Abstract
In May 2003 a survey was conducted in the Western Region of Bhutan to assess the prevalence and intensity of soil-transmitted helminth (STH) infections after 15 years of school deworming in the country.
Five schools were randomly selected in the region and 266 schoolchildren were examined. Stool samples were collected from each child as well as nutritional indicators and general information on each school.
The survey found a cumulative prevalence of 16.5% STH (4.8% in schools treated in the last three months and 24% in the untreated schools). An unexpected finding was that tapeworm infection rate of 6.7%.
These results indicate a high reinfection rate in this area.
WHO recommends a 50% prevalence as the threshold for the establishment of community intervention. However, in our view, Bhutan needs to continue its deworming programme because the present, relatively low, prevalence level was found despite a long period of intervention; an interruption of the control activities will result in a return to very high levels of prevalence and intensity of infection.
Introduction
It is estimated that more than 1 billion people in the world are infected by Soil-Transmitted Helminths (STH) which include Ascaris lumbricoides, Trichuris trichiura and hookworms (Crompton, 1999). These infections most frequently affect children in developing countries and are associated with poor growth, reduced physical activity and impaired learning ability (Stephenson et al., 1990, Nokes et al., 1992, Adams et al., 1994, Koroma et al., 1996, Stoltzfus et al., 1996). Ultimately, infection can only be controlled by improving sanitation and living conditions, but these measures often take long time and can be extremely costly. On the other hand, regular treatment of the population at risk with a broad spectrum anti-helminthic drug has been advocated as a cheap and effective means of reducing the worm burden and its related morbidity (WHO 2003).
Bhutan is situated in the Eastern Himalayas between India and China and has one of the most rugged terrain in the world. The economy is largely agro-based and the total population of around 2 million (UN, 2000) live in scattered, small rural settlements and survive on subsistence farming. The country can be roughly divided into three climatic zones: the north is characterized by high mountains and is extremely cold in winter and therefore unfavourable to STH transmission. The central belt of the country is more tropical and can be subdivided into the western region which has a better network of roads and access, and the eastern area where settlements are more remote and sanitation reputedly less adequate. The southern belt is dramatically hotter. Three STH surveys have been carried out, in 1985, 1986 and 1989. None of these surveys were published in peer review journals and there is no clear description of the methodology making it difficult to assess their accuracy. These surveys found a prevalence of STH infection between 20% and 70%.
Bhutan has had a school deworming programme in place since 1988. A single dose of albendazole (400 mg) is administered yearly to the schoolchildren. In addition preschool children are dewormed when they visit the Health Units. Unfortunately data on school deworming are not systematically collected and detailed reports are not compiled; teachers confirm that albendazole (400 mg) is distributed annually, but it is not possible to obtain more detailed information about the precise date of drug distribution or coverage apart from the most recent rounds.
The objective of the survey presented here was to assess the prevalence and intensity of STH in school-age children (6-15 years) in the western part of the central belt of the country.
Materials and Methods
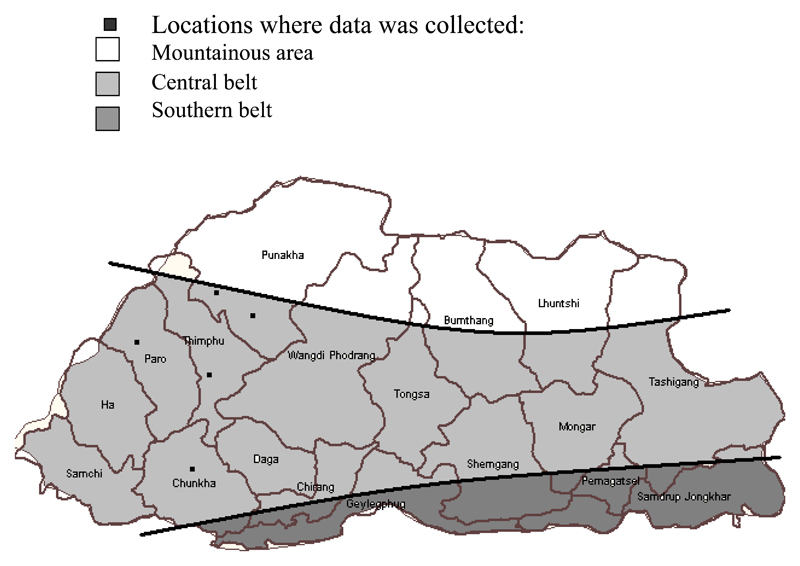
The guidelines 'Helminth Control in school-age children' (Montresor et al., 2002) were followed for the implementation of the survey. The data were collected from children of five schools randomly selected in the Western Region of the country (see Figure). Children from two schools had received deworming treatment during the three months prior to the survey. The remaining schools had not been dewormed recently. In each school 50 children in Class III (9 year olds) were selected. If Class III did not have the required number, then the whole of Class IV (10 year olds) was also surveyed.
Figure.
Map of Bhutan showing the districts where data was collected and the ecological areas of the country
The data collection was performed by two teams each one composed of a team leader, a medical technician, an experienced lab technician, a Basic Health Unit worker and a driver. Before the fieldwork, the technicians were refreshed in the Kato Katz technique at the Thimphu Referral Hospital laboratory. Both teams surveyed the first two schools together and then divided to cover the remaining three schools.
For each child, data was collected on age, sex, height (by standard measuring tape) and weight (UNICEF scales). A blood sample was collected by finger prick using a sterile lancet and analysed with portable spectrophotometer (HemoCue AB, Angelhom, Sweden). Children with Haemoglobin <11 g/dl were considered anaemic and children with Hb <7 g/dl were considered severely anaemic. Faecal samples were collected in plastic containers and analysed for parasite eggs on same day of collection using the Kato Katz technique (WHO, 1993). The intensity of infection was classified according the WHO thresholds (WHO, 2003).
Additional information on the school including the condition of the latrines and water sources was also collected. All parasitological data was analysed using software packages SIP Survey and Epi-Info.
Results
The total number of children examined was 266 (60% girls). The mean age was 11.5 years (range 6 - 17). In the schools which had been dewormed, the mean age was respectively 12.2 years (6-17) and in the schools which had not been dewormed, the mean age was 11.1 years (8-16). The percentage of girls was respectively 62% and 58%. The parasitological results are presented in Table 1.
Table.
Summary of Key Findings
| Total sample (n=266) |
Schools treated in the last three months (n=104) |
Schools not treated in the last three months (n=162) |
||||
|---|---|---|---|---|---|---|
| Prevalence | Moderate heavy intensity | Prevalence | Moderate heavy intensity | Prevalence | Moderate heavy intensity | |
| Ascaris lumbricoides | 12.8% | 3.0% | 1.9 %* | 1.3% | 19.8%* | 4.0% |
| Trichuris trichuria | 5.6% | - | 2.9% | -- | 7.4% | -- |
| Hookworm | 1.1% | - | -- | -- | 1.9% | -- |
| Prevalence of any STH infection | 16.5% | 3.0% | 4.8%* | 1.3% | 24%* | 4.0% |
| Taenia solium | 6.7% | NA | 0 | NA | 11% | NA |
(*p <0.001)
The total number of anaemic children was 14 (5.3%); only 1 case (0.4%) of severe anaemia was identified.
Discussion
In our view, the present prevalence and intensity of STH in Bhutan should be interpreted in the light of the fact that deworming activities have been in place in the schools for approximately 15 years.
According to WHO guidelines (WHO, 2003), a baseline prevalence of 16% with 3% of infection of moderate intensity does not require community intervention. However, these levels were found after several years of drug distribution, demonstrating, in our view, that reinfection rates are very high in the area. This analysis is confirmed by the significant difference between schools that had received treatment in the three months before data collection and the ones which had not.
We recommend that the monitoring and reporting system of Bhutan's programme should be strengthened to allow a better evaluation of the situation in the future.
With such a high level of transmission, we recommend chemotherapy should be continued and at the same time sanitation and education in personal hygiene needs to be improved.
The low rates of anaemia found in this age group, compared with a more severe situation in older age groups (MOHE, 2001) would also indicate that the deworming programme is having a positive nutritional impact and should be continued.
The prevalence of tapeworm infection measured in the sample is, in our view, indicative of a serious public health problem. It is well known that direct microscopic examination underestimate the true prevalence of tapeworm by several fold and concentration techniques are normally required to evaluate the real prevalence (WHO, 1993). Data from neighbouring Nepal confirm this hypothesis (Joshi et al., 2001).
Contributor Information
Henrietta Allen, World Health Organization, Geneva, Switzerland.
Gyambo Sithey, Ministry of Health and Education, Bhutan.
EA Padmasiri, World Health Organization, Regional Office for South East Asia.
Antonio Montresor, World Health Organization, Geneva, Switzerland.
References
- Adams EJ, Stephenson LS, Latham MC, Kinoti SN. Physical activity and growth of Kenyan school children with hookworm, Trichuris trichiura and Ascaris lumbricoides infections are improved after treatment with Albendazole. J Nutr. 1994;124:1199–1206. doi: 10.1093/jn/124.8.1199. [DOI] [PubMed] [Google Scholar]
- Crompton DWT. How much human helminthiasis is there in the world? J Parasitol. 1999;85:397–403. [PubMed] [Google Scholar]
- Joshi DD, Poudyal PM, Jimba M, Mishra PN, Neave LA, Maharjan M. Controlling Taenia solium in Nepal using the PRECEDE-PROCEED model. Southeast Asian J Trop Med Public Health. 2001;32(Suppl 2):94–7. [PubMed] [Google Scholar]
- Koroma MM, Williams AM, De La Haye RR, Hodges M. Effects of Albendazole on growth of primary school children and the prevalence and intensity of soil-transmitted helminths in Sierra Leone. J Trop Ped. 1996;42:371–372. doi: 10.1093/tropej/42.6.371. [DOI] [PubMed] [Google Scholar]
- Ministry of Health and Education, Bhutan. National Anaemia Survey (2001) 2003 in press. [Google Scholar]
- Montresor A, Gyorkos T, Crompton DWT, Savioli L. Helminth Control in school-age children. World Health Organization; Geneva: 2002. [Google Scholar]
- Nokes C, Grantham-McGregor SM, Sawyer AW, Cooper ES, Bundy DAP. Parasitic helminth infection and cognitive function in school children. Proc R Soc Lond. 1992;247:77–81. doi: 10.1098/rspb.1992.0011. [DOI] [PubMed] [Google Scholar]
- Stephenson LS, Latham MC, Kinoti SN, Kurz KM, Brigham H. Improvement in physical fitness of Kenyan schoolboys infected with hookworm, Trichuris trichiura and Ascaris lumbricoides following a single dose of Albendazole. Trans R Soc Trop Med Hyg. 1990;84:277–282. doi: 10.1016/0035-9203(90)90286-n. [DOI] [PubMed] [Google Scholar]
- Stoltzfus J, Albonico M, Chwaya HM. Hemoquant determination of hookworm-related blood loss and its role in iron deficiency in African children. Am J Trop Med Hyg. 1996;55:399–404. doi: 10.4269/ajtmh.1996.55.399. [DOI] [PubMed] [Google Scholar]
- UN Population Division. World Population Prospects: The 2002 Revision Population Database. http://www.un.org/esa/population/unpop.htm.
- WHO. Basic laboratory techniques in medical parasitology. WHO; Geneva: 1993. [Google Scholar]
- WHO. Prevention and control of schistosomiasis and soil-transmitted helminthiasis. Report of a WHO Expert Committee. WHO; Geneva: 2003. [PubMed] [Google Scholar]