Abstract
Background
Evaluation of sexual disorders among persons receiving methadone replacement therapy is of great importance, because these problems may lead to non-compliance and relapse. This study aimed to estimate the effect of methadone maintenance therapy (MMT) on sexual function among addicted Iranian men using met-analysis.
Methods
Investigating the available data banks, relevant studies were identified. After exclusion of duplicates, irrelevant papers and low quality articles, eligible papers were entered into the meta-analysis. Prevalence and standardized mean difference of sexual function scores were illustrated by forest plots based on sexual desire, orgasm and erectile function.
Findings
During the primary search, 5341 evidences were identified. After application of the inclusion/exclusion criteria and quality assessment, nine papers were detected eligible for final meta-analysis. Total prevalence [95% confidence intervals (CI)] of sexual disorders and erectile dysfunction among Iranian men under methadone therapy were estimated as 66.3% (27.1-105.5) and 77.5% (61.9-93.1), respectively. The standardized mean differences (95% CI) of Sexual desire, orgasm and erection before and after methadone therapy were estimated as 0.16 (-0.68, 0.99), -0.01 (-0.75, 0.74) and 0.11 (-0.41, 0.64), respectively.
Conclusion
This meta-analysis showed that methadone therapy did not significantly influence the sexual desire, erectile function and orgasm among opium dependent men.
Keywords: Methadone therapy, Sexual dysfunction, Libido, Orgasm, Erection
Introduction
Sexual problems which has involved up to 85.7% of opium users' needs to be taken into consideration.1,2 Methadone maintenance therapy (MMT) is an effective substitute treatment for opium dependency, and has led to a considerable reduction in drug abuse.3 However, sexual disorder has remained as one of the main adverse effects of this treatment.4 Prevalence of sexual disorders among Iranian people under methadone therapy has been reported from 18.3% to 94.8%.5-9 Such disorders might be ignored in clinics by patients or physicians.10,11
Many studies have shown higher prevalence of sexual dysfunctions among men receiving MMT as compared with general population. It is more important to monitor sexual problems among these patients because any sexual disorder can lead to treatment cessation and relapse to opium re-use. Moreover, these problems can reduce the marital satisfaction.12
Sexual dysfunctions are heterogeneous disorders specified with a considerable inability of sexual experience or sexual pleasure.13 According to DSM-IV-TR (Diagnostic and Statistical Manual of Mental Disorders-4th Edition-Text Revision) criteria, sexual disorders are classified as abnormality in sexual desire, sexual arousal, orgasm, sexual pain disorders, and non-classified sexual disorders.14 Sexual complications are the main cause of non-compliance among patients receiving MMT especially those under long term treatments.15 These patients might experience various complications such as sweating, constipation, sexual disorders, sleep disorders and appetite disorder from six months to three years after treatment.16
Several primary studies have been conducted to investigate the effect of methadone therapy on sexual function among Iranian opium users. These studies reported various results with controversies which is difficult to be applied in policymaking. Meta-analysis is a statistical method for managing such limitations.17-19 This study aimed to estimate the total prevalence of sexual disorders among Iranian opium users during methadone replacement therapy using meta-analytic techniques.
Methods
Relevant studies published in Persian and English until 29 February 2016 were searched within available databanks such as PubMed, Web of Sciences, Google Scholar, Scopus, SID, Iranmedex, Magiran and Irandoc. The search strategy was using the following keywords or their Persian equivalents as well as “AND” and “OR” operators:
“Erectile function, sexual disorder, sexual dysfunction, methadone maintenance therapy, MMT, erectile dysfunction, impotence, orgasm disorders, sexual performance, delayed ejaculation, premature ejaculation.”
The search was conducted during 1-10 march 2016 by two independent researchers. A third researcher was assigned to manage any probable disagreements. To increase the number of identified studies, all references as well as unpublished studies were reviewed and researchers tried to interview with specialists and research centers in the field of the meta-analysis question.
Inclusion criteria were all studies written in Persian or English investigating the prevalence of different sexual disorders among Iranian opium users under MMT and the relationship between these two factors (before/after mean differences). Eligible studies had to obtain enough quality scores during the quality assessment. Exclusion criteria were studies with unknown sample size, without full text, quality score less than 15.5, studies that did not use DSM-IV-TR diagnostic criteria and finally, studies that were carried out among non-Iranian populations.
Full text or abstracts of all primary studies were extracted. At first, duplicates were detected and excluded. Then, titles, abstracts and full texts were reviewed and irrelevant papers were identified and removed. The researchers investigated the results of the primary studies in detail to detect repeated results.
The quality of the primary studies was assessed using STROBE (Strengthening The Reporting of OBservational Studies in Epidemiology) checklist including 22 methodological questions such as sample size and sampling method, study design and objectives, data collection, definition of the main variables and statistical tests.20 Studies were classified into three categories: low quality (less than 15.5), moderate quality (15.5-29.5) and high quality (30-44). Only moderate and high quality studies were entered into the final meta-analysis.20
Two independent researchers extracted all necessary information such as author name, date of study conduction, country of origin, total sample size, age, prevalence of abnormal libido, erectile dysfunction and orgasmic dysfunction before and after methadone therapy. The extracted results were entered into the excel spreadsheets.
Stata statistical software, Release 11.0 (Stata Corporation, College Station, TX, USA) was used for data analysis. Cochrane and I-squared indices were used to evaluate the heterogeneity between the results. Since the heterogeneity was significant, point prevalence of mean differences were pooled according to the random effect mode. Standard error of the prevalence was calculated based on binomial distribution formula. The point and pooled estimates were illustrated by forest plots including specific boxes (weight of the studies) and crossed lines [95% confidence intervals (CI)]. The probability and degree of publication bias was assessed using egger test and P-value less than 0.1 was considered statistically significant.
Results
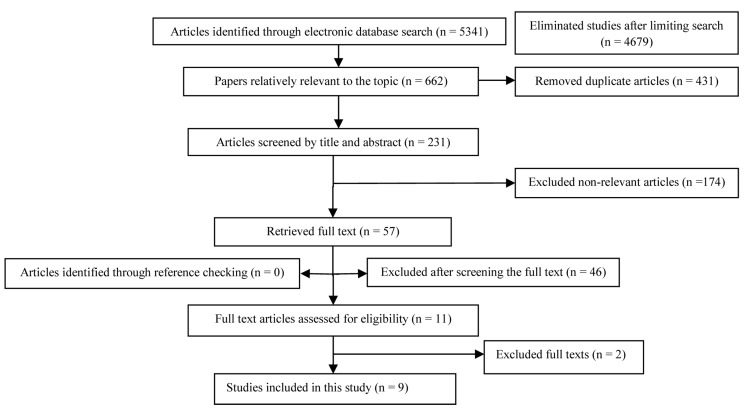
During the advanced search, 5341 primary studies were identified. After investigating and exclusion of duplicates, 231 papers remained. Investigating titles and abstracts revealed 174 irrelevant papers. Reviewing full texts, showed 46 irrelevant studies. During quality assessment as well as considering inclusion/exclusion criteria, two studies were omitted. Finally, nine articles were considered eligible for meta-analysis (Figure 1).4,5-9,21-23 Out of these eligible papers, two studies reported only mean scores of sexual disorders before and after methadone therapy, while two studies estimated both mean difference and prevalence of sexual disorders. The five remaining studies had just reported the prevalence of sexual disorders (Tables 1 and 2).
Figure 1.
Literature search and review flowchart for selection of primary studies
Table 1.
Characteristics of primary studies reporting the methadone effect before and after the methadone maintenance therapy (MMT)
| First author | Sample size | Average age (year) | Sexual desire |
Orgasm |
Erectile function |
|||
|---|---|---|---|---|---|---|---|---|
| Before |
After |
Before |
After |
Before |
After |
|||
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |||
| Babakhanian et al.4 | 30 | 34.5 | 5.1 ± 2.3 | 6.6 ± 2.1 | 4.7 ± 4.5 | 4.6 ± 1.9 | 16.80 ± 7.10 | 21.8 ± 6.4 |
| Parvaresh et al.6 | 180 | - | 3.2 ± 1.0 | 3.7 ± 1.0 | 6.5 ± 1.9 | 7.5 ± 1.8 | - | - |
| Rahbar Taramsari et al.21 | 382 | 37.6 | - | - | - | - | 18.3 ± 7.0 | 19.3 ± 5.8 |
| Roshanpajhu et al.22 | 69 | 34.6 | 3.7 ± 1.0 | 2.6 ± 2.0 | 5.9 ± 1.3 | 4.5 ± 3.3 | 2.7 ± 0.7 | 2.1 ± 1.8 |
SD: Standard deviation
Table 2.
Characteristics of primary studies reporting the prevalence of sexual disorders among men under methadone maintenance therapy (MMT)
| First author | Duration of methadone therapy | Sample size | Average age (year) | Prevalence of (%) | |
|---|---|---|---|---|---|
| Sexual dysfunction | Erectile function | ||||
| Babakhanian et al.4 | 6 month | 30 | 34.5 | 81.0 | - |
| Tatari et al.5 | At least 30 days | 72 | 36.2 | - | 93.0 |
| Hosseini et al.7 | - | 200 | 39.5 | 72.0 | - |
| Kheradmand et al.9 | At least 30 month | 185 | 36.3 | 17.8 | - |
| Tatari et al.23 | At least 30 days | 157 | 39.5 | - | 60.5 |
| Rahbar Taramsari et al.21 | - | 382 | 37.6 | - | 78.5 |
| Kheirabadi et al.8 | At least 30 month | 135 | - | 94.8 | - |
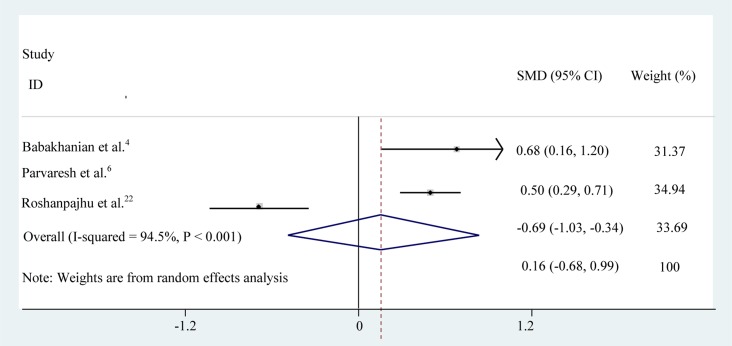
The average situation of sexual desire before and after the methadone therapy was compared among 279 opium users. A significant increase in libido was reported in the studies conducted by Babakhanian et al.4 and Parvaresh et al.6 while, Roshanpajhu et al.22 observed significant decrease in libido following treatment. Combining the results of these three studies based on random effect model (due to significant heterogeneity: I-squared = 94.5, Q = 36.5, P < 0.001), the total mean difference (95% CI) of libido before and after the methadone therapy was estimated 0.16 (0.68-0.99) (Figure 2). Eager test showed no significant publication bias (P = 0.200).
Figure 2.
Sexual desire before and after methadone maintenance therapy (MMT) SMD: Standardized mean difference; CI: Confidence interval
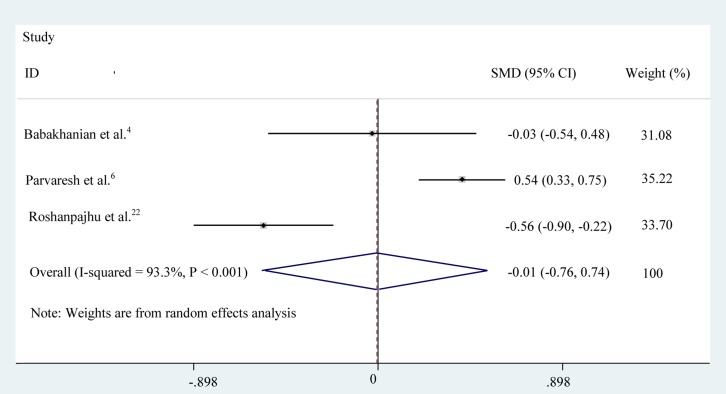
The degree of orgasmic function was reported before and after the MMT in three studies (Babakhanian et al.,4 Parvaresh et al.6 and Roshanpajhu et al22) conducted among 279 opium users. The treatment caused a significant increase in orgasm in Parvaresh et al.6 study, while decreased the orgasm in the two other studies. Combining the results of these three studies using random effect model (I-squared = 93%, Q = 29.9, P < 0.001) showed that the total mean difference (95% CI) of libido was -0.01 (-0.75-0.74) (Figure 3). Eager test showed no significant evidence of publication bias (P = 0.600).
Figure 3.
Orgasmic function before and after methadone maintenance therapy (MMT) SMD: Standardized mean difference; CI: Confidence interval
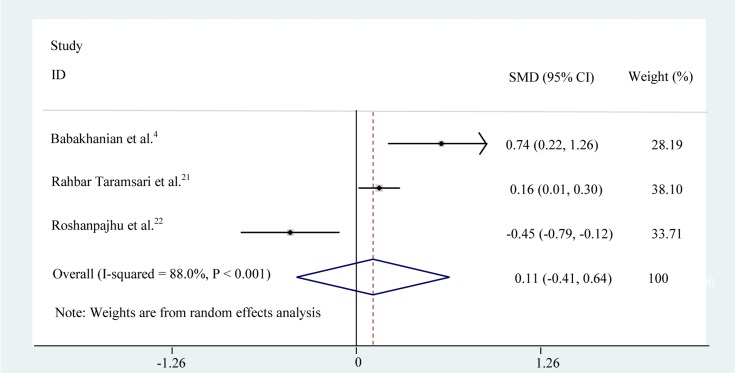
The erection status of 481 men receiving MMT were investigated by Babakhanian et al., Rahbar Taramsari et al.21 and Roshanpajhu et al.,22 two of which (Babakhanian et al.,4 Rahbar Taramsari et al.21) reported increased score of erection after treatment, while Roshanpajhu et al.22 did not find any change during treatment. The pooled estimate of mean erection score (95% CI) using random effect model (I-squared = 88%, Q = 16.6, P < 0.001) was 0.11 (-0.41-0.64) (Figure 4). No evidence of publication bias was observed based on the results of Eager test (P = 0.400).
Figure 4.
Erectile dysfunction before and after methadone maintenance therapy (MMT) SMD: Standardized mean difference; CI: Confidence interval
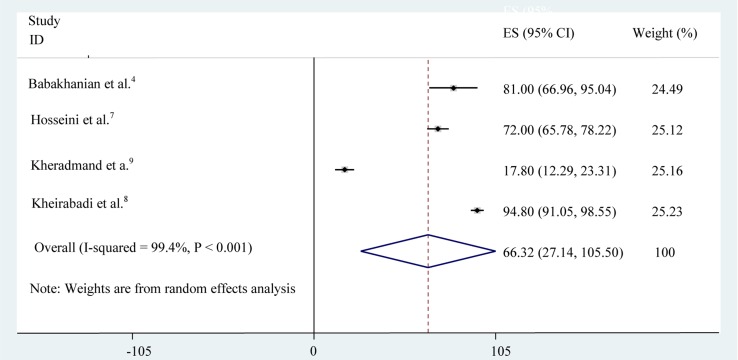
Prevalence of sexual disorders was reported in four studies varied between 17.8% in Kheradmand et al.9 study and 94.8% in Kheirabadi et al.8 study (Table 2). As illustrated in figure 5, combining the results of these four studies using random effect model (I-squared = 99.4%, Q = 515.01, P < 0.001) showed the prevalence (95% CI) of sexual disorders among opium users under MMT as 66.3% (27.1-105.5).
Figure 5.
Prevalence of sexual dysfunction among opium users receiving methadone maintenance therapy (MMT) ES: Effect size; CI: Confidence interval
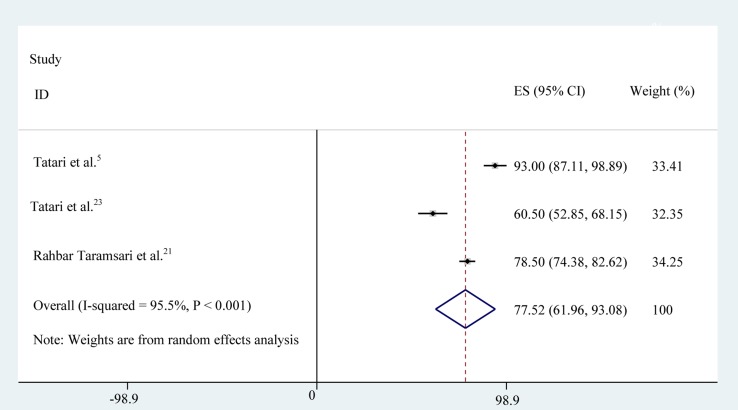
Erectile dysfunction rate among addicted men under MMT was reported in three studies varying from 60.5% to 93.0% in the two studies carried out by Tatari et al. in 201023 and 2013,5 respectively (Table 2). These results were combined and the total prevalence (95% CI) of erectile dysfunction was estimated 77.5% (61.9-93.1) (Figure 6). The heterogeneity between the primary prevalence reported in these studies was statistically significant (I-squared = 95.5%, Q = 44.1, P < 0.001).
Figure 6.
Prevalence of erectile dysfunction among opium users receiving methadone maintenance therapy (MMT) ES: Effect size; CI: Confidence interval
Discussion
Our meta-analysis showed that the average scores of sexual desire and erectile function after MMT were increased to 0.16 and 0.11, respectively. We also found 0.01 decrease in the average score of sexual desire following MMT. However, none of these changes were statistically significant. Our study also showed that 66.3% and 77.5% of men under MMT were complaining from sexual disorders and erectile dysfunction.
Results of a study showed that 85% and 87% of men and women under MMT reported sexual dysfunction during heroin abuse.24 Although MMT is an alternative treatment for opium dependent persons, several common adverse effects such as sexual dysfunction have been observed during this treatment regimen.4 Results of a study conducted in Australia as well as a meta-analysis conducted in 2014, reported about 50% and 52% sexual dysfunction during MMT, respectively.15,25
According to the primary studies of this meta-analysis, prevalence of sexual dysfunction during MMT was slightly higher in Iran than the world average. It can be due to factors such as cultural and ethnical differences, using alcohol and sedatives together with MMT and various methodologies. It seems that sexual disorder is one of the most important factors of non-compliance during MMT especially among those receiving high dose treatment. This complication can influence the marital life leading to relapse, treatment failure and sedative abuse.
According to the results of the study conducted by Trajanovska et al.26, serum prolactin level among opium users receiving an appropriate dose of methadone was significantly lower than that of street addicts consuming different kinds of substances. High prolactin level can induce sexual dysfunction even during MMT. Serum prolactin level remained low in 50%-60% one year after receiving methadone.26
Libido is defined as person’s overall sexual drive and desire for sexual activity. Sexual desire problems including hyposexuality and sexual disgust may be influenced by social, psychological, and biological factors.13 Among our primary studies, three studies investigated the sexual desire of opium users before and after MMT,4,6,22 two of them showed a positive effect of methadone therapy on sexual desire,4,6 while the third study indicated a negative effect.22 However, the total estimates showed non-significant influence of MMT.
It should be noted that in the primary studies the effect of biological and psychological confounders such as schizophrenia and depression, diabetes mellitus or history of major surgeries have been controlled. Similar to the pooled estimates in the current meta-analysis, another study carried out by Trajanovska et al. reported non-significant change in sexual desire following MMT.26 It has been shown that methadone is one of the factors which can reduce the serum testosterone level.15
Erectile dysfunction is the inability to develop or maintain penile erection during sexual activity associated with different organic, psychological and hormonal factors. Although this is not a life threatening problem, it can lead to sexual dysfunction and quality of life reduction.13 Erectile dysfunction is common among men receiving MMT and its prevalence has been estimated 68.5% among Malaysian men undergoing methadone maintenance treatment.27 The current meta-analysis did not show any significant effect of MMT on erectile function. Tatari et al. observed that treatment duration and the daily dose of methadone prescribed during MMT was associated with erectile dysfunction among men.5 Conversely, results of another study carried out in Kuala Lumpur indicated that erectile dysfunction was not related to MMT duration and methadone dose but was associated with the simultaneous use of other kinds of opiates such as heroin in combination with methadone during MMT.27
Aging and background disorders increase the risk of sexual disorders.28 However, Tatari et al. ruled out the influence of these factors. Other suspected factors are cigarette smoking, marital status, partner satisfaction, psychological factors, marriage age, educational level and patient knowledge regarding their problem and early treatment.5
Orgasm is a strong feeling of sexual pleasure experienced with perineal spasm.13 Orgasmic dysfunction can be developed following some surgeries for genitourinary system such as prostatectomy, depression and Parkinson disease. Prevalence of this problem in general population is 5%. According to the results of the two primary studies, the average orgasmic score was not improved after MMT,4,27 while Parvaresh et al. observed significant change during methadone therapy,6 Trajanovska et al. showed significant association between MMT and orgasmic dysfunction.26 Another case control study carried out in Japan in 1975, showed that seminal volume and prostatic secretion significantly decreased among patients under MMT compared to the control group.29
Conclusion
The current meta-analysis showed that MMT had no effect on the sexual desire, erectile function and orgasm among opium users. Considering the high prevalence of sexual disorders among these men, consultation and curative programs such as specific treatments with testosterone should be implemented to increase the quality of life and improve the familial relationships and prevent relapse to opium re-addiction.
Unfortunately, we found limited numbers of primary studies regarding the sexual effects of MMT. In addition, factors such as age, times spent with addiction, MMT duration, type of substance used, methadone dose and some background diseases can influence the sexual function. These factors were not estimated in most of the primary studies entered into the meta-analysis. Therefore, it was not possible to estimate the pooled effects in the subgroups. The heterogeneity between the results of primary studies was another limitation of our meta-analysis. Such heterogeneity can be due to differences in sample sizes, MMT duration, dose of methadone prescribed, different methodologies and the long effect of opium dependency on the sexual function.
The current meta-analysis provided reliable evidences regarding the effect of methadone therapy on sexual disorders which are suitable for policymakers in the field of harm reduction to plan strategies for increasing the effectiveness of MMT.
Acknowledgments
This study was financially supported by Mazandaran University of Medical Sciences, Iran. The authors would like to thank to the Mazandaran Student Research Committee for its kind cooperation.
Footnotes
Conflicts of Interest
The Authors have no conflict of interest.
REFERENCES
- 1.Chekuri V, Gerber D, Brodie A, Krishnadas R. Premature ejaculation and other sexual dysfunctions in opiate dependent men receiving methadone substitution treatment. Addict Behav. 2012;37(1):124–6. doi: 10.1016/j.addbeh.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 2.Shiri R, Falah Hassani K, Ansari M. Association between opium abuse and comorbidity in diabetic men. Am J Addict. 2006;15(6):468–72. doi: 10.1080/10550490601000421. [DOI] [PubMed] [Google Scholar]
- 3.Chen W, Li X, Li X, Ling L, Xia Y, Chen J, et al. Erectile dysfunction among male heroin addicts receiving methadone maintenance treatment in Guangdong, China. J Addict Med. 2012;6(3):212–8. doi: 10.1097/ADM.0b013e318259b2c4. [DOI] [PubMed] [Google Scholar]
- 4.Babakhanian M, Alam Mehrjerdi Z, Shenaiy Y. Sexual dysfunction in male crystalline heroin dependents before and after MMT: A pilot study. Arch Iran Med. 2012;15(12):751–5. [PubMed] [Google Scholar]
- 5.Tatari F, Shakeri J, Farnia V, Heidari F, Rezaei M. Bupropion in methadone induced erectile dysfunction. Life Sci J. 2013;10(9):330–2. [Google Scholar]
- 6.Parvaresh N, Sabahi AR, Mazhari S, Gilani H. A study of the sexual function, sleep, and weight status of patients after 6 months of methadone maintenance treatment. Addict Health. 2015;7(1-2):24–9. [PMC free article] [PubMed] [Google Scholar]
- 7.Hosseini SH, Isapour A, Tavakoli M, Taghipour M, Rasuli M. Erectile dysfunction in methadone maintenance patients: a cross sectional study in northern Iran. Iran J Psychiatry. 2013;8(4):172–8. [PMC free article] [PubMed] [Google Scholar]
- 8.Kheirabadi GR, Salehi M, Golafshan N, Maracy MR. Sexual dysfunction of men on methadone maintenance treatment mmt and its, relation with methadone dose and blood level of testosterone and prolactine. Med J Tabriz Univ Med Sci. 2012;34(4):16. [Google Scholar]
- 9.Kheradmand A, Amini Ranjbar Z, Zeynali Z, Sabahy AR, Nakhaee N. Sleep quality and sexual function in patients under methadone maintenance treatment. Int J High Risk Behav Addict. 2015;4(4):e23550. doi: 10.5812/ijhrba.23550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hanbury R, Cohen M, Stimmel B. Adequacy of sexual performance in men maintained on methadone. Am J Drug Alcohol Abuse. 1977;4(1):13–20. doi: 10.3109/00952997709002743. [DOI] [PubMed] [Google Scholar]
- 11.Risen CB. A guide to taking a sexual history. Psychiatr Clin North Am. 1995;18(1):39–53. [PubMed] [Google Scholar]
- 12.Johnson MW, Bruner NR. Test-retest reliability and gender differences in the sexual discounting task among cocaine-dependent individuals. Exp Clin Psychopharmacol. 2013;21(4):277–86. doi: 10.1037/a0033071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McCabe MP, Sharlip ID, Atalla E, Balon R, Fisher AD, Laumann E, et al. Definitions of sexual dysfunctions in women and men: A consensus statement from the fourth international consultation on sexual medicine 2015. J Sex Med. 2016;13(2):135–43. doi: 10.1016/j.jsxm.2015.12.019. [DOI] [PubMed] [Google Scholar]
- 14.Waldinger MD, Schweitzer DH. Changing paradigms from a historical DSM-III and DSM-IV view toward an evidence-based definition of premature ejaculation. Part I--validity of DSM-IV-TR. J Sex Med. 2006;3(4):682–92. doi: 10.1111/j.1743-6109.2006.00275.x. [DOI] [PubMed] [Google Scholar]
- 15.Hallinan R, Byrne A, Agho K, McMahon C, Tynan P, Attia J. Erectile dysfunction in men receiving methadone and buprenorphine maintenance treatment. J Sex Med. 2008;5(3):684–92. doi: 10.1111/j.1743-6109.2007.00702.x. [DOI] [PubMed] [Google Scholar]
- 16.Langrod J, Lowinson J, Ruiz P. Methadone treatment and physical complaints: A clinical analysis. Int J Addict. 1981;16(5):947–52. doi: 10.3109/10826088109038903. [DOI] [PubMed] [Google Scholar]
- 17.Moosazadeh M. Meta-Analysis of Prevalence of Smoking in 15-64-year-old Population of West of Iran. Int J Prev Med. 2013;4(10):1108–14. [PMC free article] [PubMed] [Google Scholar]
- 18.Moosazadeh M, Nekoei-Moghadam M, Aliram-Zany M, Amiresmaili M. Identification of mutation of glucose-6-phosphate dehy-drogenase (G6PD) in Iran: Meta- analysis study. Iran J Public Health. 2013;42(9):1007–15. [PMC free article] [PubMed] [Google Scholar]
- 19.Moosazadeh M, Amiresmaili M, Aliramezany M. Prevalence of G6PD deficiency in Iran, a mata-analysis. Acta Med Iran. 2014;52(4):256–64. [PubMed] [Google Scholar]
- 20.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Prev Med. 2007;45(4):247–51. doi: 10.1016/j.ypmed.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 21.Rahbar Taramsari M, Badsar A, Falahatkar S, Movassagh H, Fallah KarKan M, Montazeri S, et al. The Possible Effects of Methadone Maintenance Therapy on Erectile Dysfunction in Male Addicts Visiting MMT Centers of Rasht. Iran J Toxicol. 2014;8(25):1081–5. [Google Scholar]
- 22.Roshanpajhu M, Khodaei MR, Taafi E, Rezaei O, Nazeri-Astaneh A, Baghestani AR, et al. The Effect of Methadone on Sexual Function in Male Dependent to Opiates. J Rehab. 2012;12:65–71. [Google Scholar]
- 23.Tatari F, Farnia V, Nasiri RF, Najafi F. Trazodone in methandone induced erectile dysfunction. Iran J Psychiatry. 2010;5(4):164–6. [PMC free article] [PubMed] [Google Scholar]
- 24.Goldsmith D, Hunt D, Lipton D, Strug D. Methadone folklore: Beliefs about side effects and their impact on treatment. Human Organization. 1984;43(3):330–40. [Google Scholar]
- 25.Yee A, Loh HS, Hisham Hashim HM, Ng CG. The prevalence of sexual dysfunction among male patients on methadone and buprenorphine treatments: A meta-analysis study. J Sex Med. 2014;11(1):22–32. doi: 10.1111/jsm.12352. [DOI] [PubMed] [Google Scholar]
- 26.Trajanovska AS, Vujovic V, Ignjatova L, Janicevic-Ivanovska D, Cibisev A. Sexual dysfunction as a side effect of hyperprolactinemia in methadone maintenance therapy. Med Arch. 2013;67(1):48–50. doi: 10.5455/medarh.2013.67.48-50. [DOI] [PubMed] [Google Scholar]
- 27.Nik Ruzyanei NJ, Noormazita M, Azlin B, Normala I, Hazli Z, Abdul Aziz S, et al. Clinical correlates of erectile dysfunction among male patients on methadone maintenance therapy (MMT) in Kuala Lumpur. Malaysian Journal of Medicine and Health Sciences. 2012;8(1):27–35. [Google Scholar]
- 28.Hamidi Madani A, Ghanbari A, Fallah Manshadi L, Emadi SA. Survey the frequency of risk factors in men with erectile dysfunction. J Guilan Univ Med Sci. 2010;19(75):36–45. [Google Scholar]
- 29.Cicero TJ, Bell RD, Wiest WG, Allison JH, Polakoski K, Robins E. Function of the male sex organs in heroin and methadone users. N Engl J Med. 1975;292(17):882–7. doi: 10.1056/NEJM197504242921703. [DOI] [PubMed] [Google Scholar]