Abstract
Objectives
The nationwide effort to make HIV testing part of routine care in the emergency department (ED) has met with some success; however, one commonly-cited challenge to implementation is the consent process. Tablet kiosks offer one potential strategy to overcome this barrier. This pilot study aims to examine patient acceptability of using a tablet kiosk to provide and comprehend HIV testing consent.
Methods
This cross-sectional survey was conducted in an academic ED that serves a socioeconomically disadvantaged inner-city population. Coordinators recruited a convenience sample of ED patients who were interested in HIV testing, but had not yet completed informed consent. Subjects were guided through a mock pre-test counseling and consent process using a tablet kiosk. Subjects then completed a survey of HIV consent comprehension and acceptability of tablet kiosk use for STD and HIV testing.
Results
Subjects were 50.3% female, Black (74.4%), had an education level of high school degree or less (61.3%), and reported previous experience using a kiosk or tablet (68.8%). Subjects found the tablet kiosk very easy or easy to use (83.9%) and reported they were very or mostly comfortable using the tablet kiosk to consent to HIV testing (89.4%). Overall, subjects understood the aspects of consent required by Maryland law and our institution; they stated that HIV testing was voluntary (Q1: 93.0%, n = 185) and that refusal of HIV testing would not impact their clinical care (Q2: 98.5%, n = 196; Q3: 99.0%, n = 197).
Conclusions
Following a mock HIV consent process using a tablet kiosk, subjects reported they were comfortable using the tablet kiosk, found the tablet kiosk easy to use, and enjoyed using the tablet kiosk to learn about and provide consent for HIV testing. Subjects also demonstrated a remarkably high rate of comprehension of vital components of the HIV testing consent.
Keywords: HIV consent, HIV testing, tablet kiosk, patient acceptability, comprehension
Emergency Departments (ED) have been increasingly called on to take part in the public health strategy of routine HIV screening. (CDC) The availability of electronic medical records, updated testing technology including CLIA-waived point of care tests, updated CDC guidelines for consent language including opt-out language have allowed many EDs to implement routinized HIV screening programs. The rationale for these programs has been extensively described and widely accepted 1, but practical aspects of the HIV testing process have been reported in the literature that prevent streamlining and integrating HIV testing into ED clinical operations2. From a clinical perspective, the testing process involves many steps including: patient engagement, offering HIV testing, obtaining consent, requisitioning the test, and finally performing and resulting the test. Numerous barriers have been reported in the literature including: inadequate/insufficient time for testing3, financial burdens4, lack of necessary resources, the pretest counseling/consent process5, 6, and concerns regarding follow up for results/linkage to care.
Numerous studies specifically cite the lack of time needed to obtain consent for HIV testing, inadequate training of clinical staff 7, and patient confusion of opt-out versus opt-in testing8. Despite these barriers, several approaches are being evaluated to increase patient comprehension of consent. Notably, the removal of written consent per CDC recommendation has correlated with the increase in San Francisco city-wide testing rate9. Furthermore, researchers have begun investigating the effectiveness of new formats and technologies for obtaining consent and increasing patient understanding of consent for HIV testing including audiotape and booklet educational materials10, video counseling11, kiosks12, and computer-based tools13.
Novel technology systems (specifically touch screen kiosks) have been previously investigated by our group in a series of pilot studies as a strategy for engaging interested patients and gathering essential information associated with HIV testing 14, 15.
This pilot study evaluated subjects’ perceived acceptability regarding the use of touch-screen tablet kiosks to assist in the HIV testing process in the ED as well as patient comprehension of the HIV consent process. Touch-screen tablet kiosks were used to provide subjects with a mock experience of the consent process for HIV testing.
Methods
This study was a cross-sectional survey conducted from March 2014 to July 2014 in an urban academic ED that serves a socioeconomically disadvantaged inner-city population with roughly 70,000 visits per year. Approximately 75% of ED patients are African American, 15% are currently or previously injection drug users, and approximately 6–8% of patients are HIV positive.
The ED currently has a hybrid, rapid, blood-based and point of care (POC) HIV testing program that was in place at the time of the study. Trained non-clinical staff (HIV testing facilitators) work in the ED and provide rapid POC HIV testing to eligible patients who meet the following criteria: aged 18–65 not tested within the last three months, not critically ill, able to provide informed consent, and have no known HIV diagnosis. Rapid blood-based testing is fully implemented into the clinical workflow and does not involve supplementary non-clinical staff.
Materials
The main outcome variable of consent comprehension was assessed via a verbally-administered survey, which consisted of six primary true/false questions that measured patient understanding of various aspects of HIV consent. Three questions were designed to reflect information required by Maryland state law, including the voluntary nature of HIV testing (question 1) and that refusal of HIV testing would not impact a patient’s clinical care (questions 2 and 3). The remaining three questions assessed supplementary information regarding the HIV testing process at our institution, specifically that following a reactive oral test, a confirmatory blood test will be performed (questions 4 and 5) and that positive results will be shared with the local Health Department (question 6). Moreover, some questions (e.g. questions 2 and 3, questions 4 and 5) were originally developed as paired items to assess knowledge of the same concept. When subjects answered a non-paired question incorrectly, additional follow-up questions were asked by the study coordinator in a yes/no format.
Additional outcome variables related to patient acceptability of kiosk use were assessed via survey that was also verbally administered by the study coordinator. Subjects were asked about their comfort with the tablet kiosk, if they liked using the tablet kiosk, its ease of use, their preference between the tablet kiosk and a healthcare worker, and their opinion of the language and length of the consent materials presented.
Procedure
This tablet kiosk consent study was approved by the Johns Hopkins Medicine Institutional Review Board, and all subjects provided verbal consent prior to any study-related activities.
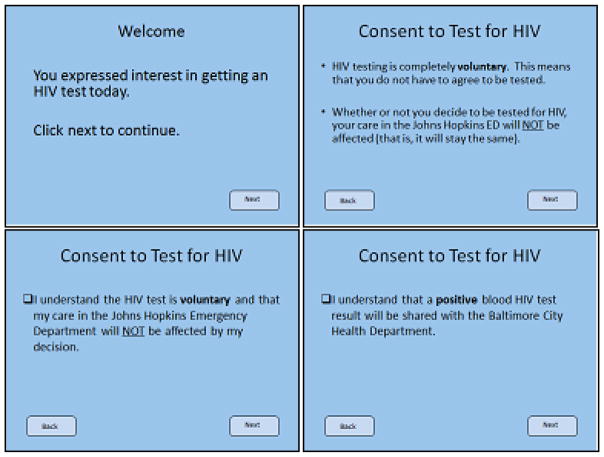
Study coordinators recruited a convenience sample of ED patients who were interested in having an HIV test, but had not yet completed informed consent for testing. Consent for the study was obtained via verbal consent and subjects were then given a touch-screen tablet kiosk that guided them through a mock pre-test counseling and HIV testing consent process developed using Microsoft PowerPoint, Microsoft Access, and Visual Basic. Material was presented visually through text on screen paired with audio recordings that were HHS 508 compliant. The mock pre-test counseling was designed to mimic in-person pre-test counseling that is standard of care and included all necessary components of HIV consent and testing processes at our institution. Subjects swiped or clicked the touch-screen tablet kiosk to progress through a collection of seven screens, as seen in figure 1. Screens one through four presented key material for the HIV consent and testing process, while screens five through seven asked subjects to “checkmark” boxes to indicate their understanding of the material.
Figure 1.
Screens 1–2 and 6–7 of touch-screen tablet kiosk.
After check marking the final item on the last screen, the subjects were finished with the tablet kiosk portion of study procedures and handed the tablet kiosk to the study coordinator. Subjects then completed a structured, Likert-type questionnaire including a demographics, a survey of HIV consent comprehension, and a survey of patient acceptability of tablet kiosk use for STD and HIV testing. Study coordinators verbally administered the questionnaire and manually recorded patient responses. Table 1.
Table 1.
Consent Comprehension Questions with Follow up Questions.
1. You do not have to be tested for HIV today. (T/F)
|
2. You will receive the same level of care in the Johns Hopkins Emergency Department even if you do not agree to an HIV test. (T/F)
|
| 3. You can decide not to be tested for HIV and your decision will not affect the services and treatment you receive in the Johns Hopkins Emergency Department. (T/F) |
4. If your oral HIV test result is positive, you do not need to have an additional blood test to find out if you really have HIV. (T/F)
|
5. If your oral HIV test result is negative, you will need to have an additional blood test to find out if you really have HIV. (T/F)
|
6. If your blood HIV test result is positive, the Johns Hopkins Hospital is required to share your result with the Baltimore City Health Department. (T/F)
|
Upon completion of all study-related procedures, subjects were consented and tested by our department’s HIV testing facilitators. Descriptive analyses were conducted to summarize demographic characteristics of subjects, acceptability of tablet or kiosk use, and comprehension of consent.
Results
During the study period, 202 subjects were enrolled. Data from three subjects were excluded if they were earlier consented at triage for an HIV test, previously enrolled in the study, or did not provide complete survey data. Overall, data from 199 subjects were included in analyses.
Subjects were approximately evenly distributed between males (49.7%) and females (50.3%) with an average age of approximately 43 years old. The majority of subjects were Black or African American (74.4 %), had obtained an education level of high school degree or less (61.3%), and reported using a computer or tablet 6–7 days a week (43.2%) (Table 2). Most subjects stated they had previous experience using a kiosk or tablet-like device (68.8%).
Table 2.
Demographic Characteristics of Subjects.
| N=199 | n (SD) | % |
|---|---|---|
| Age | 42.69 (13.00) | |
|
| ||
| Gender | ||
| Male | 99 | 49.7 |
| Female | 100 | 50.3 |
|
| ||
| Race | ||
| Black/African American | 148 | 74.4 |
| White | 36 | 18.1 |
| Two or More | 8 | 4.0 |
| Asian | 4 | 2.0 |
| Decline | 3 | 1.5 |
|
| ||
| Education | ||
| Middle school/Some high school | 44 | 22.1 |
| High School degree/GED | 78 | 39.2 |
| Trade School | 4 | 2.0 |
| Some college/associate’s degree | 45 | 22.6 |
| College degree or higher | 28 | 14.1 |
|
| ||
| Computer use days/week | ||
| 0 | 60 | 30.1 |
| 1–2 | 31 | 15.6 |
| 3–5 | 22 | 11.1 |
| 6–7 | 86 | 43.2 |
Generally, subjects reported a positive experience using the tablet kiosk as a means to give consent for HIV testing. A vast majority of subjects (83.9%) found the tablet kiosk very easy or easy to use, 89.4% reported they were very or mostly comfortable using the tablet kiosk to consent to HIV testing, and 77.9% of subjects liked using the kiosk to learn about the HIV testing and consent processes (Table 3a). Almost all subjects found the length of the informational program to be just right (95.0%) and agreed that the language and questions used in the program were very easy or easy to understand (94.9 %). When asked their preference between using the tablet kiosk and speaking with a healthcare professional about HIV testing, 21.1% of subjects preferred using a tablet kiosk, 29.6% preferred a healthcare professional, and 48.7% of subjects reported they would prefer both or had no preference (Table 3b).
Table 3a.
Subject Acceptability of Kiosk Tablet.
| N=199 | n (%) very much |
n (%) mostly |
n (%) somewhat |
n (%) not at all |
n (%) missing |
|
|---|---|---|---|---|---|---|
| Comfort using kiosk | 128 (64.3) | 50 (25.1) | 15 (7.5) | 5 (2.5) | 1 (0.5) | |
| Like using kiosk | 111 (55.8) | 44 (22.1) | 39 (19.6) | 4(2.0) | 1 (0.5) | |
|
n (%) very easy |
n (%) easy |
n (%) somewhat easy |
n (%) difficult |
n (%) very difficult |
n (%) missing |
|
| Easy to understand | 133 (66.8) | 56 (28.1) | 9 (4.5) | 1 (0.5) | ||
| Easy to use | 108 (54.3) | 59 (29.6) | 17 (8.5) | 4 (2.0) | 11 (5.5) |
Table 3b.
Responses to question “Do you prefer using the kiosk or talking to a healthcare professional about HIV testing?” with associated comments.
| n (%) | Associated comments | |
|---|---|---|
| Kiosk | 42 (21.1) | Kiosk is more private Kiosks are a good idea Great, but audio could be louder |
| HCW | 59 (29.6) | Tablet was repetitive, need to get the hang of it HCW is better because you can ask questions and understand better Prefer HCW because they can answer more questions |
| Both/either | 97 (48.7) | Prefer to ask questions after using kiosk Kiosk is more discreet Headphones would be nice for privacy Would like to ask follow up questions of HCW after using kiosk |
| Missing | 1 (0.5) |
Overall, subjects understood the aspects of consent required by Maryland law and our institution. An overwhelming majority of subjects correctly acknowledged that HIV testing was voluntary (Q1: 93.0%, n = 185) and that refusal of HIV testing would not impact their clinical care (Q2: 98.5%, n = 196; Q3: 99.0%, n = 197). Of the 14 subjects who answered question 1 incorrectly, 11 then answered a follow-up question correctly, 2 answered incorrectly, and 1 was not asked a follow up question. This reduced the error rate from 7.0% to 1.5% of all subjects. Upon further analysis, a greater portion of these 14 subjects had an education level of high school or less (71.4% compared to 61.3% in the larger sample) and reported daily computer use at a lower rate (21.4% compared to 43.2% in the larger sample). This could potentially explain a misunderstanding of this questionnaire item, especially due to its verbal administration. Of the 3 subjects who answered question 2 incorrectly, 0 then answered the follow-up question correctly, 2 answered incorrectly, and 1 participant was not asked a follow up question. However, 2 of these same subjects answered question 3 correctly. Since these questions assess the same concept, that their care would not change if the patient declined an HIV test, we could perhaps attribute this discrepancy to the wording differences between the two items.
Limitations
Data from this study should be interpreted with the following limitations in mind. Firstly, the study design did not include a control group to which comparisons of consent comprehension rates could be made. To our knowledge, there is no published data of patient comprehension of HIV consent to which findings from this study could be compared. A study with somewhat comparable outcomes12, demonstrated that 97% of subjects reported they had been informed about HIV testing when an opt-in kiosk consent process was used, compared to 46% of subjects when an opt-out kiosk consent process was used. Researchers operationalized comprehension as a subjects’ understanding of whether or not they had been informed about HIV testing. Patient self-report that they have been informed about HIV testing and HIV consent comprehension are associated; however, they are not analogous concepts.
A second limitation of this study is the impact of potential selection bias, due to the use of a convenience sample. During the recruitment period of this study, a triage RN-based HIV screening process was implemented at our ED. As part of this process, triage RNs offer HIV testing, consent willing patients, and place an order for an HIV test. HIV testing facilitators receive an EMR-generated page for the patient and proceed through the testing process as outlined in the methods section. This restricted our sample to those who had been missed by triage or declined an HIV test at triage, so as to avoid the potential confound of having already consented to an HIV test during the current visit.
Discussion and Conclusions
In the last decade, EDs have increasingly implemented HIV testing programs to meet the CDC’s 2006 recommendation for routine HIV screening for all persons 13 and older. Despite successes, many EDs encounter barriers to implementing a program streamlined with clinical care. An oft-cited barrier is the lengthy and elaborate consent process, for which touch-screen tablet kiosks provide a novel solution.
Findings from our study demonstrate high rates of patient acceptability for a tablet-based kiosk-facilitated consent process, the first study to demonstrate the acceptability of kiosks for HIV testing consent. Subjects were comfortable using the tablet kiosk during the mock HIV consent process, found the tablet kiosk easy to use, and enjoyed using the tablet kiosk to learn about and provide consent for HIV testing. Previous studies from our ED and elsewhere have demonstrated the acceptability and feasibility of using kiosks for patient registration and screening 16, offering HIV testing15, improving patient flow17, providing patients with information regarding public health interventions 18, 19, and providing patient education 20–22.
Several pilot proof of principle studies for using kiosks in the context of HIV have been performed in non-ED settings. In a study of kiosk-based HIV education in a primary care setting, authors concluded that kiosks are effective tools for delivering targeted HIV screening information 23. Other non-HIV related studies are also relevant to our project. One food safety education study, conducted in a primarily African American population, found that individuals with no college education preferred learning through kiosks over pamphlets and found that patients expressed significant interest in learning about other subject areas through kiosks 24.
Additionally, we found an extraordinary rate of comprehension of vital components of the HIV testing consent, including the voluntary nature of HIV testing (Q1: 93.0%, n = 185) and that refusal of HIV testing would not impact patient care (Q2: 98.5%, n = 196; Q3: 99.0%, n = 197). Although these findings are significant in their own right, it is of note that this study assessed patient acceptability and comprehension of HIV consent in a highly structured experiment without the complications of clinical and patient flow in a high volume episodic care center.
Further studies could explore the optimization of tablets/kiosks by fully integrating them into clinical flow and the electronic medical record. Jones 17 recommends that kiosks be integrated with services in order for kiosks to succeed in healthcare settings. Ideally, a tablet-kiosk could be used up front for patient registration (including providing insurance and billing information) 25, offer HIV screening to eligible patients, provide pre-test counseling information, obtain consent for an HIV test, and automatically trigger a test order when a patient consents. Preferably, this process would occur before a patient is even triaged up front by a triage RN. The face-to-face triage interaction would give the patient an opportunity to ask any questions regarding the HIV testing process and the potential to self-collect an oral swab for POC testing with supervision by an RN.
Table 4.
Subject Comprehension of HIV Consent and Testing.
| Consent Comprehension Questions N=199 |
True n (%) |
False n (%) |
|---|---|---|
| 1. You do not have to be tested for HIV today. | 185 (93.0) | 14 (7.0) |
| 2. You will receive the same level of care in the Johns Hopkins Emergency Department even if you do not agree to an HIV test. | 196 (98.5) | 3 (1.5) |
| 3. You can decide not to be tested for HIV and your decision will not affect the services and treatment you receive in the Johns Hopkins Emergency Department. | 197 (99.0) | 2 (1.0) |
| 4. If your oral HIV test result is positive, you do not need to have an additional blood test to find out if you really have HIV. | 38 (19.1) | 160 (80.4) |
| 5. If your oral HIV test result is negative, you will need to have an additional blood test to find out if you really have HIV. | 51 (25.6) | 148 (74.3) |
| 6. If your blood HIV test result is positive, the Johns Hopkins Hospital is required to share your result with the Baltimore City Health Department. | 191 (96.0) | 8 (4.0) |
Correct responses are bolded.
Acknowledgments
Funding: U54EB007958, NIBIB, NIH; U-01068613-01, NIH, NIAID
Funding
This work was supported by a grant from the National Institutes of Health U54EB007958. The authors would like to thank the HIV testing staff at Johns Hopkins Emergency Department for their assistance.
Footnotes
Declaration of Conflicting Interests
The authors declare that there is no conflict of interest.
References
- 1.Kelen GD, Rothman RE. Emergency department–based HIV testing: too little, but not too late. Ann Emerg Med. 2009;54:65–71. doi: 10.1016/j.annemergmed.2009.03.027. [DOI] [PubMed] [Google Scholar]
- 2.Moran GJ, Talan DA. Processes and models for HIV screening in the emergency department: can and should we do this? Ann Emerg Med. 2011;58:S172–S173. doi: 10.1016/j.annemergmed.2011.03.044. [DOI] [PubMed] [Google Scholar]
- 3.Arbelaez C, Wright EA, Losina E, et al. Emergency provider attitudes and barriers to universal HIV testing in the emergency department. J Emerg Med. 2012;42:7–14. doi: 10.1016/j.jemermed.2009.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Irvin CB, Flagel BT, Fox JM. The emergency department is not the ideal place for routine HIV testing. Ann Emerg Med. 2007;49:722. doi: 10.1016/j.annemergmed.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 5.Cohan D, Gomez E, Dowling T, et al. HIV testing attitudes and practices among clinicians in the era of updated Centers for Disease Control and Prevention recommendations. J Acquir Immune Defic Syndr. 2009;50:114–116. doi: 10.1097/QAI.0b013e31818d5f86. [DOI] [PubMed] [Google Scholar]
- 6.Jain CL, Wyatt CM, Burke R, et al. Knowledge of the Centers for Disease Control and Prevention’s 2006 routine HIV testing recommendations among New York City internal medicine residents. AIDS Patient Care STDS. 2009;23:167–176. doi: 10.1089/apc.2008.0130. [DOI] [PubMed] [Google Scholar]
- 7.Burke RC, Sepkowitz KA, Bernstein KT, et al. Why don’t physicians test for HIV? A review of the US literature AIDS. 2007;21:1617–1624. doi: 10.1097/QAD.0b013e32823f91ff. [DOI] [PubMed] [Google Scholar]
- 8.Haukoos JS, Hopkins E, Byyny RL, et al. Patient acceptance of rapid HIV testing practices in an urban emergency department: assessment of the 2006 CDC recommendations for HIV screening in health care settings. Ann Emerg Med. 2008;51:303–309. e1. doi: 10.1016/j.annemergmed.2007.10.028. [DOI] [PubMed] [Google Scholar]
- 9.Zetola NM, Klausner JD, Haller B, et al. Association between rates of HIV testing and elimination of written consents in San Francisco. JAMA. 2007;297:1057–1062. doi: 10.1001/jama.297.10.1061. [DOI] [PubMed] [Google Scholar]
- 10.Coletti AS, Heagerty P, Sheon AR, et al. Randomized, controlled evaluation of a prototype informed consent process for HIV vaccine efficacy trials. JAIDS J Acquired Immune Defic Syndromes. 2003;32:161–169. doi: 10.1097/00126334-200302010-00008. [DOI] [PubMed] [Google Scholar]
- 11.Calderon Y, Leider J, Hailpern S, et al. A randomized control trial evaluating the educational effectiveness of a rapid HIV posttest counseling video. Sex Transm Dis. 2009;36:207–210. doi: 10.1097/OLQ.0b013e318191ba3f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haukoos JS, Hopkins E, Bender B, et al. Use of Kiosks and Patient Understanding of Opt-out and Opt-in Consent for Routine Rapid Human Immunodeficiency Virus Screening in the Emergency Department. Acad Emerg Med. 2012;19:287–293. doi: 10.1111/j.1553-2712.2012.01290.x. [DOI] [PubMed] [Google Scholar]
- 13.Kurth AE, Severynen A, Spielberg F. Addressing unmet need for HIV testing in emergency care settings: a role for computer-facilitated rapid HIV testing? AIDS Educ Prev. 2013;25:287–301. doi: 10.1521/aeap.2013.25.4.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gaydos CA, Solis M, Hsieh YH, et al. Use of tablet-based kiosks in the emergency department to guide patient HIV self-testing with a point-of-care oral fluid test. Int J STD AIDS. 2013;24:716–721. doi: 10.1177/0956462413487321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsieh YH, Gauvey-Kern M, Peterson S, et al. An emergency department registration kiosk can increase HIV screening in high risk patients. J Telemed Telecare. 2014;20:454–459. doi: 10.1177/1357633X14555637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Porter SC, Cai Z, Gribbons W, et al. The asthma kiosk: a patient-centered technology for collaborative decision support in the emergency department. J Am Med Inform Assoc. 2004;11:458–467. doi: 10.1197/jamia.M1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jones R. The role of health kiosks in 2009: literature and informant review. International journal of environmental research and public health. 2009;6:1818–1855. doi: 10.3390/ijerph6061818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cupertino AP, Richter K, Cox LS, et al. Feasibility of a Spanish/English computerized decision aid to facilitate smoking cessation efforts in underserved communities. J Health Care Poor Underserved. 2010;21:504–517. doi: 10.1353/hpu.0.0307. [DOI] [PubMed] [Google Scholar]
- 19.Holmes AS, Estabrooks PA, Davis GC, et al. Effect of a grocery store intervention on sales of nutritious foods to youth and their families. Journal of the Academy of Nutrition and Dietetics. 2012;112:897–901. doi: 10.1016/j.jand.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 20.Chan YY, Nagurka R, Bentley S, et al. Medical Utilization of Kiosks in the Delivery of Patient Education: A Systematic Review. Health promotion perspectives. 2014;4:1. doi: 10.5681/hpp.2014.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joshi A, Weng W, Lichenstein R, et al. Prospective tracking of a pediatric emergency department e-kiosk to deliver asthma education. Health Informatics J. 2009;15:282–295. doi: 10.1177/1460458209345899. [DOI] [PubMed] [Google Scholar]
- 22.Tony R, SARAH T, Dhinagaran D, et al. Design, Development and Implementation of a Touch-Screen Health Information Kiosk for Patients at the Outpatient Waiting Area in a Large Tertiary Care Hospital in India: An Evaluation of User Satisfaction. Journal of Health Informatics in Developing Countries. 2013:7. [Google Scholar]
- 23.Sun BC, Knapp H, Shamouelian A, et al. Effect of an education kiosk on patient knowledge about rapid HIV screening. J Telemed Telecare. 2010;16:158–161. doi: 10.1258/jtt.2009.090815. [DOI] [PubMed] [Google Scholar]
- 24.Trepka MJ, Newman FL, Huffman FG, et al. Food safety education using an interactive multimedia kiosk in a WIC setting: correlates of client satisfaction and practical issues. Journal of nutrition education and behavior. 2010;42:202–207. doi: 10.1016/j.jneb.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 25.Lawrence D. Cashing In On Check-In-As hospitals face steeper challenges in collecting for service, bringing the revenue cycle to kiosks is one answer. Healthcare Inf. 2010:18. [PubMed] [Google Scholar]