Abstract
Chronic hyperglycaemia of Type 2 diabetes mellitus causes long term damage to heart resulting in coronary artery disease (CAD), myocardial infarction (MI), congestive heart failure (CHF), and sudden death from arrhythmias. AIMS: To study the prevalence of different types of arrhythmias in T2DM, particularly in association with Cardiac Autonomic Neuropathy (CAN). METHODS: A cross-sectional study including 100 patients of Type 2 Diabetes Mellitus (T2DM) presenting with cardiac arrhythmias, was done at our hospital over 2 years. Detailed history along with physical examination and tests for CAN were done. Routine investigations along with echocardiography, stress test, Holter monitoring were done. RESULTS: Sinus Tachycardia (ST) was the commonest arrhythmia, found in 32% of patients. 20% had Complete Heart Block (CHB), 15% had Sinus Bradycardia (SB), and 15% had Atrial Fibrillation (AF). Ventricular Premature Complex (VPC) was found in 10% and 3% had Atrial Premature Complex (APC). 3% had first degree AV block, whereas 1% had Paroxysmal Supra Ventricular Tachycardia (PSVT), and another 1% had Ventricular Tachycardia (VT). Poorly controlled diabetes and co-morbidities was associated with higher incidence of arrhythmias. 62% of patients had prolonged QTc, majority of which had CAN. Most of the patients responded to standard therapy.
Keywords: Arrythmias, type 2 diabetes mellitus, cardiac autonomic neuropathy, QTc interval
INTRODUCTION
Chronic hyperglycemia of type 2 diabetes mellitus (T2DM) causes long-term damage to the heart resulting in coronary artery disease (CAD), myocardial infarction (MI), congestive heart failure (CHF), and sudden death from arrhythmias. Previous studies have shown that ventricular arrhythmias are frequent in T2DM.[1] Hypoglycemia associated with intensive glycemic control and cardiac autonomic neuropathy (CAN) associated with diabetes are associated with heart rate variability and changes in ventricular repolarization.[1,2] Increase in QT interval–heart rate relationship is used for the diagnosis of CAN. Corrected QT interval (QTc) prolongation, increased QT dispersion (QTd), and increased HbA1c are associated with increased mortality, especially in elderly type 2 diabetics.
Aims
To study the prevalence of different types of arrhythmias in T2DM, particularly in association with CAN.
METHODS
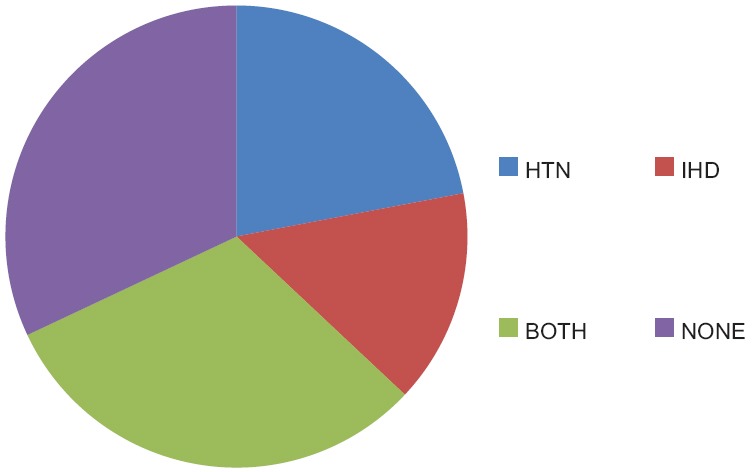
A cross-sectional study was conducted at our hospital over 2 years, which included 100 patients of T2DM presenting with cardiac arrhythmias (clinically or on electrocardiogram [ECG]). Written informed consent was obtained prior to enrollment. Detailed history along with physical examination was done. Wherever permissible, depending on the patient's clinical state, tests for CAN were done. In the scenario of severe hypertension (HTN), these tests were done once the blood pressure was controlled. In patients with acute MI, tests for CAN [Table 1] were done after 1 week and the tests involving Valsalva maneuver were not done.
Table 1.
Tests for cardiac autonomic neuropathy
Besides routine investigations such as blood sugar levels, HbA1c levels, urine examination, serum electrolytes, ECG with rhythm strip and calculation of QTc interval, QTd, Tp-e interval, Tp-e/QT ratio, Tp-e/QTc ratio were done. Two-dimensional echocardiography, stress test, Holter monitoring, thyroid function tests, serum magnesium, and cardiac enzyme tests were done as indicated.
The data were compiled and analyzed using Statistical Package for Social Sciences (SPSS version 16) software.
-
Inclusion criteria
- Patients suffering from T2DM and having arrhythmias clinically or on ECG during presentation or stay at hospital were enrolled in the study.
-
Exclusion criteria
- Patients suffering from T2DM with normal sinus rhythm and no arrhythmia on ECG were excluded from the study.
RESULTS
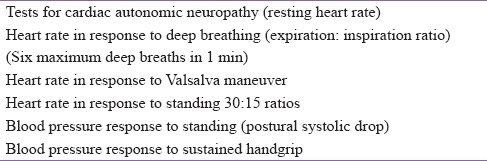
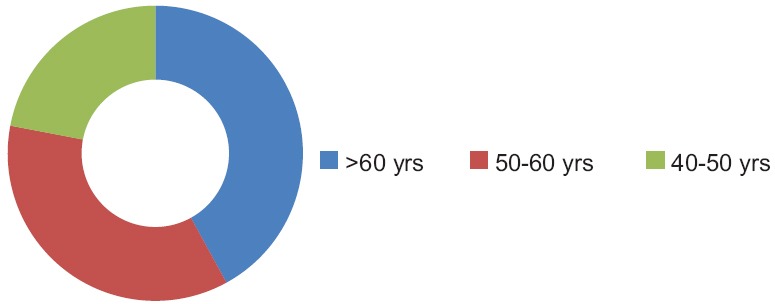
One hundred (60 males and 40 females) patients having T2DM with arrhythmias were studied. Sinus tachycardia (ST) was the most common arrhythmia, found in 32% of patients (20 males and 12 females). Around 20% (15 males and 5 females) of the patients had complete heart block (CHB), 15% (5 males and 10 females) had sinus bradycardia (SB), and 15% (8 males and 7 females) had atrial fibrillation (AF). Ventricular premature complex (VPC) was found in 10% (7 males and 3 females) and 3% (2 males and 1 female) had atrial premature complex (APC). Nearly 3% (2 males and 1 female) had first-degree atrioventricular (AV) block, whereas 1% (female) had paroxysmal supraventricular tachycardia (PSVT), and another 1% (male) had ventricular tachycardia (VT) [Figure 1].
Figure 1.
Frequency of different types of arrythmias
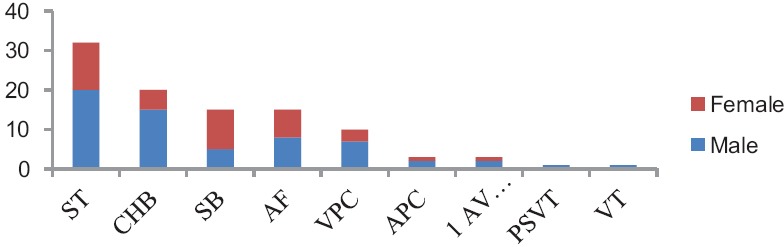
HbA1c levels were used to classify the glycemic control of patients into good (7%–8.5%), average (8.5%–9.5%), and poor (above 9.5%). About 55 patients showed poor glycemic control, 32 had average control, and 13 patients had good glycemic control. Among patients with poor glycemic control, 16 had ST, 12 had CHB, 5 had SB, 10 had AF, and 7 had VPC. Two patients had first-degree AV block and one had APC. The single case each of PSVT and VT occurred in patients with poor glycemic control [Figure 2].
Figure 2.
Distribution of different arrhythmias according to HBA1c level
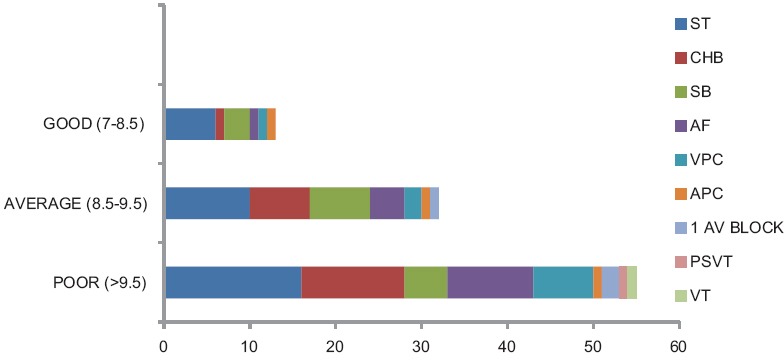
Out of the 100 patients, 22 had HTN, 15 had ischemic heart disease (IHD), 31 had both HTN and IHD, and 32 had no comorbidities. Patients with HTN and/or IHD were associated with higher incidence of arrhythmias, particularly AF and VPCs [Figure 3].
Figure 3.
Co-morbidities in the study sample
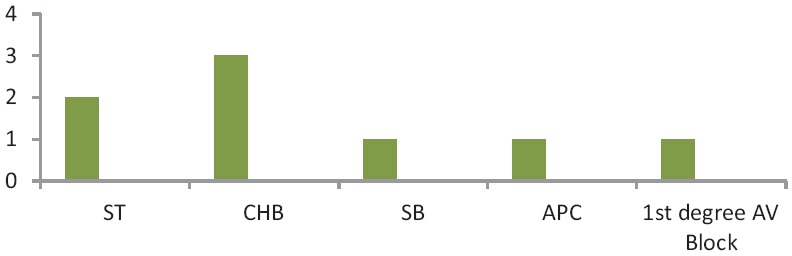
Among the 100 patients, 42 were more than 60 years of age, 36 were between 50 and 60 years of age, and 22 were between 40 and 50 years of age. Increasing age was associated with higher incidence of arrhythmias, particularly AF and CHB [Figure 4].
Figure 4.
Age distribution of study sample
Almost 62% patients in our study had prolonged QTc, out of which 36% were males and 26% were females. The remaining 38% of patients had normal QTc. About seventy patients could be tested for CAN. A total of 64 patients had CAN. Fifty-six patients had CAN with prolonged QTc, while 8 had CAN despite normal QTc. Among the 56 patients with prolonged QTc and CAN, 28 had ST, 12 had CHB, 5 had SB, 6 had VPCs, 2 had first-degree AV block, 1 had APC, 1 had PSVT, and 1 had VT [Figure 5]. Out of the eight patients with normal QTc and CAN, two had ST, three had CHB, one had SB, one had APC, and one had first-degree AV block [Figure 6].
Figure 5.
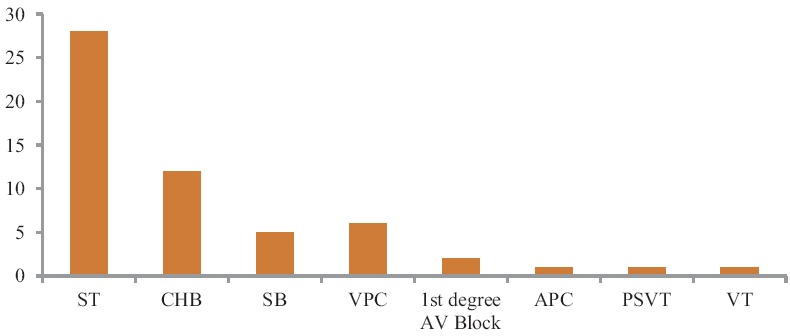
Patients with prolonged QTc and cardiac autonomic neuropathy
Figure 6.
Patients with normal QTc and cardiac autonomic neuropathy
Patients with prolonged corrected QT interval and cardiac autonomic neuropathy
Patients with normal corrected QT interval and cardiac autonomic neuropathy
Nearly 76% of patients in our study had increased QTd, which correlated better with the presence of arrhythmias than the QTc interval. The peak and the end of the T-wave (Tp-e) interval and associated Tp-e/QT ratio are promising measures of ventricular repolarization indicating transmural dispersion of repolarization. Tp-e interval, Tp-e/QT ratio, and Tp-e/QTc ratio were prolonged in 73% of our patients. Patients with prolonged Tp-e interval and ratios had much higher incidence of arrhythmias as compared to patients with normal Tp-e interval and ratios.
Around 20%–30% of our patients experienced one or more episodes of hypoglycemia during the study period of 2 years, and the development of hypoglycemia was associated with prolonged QTc interval as well as increase in QTd and arrhythmias.
A total of 22 patients in the study were found to have hyperkalemia associated with diabetic kidney disease, among which 10 had CHB. Some of these patients with hyperkalemia and CHB also had CAN.
Hypomagnesemia was present in only eight patients (five males and three females) and was normal in the rest. One of these had an acute MI, while the rest had only ST.
Hypothyroidism was detected only in ten patients (two males and eight females), while the rest had normal thyroid function. Six patients with hypothyroidism had bradyarrhythmias (three CHB and three SB).
All our patients with CHB, AF, PSVT, and VT were treated using standard treatment strategies, tailored according to the presence or absence of acute coronary syndromes. Pacemaker implantation was effective in all cases of CHB. Most of the patients responded favorably to treatment, but eight patients died during the study period of 2 years.
DISCUSSION
Nowadays, complications of T2DM such as infection or dyselectrolytemia rarely result in death. Death occurs mainly due to long-term micro- and macro-vascular complications of diabetes, particularly CAD.[3] The Framingham Heart Study and the OASIS registry have shown the association of diabetes with increased all-case death, new MI, stroke, heart failure, and arrhythmias.[4]
Low heart rate variability and reduced sinus arrhythmia indicate diabetic CAN, which is a definite risk factor for arrhythmias and sudden cardiac death in T2DM patients, as seen in this study.[5]
Sympathetic overactivity is directly correlated to the degree of insulin resistance, which is associated with major cardiovascular accidents and arrhythmias.[6]
Measures of ventricular repolarization such as QTc and QTd are significant predictors of the risk of arrhythmias and poor prognosis in T2DM patients.[1] In our study, 62% of patients had prolonged QTc and 76% had increased QTd, which was associated with CAN and significantly higher incidence of arrhythmias in our patients. New measures of ventricular repolarization such as Tp-e interval and Tp-e/QTc ratio were also prolonged in 73% of our patients, indicating cardiac electrical inhomogeneity, which may well be one of the leading causes of increased incidence of arrhythmias in patients with T2DM. T2DM thereby leads to augmentation of transmural dispersion of repolarization suggesting increased risk for malignant ventricular arrhythmias.[7]
In our study, ten patients with poor glycemic control and four patients with average glycemic control had AF, indicating that poor glycemic control and longer duration of diabetes is an independent risk factor for AF, independent of CAD or CHF.
As evidenced by the higher incidence of ventricular arrhythmias in our patients with poor glycemic control (seven patients had VPCs and one had VT), T2DM is associated with higher prevalence of ventricular arrhythmias independent of CAD or CHF.
Around 20%–30% of patients in our study developed hypoglycemia, which was associated with QTc prolongation and arrhythmias, reflecting that hypoglycemia in T2DM also leads to significant changes in cardiac repolarization and arrhythmias.
A total of 22 patients in our study had hyperkalemia, among which 10 developed CHB, reflecting the increased incidence of CHB in diabetic patients who develop chronic kidney disease and hyperkalemia.
Movahed and Hashemzadeh in their study showed that AF occurred in 14.9% of T2DM patients compared to 10.3% in the control group. They also showed that CHB was present in 1.1% of T2DM patients compared to 0.6% in non-T2DM patients.[1]
Rustom et al. also showed that the prevalence of AF was higher in patients with DM and HTN compared to HTN alone. These studies were in concordance with our study showing higher prevalence of AF in T2DM.
Hasslacher and Wahl et al. also showed higher incidence of first-degree AV block and CHB in T2DM patients.
In our study also, CHB was strongly associated with T2DM and was the second most common arrhythmia.
Mathur et al. in their study showed that diabetics with CAN had significant QTc prolongation compared to diabetics without CAN and controls.
CONCLUSIONS
T2DM is associated with a significant increase in the risk for arrhythmias and sudden cardiac death, as demonstrated in our study. Each case of arrhythmia in T2DM warrants further evaluation. CAN is the most important predictor for the development of arrhythmias in T2DM. QTc, QTd, Tp-e interval, and Tp-e/QTc ratio along with reduced sinus arrhythmia are simple, yet invaluable tools to arouse the suspicion of CAN. Comorbidities, poor glycemic control, prolonged QTc, and hyperkalemia are associated with worse prognosis.
Limitations
The sample was too small to generalize the results of the study and prognosis could not be ascertained as the study was cross-sectional in nature. Additional imaging investigations for cardiac perfusion would have added value for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Movahed MR, Hashemzadeh M. Strong independent association between type 2 diabetes mellitus and third degree AV-block. doi: 10.1016/j.diabres.2023.110948. [DOI] [PubMed] [Google Scholar]
- 2.Krishna K, Jha Y, Tuteja A, Adukia S, Dharamsi S, Chauhan R. Probing into arrhythmias in type 2 diabetics. Indian J Appl Res. 2015;5:781–3. [Google Scholar]
- 3.Fairfax AJ, Leatham A. Idiopathic heart block: Association with vitiligo, thyroid disease, pernicious anaemia, and diabetes mellitus. Br Med J. 1975;4:322–4. doi: 10.1136/bmj.4.5992.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Powers AC. Diabetes mellitus: Complications. In: Kasper DL, Fauci AS, Hauser SL, Longo DL, Jameson JL, Loscalzo J, editors. 19th ed. Vol. 2. USA: McGraw Hill; 2015. pp. 2422–30. [Google Scholar]
- 5.Kataoka M, Ito C, Sasaki H, Yamane K, Kohno N. Low heart rate variability is a risk factor for sudden cardiac death in type 2 diabetes. Diabetes Res Clin Pract. 2004;64:51–8. doi: 10.1016/j.diabres.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 6.Perciaccante A, Fiorentini A, Paris A, Serra P, Tubani L. Circadian rhythm of the autonomic nervous system in insulin resistant subjects with normoglycemia, impaired fasting glycemia, impaired glucose tolerance, type 2 diabetes mellitus. BMC Cardiovasc Disord. 2006;6:19. doi: 10.1186/1471-2261-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Movahed MR, Hashemzadeh M, Jamal M. Increased prevalence of ventricular fibrillation in patients with type 2 diabetes mellitus. Heart Vessels. 2007;22:251–3. doi: 10.1007/s00380-006-0962-9. [DOI] [PubMed] [Google Scholar]


