Abstract
Background
In recent years, single-port video-assisted thoracoscopic surgery (VATS) for lobectomy in non-small cell lung cancer (NSCLC) patients has become increasingly common. The objective of this study was to compare the feasibility and safety of single-port and triple-port VATS lobectomy.
Methods
A total of 73 patients with NSCLC who underwent VATS lobectomy from December 2011 to August 2016 were retrospectively reviewed, including 47 in the triple-port group and 26 in the single-port group. Statistical analysis was performed after propensity score matching. Patients were matched on a 1-to-1 basis.
Results
Operative time and intraoperative blood loss in the triple-port group and the single-port group were similar (189.4±50.8 minutes vs. 205.4±50.6 minutes, p=0.259; 286.5±531.0 mL vs. 314.6±513.1 mL, p=0.813). There were no cases of morbidity or mortality. No significant differences in complications or the total number of dissected lymph nodes were found between the 2 groups. In the single-port group, more mediastinal lymph nodes were dissected than in the triple-port group (1.7±0.6 vs. 1.2±0.5, p=0.011). Both groups had 1 patient with bronchopleural fistula. Chest tube duration and postoperative hospital stay were shorter in the single-port group than in the triple-port group (8.7±5.1 days vs. 6.2±6.6 days, p=0.130; 11.7±6.1 days vs. 9.5±6.4 days, p=0.226). However, the differences were not statistically significant. In the single-port group, the rate of conversion to multi-port VATS lobectomy was 11.5% (3 of 26). The rates of conversion to open thoracotomy in the triple-port and single-port groups were 7.7% and 3.8%, respectively (p=1.000).
Conclusion
In comparison with the triple-port group, single-port VATS lobectomy showed similar results in safety and efficacy, indicating that single-port VATS lobectomy is a feasible and safe option for lung cancer patients.
Keywords: Video-assisted thoracic surgery, Lobectomy, Lung neoplasms
Introduction
The first lobectomy was successfully performed using single-port video-assisted thoracoscopic surgery (VATS) by Gonzalez et al. [1] in 2011. Subsequently, the number of attempted single-port VATS lobectomies has increased. Studies have evaluated the effectiveness and feasibility of single-port VATS lobectomy [2–7]. However, due to the difficulty of the procedure, single-port VATS lobectomy is only performed in a limited range of hospitals. In South Korea, the first single-port VATS lobectomy was performed by Kang et al. [8] in 2012. In Dongsan Medical Center, it has been routinely performed since September 2015. Only a few results have been reported comparing the effectiveness of single-port VATS lobectomy and conventional triple-port VATS lobectomy. The objective of this study was to compare the feasibility and safety of single-port and triple-port VATS lobectomy for lung cancer patients.
Methods
1) Patients
A total of 73 patients with non-small cell lung cancer (NSCLC) who underwent VATS lobectomy from December 2011 to August 2016 were retrospectively reviewed, including 47 in the triple-port group and 26 in the single-port group. The preoperative staging workup included a complete blood count, serum biochemistry tests, computed tomographic (CT) scan of the chest, and positron emission tomography-CT and magnetic resonance imaging of the brain. The operability workup included pulmonary function tests (PFT) and a transthoracic echocardiogram.
The variables studied in each patient included age, sex, smoking habit, PFT, the presence of associated comorbidities, tumor type and location, type and duration of surgical intervention, operation-associated adhesion, cancer stage, histologic type, tumor size, lymph node staging (number of lymph nodes retrieved and number of nodal stations explored), duration of chest tube in place, length of hospital stay, postoperative complications, and intraoperative bleeding.
The selection criteria between single-port and triple-port VATS were not complicated. After September 2015, single-port VATS lobectomy was performed in all NSCLC patients except for those with bronchogenic lung cancer or tight pleural adhesion.
2) Propensity score matching
To create comparable groups of patients, propensity score matching (PSM) between triple-port VATS and single-port VATS lobectomy patients was performed. Patients were matched at a 1-to-1 ratio. The propensity score was calculated using clinical variables such as age, sex, smoking habit, PFT, comorbidities, pulmonary disease, preoperative T and N staging, pleural adhesion, incomplete fissure, and body mass index. Finally, a total of 52 patients, including 26 who underwent triple-port VATS lobectomy and 26 who underwent single-port VATS lobectomy, were enrolled in this study.
3) Operative procedure
In both groups, all patients were given general anesthesia with double-lumen endobronchial tube intubation. The operation was performed with 1-lung ventilation in the decubitus position. For triple-port VATS lobectomy, a 10-mm 2-port incision was made in the seventh intercostal space at the midaxillary line and the scapular line. After that, a minimal thoracotomy, with a size of approximately 2.0 to 3.0 cm, was made on the fourth or fifth intercostal space of the anterior axillary line. In the single-port group, a 2.0- to 3.0-cm minimal thoracotomy incision was made in the sixth intercostal space of the anterior axillary line. The operation was performed after attaching a wound protector (Elexis Wound Protector/Retractor; Applied Medical Technology Inc., Brecksville, OH, USA) to the minimal thoracotomy site. In the triple-port group, a 10-mm, 30° oblique-viewing thoracoscope was used. At the end of the operation, a chest drain was placed through the 10-mm port incision site in the seventh intercostal space.
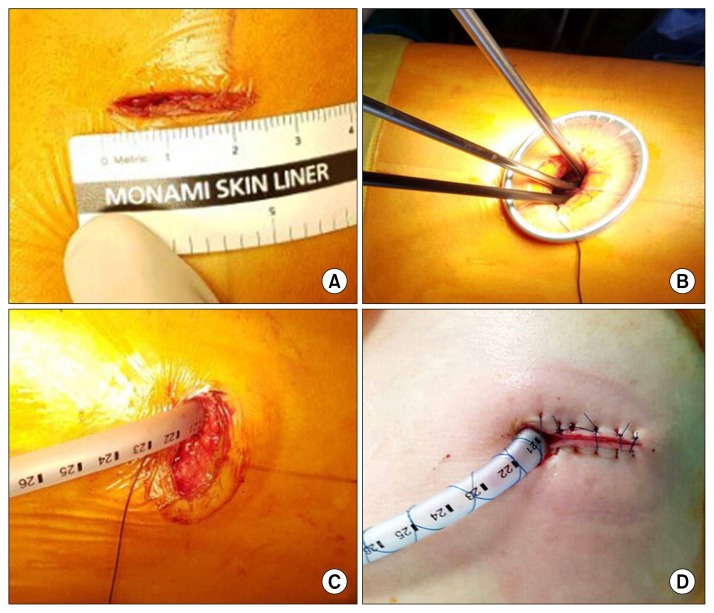
Single-port VATS lobectomy was performed using a 5-mm, 30° oblique-viewing thoracoscope. A 2.0- to 3.0-cm minimal thoracotomy was made in the sixth intracostal space at the anterior axillary line after checking for pleural adhesion through a 5-mm trocar (Fig. 1A, B). The majority of dissections were done using endoscopic hook electrocautery and a peanut dissector. After dissection of the pulmonary vessels and bronchus, resection was performed using flexible curved-tip endoscopic staplers. Lymphadenectomy was facilitated by electrocautery. After lobectomy, a protective specimen bag was used to remove specimens through minimal thoracotomy, and a single chest tube (24-Fr chest tube) was placed at the end of the incision (Fig. 1C, D).
Fig. 1.
(A) A minimal thoracotomy incision of 2.0 to 3.0 cm was made in the sixth intercostal space. (B) We used a 5-mm, 30° oblique-viewing thoracoscope. (C, D) After lobectomy, a 24-Fr chest tube was placed at the end of the incision.
In both groups, lymph node dissections including mediastinal, subcarinal, and lobe-specific lymph nodes were performed. In lobectomies on the left side, the para-aortic and subaortic lymph nodes were also dissected.
4) Postoperative course
All patients stayed in the intensive care unit for 1 night. Their chest drain was removed according to the following criteria: (1) the amount of chest drainage was less than 200 mL without air leakage; and (2) there was no pneumothorax or localized pleural effusion on chest X-rays. Patients were discharged from the hospital 2 days after removing the chest tube.
5) Statistical analysis
Continuous variables are presented as means with standard deviations, while categorical variables are presented as frequencies and percentages. The propensity score was calculated using multivariate logistic regression. To compare the 2 groups, the independent-samples t-test was used for continuous variables, while the Fisher exact test was used for categorical variables. IBM SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA) was used for all statistical analyses. All p-values <0.05 were considered to indicate statistical significance.
Results
From February 2011 to August 2016, 73 patients underwent curative thoracoscopic lobectomy, including 47 patients who underwent triple-port VATS from February 2011 to September 2015. Single-port VATS was performed in 26 patients by the same thoracic surgeon from September 2015 to August 2016. Patients in both groups were matched 1-to-1 with respect to clinical variables. After PSM, the male-to-female ratio, age, and results of preoperative PFT were similar between the triple-port group and the single-port group (57.7% versus 57.7%; 65.0±9.4 years versus 64.8±9.7 years; 2.3±0.4 L versus 2.3±0.7 L) (Table 1).
Table 1.
Patient characteristics before and after PSM
| Characteristic | Before PSM | After PSM | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Triple port (N=47) | Single port (N=26) | p-value | Triple port (N=26) | Single port (N=26) | p-value | |
| Age (yr) | 64.6±8.9 (45–80) | 64.8±9.5 (41–83) | 0.912 | 65.0±9.4 (45–80) | 64.8±9.7 (41–83) | 0.954 |
|
| ||||||
| Sex (male) | 25 (53.2) | 15 (57.7) | 0.957 | 15 (57.7) | 15 (57.7) | 1.000 |
|
| ||||||
| Smoking | 25 (53.2) | 15 (57.7) | 0.845 | 15 (57.7) | 15 (57.7) | 1.000 |
|
| ||||||
| Comorbidity | ||||||
|
| ||||||
| Chronic obstructive pulmonary disease | 4 | 3 | 1.000 | 4 | 3 | 1.000 |
|
| ||||||
| Tuberculosis | 3 | 1 | 1.000 | 1 | 1 | 1.000 |
|
| ||||||
| Asthma | 1 | 0 | 1.000 | 0 | 0 | 1.000 |
|
| ||||||
| Cardiac disease | 3 | 2 | 1.000 | 2 | 2 | 1.000 |
|
| ||||||
| Previous cancer | 7 | 2 | 0.476 | 3 | 2 | 1.000 |
|
| ||||||
| Preoperative forced expiratory volume in 1 second (L) | 2.2±0.5 (1.3–3.3) | 2.3±0.1 (1.3–3.6) | 0.841 | 2.3±0.4 (1.4–3.4) | 2.3±0.7 (1.3–3.6) | 0.887 |
Values are presented as mean±standard deviation (range) or number (%).
PSM, propensity score matching.
In terms of histologic factors, the mean tumor size in the triple-port and the single-port groups was 23.2±9.4 mm and 23.2±14.8 mm, respectively. The most common procedures in the triple-port group were right upper lobectomy (30.8%) and left lower lobectomy (30.8%). In the single-port group, the most common procedure was right lower lobectomy (46.2%). In both groups, adenocarcinoma was the most common type of cancer (73.1% in the triple-port group and 65.4% in the single-port group). The percentage of stage I lung cancer was 76.9% in the triple-port group and 65.4% in the single-port group (Table 2).
Table 2.
Histopathological factors after propensity score matching
| Variable | Triple port (N=26) | Single port (N=26) | p-value |
|---|---|---|---|
| Tumor size (mm) | 23.2±9.4 (7–46) | 23.2±14.8 (6–65) | 0.772 |
| Location of cancer | 0.198 | ||
| Right upper lobe | 8 (30.8) | 5 (19.2) | |
| Right middle lobe | 0 | 1 (3.8) | |
| Right lower lobe | 5 (19.2) | 12 (46.2) | |
| Left upper lobe | 5 (19.2) | 4 (15.4) | |
| Left lower lobe | 8 (30.8) | 4 (15.4) | |
| Type of cancer | 0.555 | ||
| Adenocarcinoma | 19 (73.1) | 17 (65.4) | |
| Squamous cell carcinoma | 7 (26.9) | 8 (30.8) | |
| Adenosquamous carcinoma | 0 | 1 (3.8) | |
| Large cell cancer | 0 | 0 | |
| Pathologic stage | 0.363 | ||
| Stage Ia | 13 (50.0) | 11 (42.3) | |
| Stage Ib | 7 (26.9) | 6 (23.1) | |
| Stage IIa | 5 (19.2) | 6 (23.1) | |
| Stage IIb | 0 | 3 (11.5) | |
| Stage IIIa | 1 (3.8) | 0 |
Values are presented as mean±standard deviation (range) or number (%).
In terms of operative factors, the operative time and intraoperative bleeding in the triple-port group and single-port group were similar (189.4±50.8 minutes versus 205.4±50.6 minutes, p=0.259; 286.5±312.9 mL versus 314.6±513.1 mL, p=0.813). The numbers of resected lymph nodes in the triple-port group and the single-port group were 10.8±10.3 and 11.1±4.3, respectively (p=0.889). The mean number of nodal stations explored in the triple-port group and the single-port group was 2.8±1.2 and 3.6±1.2, respectively (p=0.020). The mean number of mediastinal lymph node stations in the triple-port group and the single-port group was 1.2±0.5 and 1.7±0.6, respectively (p=0.011) (Table 3). The rate of conversion to open thoracotomy was 7.7% in the triple-port group and 3.8% (p=0.100) in the single-port group. In the single-port group, conversion to multiple-port lobectomy (2- or 3-port lobectomy) occurred in 3 patients (11.5%) (Table 3).
Table 3.
Postoperative outcomes related to major lung resection after propensity score matching
| Variable | Triple port (N=26) | Single port (N=26) | p-value |
|---|---|---|---|
| Operative time (min) | 189.4±50.8 | 205.4±50.6 | 0.259 |
| Blood loss (mL) | 286.5±312.9 | 314.6±513.1 | 0.813 |
| Pleural adhesion | 3 | 4 | 1.000 |
| Incomplete fissure | 11 | 10 | 0.777 |
| Postoperative complications | |||
| Prolonged air leak (>5 day) | 2 (7.7) | 2 (7.7) | 1.000 |
| Pneumonia | 1 (3.8) | 0 | 1.000 |
| Bronchopleural fistula | 1 (3.8) | 1 (3.8) | 1.000 |
| No. of dissected lymph nodes | 10.8±10.3 | 11.1±4.3 | 0.889 |
| No. of dissected lymph node regions | 2.8±1.2 | 3.6±1.2 | 0.020 |
| No. of dissected mediastinal lymph nodes | 1.2±0.5 | 1.7±0.6 | 0.011 |
| Hospital stay after lobectomy (day) | 11.7±6.1 | 9.5±6.4 | 0.226 |
| Duration of chest tube (day) | 8.7±5.1 | 6.2±6.6 | 0.130 |
| Conversion rate | |||
| To open thoracotomy | 2 (7.7) | 1 (3.8) | 1.000 |
| To multiport | 3 (11.5) | ||
Values are presented as mean±standard deviation or number (%).
A prolonged air leak was defined as an air leak for over 5 days after the lobectomy. Prolonged air leak developed in 7.7% of patients in both groups (p= 1.000). One case of bronchopleural fistula occurred in each group. In both groups, the hospital stay after lobectomy and chest drain duration were shorter in the single-port group than in the triple-port group (9.5±6.4 days versus 11.7±6.1 days, p=0.226; 6.2±6.6 days versus 8.7±5.1 days, p=0.130). However, the differences were not statistically significant. Postoperative pneumonia occurred in 1 patient in the triple-port group. There were no cases of postoperative bleeding, morbidity, or mortality in either group (Table 3).
Discussion
VATS lobectomy was introduced in 1992. Since then, VATS lobectomy has been widely practiced using 3 to 4 port incisions [9–15]. In 2011, Gonzalez et al. [1] reported the first successful VATS lobectomy using a single port. After that, good results have been reported for single-port VATS lobectomy [2–7,16]. Today, single-port VATS is also used in pneumonectomy, sleeve lobectomy, and chest wall resection procedures [17–19]. However, single-port VATS lobectomy is performed only in a limited number of hospitals in several countries due to its technical difficulty. In this study, the safety and effectiveness of triple-port and single-port VATS lobectomy were compared retrospectively.
The results of this study revealed that the operative time and intraoperative bleeding for both groups were similar (189.4±50.8 minutes versus 205.4±50.6 minutes, p=0.259; 286.5±312.9 mL versus 314.6±513.1 mL, p=0.813). In addition, the rates of conversion to open thoracotomy in the triple-port and single-port groups were similar (7.7% versus 3.8%, p=1.000). These results indicate that the safety and efficacy of single-port and triple-port VATS lobectomy procedures were similar. Other studies have similarly indicated that the operative time, intraoperative bleeding, and rate of conversion to open thoracotomy in triple- and single-port VATS lobectomies were similar [3–7,20]. Those studies reported that the operative time and intraoperative bleeding of the single-port group were 154.1 to 198.8 minutes and 38.4 to 99.1 mL, respectively [4–7].
Regarding the results of dissection for mediastinal lymph nodes, the single-port group had better outcomes than the triple-port group. This indicates that the dissection of mediastinal lymph nodes via single-port VATS was not more difficult than in triple-port VATS. Other centers have reported that the number of dissected mediastinal lymph nodes did not significantly differ between the 2 procedures [2–4].
After lobectomy, the occurrence of complications was not different between the 2 groups (Table 3). In addition, the recovery period in both groups was similar. This suggests that single-port VATS lobectomy is not more traumatic than triple-port VATS lobectomy.
This study has several limitations. First, the operator effort could affect the number of excised mediastinal lymph nodes. Starting in 2015, the Department of Health Insurance Review and Assessment Service in Republic of Korea has recommended performing mediastinal lymph node biopsy in more than 2 mediastinal lymph node areas for lobectomy in lung cancer patients. Thus, the surgeon responsible for the procedures analyzed in this study endeavored to comply with that recommendation. This change might have made a difference in the results for the 2 groups. In other reports, the numbers of excised mediastinal lymph nodes were similar in both groups [2–4]. Second, this study included no long-term follow-up data after single-port VATS lobectomy on oncologic factors such as recurrence of cancer or survival rate. After accumulating long-term data for single-port VATS, these results will be reported. Third, we performed triple- and single-port VATS lobectomy in different periods. There may have been differences in the devices used and in the accumulated experience of the surgeon. This might have resulted in research or intentional bias between the 2 groups.
Because single-port VATS lobectomy is a relatively new procedure, there is still not enough evidence to support its superiority to triple-port VATS for lobectomy. However, more results on single-port VATS lobectomy are being reported and the number of thoracic surgeons performing single-port VATS lobectomy is increasing. As a result, for a thoracic surgeon with experience in thoracoscopic surgery, single-port lobectomy is an effective and feasible option.
In conclusion, our experience showed that single-port VATS lobectomy and triple-port VATS lobectomy had similar safety and efficacy. This indicates that single-port VATS lobectomy is a feasible and safe option for lung cancer patients.
Acknowledgments
This study was supported by a Grant of the Samsung Vein Clinic Network (Daejeon, Anyang, Cheongju, Cheonan; Fund no. KTCS04-084).
Footnotes
Conflict of interest
No potential conflicts of interest relevant to this article are reported.
References
- 1.Gonzalez D, de la Torre M, Paradela M, et al. Video-assisted thoracic surgery lobectomy: 3-year initial experience with 200 cases. Eur J Cardiothorac Surg. 2011;40:e21–8. doi: 10.1016/j.ejcts.2011.02.051. [DOI] [PubMed] [Google Scholar]
- 2.Shen Y, Wang H, Feng M, Xi Y, Tan L, Wang Q. Single- versus multiple-port thoracoscopic lobectomy for lung cancer: a propensity-matched study. Eur J Cardiothorac Surg. 2016;49(Suppl 1):i48–53. doi: 10.1093/ejcts/ezv358. [DOI] [PubMed] [Google Scholar]
- 3.Han KN, Kim HK, Choi YH. Comparison of single port versus multiport thoracoscopic segmentectomy. J Thorac Dis. 2016;8(Suppl 3):S279–86. doi: 10.3978/j.issn.2072-1439.2016.02.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhu Y, Liang M, Wu W, et al. Preliminary results of single-port versus triple-port complete thoracoscopic lobectomy for non-small cell lung cancer. Ann Transl Med. 2015;3:92. doi: 10.3978/j.issn.2305-5839.2015.03.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg. 2013;95:426–32. doi: 10.1016/j.athoracsur.2012.10.070. [DOI] [PubMed] [Google Scholar]
- 6.Hirai K, Takeuchi S, Usuda J. Single-port video-assisted thoracic surgery for early lung cancer: initial experience in Japan. J Thorac Dis. 2016;8(Suppl 3):S344–50. doi: 10.3978/j.issn.2072-1439.2016.02.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang BY, Tu CC, Liu CY, Shih CS, Liu CC. Single-incision thoracoscopic lobectomy and segmentectomy with radical lymph node dissection. Ann Thorac Surg. 2013;96:977–82. doi: 10.1016/j.athoracsur.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 8.Kang DK, Min HK, Jun HJ, Hwang YH, Kang MK. Single-port video-assisted thoracic surgery for lung cancer. Korean J Thorac Cardiovasc Surg. 2013;46:299–301. doi: 10.5090/kjtcs.2013.46.4.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daniels LJ, Balderson SS, Onaitis MW, D’Amico TA. Thoracoscopic lobectomy: a safe and effective strategy for patients with stage I lung cancer. Ann Thorac Surg. 2002;74:860–4. doi: 10.1016/S0003-4975(02)03764-5. [DOI] [PubMed] [Google Scholar]
- 10.Swanson SJ, Herndon JE, 2nd, D’Amico TA, et al. Video-assisted thoracic surgery lobectomy: report of CALGB 39802: a prospective, multi-institution feasibility study. J Clin Oncol. 2007;25:4993–7. doi: 10.1200/JCO.2007.12.6649. [DOI] [PubMed] [Google Scholar]
- 11.McKenna RJ, Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg. 2006;81:421–5. doi: 10.1016/j.athoracsur.2005.07.078. [DOI] [PubMed] [Google Scholar]
- 12.Hansen HJ, Petersen RH. A video-atlas of video-assisted thoracoscopic lobectomy using a standardized three-port anterior approach. Ann Cardiothorac Surg. 2012;1:104. doi: 10.3978/j.issn.2225-319X.2012.04.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg. 2004;77:726–8. doi: 10.1016/S0003-4975(03)01219-0. [DOI] [PubMed] [Google Scholar]
- 14.Landreneau RJ, Mack MJ, Hazelrigg SR, et al. Video-assisted thoracic surgery: basic technical concepts and intercostal approach strategies. Ann Thorac Surg. 1992;54:800–7. doi: 10.1016/0003-4975(92)91040-G. [DOI] [PubMed] [Google Scholar]
- 15.Roviaro G, Rebuffat C, Varoli F, Vergani C, Mariani C, Maciocco M. Videoendoscopic pulmonary lobectomy for cancer. Surg Laparosc Endosc. 1992;2:244–7. [PubMed] [Google Scholar]
- 16.Wang BY, Liu CY, Hsu PK, Shih CS, Liu CC. Single-incision versus multiple-incision thoracoscopic lobectomy and segmentectomy: a propensity-matched analysis. Ann Surg. 2015;261:793–9. doi: 10.1097/SLA.0000000000000712. [DOI] [PubMed] [Google Scholar]
- 17.Gonzalez-Rivas D, de la Torre M, Fernandez R, Garcia J. Video: single-incision video-assisted thoracoscopic right pneumonectomy. Surg Endosc. 2012;26:2078–9. doi: 10.1007/s00464-011-2127-x. [DOI] [PubMed] [Google Scholar]
- 18.Gonzalez-Rivas D, Delgado M, Fieira E, Fernandez R. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg. 2014;3:E2. doi: 10.3978/j.issn.2225-319X.2014.03.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gonzalez-Rivas D, Fernandez R, Fieira E, Mendez L. Single-incision thoracoscopic right upper lobectomy with chest wall resection by posterior approach. Innovations (Phila) 2013;8:70–2. doi: 10.1097/IMI.0b013e3182852005. [DOI] [PubMed] [Google Scholar]
- 20.Harris CG, James RS, Tian DH, et al. Systematic review and meta-analysis of uniportal versus multiportal video-assisted thoracoscopic lobectomy for lung cancer. Ann Cardiothorac Surg. 2016;5:76–84. doi: 10.21037/acs.2016.03.17. [DOI] [PMC free article] [PubMed] [Google Scholar]