Highlights
-
•
Treating the central nervous system and psychosocial factors in chronic spinal pain.
-
•
This protocol combines pain neuroscience education and cognition targeted exercises.
-
•
This paper can be used as guidelines for implementation in clinical practice.
Keywords: Chronic spinal pain, Pain neuroscience education, Exercise therapy, Patient communication, Treatment protocol
Abstract
Background
Nonspecific chronic spinal pain is a common problem within the chronic pain population and is characterized by high social, economic and personal impact. To date, therapists are still struggling in adequately treating these types of patients, as seen in the small and short-term benefits of frequently applied primary care treatments. It is remarkable that despite the well-documented presence of abnormalities in central nociceptive processing in nonspecific chronic spinal pain patients, the implementation of this knowledge in clinical practice is still nearly non-existent.
Methods
This paper provides the treatment protocol used in a large randomized controlled trial that aimed to assess the effectiveness of a modern neuroscience approach compared to usual care evidence-based physiotherapy. This comprehensive pain neuroscience treatment program combines pain neuroscience education and cognition-targeted exercise therapy.
Conclusion
Based on previous small-scaled studies, this treatment protocol is expected to normalize central alterations by addressing central nervous system dysfunctions, psychological factors, as well as peripheral dysfunctions in a broader biopsychosocially-driven framework.
Introduction
Nonspecific chronic spinal pain (nCSP) accounts for a large proportion of the chronic pain population and includes, i.e. chronic low back pain, failed back surgery, chronic whiplash associated disorders, and chronic non-traumatic neck pain.1, 2 Besides its high prevalence (31% and 22% in women and men respectively in Belgium), nCSP is severely disabling and characterized by tremendous personal and socioeconomic impact, with long-term sick-leave, low quality of life and high socio-economic costs.3 No wonder that research on the most efficient and affordable strategies to deal with nCSP has been strongly advocated.4, 5, 6 To meet this need, a large randomized controlled trial investigating the effectiveness of such modern approach is currently ongoing. The protocol of this study is published7 and registered online (clinicaltrials.gov NCT02098005). However, these documents are focussed on the global study design without giving details on treatment aspects. Therefore, this paper aims at giving full transparency regarding the experimental treatment used in this study. This multicentre randomized controlled trial was approved by the local ethics committees of University Hospital Ghent (ID: 2013/1133) and University Hospital Brussels (ID: 2013/385).
Why using a modern neuroscience approach?
nCSP management should aim at achieving and maintaining a clinically important reduction in pain and disability, with optimal cost-effectiveness and minimal inconveniences. Yet, systematic reviews on the most frequently applied primary care treatments for nCSP (i.e. mobilization, manipulation, exercise therapy, back schools, NSAID's, TENS, etc.) report small, short-term benefits when compared to no, sham or other forms of treatment.4, 8, 9, 10, 11, 12 Physiotherapy in nCSP is often limited to a biomedical (i.e. neuromuscular training) or psychological model (i.e. graded exposure, graded activity, etc.), without accounting for the underlying pain mechanisms and the present understanding of modern pain neuroscience.13 These types of therapy are focused either on input mechanisms (treating peripheral elements like joints and muscles) or output mechanisms (motor control), while there is less attention for the well documented abnormalities in central nociceptive processing mechanisms 14, 15, 16, 17, 18, 19, 20, 21, 22.
These central nociceptive processing abnormalities include alterations in brain activity and morphology, hyperexcitability of the central nervous system and central sensitization.13, 22, 23, 24, 25, 26 This knowledge provides arguments for choosing a challenging new direction by developing novel clinical strategies targeting the brain and aiming at normalizing central alterations. This approach may increase the effect sizes and socioeconomic impact of treatment of nCSP.
Inspired by this state of the art, treatment should aim at addressing central nervous system dysfunctions,27, 28 psychosocial factors,13, 29 as well as peripheral dysfunctions in a broader biopsychosocially-driven framework. Although the problem in nCSP is not related to a dominant ‘input’ mechanism, there is still compelling evidence for impaired motor control.30, 31, 32, 33, 34, 35 Therefore, therapy should focus primarily at central nociceptive processing problems, in a balanced combination with targeting specific ‘output’ mechanisms given the maladaptive movement and activity strategies these patients display. This can be implemented in a modern neuroscience approach by using a comprehensive pain neuroscience treatment program comprising pain neuroscience education (PNE) followed by cognition-targeted exercise therapy.13 The randomized controlled trial investigating the effectiveness of this approach is currently ongoing.7 Here we provide the detailed experimental treatment protocol of this study.
The modern neuroscience approach
Step 1: Pain Neuroscience Education (PNE)
Both the practical application and positive clinical effects of PNE have been described extensively in nCSP and other chronic pain populations.36, 37, 38, 39, 40, 41, 42, 43, 44 PNE aims at reconceptualizing pain, by explaining that all pain is in the brain and that, rather than local tissue damage, hypersensitivity of the central nervous system may be the cause of the pain problem. PNE enables patients to understand the controversy surrounding their pain, including the lack of objective biomarkers or imaging findings.
Based on cost-effectiveness arguments,42 preference was given to the combination of a group, an online and an individual session completed with an informational leaflet to read at home, as an individual session of PNE is more effective for reducing pain and disability, but a group session is more cost-effective. General principles of PNE were explained in the group session, using examples and metaphors based on the individual experiences of the participating persons. Groups were kept small (i.e. 6 persons/group) in order to maintain an interactive and individualized approach. Between the group and individual session, the patient was asked to read an informational leaflet and to complete an online session. An example of the latter can be found at www.retrainpain.org in several languages. This online session45 covers the same information as the group session in order to facilitate deep learning and was adapted with different questions to assess the knowledge, perceptions and opinions of the patient regarding the PNE content. The information extracted from these questions was used to optimize and to individualize the third (individual) PNE session to increase its effectiveness. In addition to the educational sessions, the Neurophysiology of Pain test was used as part of the intervention to ascertain the quality of the education program by further discussing the patients’ misinterpretations upon completion of the questionnaire.46, 47
As such, PNE was used to reach therapeutic alliance between the patient and his/her therapist, which is a crucial milestone in the modern neuroscience approach of nCSP. PNE includes a transfer of knowledge, which enables applying the time-contingent approach that is a critical feature of the following step (cognition-targeted exercise training). An example of the communication preparing the patient for the exercise training can be found in Box 1. Implementing this next step is essential, as PNE as a sole treatment has rather small effect sizes.38 Once the patient has adopted new beliefs and cognitions, exercise therapy with special emphasis on cognitions and perceptions (including retraining pain memories) can be applied. The patient needs to understand that the applied exercises do not intend to address local neck or back problems, but aim at ‘retraining the brain’. Therefore, it is crucial not to initiate the exercise training before therapeutic alliance regarding the nature of the patient's (spinal) pain has been reached. More information on five requirements for effective PNE in physiotherapy practice can be found elsewhere.48 Briefly, these requirements include: (1) interaction with a therapist is necessary to obtain clinically meaningful effects on pain; (2) only patients dissatisfied with their current perceptions about pain are prone to reconceptualise pain; (3) a new explanation must be intelligible to the patient; (4) any new explanation must appear plausible and beneficial to the patient; and (5) the new explanation should be shared and confirmed by the direct environment of the patient.
Box 1. Communication regarding the transfer from theory (PNE) to practice (cognition-targeted exercises).
| Therapist (T): “We have been discussing and talking a lot regarding the underlying mechanisms of your pain problem. I know that you have got a lot of new information. How are you processing this? Do you feel like this new knowledge is applicable to your situation?” |
| Patient (P): “Well, as you indicate, it has been a great deal of new information, a lot of things I have never heard of, but it is all very recognizable and it gives me a little relieve. I am still a bit reticent, but I feel confident.” |
| T: “Do you now understand how pain, behavior, thoughts and emotions are related and how they all influence and maintain each other? Is it clear that avoiding certain painful or fearful movements will maintain the pain problem?” |
| P: “Yes, that is clear, but I do not see how we will change this?” |
| T: “Well, that is something we will do together during the next step of this therapy, in which we will initiate certain movements and activities. During these movements/activities we will no longer pay attention to the pain, this pain will no longer be of any value to you. Do you understand why?” |
| P: “Because the pain signal is not a reliable signal and not an accurate representation of what is effectively going on in my neck/back? |
| T: “Indeed! This means that when pain occurs while performing a certain exercise, you will not stop this exercise. You will complete the exact amount of repetitions we agreed on before starting the exercise. Do you feel confident about this approach?” |
| P: “I understand why I have to do this, but I am still a bit nervous about actually doing it.” |
| T: “That makes sense, that is why we will start with easily accessible exercises. I will guide you, perform the exercises together with you and all exercises will be applied in mutual agreement of both of us. |
Step 2: cognition-targeted exercise therapy
This step comprised two main phases: cognition-targeted motor control training and cognition-targeted dynamic and functional exercises. Both phases of this step were intertwined during treatment. Besides the willingness of the patient, there were no specific requirements to initiate a specific exercise or movement.
The main principles of “cognition-targeted” were applicable to all implemented exercises and were applied consistently.13 Detailed information can be found elsewhere,13, 49 but in general these principles include the following:
-
•
All exercises should be performed in a time-contingent (“Perform this exercise 10 times, regardless of the pain”) rather than in a symptom-contingent way (“Stop or adjust the exercise when it hurts”).
-
•
Goal setting is essentially done together with the patient, focussing on functionality instead of pain relief.
-
•
The treating physical therapist should continuously assess and challenge the patients’ cognitions and perceptions about the pain and the anticipated outcome of each exercise to change maladaptive cognitions and perceptions into positive ones. Specific instructions on required communication skills are described extensively elsewhere.49
-
•
Exercises should progress towards more feared movements and activities. Fears and maladaptive perceptions on negative consequences should be discussed thoroughly.
-
•
Progression to more feared exercises can be preceded by a phase of motor imagery, provided that the perceived fear is high enough (more information in Box 2).
Box 2. Patient information form on motor imagery.
MOTOR IMAGERY
-
a.What?
- Imagine the performance of a certain movement or activity in a very realistic and detailed way, without actually performing the movement or activity itself.
-
b.Why?
-
-Motor imagery can refine and facilitate actual movements. During motor imagery, the same brain areas are activated as during the performance of movements. This enables us to train the brain, without actually moving.
-
-This method is already used in paralyzed patients, to activate the paralyzed limbs again.
-
-This method is also used in (elite) sports to optimize movements and to increase the training effect.
-
-Motor imagery can reduce concerns regarding the actual movement or activity and can increase self-confidence.
-
-
-
c.How?
-
1.Sit down in a comfortable position that you can maintain easily.
-
2.Close your eyes and breath calmly.
-
3.Imaging the performance of a certain movement, while paying attention to the following:
-
•The duration of the motor imagery should be equal to performing the actual movement.
-
•Imagine the movement or activity in detail: including the environment, the preparation of the movement or activity, … The similarity between the motor imagery and the actual movement is essential!
-
•Imagine the movement or activity complete and accurately.
-
•Maintain high focus and concentration.
-
•
-
4.Keep the motor imagery session short to maintain high concentration.
-
1.
Phase a: cognition-targeted motor control training
This phase comprised sensorimotor control training based on the principles of Sahrmann,50 Comerford and Mottram,51 and Richardson and Jull52: these include targeting the deep cervical flexors and scapular muscles in patients with chronic neck pain, and balanced activation of the deep muscles surrounding the lumbopelvic region in patients with low back pain (e.g. multifidus, transversus abdominis, and pelvic floor muscles).
Crucial again was to use a cognition-targeted approach to comply with modern pain neuroscience. Therefore, communication regarding these exercises should be aligned with the content of the PNE. For example, the communication regarding the performance of an isolated muscle contraction of the multifidus or scapular setting is presented in Box 3.
Box 3. Communication regarding cognition-targeted motor control training.
| Therapist (T): “During this exercise you will perform a contraction (e.g. 10 s) of some specific muscles in the painful region. Do you have any idea why we are activating these specific muscles?” |
| Patient (P): “Maybe to strengthen these muscles so they will hurt less?” |
| T: “Remember all the things we discussed before. We then agreed on the fact that you have become more sensitive to signals coming from the neck/back than people without chronic neck/back pain. Remember that I have examined your neck/back before you started this program and that I did not find any important abnormalities in muscle strength or endurance. What does that tell you about this exercise now?” |
| P: “That it is not aiming at strengthening my muscles, but that it is targeting my pain system? But how does that work?” |
| T: “Indeed! When activating muscles, this will send signals to the brain. Normally these signals should be interpreted correctly, leading to the information that your muscles are working. Do you know why this leads to pain in your case?” |
| P: “Yes, because of the education I now understand that certain signals coming from my neck/back are interpreted as pain or danger, while they are just messages of movement.” |
| T: “Correctly, so when you are performing this exercise, muscles are being activated and sending signals to the brain. It is important that when you experience pain during this exercise, you are aware of this information and that you know that the pain is not a reliable signal.” |
Essential here, was the interpretation of painful signals and the theory behind the implementation of these motor control exercises. Many nCSP patients have the impression that the targeted muscles are “hurting”. Evidence indicates that these muscles display alterations in structure and/or function that may or may not be related to pain.31, 53, 54, 55, 56 However, the muscle ‘itself’ is only very rarely the actual cause of pain. Hence, these exercises were delivered with regard to the PNE content and the newly derived knowledge and perceptions. The patient was made aware that during the muscle contraction, the perceived pain is not related to the muscle itself, but rather a product of the brain and an enhanced central nociceptive processing.
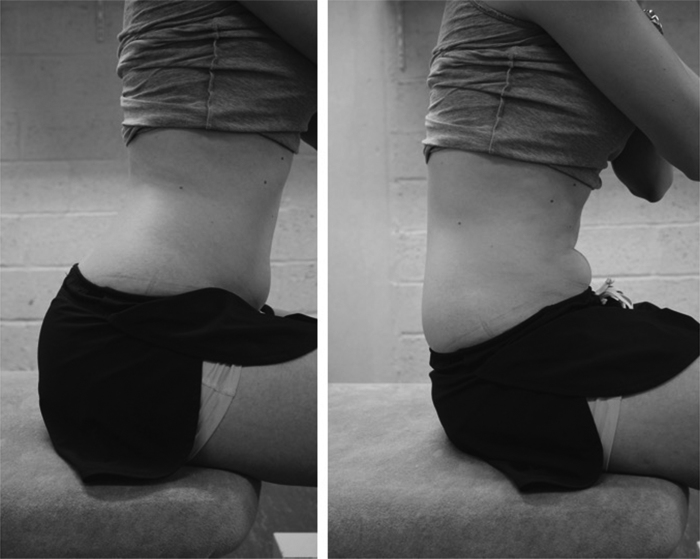
In addition, the exercise program also involved teaching the patient to start moving the neck/back region on a regular basis. This was done by standardized exercises, including the pelvic tilt for chronic low back pain patients (see Fig. 1) and shoulder shrugs (see Fig. 2) or gentle movement of the neck (see Fig. 3) in chronic neck pain patients. Patients were instructed to perform this exercise every 30 min during prolonged sitting or standing. Communication regarding this exercise was built upon the fact that endogenous analgesia is activated during movement, and that movement stimulates blood circulation (i.e. normal tissue physiology and metabolism). An example of this communication is presented in Box 4.
Figure 1.
Pelvic tilt. This exercise was used in chronic low back pain patients as standardized exercise to move the lower back every 30 min during prolonged sitting or standing.
Figure 2.
Shoulder shrugs. This exercise was used in chronic neck pain patients as standardized exercise to move the neck every 30 min during prolonged sitting or standing.
Figure 3.
Head swings. This exercise was used in chronic neck pain patients as standardized exercise to move the neck every 30 min during prolonged sitting or standing.
Box 4. Communication regarding regular movement.
| Therapist (T): “During prolonged sitting, your muscles are logically registering this and certain signals will be produced. We already discussed that this is giving you pain because of your hypersensitive pain system, while normally (in non-pain persons) this should give at most a certain inconvenience. Could you come up with an explanation why regular movement will help you in this situation?” |
| Patient (P): “Because regular movement will prevent these certain signals to be produced?” |
| T: “Indeed, that is one of the explanations! Besides this, there is also another very important mechanism that becomes active during movement. Do you remember the example I gave about the cyclists who reached the finish during a race even a broken collarbone?” |
| P: “Yes, I remember the story. I think it had something to do with what you called the ‘pharmacy’ in our body, which contains very strong analgesics.” |
| T: “Correct! Do you remember what can activate this pharmacy?” |
| P: “Physical activity.” |
| T: “Indeed, so does it sound logical that regular movement during prolonged sitting will also induce pain relieve by activating the pharmacy?” |
| P: “Yes, I guess it is worth a try.” |
Phase b: cognition-targeted dynamic and functional exercises
The purpose of this phase was to confront the patient with movements and activities that are feared, avoided and/or painful. Both in the physiotherapy sessions, during home exercises and in daily life it was crucial to avoid all ‘safety behaviour’ and to focus on normal and functional movements in a relaxed way (i.e. without consciously contracting specific muscles or maladaptive compensation strategies). Progression was targeted towards more complex and more feared movements and activities.
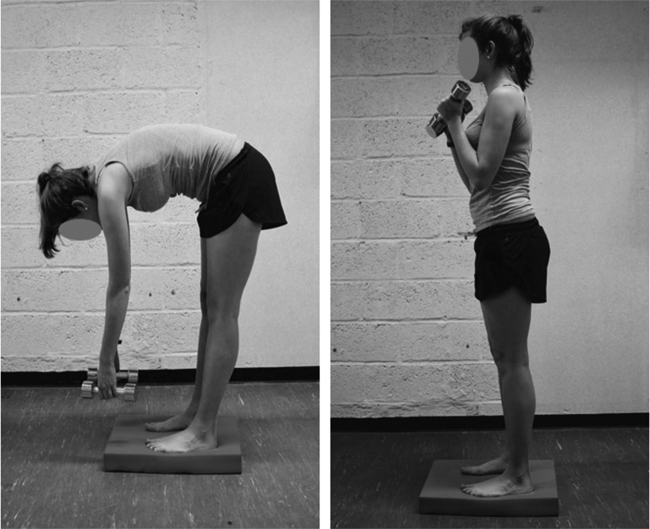
In order to detect fearful and/or painful movements and activities an ‘activity form’ was completed by the patient prior to PNE. This form asks the patient to list movements or activities of which the patient thinks they will worsen his/her complaints or disorder, and/or movements/activities that are limited due to their (spinal) pain. An example can be found in Table 1. This form enabled the therapist to detect movements or activities that needed to be addressed during therapy. In consultation with the patients, these movements and activities were sorted according to the amount of fear/pain they induce. The progression of these cognition-targeted exercises is illustrated in Box 5, using the example of bending forward in a chronic low back pain patient. The presented progression complies with what is generally seen in chronic low back pain patients. Logically, this progression was tailored to the individual patient, depending on his/her fearful movements. Other movements or activities in both chronic low back and neck pain were introduced following the same idea. Generally, the first exercises induced a similar movement as the finally intended activity, but without raising an association with the actual fearful/painful movement. Ideally, these first exercises induced some fear or stress in order to evoke a successful learning experience leading to increased confidence. For some examples of basic and advanced exercises, see Figure 4, Figure 5, Figure 6, Figure 7, Figure 8.
Table 1.
Example of an ‘activity form’ completed by a chronic low back pain patient.
| Write down movements/activities of which you think they will worsen your complaints or disorder, and/or that are limited due to your pain | Level of conviction 0-------------------------------10 |
|
|---|---|---|
| Unconvinced | Extremely convinced | |
| Vacuuming, mopping the floor, bending forward | 9 | |
| Bending forward and lifting something heavy | 10 | |
| Carrying groceries on one side | 8 | |
| Rotational movements of the back | 6 | |
| Prolonged sitting or standing | 6 | |
Box 5. Example of progression: Bending forward in chronic low back pain patients.
-
-
Flexion in supine position: moving the knees towards the chest
-
-
Flexion while being on hands and knees: moving the buttocks towards the heels
-
-Flexion while seated:
-
•Reaching forward on a table while bending the back
-
•Sustained flexion of the back while reaching left/right
-
•
-
-Flexion while standing:
-
•Flexion of the back and returning to an upright position supported by one hand on a table
-
•Flexion of the back without support
-
•Sustained flexion of the back, while performing a rotation or side bending
-
•Flexion of the back and returning to an upright position combined with rotation
-
•
-
-General principles for progression in each exercise:
-
•Using increasing weights
-
•Increasing the load arm of the used weights
-
•Increasing the speed of exercises
-
•Combining movements (e.g. flexion + rotation)
-
•Progressing to an unstable base
-
•Change in context/environment to increase threating value
-
•
Figure 4.

Example of a basic exercise for chronic neck pain patients: neck extension. Specific exercises should be individually-tailored and depending on the fearful movements of the patient. Communication to change inappropriate cognitions and expectations regarding the exercises is as important as providing individualized therapy.
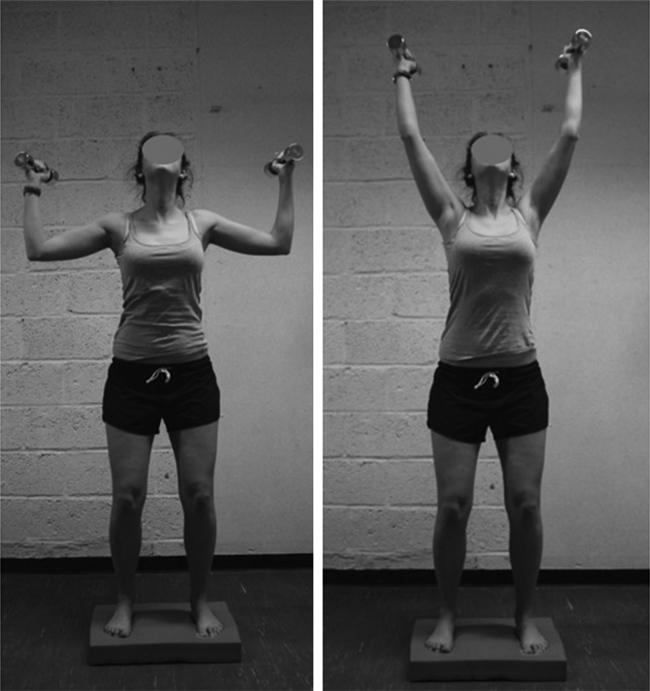
Figure 5.
Example of an advanced exercise for chronic neck pain patients: unstable base, patient keeps his/her head in extension while performing an arm exercise with weights. Exercises should be individually-tailored and progressing towards fearful movements. Communication to change inappropriate cognitions and expectations regarding the exercises is as important as providing individualized therapy.
Figure 6.

Example of a basic exercise for chronic low back pain patients: exercises that induce some flexion of the back, without raising an association with the actual fearful/painful movement (e.g. bending forward). Communication to change inappropriate cognitions and expectations regarding the exercises is as important as actually performing the exercise.
Figure 7.

Example of a basic exercise for chronic low back pain patients: exercises that induce some flexion of the back, without raising an association with the actual fearful/painful movement (e.g. bending forward). Communication to change inappropriate cognitions and expectations regarding the exercises is as important as actually performing the exercise.
Figure 8.
Example of an advanced exercise for chronic low back pain patients: unstable base, patient performs a flexion and extension of the back with weights without ‘safety behaviour’. Exercises should be individually-tailored and progressing towards fearful movements. Communication to change inappropriate cognitions and expectations regarding the exercises is as important as providing individualized therapy.
Again, it should be acknowledged that communication on cognitions, perceptions and expectations was an essential component of cognition-targeted exercises as described above. The exercises were not used to target local aspects of the neck/back, but were rather behavioural experiments targeting the brain. Specific examples of cognition-targeted communication during exercises between the physiotherapist and a chronic pain patient are extensively described elsewhere.49
Exercise program at home
Several exercises, movements and activities used in the exercise program were also practiced at home. However, some general principles were applied:
-
•
The content, frequency and amount of home exercises should always be decided in consultation with the patient.
-
•
Home-exercises should also be applied using a time-contingent approach.
-
•
Home exercises should be implemented in a functional way (e.g. bending forward while unloading the dishwasher).
-
•
Exercises should only be performed at home when the patient is confident and secure to perform the exercise alone.
-
•
Communication for home exercises is equal important as communication during the exercises in therapy (see Box 6).
Box 6. Communication regarding home exercises.
| Therapist (T): “You have been practicing this exercise very well here in therapy. How do you feel about trying it also at home?” |
| Patient (P): “I feel confident.” |
| T: “Great! Here you performed 10 repetitions; I propose to do the same at home. Are you ok with that?” |
| P: “Yes.” |
| T: “Perfect. Imagine, you are at home, doing this exercise and during the 6threpetition, you suddenly feel a pang in the neck/back. What will you do?” |
| P: “I stop the exercise and try it again later?” |
| T: “Everything depends on the value and explanation you give to this pang. When it occurs, does it mean that something is wrong in your neck/back?” |
| P: “Right, the pain I feel in my neck/back is an unreliable signal and I should continue performing the exercise.” |
| T: “Indeed, and do not forget that you have been performing the exercise excellent during the therapy here, this should give you a lot of confidence to perform it at home.” |
Conflicts of interest
JN has co-authored a Dutch book for clinicians on pain neuroscience education, but the royalties for that book are collected by the Vrije Universiteit Brussel and not him personally. Besides that, the authors have no conflict of interest to disclose.
Footnotes
Clinicaltrials.gov NCT02098005.
References
- 1.InSites Consulting . 2010. Pain Proposal Patient Survey. [Google Scholar]
- 2.https://kce.fgov.be/sites/default/files/page_documents/d20061027363.pdf
- 3.https://www.wiv-isp.be/epidemio/epinl/CROSPNL/HISNL/his08nl/belangrijkste20%resultaten_NL.pdf
- 4.Keller A., Hayden J., Bombardier C., van Tulder M. Effect sizes of non-surgical treatments of non-specific low-back pain. Eur spine J. 2007;16(11):1776–1788. doi: 10.1007/s00586-007-0379-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murray C.J.L., Vos T., Lozano R. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 6.Mokdad A.H., Jaber S., Aziz M.I.A. The state of health in the Arab world, 1990–2010: an analysis of the burden of diseases, injuries, and risk factors. Lancet. 2014;383(9914):309–320. doi: 10.1016/S0140-6736(13)62189-3. [DOI] [PubMed] [Google Scholar]
- 7.Dolphens M., Nijs J., Cagnie B. Efficacy of a modern neuroscience approach versus usual care evidence-based physiotherapy on pain, disability and brain characteristics in chronic spinal pain patients: protocol of a randomized clinical trial. BMC Musculoskelet Disord. 2014;15:149. doi: 10.1186/1471-2474-15-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Tulder M.W., Koes B., Malmivaara A. Outcome of non-invasive treatment modalities on back pain: an evidence-based review. Eur spine J. 2006;15:S64–S81. doi: 10.1007/s00586-005-1048-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Machado L.A.C., Kamper S.J., Herbert R.D., Maher C.G., McAuley J.H. Analgesic effects of treatments for non-specific low back pain: a meta-analysis of placebo-controlled randomized trials. Rheumatology. 2009;48(5):520–527. doi: 10.1093/rheumatology/ken470. [DOI] [PubMed] [Google Scholar]
- 10.Artus M., van der Windt D.A., Jordan K.P., Hay E.M. Low back pain symptoms show a similar pattern of improvement following a wide range of primary care treatments: a systematic review of randomized clinical trials. Rheumatology. 2010;49(12):2346–2356. doi: 10.1093/rheumatology/keq245. [DOI] [PubMed] [Google Scholar]
- 11.van Middelkoop M., Rubinstein S.M., Kuijpers T. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. Eur spine J. 2011;20(1):19–39. doi: 10.1007/s00586-010-1518-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schroeder J., Kaplan L., Fischer D.J., Skelly A.C. The outcomes of manipulation or mobilization therapy compared with physical therapy or exercise for neck pain: a systematic review. Evid Based Spine Care J. 2013;4(1):30–41. doi: 10.1055/s-0033-1341605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nijs J., Meeus M., Cagnie B. A modern neuroscience approach to chronic spinal pain: combining pain neuroscience education with cognition-targeted motor control training. Phys Ther. 2014;94(5):730–738. doi: 10.2522/ptj.20130258. [DOI] [PubMed] [Google Scholar]
- 14.Seminowicz D.A., Wideman T.H., Naso L. Effective treatment of chronic low back pain in humans reverses abnormal brain anatomy and function. J Neurosci. 2011;31(20):7540–7550. doi: 10.1523/JNEUROSCI.5280-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Apkarian A.V., Sosa Y., Sonty S. Chronic back pain is associated with decreased prefrontal and thalamic gray matter density. J Neurosci. 2004;24(46):10410–10415. doi: 10.1523/JNEUROSCI.2541-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Buckalew N., Haut M.W., Morrow L., Weiner D. Chronic pain is associated with brain volume loss in older adults: preliminary evidence. Pain Med. 2008;9(2):240–248. doi: 10.1111/j.1526-4637.2008.00412.x. [DOI] [PubMed] [Google Scholar]
- 17.Ung H., Brown J.E., Johnson K.A., Younger J., Hush J., Mackey S. Multivariate classification of structural MRI data detects chronic low back pain. Cereb Cortex. 2014;24(4):1037–1044. doi: 10.1093/cercor/bhs378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Giesecke T., Gracely R.H., Grant M.A.B. Evidence of augmented central pain processing in idiopathic chronic low back pain. Arthritis Rheum. 2004;50(2):613–623. doi: 10.1002/art.20063. [DOI] [PubMed] [Google Scholar]
- 19.Schmidt-Wilcke T., Leinisch E., Ganssbauer S. Affective components and intensity of pain correlate with structural differences in gray matter in chronic back pain patients. Pain. 2006;125(1–2):89–97. doi: 10.1016/j.pain.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 20.Wood P.B. Variations in brain gray matter associated with chronic pain. Curr Rheumatol Rep. 2010;12(6):462–469. doi: 10.1007/s11926-010-0129-7. [DOI] [PubMed] [Google Scholar]
- 21.Siddall P.J., Stanwell P., Woodhouse A. Magnetic resonance spectroscopy detects biochemical changes in the brain associated with chronic low back pain: a preliminary report. Anesth Analg. 2006;102(4):1164–1168. doi: 10.1213/01.ane.0000198333.22687.a6. [DOI] [PubMed] [Google Scholar]
- 22.Roussel N.A., Nijs J., Meeus M., Mylius V., Fayt C., Oostendorp R. Central sensitization and altered central pain processing in chronic low back pain: fact or myth? Clin J Pain. 2013;29(7):625–638. doi: 10.1097/AJP.0b013e31826f9a71. [DOI] [PubMed] [Google Scholar]
- 23.Wand B.M., O’Connell N.E. Chronic non-specific low back pain – sub-groups or a single mechanism? BMC Musculoskelet Disord. 2008;9:11. doi: 10.1186/1471-2474-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nijs J., Daenen L., Cras P., Struyf F., Roussel N., Oostendorp R.A.B. Nociception affects motor output: a review on sensory-motor interaction with focus on clinical implications. Clin J Pain. 2012;28(2):175–181. doi: 10.1097/AJP.0b013e318225daf3. [DOI] [PubMed] [Google Scholar]
- 25.Mansour A.R., Baliki M.N., Huang L. Brain white matter structural properties predict transition to chronic pain. Pain. 2013;154(10):2160–2168. doi: 10.1016/j.pain.2013.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buckalew N., Haut M.W., Aizenstein H. White matter hyperintensity burden and disability in older adults: is chronic pain a contributor? PM R. 2013;5(6):471–480. doi: 10.1016/j.pmrj.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nijs J., Kosek E., Van Oosterwijck J., Meeus M. Dysfunctional endogenous analgesia during exercise in patients with chronic pain: to exercise or not to exercise? Pain Physician. 2012;15:ES205–ES213. [PubMed] [Google Scholar]
- 28.Van Oosterwijck J., Nijs J., Meeus M., Paul L. Evidence for central sensitization in chronic whiplash: a systematic literature review. Eur J Pain. 2013;17(3):299–312. doi: 10.1002/j.1532-2149.2012.00193.x. [DOI] [PubMed] [Google Scholar]
- 29.Nicholls E.E., Hill S., Foster N.E. Musculoskeletal pain illness perceptions: factor structure of the Illness Perceptions Questionnaire-Revised. Psychol Health. 2013;28(1):84–102. doi: 10.1080/08870446.2012.714782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tsao H., Danneels L.A., Hodges P.W. ISSLS prize winner: smudging the motor brain in young adults with recurrent low back pain. Spine. 2011;36(21):1721–1727. doi: 10.1097/BRS.0b013e31821c4267. [DOI] [PubMed] [Google Scholar]
- 31.D’hooge R., Hodges P., Tsao H., Hall L., Macdonald D., Danneels L. Altered trunk muscle coordination during rapid trunk flexion in people in remission of recurrent low back pain. J Electromyogr Kinesiol. 2013;23(1):173–181. doi: 10.1016/j.jelekin.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 32.Hodges P.W. The role of the motor system in spinal pain: implications for rehabilitation of the athlete following lower back pain. J Sci Med Sport. 2000;3(3):243–253. doi: 10.1016/s1440-2440(00)80033-x. [DOI] [PubMed] [Google Scholar]
- 33.Cagnie B., Dirks R., Schouten M., Parlevliet T., Cambier D., Danneels L. Functional reorganization of cervical flexor activity because of induced muscle pain evaluated by muscle functional magnetic resonance imaging. Man Ther. 2011;16(5):470–475. doi: 10.1016/j.math.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 34.Roussel N., De Kooning M., Schutt A. Motor control and low back pain in dancers. Int J Sports Med. 2013;34(2):138–143. doi: 10.1055/s-0032-1321722. [DOI] [PubMed] [Google Scholar]
- 35.Roussel N., Nijs J., Truijen S., Vervecken L., Mottram S., Stassijns G. Altered breathing patterns during lumbopelvic motor control tests in chronic low back pain: a case–control study. Eur spine J Off Publ Eur Spine Soc. 2009;18(7):1066–1073. doi: 10.1007/s00586-009-1020-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Van Oosterwijck J., Meeus M., Paul L. Pain physiology education improves health status and endogenous pain inhibition in fibromyalgia: a double-blind randomized controlled trial. Clin J Pain. 2013;29(10):873–882. doi: 10.1097/AJP.0b013e31827c7a7d. [DOI] [PubMed] [Google Scholar]
- 37.Van Oosterwijck J., Nijs J., Meeus M. Pain neurophysiology education improves cognitions, pain thresholds, and movement performance in people with chronic whiplash: a pilot study. J Rehabil Res Dev. 2011;48(1):43–58. doi: 10.1682/jrrd.2009.12.0206. [DOI] [PubMed] [Google Scholar]
- 38.Nijs J., Paul van Wilgen C., Van Oosterwijck J., van Ittersum M., Meeus M. How to explain central sensitization to patients with “unexplained” chronic musculoskeletal pain: practice guidelines. Man Ther. 2011;16(5):413–418. doi: 10.1016/j.math.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 39.Meeus M., Nijs J., Van Oosterwijck J., Van Alsenoy V., Truijen S. Pain physiology education improves pain beliefs in patients with chronic fatigue syndrome compared with pacing and self-management education: a double-blind randomized controlled trial. Arch Phys Med Rehabil. 2010;91(8):1153–1159. doi: 10.1016/j.apmr.2010.04.020. [DOI] [PubMed] [Google Scholar]
- 40.van Wilgen C.P., Nijs J. Bohn Stafleu van Loghum; Houten: 2010. Pijneducatie – een praktische handleiding voor (para)medici. [Google Scholar]
- 41.Butler D.S., Moseley G.L. NOI Group Publishing; Adelaide: 2003. Explain Pain. [Google Scholar]
- 42.Moseley G.L. Joining forces – combining cognition-targeted motor control training with group or individual pain physiology education: a successful treatment for chronic low back pain. J Man Manip Ther. 2003;11(2):88–94. [Google Scholar]
- 43.Moseley L. Combined physiotherapy and education is efficacious for chronic low back pain. Aust J Physiother. 2002;48(4):297–302. doi: 10.1016/s0004-9514(14)60169-0. [DOI] [PubMed] [Google Scholar]
- 44.Meeus M., Nijs J., Hamers V., Ickmans K., van Oosterwijck J. The efficacy of patient education in whiplash associated disorders: a systematic review. Pain Physician. 2012;15(5):351–361. [PubMed] [Google Scholar]
- 45.Retrain Pain Foundation. Online Pain Course [Internet]. Available from: http://www.retrainpain.org.
- 46.Meeus M., Nijs J., Elsemans K.S., Truijen S., De Meirleir K. Development and properties of the Dutch neurophysiology of pain test in patients with chronic fatigue syndrome. J Musculoskelet Pain. 2010;18(1):58–65. [Google Scholar]
- 47.Catley M.J., O’Connell N.E., Moseley G.L. How good is the neurophysiology of pain questionnaire? A Rasch analysis of psychometric properties. J Pain. 2013;14(8):818–827. doi: 10.1016/j.jpain.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 48.Nijs J., Meeus M. 2015. Five Requirements for Effective Pain Neuroscience Education in Physiotherapy Practice. (nuzzel.com) [Google Scholar]
- 49.Nijs J., Lluch Girbes E., Lundberg M., Malfliet A., Sterling M. Exercise therapy for chronic musculoskeletal pain: innovation by altering pain memories. Man Ther. 2015;20(1):216–220. doi: 10.1016/j.math.2014.07.004. [DOI] [PubMed] [Google Scholar]
- 50.Sahrmann S.A. Does postural assessment contribute to patient care? J orthop Sports Phys Ther. 2002;32:376–379. doi: 10.2519/jospt.2002.32.8.376. [DOI] [PubMed] [Google Scholar]
- 51.Comerford M.J., Mottram S.L. Functional stability re-training: principles and strategies for managing mechanical dysfunction. Man Ther. 2001;6(1):3–14. doi: 10.1054/math.2000.0389. [DOI] [PubMed] [Google Scholar]
- 52.Richardson C.A., Jull G.A. Muscle control-pain control. What exercises would you prescribe? Man Ther. 1995;1(1):2–10. doi: 10.1054/math.1995.0243. [DOI] [PubMed] [Google Scholar]
- 53.D’hooge R., Cagnie B., Crombez G., Vanderstraeten G., Dolphens M., Danneels L. Increased intramuscular fatty infiltration without differences in lumbar muscle cross-sectional area during remission of unilateral recurrent low back pain. Man Ther. 2012;17(6):584–588. doi: 10.1016/j.math.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 54.D’hooge R., Cagnie B., Crombez G., Vanderstraeten G., Achten E., Danneels L. Lumbar muscle dysfunction during remission of unilateral recurrent nonspecific low-back pain: evaluation with muscle functional MRI. Clin J Pain. 2013;29(3):187–194. doi: 10.1097/AJP.0b013e31824ed170. [DOI] [PubMed] [Google Scholar]
- 55.O’Leary S., Cagnie B., Reeve A., Jull G., Elliott J.M. Is there altered activity of the extensor muscles in chronic mechanical neck pain? A functional magnetic resonance imaging study. Arch Phys Med Rehabil. 2011;92(6):929–934. doi: 10.1016/j.apmr.2010.12.021. [DOI] [PubMed] [Google Scholar]
- 56.Falla D., O’Leary S., Farina D., Jull G. The change in deep cervical flexor activity after training is associated with the degree of pain reduction in patients with chronic neck pain. Clin J Pain. 2012;28(7):628–634. doi: 10.1097/AJP.0b013e31823e9378. [DOI] [PubMed] [Google Scholar]