Introduction
In recent years, there has been a marked decline in applicants to United States nephrology programs (1). Although a multipronged approach is clearly needed to increase interest in nephrology, it is important that we ensure that our applicants/future colleagues are treated in the most fair and equitable manner possible, and we believe that 100% participation in the National Residency Matching Program (NRMP) is vitally important to achieving that goal. In this perspectives article, we will briefly review the evolution of the Match since it was implemented for appointment year (AY) 2009, the successes achieved, and the challenges ahead.
A Brief History of the Nephrology Match
In June of 2007, the Nephrology Training Program Directors (TPDs) voted by an overwhelming majority in favor of nephrology joining the Medical Subspecialties Matching Program (MSMP) administered by the NRMP. This decision occurred after years of vigorous debate and was precipitated in large part by the implementation of the Electronic Residency Application System (ERAS), the web-based platform used by applicants to residency and fellowship programs, in 2005. The ERAS, which was created for use in the context of the Match, established a uniform date when all TPDs could simultaneously access applications. However, without the protections for applicants and programs established by the Match, the ERAS incentivized TPDs to exert pressure on applicants to commit to their programs before applicants had an opportunity to interview at other programs. After attempts to remedy this situation by establishing a “uniform offer date” proved to be similarly flawed, the Nephrology TPDs voted in favor of the Match, because most felt that it was the best mechanism available to protect applicants from being pressured to commit to programs before they had adequate opportunity to interview at all programs in which they had an interest.
Another change that affected fellow recruitment occurred when the NRMP moved the recruitment season for the Medical Specialties Matching Program (MSMP) 6 months closer to the start of fellowship training. This occurred for AY 2013 and was done in response to requests from Internal Medicine Program Directors who believed that residents would benefit from additional time to discern their preferred career paths. This change caused concern among many Nephrology TPDs that it would become more difficult for international medical graduates (IMGs) to apply for fellowship during their third year of residency, creating a compressed timeframe for them to obtain visas.
During AY 2009, the first year of the Nephrology Match, there were 578 applicants for 367 positions (1.6 applicants per position) at 121 programs offered via the Match. Survey of TPDs after the first year of the Match revealed that the majority of respondents had positive experiences and received more positive than negative comments from applicants concerning the Match (2). During the next 4 years, the number of nephrology fellowship positions offered via the Match increased each year until AY 2013, when 416 positions were offered. The increase in the number of positions offered via the Match was driven by both an increase in the size of programs and an increase in the proportion of positions offered via the Match (3). During that same period, the ratio of applicants to available positions declined to 1.0, and the success rate for applicants seeking to match at nephrology programs rose to 89%. The number of nephrology fellowship positions offered in the Match subsequently declined for the first time in AY 2014 by 3% and by an additional 7% in AY 2015.
Of the internal medicine subspecialties, gastroenterology has the best documented experience in the effects of withdrawing from the Match on the recruitment process. In 1999, after several years of declining Match participation, gastroenterology withdrew from the Match. The subsequent 7 years brought “unheralded chaos” on their application processes, and gastroenterology subsequently voted to reinstate the Match for AY 2007 (4). After reimplementation of the Match, a survey of TPDs revealed that 93% felt that re-entering the Match was “good for the gastroenterology profession as a whole” (5).
Nephrology Goes All in for the Match
Because of concerns that the decline in the percentage of United States nephrology programs participating in the Match might threaten the ability of nephrology to continue to participate in the Match (then the NRMP required 75% of programs and total positions to be filled via the Match as a prerequisite for specialty participation), the American Society of Nephrology (ASN), the sponsoring organization of the Nephrology Match, took action (6). To ensure the future integrity of the Nephrology Match and maximize the benefits of the protections offered by the Match for applicants and programs, the ASN became the first internal medicine subspecialty to adopt an All-In policy, requiring all nephrology training programs accredited by the Accreditation Council for Graduate Medical Education to participate in the NRMP MSMP and offer all training positions through the MSMP.
To maximize adherence to All-In, certain benefits were restricted to participating programs (https://www.asn-online.org/education/training/match/). Because the ERAS and the NRMP are separate entities with different registration dates, the ASN requires that programs sign a memorandum of understanding (MOU) indicating that they will adhere to the All-In policy, and only programs that submit a signed MOU are granted access to the ERAS. There are also several ASN-specific benefits that are restricted to participating programs, including access to certain ASN website functions, access to ASN-sponsored grants, and other opportunities. In 2015, the ASN and the ASN Match Committee strongly encouraged all programs to participate in the Match, but the All-In policy was not able to be fully implemented, because it was too late in the recruitment season. The All-In policy was fully implemented for the AY 2016 recruitment season, and an MOU was distributed to all programs, which was signed by 100% of the 145 eligible programs. By this time, the NRMP had also agreed to help adjudicate the All-In agreement for the Match and issue sanctions to those programs that did not adhere to their Match Participation Agreement.
Since nephrology became the first internal medicine subspecialty to adopt All-In, infectious diseases, sleep medicine, and medical genetics have subsequently implemented All-In policies.
Successes and Challenges of All-In
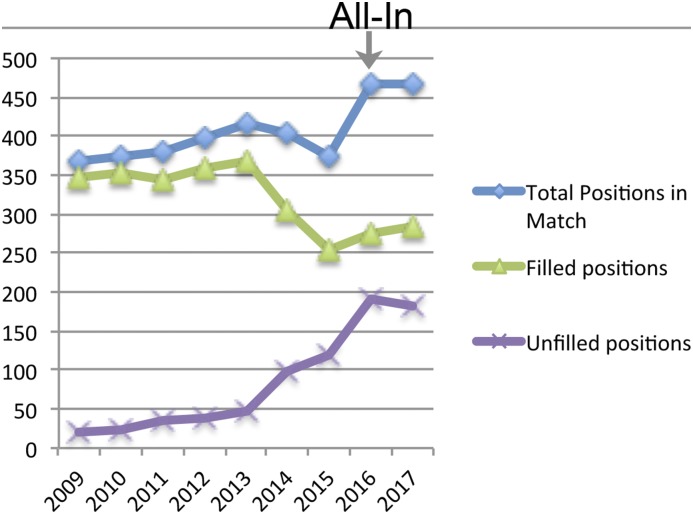
Before implementation of All-In, participation in the Match by nephrology fellowship programs decreased for AY 2014 and AY 2015 (Figure 1). Since implementation of the All-In policy, the numbers of positions and tracks offered in the Match increased by 8% and 8.5%, respectively, from AY 2015 to AY 2016 (Figure 1). After extensive review of data from the AY 2016 Match, the ASN staff contacted programs suspected of not fully conforming to the All-In policy. Very few programs were found to have not fully adhered to All-In, and further discussions with leadership at these programs resulted in 100% of eligible programs committing to adhere to All-In for AY 2017. The success of All-In is supported by data showing that AY 2017 was notable for the highest-ever number of fellowship positions (467) and tracks (165) offered via the Match (Figure 1). Further review of data by the ASN Match Oversight Task Force and follow-up by the ASN staff have revealed no definitive evidence of violations of the All-In policy for AY 2016.
Figure 1.
The figure shows the number of unfilled positions in part due to the increased number of positions due to All-In.
Despite the success of All-In encouraging full participation in the Match, there have been some challenges. For some programs, especially research fellowships and others offering specialized training tracks, the requirement that 100% of fellows must be recruited via the Match has made recruitment more complex. Potential adverse consequences of All-In include increased time and financial costs required for applicants and programs that would otherwise prefer out of Match offers and the possibility of an applicant not matching at the preferred program due to errors by the applicant or program in creating or certifying rank lists. However, although a TPD may believe that an applicant prefers the perceived simplicity of an out of match offer, that applicant might disagree but be reluctant to decline the offer out of fear of losing the option of obtaining a position in that program. Moreover, requiring research residency applicants to apply via the Match gives applicants unencumbered opportunities to pursue a fellowship at another program if they decide during the course of residency that another program would allow them to better achieve their professional or personal goals. Many nephrology programs with research and combined training pathways have successfully adhered to an All-In strategy since the inception of the Nephrology Match, and the ASN Council has endorsed the All-In policy to minimize exceptions and promote confidence among all programs that the policy is being implemented as equitably as possible.
Although we are encouraged by the recent high levels of Match participation, it must be acknowledged that the All-In policy and the Match do not address the underlying issue of the decline in the number of nephrology fellowship applicants in recent years. The ratio of applicants per position offered in the Match steadily declined from 1.55 in AY 2009 to 0.6 in AY 2016, and this ratio finally stabilized in AY 2017, as did the percentage of programs completely filling via the Match (41% and 42% for AY 2016 and AY 2017, respectively). Among internal medicine subspecialties with ≥25 positions in the Match, rheumatology and gastroenterology had the highest ratios of applicants per position (1.6 and 1.5, respectively), whereas geriatric medicine had the lowest (0.5). Surprisingly, current ERAS data for the AY 2015 showed that 265 of 446 (59%) of nephrology applicants simultaneously applied to other subspecialties, with the highest number of applicants applying for pulmonary and/or critical care. These numbers are higher than those for most other internal medicine subspecialties; the percentages of gastroenterology, endocrinology, and infectious diseases applicants applying to other subspecialties were 18%, 31%, and 41%, respectively. Although these data are concerning and the reasons require further study, the TPDs must adhere to the NRMP Match Communication Code of Conduct, which forbids interviewers from asking applicants about other programs to which they are applying to respect their right to privacy and confidentiality (www.nrmp.org/communication-code-of-conduct).
How Do We Increase the Number of Fellowship Applicants?
It is clear that a multipronged approach is needed to reverse the trend of decreasing nephrology applicants. The ASN, the ASN Workforce Committee, and the TPD Executive Committee have worked to develop new programs to increase interest in nephrology. The ASN sponsors the Kidney Students and Residents program and provides funding for up to 200 medical students, residents, or hospitalists to attend Kidney Week, where they are mentored by the TPDs and provided with several trainee-oriented sessions. The innovative ASN Kidney Tutored Research and Education for Kidney Scholars program was established by the ASN to increase interest in nephrology and research through a week-long research retreat and long-term mentorship (7).
We believe that efforts are needed by nephrologists to enhance educational experiences for medical students and residents. Nephrology programs should partner with local internal medicine program leadership and should increase exposure of trainees to outpatient nephrology and kidney transplantation and to the most outstanding nephrology educators/mentors (8,9). Early identification of first or second year internal medicine residents interested in nephrology allows the nephrology fellowship director to establish a mentoring relationship early in their careers.
Increasing interest in nephrology will also be highly dependent on ensuring that there are rewarding employment opportunities available for fellows at the completion of their training. The recent The US Adult Nephrology Workforce 2016: Developments and Trends report (3) showed that efforts are needed to improve the job market for nephrologists, and this may require reducing the number of fellows trained in United States programs. The results of this survey should be interpreted with some caution, because only approximately one third of fellows participated; also, it is not clear if the results are generalizable to all nephrology fellows. Considerations regarding strategies for “right sizing” nephrology training programs have been reviewed and are an active point of discussion in the nephrology community (6).
Finally, the number of IMGs applying for nephrology fellowships has decreased by 26% in the past 5 years, which is a greater decline than in other internal medicine subspecialties with ≥25 annual positions in the Match (preliminary 2017 ERAS fellowship data from https://www.aamc.org/services/eras/stats/359278/stats.html). Because nephrology has a high percentage of IMG trainees, efforts are needed to help increase interest among IMG trainees and provide IMG fellows with assistance in navigating the job market, especially those who are on visas and require special considerations. Unfortunately, it is possible that recently proposed changes to United States immigration policies may significantly decrease the number of IMGs applying for nephrology fellowships. In conclusion, the ASN All-In policy has been effective in encouraging full participation in the Match by nephrology fellowship programs, which we believe serves the best interests of our trainees and programs. However, additional efforts are needed to increase the number of trainees choosing careers in nephrology.
Disclosures
None.
Acknowledgments
The authors thank Sharon Adler, Steven Cheng, and Scott Gilbert, who are members of the American Society of Nephrology Match Oversight Committee, for their contributions.
The content of this article does not reflect the views or opinions of The American Society of Nephrology (ASN) or the Clinical Journal of the American Society of Nephrology (CJASN). Responsibility for the information and views expressed therein lies entirely with the author(s).
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Berns JS, Ellison DH, Linas SL, Rosner MH: Training the next generation’s nephrology workforce. Clin J Am Soc Nephrol 9: 1639–1644, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kohan DE, Rosenberg ME: Nephrology training programs and applicants: A very good match. Clin J Am Soc Nephrol 4: 242–247, 2009 [DOI] [PubMed] [Google Scholar]
- 3.Salsberg E, Quigley L, Mehfoud N, Masselink L, Collins A: The US Nephrology Workforce 2016: Developments and Trends, Washington, DC, American Society of Nephrology, 2016 [Google Scholar]
- 4.Proctor DD, Decross AJ, Willis CE, Jones TN, Pardi DS: The match: Five years later. Gastroenterology 140: 15–18, 2011 [DOI] [PubMed] [Google Scholar]
- 5.Niederle M, Proctor DD, Roth AE: The gastroenterology fellowship match--the first two years. Gastroenterology 135: 344–346, 2008 [DOI] [PubMed] [Google Scholar]
- 6.Hsu CY, Parker MG, Ross MJ, Schmidt RJ, Harris RC; ASN Nephrology Match Task Force: Improving the nephrology match: The path forward. J Am Soc Nephrol 26: 2634–2639, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maursetter LJ, Stern LD, Sozio SM, Patel AB, Rao R, Shah HH, Leight K, Okusa MD, Zeidel ML, Parker MG: Enhancing nephrology career interest through the ASN kidney TREKS program. J Am Soc Nephrol 27: 1604–1607, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jhaveri KD, Shah HH, Mattana J: Enhancing interest in nephrology careers during medical residency. Am J Kidney Dis 60: 350–353, 2012 [DOI] [PubMed] [Google Scholar]
- 9.Agrawal V, Jhaveri KD, Shah HH: Enhancing outpatient nephrology experience for internal medicine residents. Clin Kidney J 2017, in press [DOI] [PMC free article] [PubMed] [Google Scholar]