlled community-based trial. Cancer Epidemiol Biomarkers Prev. 2014;23(3):392–401. doi: 10.1158/1055-9965.EPI-13-0744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Torres JB. Communication patterns and direct social work practice with Latinos in the US. J Human Behav Soc Environ. 2000;3:23–42. [Google Scholar]
- 26.Umutyan A, Chiechi C, Beckett LA, Paterniti DA, Turrell C, Gandara DR, Davis SW, Wun T, Chen MS, Jr, Lara PN., Jr Overcoming barriers to cancer clinical trial accrual: impact of a mass media campaign. Cancer. 2008;112(1):212–219. doi: 10.1002/cncr.23170. [DOI] [PubMed] [Google Scholar]
- 27.Vadaparampil ST, Quinn GP, Dutil J, Puig M, Malo TL, McIntyre J, Perales R, August EM, Closser Z. A pilot study of knowledge and interest of genetic counseling and testing for hereditary breast and ovarian cancer syndrome among Puerto Rican women. J Community Genet. 2011;2(4):211–221. doi: 10.1007/s12687-011-0058-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wells KJ, Arevalo M, Meade CD, Gwede CK, Quinn GP, Luque JS, San Miguel G, et al. Development and validation of the biobanking attitudes and knowledge survey (BANKS) Cancer Epidemiol Biomarkers Prev. 2014;23(3):374–382. doi: 10.1158/1055-9965.EPI-13-0746. [DOI] [PMC free article] [PubMed] [Google Scholar]