Abstract
Background
Ventilator-associated pneumonia (VAP) is a common disease that may contribute to morbidity and mortality among trauma patients in the intensive care unit (ICU). This study evaluated the associations between trauma factors and the development of VAP in ventilated patients with multiple rib fractures.
Methods
We retrospectively and consecutively evaluated 101 patients with multiple rib fractures who were ventilated and managed at our hospital between January 2010 and December 2015, analyzing the associations between VAP and trauma factors in these patients. Trauma factors included sternal fracture, flail chest, diaphragm injury, traumatic aortic dissection, combined cardiac injury, pulmonary contusion, pneumothorax, hemothorax, hemopneumothorax, abbreviated injury scale score, thoracic trauma severity score, and injury severity score.
Results
Forty-six patients (45.5%) had at least 1 episode of VAP, 10 (21.7%) of whom died in the ICU. Of the 55 (54.5%) patients who did not have pneumonia, 9 (16.4%) died in the ICU. Using logistic regression analysis, we found that VAP was associated with severe lung contusion (odds ratio, 3.07; 95% confidence interval, 1.12 to 8.39; p=0.029).
Conclusion
Severe pulmonary contusion (pulmonary lung contusion score 6–12) is an independent risk factor for VAP in ventilated trauma patients with multiple rib fractures.
Keywords: Ventilator-associated pneumonia, Thoracic injuries, Wounds and injuries, Injuries
Introduction
Hospital-acquired infections (HAI) are infections acquired in hospitals and other healthcare facilities. HAIs are common complications among patients admitted to intensive care units (ICUs), especially those requiring endotracheal intubation with mechanical ventilation [1]. Ventilator-associated pneumonia (VAP) results from an invasion of the lower respiratory tract and lung parenchyma by microorganisms. It is defined as pneumonia occurring more than 48 hours after intubation and mechanical ventilation with radiologic evidence of new or progressive infiltrates, laboratory detection of the causative agent, and symptomatic evidence of systemic infection [2].
Green et al. [3] reported a high incidence of pulmonary infection in patients with multiple trauma that was attributable to a decrease in the efficacy of immune defense mechanisms. Upper airway colonization, trauma requiring surgical treatment, immunosuppression by sedative drugs, or excessive bleeding due to multiple trauma can reduce the immune defense functions [3]. Previous studies found that scoring systems reflecting the severity of trauma, such as the injury severity score (ISS), the thoracic trauma severity score (TTSS), and the rib score, were independent risk factors for the development of pneumonia. In addition, multiple studies have shown that pulmonary contusion and sternal fracture increase the risk of developing pneumonia [4–6]. However, the incidence of pneumonia and the related risk factors in cases of multiple trauma are still under debate, especially for patients with multiple rib fractures who require mechanical ventilation. Therefore, the present study evaluated the association between trauma factors and the development of VAP in ventilated patients with multiple rib fractures.
Methods
1) Study population
This retrospective study was approved by the institutional review board of the Gyeongsang National University Hospital (GNUH 2016-10-028-003). We retrospectively and consecutively evaluated all patients with multiple rib fractures who required mechanical ventilation in the ICU; all patients were admitted at a single center between January 2010 and December 2015. We identified 110 trauma patients who received mechanical ventilation. We excluded patients who died within 48 hours of injury, those who were discharged from the ICU within 24 hours, those who had single rib fractures, and those who had stab injuries. Based on these criteria, 9 patients were excluded, and 101 ventilated patients were finally included in our study. Data extracted from the medical records included demographic characteristics, mechanism of injury, number and laterality of rib fractures, associated injuries, rib score, TTSS, ISS, clinical course, and outcomes.
2) Definitions
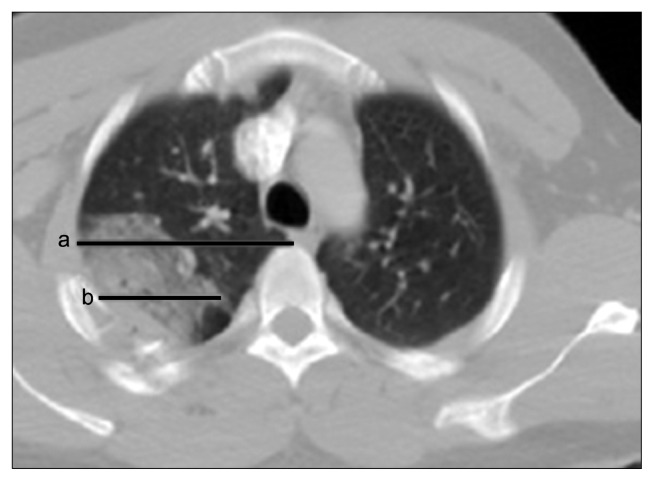
We defined multiple rib fractures as more than 3 fractures of the ribs. Pulmonary contusion was categorized into 3 levels of severity based on a scoring system. We calculated 2 lengths (a and b) after dividing both lungs into the following 4 areas: right upper plus right middle lobe, right lower lobe, left upper lobe, and left lower lobe. ‘a’ was the length of the transverse axis of the lung, with the largest area of pulmonary contusion visualized and measured by means of computed tomography (CT) of the chest. ‘b’ was the length of the longest pulmonary contusion. The pulmonary contusion score (PCS) for a lobe was calculated as (b/a)×3. We rounded up fractions of 0.5 or greater to the next whole-number unit (Fig. 1) and summed the scores of the lobes. The total PC S was then defined as mild (0–2), moderate (3–5), or severe (6–12) [7].
Fig. 1.
The PCS. The PCS is determined by summing each of the lengths (a and b). a: The length of the transverse axis of the lobe with the largest pulmonary contusion visualized by computed tomography of the chest. b: The length of the longest pulmonary contusion. PCS of 1 lobe=(b/a)×3. Fractions of 0.5 and higher were rounded up to the nearest whole number. PCS, pulmonary contusion score.
The ISS is an anatomic scoring system that provides an overall score for patients with multiple injuries. Each injury is assigned an abbreviated injury scale (AIS) score and is associated with 1 of the following 6 body regions: head, face, chest, abdomen, extremities (including the pelvis), and external. Only the highest AIS score in each body region is used. The sum of the squares of the 3 most severely injured body regions is then used to calculate the ISS [8]. The TTSS combines the patient’s age, resuscitation parameters, and radiologic assessment of thoracic trauma (Table 1) [6].
Table 1.
The thoracic trauma severity score
| Grade | Sa) | Rib fractures | Contusion | Pleural involvement | Age (yr) | Points |
|---|---|---|---|---|---|---|
| 0 | 400≤S | 0 | None | None | <30 | 0 |
| I | 300≤S<400 | 1–3 | 1 lobe, unilateral | PTX | 30–41 | 1 |
| II | 200≤S<300 | >4 | Unilobar bilateral or bilobar unilateral | HTX/HPTX unilateral | 42–54 | 2 |
| II | 150≤S<200 | >3 bilateral | <2 lobes bilateral | HTX/HPTX bilateral | 55–70 | 3 |
| IV | S<150 | Flail chest | ≥2 lobes bilateral | TPTX | >70 | 5 |
For calculation of the total score, all categories are summed. The score can range from 0 to 25.
PTX, pneumothorax; HTX, hemothorax; HPTX, hemopneumothorax; TPTX, tension pneumothorax.
S is PaO2/FiO2.
The patients with pneumonia satisfied all of the following criteria: (1) core temperature >38.3°C; (2) a white blood cell count >10.0×109/L; (3) purulent tracheobronchial secretions; (4) worsening of pulmonary gas exchange levels; and (5) persistence of pulmonary infiltrates on radiographic images (>24 hours) [9]. VAP was defined as pneumonia occurring more than 48 hours after intubation and initiation of mechanical ventilation with radiologic evidence of new or progressive infiltrates, laboratory detection of a causative agent, and symptomatic evidence of systemic infection [2,4].
3) Treatment
Endotracheal intubation was performed in patients with at least 1 of the following 5 indications: (1) inability to maintain airway patency; (2) inability to protect the airway against aspiration; (3) ventilator compromise; (4) failure to adequately oxygenate pulmonary capillary blood; and (5) anticipation of a deteriorating course that would eventually lead to the inability to maintain airway patency or protection [10]. All patients received prophylactic antibiotics. The most commonly used antibiotics were second-generation cephalosporins, such as cefotiam. We used additional antibiotics for other conditions, such open wounds, and as a surgical prophylaxis.
4) Data analysis
Missing data were not replaced or imputed. We calculated p-values using the Fisher exact test or the Pearson chi-square test for categorical variables and used the Mann-Whitney U-test for continuous variables. Significance was set at p<0.05. To evaluate the risk factors for a poor outcome, we used logistic regression analysis. In the multivariate model of efficacy, we included relevant variables with p<0.10 in the univariate analysis. We calculated associations between the variables included in the multivariate analysis, with significance set at p<0.05. All statistical analyses were performed using IBM SPSS software ver. 24.0 (IBM Corp., Armonk, NY, USA).
Results
Between January 2010 and December 2015, Gyeongsang National University Hospital provided mechanical ventilation to 101 patients with multiple rib fractures. The median age of the patients was 66 years, and the majority of patients were male (80.2%). Fifty-three patients (52.5%) were smokers or ex-smokers (the latter group had not smoked within the last 1 year), and 13 patients (12.9%) had a history of lung disease: 4 (4%) had chronic obstructive lung disease, 8 (7.9%) had asthma, and 1 (1.0%) had pulmonary tuberculosis. Motor vehicle collisions were the main cause of trauma (79.2%), and included car (23.8%), motorcycle (19.8%), pedestrian (18.8%), and cultivator (16.8%) accidents. Overall, 63 patients (62.4%) had bilateral rib fractures, and the median number of rib fractures was 10. Of the 101 patients in the study, 46 (45.5%) developed pneumonia (the VAP group) and 55 (54.5%) did not (the non-VAP group). There were no significant differences in age or sex between the groups. Additionally, the mechanisms of trauma and the mean number of rib fractures was not significantly different between the groups (Table 2).
Table 2.
Demographic and clinical characteristics of patients with multiple rib fractures receiving mechanical ventilation
| Characteristic | Total (n=101) | No pneumonia (n=55) | Pneumonia (n=46) | p-value |
|---|---|---|---|---|
| Age (yr) | 66 (50–74) | 61 (43–75) | 68 (45–74) | 0.179 |
| Male sex | 81 (80.2) | 44 (80) | 37 (80.4) | 0.956 |
| Smoking | 53 (52.5) | 28 (50.9) | 25 (54.3) | 0.842 |
| Comorbidity | ||||
| Chronic obstructive pulmonary disease | 4 (4) | 1 (1.8) | 3 (6.5) | 0.328 |
| Asthma | 8 (7.9) | 4 (7.3) | 4 (8.7) | 1 |
| Tuberculosis | 1 (1) | 0 | 1 (2.2) | 0.455 |
| Mechanism of trauma | ||||
| Motor vehicle collision | 80 (79.2) | 42 (76.4) | 38 (82.6) | 0.472 |
| Car accident | 24 (23.8) | 12 (21.8) | 12 (26.1) | 0.645 |
| Pedestrian | 19 (18.8) | 11 (20) | 8 (17.4) | 0.471 |
| Motorcycle | 20 (19.8) | 13 (23.6) | 7 (15.2) | 0.211 |
| Cultivator | 17 (16.8) | 6 (10.9) | 11 (23.9) | 0.11 |
| Falls | 21 (20.8) | 13 (23.6) | 8 (17.4) | 0.472 |
| No. of fractures | 10 (5–14) | 10 (6–14) | 9 (5–13) | 0.547 |
| Bilateral rib fractures | 63 (62.4) | 37 (67.3) | 26 (56.5) | 0.306 |
Values are presented as median (interquartile range) or number (%). All p-values were calculated using the Fisher exact test or the Pearson chi-square test for categorical variables and the Mann-Whitney U-test, as appropriate.
The differences in individual trauma factors between the VAP and control groups were studied. We assessed sternal fracture, flail chest, diaphragm injury, traumatic aortic dissection, combined cardiac injury, pulmonary contusion, pneumothorax, hemothorax, hemopneumothorax, AIS score, TTSS, and ISS. Sternal fractures were noted in 18 patients (17.8%), flail chest in 75 patients (74.3%), and pulmonary contusion in 101 patients (100%). Traumatic diaphragm injury was noted in 5 patients (5%), all of whom underwent surgical repair. Seven patients (6.9%) had traumatic aortic dissection; 3 of these patients underwent thoracic endovascular aortic repair once their condition was suitable (1–2 weeks post-injury). Three patients (3%) sustained traumatic heart injuries: 1 had a traumatic tricuspid injury, 1 had a traumatic aortic valve injury, and 1 had a ruptured left atrium. Pneumothorax was noted in 80 patients (79.2%), hemothorax in 94 patients (93.1%), and hemopneumothorax in 77 patients (76.2%). The most commonly combined injuries were external, extremity, abdomen, face, and head and neck injuries. Emergency neurosurgery due to intracranial hemorrhage was performed in 24 patients (23.8%). Thirteen patients (12.9%) underwent emergency abdominal surgery. Emergency embolization was performed in 25 patients (24.8%) due to hepatic (n=10 [9.9%]), splenic (n=7 [6.9%]), or retroperitoneal (n=9 [8.9%]) injury. Severe pulmonary contusion (p=0.046) and the ISS (p<0.001) were the only trauma factors that differed significantly between the VAP and control groups (Table 3).
Table 3.
Intrathoracic injuries, combined injuries, AIS score, TTSS, and ISS of patients with multiple rib fractures receiving mechanical ventilation
| Characteristic | Total (n=101) | No pneumonia (n=55) | Pneumonia (n=46) | p-value |
|---|---|---|---|---|
| Sternal fracture | 18 (17.8) | 14 (25.5) | 9 (19.6) | 0.634 |
| Flail chest | 75 (74.3) | 40 (72.7) | 35 (76.1) | 0.82 |
| Bilateral | 51 (50.5) | 31 (56.4) | 20 (43.5) | 0.233 |
| Diaphragm injury | 5 (5) | 4 (7.3) | 1 (2.2) | 0.373 |
| Traumatic aortic dissection | 7 (6.9) | 4 (7.3) | 3 (6.5) | 1 |
| Combined cardiac injury | 10 (9.9) | 4 (7.3) | 6 (13) | 0.506 |
| Pulmonary contusiona) | 101 (100) | 55 (100) | 46 (100) | 1 |
| Mild | 24 (23.8) | 16 (29.1) | 8 (17.4) | 0.241 |
| Moderate | 25 (24.8) | 16 (29.1) | 9 (19.6) | 0.356 |
| Severe | 52 (51.5) | 23 (41.8) | 29 (63) | 0.046 |
| Pneumothorax+ | 80 (79.2) | 44 (80) | 36 (78.3) | 1 |
| Hemothorax | 94 (93.1) | 50 (90.9) | 44 (95.7) | 0.45 |
| Hemopneumothorax | 77 (76.2) | 41 (74.5) | 36 (78.3) | 0.815 |
| Both hemopneumothorax | 21 (20.8) | 10 (18.2) | 11 (23.9) | 0.623 |
| Other site injuries | ||||
| Head and neck | 52 (51.5) | 29 (52.7) | 23 (50) | 0.843 |
| Face | 65 (64.4) | 37 (67.3) | 28 (60.9) | 0.537 |
| Abdomen | 82 (71.3) | 45 (81.8) | 37 (80.4) | 0.859 |
| Extremity | 82 (81.2) | 45 (81.8) | 37 (80.4) | 1 |
| External | 89 (88.1) | 48 (87.3) | 41 (89.1) | 1 |
| AIS score | ||||
| Head and neck | 1 (0–3) | 2 (0–3) | 1 (0–4) | 0.746 |
| Face | 1 (0–1) | 1 (0–1) | 1 (0–1) | 0.635 |
| Thorax | 4 (3–5) | 4 (3–5) | 4 (3–5) | 0.539 |
| Abdomen | 3 (1–4) | 2 (1–3) | 3 (2–4) | 0.067 |
| Extremity | 2 (1–3) | 2 (2–3) | 2 (1–3) | 0.795 |
| External | 1 (1–2) | 1 (1–2) | 1 (1–2) | 0.775 |
| TTSS | 20 (18–23) | 21 (17–23) | 20 (19–24) | 0.056 |
| ISS | 36 (29–42) | 34 (29–38) | 38 (33–43) | <0.001 |
Values are presented as median (interquartile range) or number (%).
AIS, abbreviated injury scale; TTSS, thoracic trauma severity score; ISS, injury severity score.
Categorized into 3 levels of severity based on the pulmonary contusion scoring system: mild, 0–2 moderate, 3–5 severe, 6–12.
Patients with suspected VAP were initially treated with ceftriaxone or an antimicrobial agent such as a respiratory fluoroquinolone, ampicillin/sulbactam, or meropenem. Bronchoalveolar lavage fluid and blood culture specimens were obtained from patients with suspected VAP. The causative organisms identified from these specimens were Staphylococcus aureus (45.7%), Acinetobacter baumanii (21.7%), Klebsiella pneumoniae (13%), Pseudomonas aeruginosa (13%), Candida albicans (4.3%), and Staphylococcus epidermidis (2.2%) (Table 4). When a causative organism was identified, the administered antibiotic treatment was appropriately modified upon consultation with specialist physicians.
Table 4.
Organism causing ventilator-associated pneumonia in patients with multiple rib fractures receiving mechanical ventilation (n=46)
| Causative organism | No. of patients (%) |
|---|---|
| Staphyloccocus aureus | 21 (45.7) |
| Acinetobactor baumanii | 10 (21.7) |
| Klebsiella pneumoniae | 6 (13) |
| Pseudomonas aeruginosa | 6 (13) |
| Candida albicans | 2 (4.3) |
| Staphyloccocus epidermidis | 1 (2.2) |
Generally, patients in the VAP group had longer hospital stays than those in the control group. Additionally, the duration of the ICU stay (p=0.002) and the duration of mechanical ventilation (p<0.001) were significantly longer in the VAP group than in the control group. We assessed complications, such as acute respiratory distress syndrome, acute renal failure, gastrointestinal bleeding, atrial fibrillation, and disseminated intravascular coagulation. Overall, the rate of complications was higher in the VAP group than in the control group; however, the difference was not significant. The mortality rate was defined as the rate of all-cause mortality, and it was comparable between the 2 groups (Table 5).
Table 5.
Clinical course and outcomes of patients with multiple rib fractures receiving mechanical ventilation
| Risk factors | Total (n=101) | No pneumonia (n=55) | Pneumonia (n=46) | p-value |
|---|---|---|---|---|
| Intensive care unit stay (day) | 15 (6–24) | 14 (5–20) | 18 (8–27) | 0.002 |
| Hospital stay (day) | 44 (20–83) | 34 (13–65) | 46 (27–61) | 0.054 |
| Duration of mechanical ventilation use (day) | 15 (6–24) | 11 (4–17) | 18 (9–36) | <0.001 |
| Tracheostomy | 50 (49.5) | 22 (40) | 28 (60.9) | 0.046 |
| Closed thoracotomy | 94 (93.1) | 50 (90.9) | 44 (95.7) | 0.45 |
| Transfusion | 80 (79.2) | 34 (73.9) | 46 (83.6.4) | 0.137 |
| Mortality | 19 (18.8) | 9 (16.4) | 10 (21.7) | 0.491 |
| Complications | ||||
| Acute respiratory distress syndrome | 5 (5) | 2 (3.6) | 3 (6.5) | 0.657 |
| Acute renal failure | 19 (18.8) | 8 (14.5) | 11 (23.9) | 0.308 |
| Gastrointestinal bleeding | 4 (4) | 2 (3.6) | 2 (4.3) | 1 |
| New onset atrial fibrillation | 7 (6.9) | 2 (3.6) | 2 (4.3) | 1 |
| Disseminated intravascular coagulation | 4 (4) | 1 (1.8) | 3 (6.5) | 0.328 |
Values are presented as median (interquartile range) or number (%).
Univariate logistic regression analysis revealed that the development of VAP was significantly associated with severe pulmonary contusion and the ISS. The odds of VAP were 2.4 times higher in patients with severe pulmonary contusion than in those without, and the odds were 2.2 times higher in patients with a high ISS than those with a low ISS. Age, sex, mechanism of trauma, number of rib fractures, thoracic injuries other than severe pulmonary contusion, and other sites of injury were not significantly associated with VAP. Multivariate logistic regression analysis confirmed that the development of VAP was independently associated with severe pulmonary contusion (odds ratio [OR], 3.07; 95% confidence interval [CI], 1.12 to 8.39; p=0.029) (Table 6).
Table 6.
Logistic regression analysis of the risk factors for patients with multiple rib fractures receiving mechanical ventilation (n=101)
| Risk factors | Univariate | Multivariate | ||
|---|---|---|---|---|
|
|
|
|||
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Age | 2 (0.89–4.38) | 0.093 | 2.06 (0.75–5.68) | 0.163 |
|
| ||||
| Male sex | 1.03 (0.38–2.75) | 0.956 | ||
|
| ||||
| Mechanism of trauma | ||||
|
| ||||
| Motor vehicle collision | 1.47 (0.55–3.93) | 0.443 | ||
|
| ||||
| Car accident | 1.27 (0.51–3.17) | 0.616 | ||
|
| ||||
| Pedestrian | 0.84 (0.31–2.31) | 0.738 | ||
|
| ||||
| Motorcycle | 0.58 (0.21–1.6) | 0.294 | ||
|
| ||||
| Cultivator | 2.57 (0.87–7.6) | 0.089 | 1.97 (0.54–7.21) | 0.307 |
|
| ||||
| Falls | 0.68 (0.25–1.82) | 0.443 | ||
|
| ||||
| Rib fractures >10 | 0.83 (0.37–1.84) | 0.647 | ||
|
| ||||
| Both rib fractures | 0.63 (0.28–1.42) | 0.268 | ||
|
| ||||
| Sternal fracture | 0.71 (0.28–1.84) | 0.483 | ||
|
| ||||
| Pulmonary contusion | ||||
|
| ||||
| Mild | 0.51 (0.2–1.33) | 0.173 | ||
|
| ||||
| Moderate | 0.59 (0.23–1.51) | 0.272 | ||
|
| ||||
| Severe | 2.37 (1.06–5.3) | 0.035 | 3.07 (1.12–8.39) | 0.029 |
|
| ||||
| Pneumothorax | 0.9 (0.34–2.36) | 0.83 | ||
|
| ||||
| Hemothorax | 2.2 (0.41–11.91) | 0.36 | ||
|
| ||||
| Hemopneumothorax | 1.23 (0.49–3.11) | 0.662 | ||
|
| ||||
| Bilateral | 1.41 (0.54–3.71) | 0.481 | ||
|
| ||||
| Other site injuries | ||||
|
| ||||
| Head and neck | 0.88 (0.41–1.97) | 0.785 | ||
|
| ||||
| Face | 0.76 (0.33–1.71) | 0.504 | ||
|
| ||||
| Abdomen | 0.91 (0.34–2.48) | 0.859 | ||
|
| ||||
| Extremity | 0.91 (0.34–2.48) | 0.86 | ||
|
| ||||
| External | 1.2 (0.35–4.05) | 0.774 | ||
|
| ||||
| Tracheostomy | 2.33 (1.05–5.2) | 0.038 | 2.42 (0.96–6.12) | 0.061 |
|
| ||||
| Transfusion | 2.11 (0.795–5.58) | 0.134 | ||
|
| ||||
| Intensive care unit stay >15 days | 1.95 (0.88–4.32) | 0.099 | 1.64 (0.64–4.16) | 0.302 |
|
| ||||
| TTSS >20 | 2.2 (0.98–4.91) | 0.053 | 1.26 (0.44–3.59) | 0.663 |
|
| ||||
| ISS >36 | 2.25 (1–5.04) | 0.049 | 2.15 (0.87–5.32) | 0.096 |
Multivariate analysis includes variables with significant associations in univariate analysis (p<0.1). Boldface indicates significant differences in statistical comparisons of baseline characteristics. Age, number of rib fractures, duration of mechanical ventilation, TTSS, and ISS are divided into 2 groups based on the median value.
OR, odds ratio; CI, confidence interval; TTSS, thorax trauma severity score; ISS, injury severity score.
Discussion
Trauma is a major public health problem worldwide; it is associated with high morbidity and mortality. Thoracic trauma accounts for 10% to 15% of all trauma [11]. Chest injuries can pose a threat to the airway, circulation, and breathing and can thus directly affect the patient’s clinical course and outcome. Additionally, thoracic trauma has been reported to be the leading cause of death, hospitalization, and long-term disability in the first 4 decades of life. In the United States and Europe, 20% to 25% of deaths occurring in polytrauma patients are attributed to chest injuries [12]. Rib fractures are a major part of chest trauma, and each additional rib fracture is associated with a 19% increase in the odds of mortality and a 27% increase in the odds of developing pneumonia [13]. Critically injured trauma patients admitted to the ICU are at risk of death, not only because of their critical status but also because of secondary conditions, such as VAP. VAP is the second-most common nosocomial infection occurring in critically ill patients in the ICU, affecting 27% of such patients [14]. We believe that identifying the trauma factors associated with pneumonia in patients with multiple rib fractures receiving mechanical ventilation is important for improving their prognosis.
We analyzed the association between various trauma factors, such as sternal fracture, pulmonary contusion, pneumothorax, hemothorax, hemopneumothorax, combination injuries, and ISS—all of which indicate trauma severity—and the development of pneumonia in ventilated patients with multiple rib fractures. In accordance with previous studies on VAP in trauma patients, the mechanism of infection involves upper-airway colonization, trauma lesions requiring surgical treatment, immunosuppression by sedative drugs, or excessive bleeding due to multiple trauma; the process is accelerated in trauma patients who develop pneumonia while on ventilation [3]. Rodriguez et al. [15] showed that trauma factors in ventilated patients are associated with the development of pneumonia. In trauma patients, additional variables, such as the ISS and the critical need for prehospital intubation, increase the risk of developing pneumonia [15]. Multiple previous studies have reported that trauma factors, such as pulmonary contusion, rib fracture, sternal fracture, and traumatic brain injury, increased the risk of developing pneumonia [4,5,16,17]. In the present study, the overall rate of VAP development was approximately 45.5%. We identified severe pulmonary contusion and the ISS as being statistically significant risk factors in the univariate logistic regression analysis. In the multivariate analysis, severe pulmonary contusion was identified as a risk factor for the development of pneumonia in ventilated trauma patients with multiple rib factors.
A pulmonary contusion is a contusion of the lung caused by chest trauma. As a result of damage to capillaries, blood and other fluids accumulate in lung tissue, interfering with gas exchange, potentially leading to hypoxia. Pulmonary contusions occur in approximately 20% of blunt chest trauma cases with an ISS >15. The reported mortality rate is 10% to 25%, and 40% to 60% of patients will require mechanical ventilation [18]. CT is very sensitive for the identification of pulmonary contusion and allows for 3-dimensional assessment and calculation of the size of the contusion [6,19]. However, the association between CT findings and the clinical course is still under debate. Wagner and Jamieson [19] showed that the association between CT findings and histologic results led to pulmonary contusion being considered a pulmonary laceration with blood pneumonia rather than an interstitial disease. Kim et al. [7] showed that severe pulmonary lung contusion was an independent risk factor for ICU admission. We found that severe pulmonary contusion was an independent risk factor for the development of pneumonia in ventilated trauma patients with multiple rib fractures (OR, 3.07; 95% CI, 1.12 to 8.39; p=0.029).
Pape et al. [20] developed the TTSS in 2000, based on the results of a retrospective study of 4,571 cases of blunt trauma. The TTSS incorporates data regarding a patient’s age, the resuscitation parameters, and a radiologic assessment of the thoracic trauma. After the publication of the TTSS in 2000, some studies reported an association between the TTSS and thoracic trauma–related mortality or morbidity. In 2011, Aukema et al. [6] suggested that the TTSS was useful for predicting mortality and acute respiratory distress syndrome. In 2016, Martinez Casas et al. [21] reported that the TTSS is an appropriate and feasible tool to predict the development of complications or mortality in patients with mild thoracic trauma. In the present study, the multivariate analysis showed no association between the TTSS and the odds of VAP (OR, 1.26; 95% CI, 0.44 to 3.59; p=0.663). However, in the univariate analysis, the TTSS showed a meaningful trend toward an association with VAP (p=0.053). Hence, further research on the relationship between the TTSS and the incidence of VAP is warranted.
The present study has several limitations. First, we only evaluated patients from a single hospital, which may have introduced selection bias and may limit the extrapolation of our findings to the entire population of ventilated trauma patients with multiple rib fractures. Second, our study evaluated a relatively small number of ventilated trauma patients with multiple rib fractures; thus, larger studies are needed to validate our findings. We agree that the association between pulmonary contusion and the development of VAP in trauma patients with multiple rib fractures receiving mechanical ventilation remains a controversial subject; further prospective studies are required.
Despite these limitations, this study is an important investigation of the characteristics and risk factors associated with the development of VAP in trauma patients with multiple rib fractures receiving mechanical ventilation. Our study showed that severe pulmonary contusion is an independent risk factor for the development of VAP in such patients. Comparisons of these findings with those of other reports will enhance the prediction of VAP development. Further research on the association between TTSS and the incidence of VAP is also needed. Moreover, ventilated trauma patients with multiple rib fractures and severe pulmonary contusion require close monitoring for the development of VAP.
Acknowledgments
We acknowledge the outstanding contributions of the technicians and nursing staff at the Gyeongsang National University Hospital, Korea.
This study was supported by a Grant of the Samsung Vein Clinic Network (Daejeon, Anyang, Cheongju, Cheonan; Fund no. KTCS04-081).
Footnotes
Conflict of interest
No potential conflicts of interest relevant to this article are reported.
References
- 1.O’Grady NP, Murray PR, Ames N. Preventing ventilator-associated pneumonia: does the evidence support the practice? JAMA. 2012;307:2534–9. doi: 10.1001/jama.2012.6445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36:309–32. doi: 10.1016/j.ajic.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 3.Green GM, Jakab GJ, Low RB, Davis GS. Defense mechanisms of the respiratory membrane. Am Rev Respir Dis. 1977;115:479–514. doi: 10.1164/arrd.1977.115.3.479. [DOI] [PubMed] [Google Scholar]
- 4.Byun JH, Kim HY. Factors affecting pneumonia occurring to patients with multiple rib fractures. Korean J Thorac Cardiovasc Surg. 2013;46:130–4. doi: 10.5090/kjtcs.2013.46.2.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oyetunji TA, Jackson HT, Obirieze AC, et al. Associated injuries in traumatic sternal fractures: a review of the National Trauma Data Bank. Am Surg. 2013;79:702–5. [PubMed] [Google Scholar]
- 6.Aukema TS, Beenen LF, Hietbrink F, Leenen LP. Validation of the Thorax Trauma Severity Score for mortality and its value for the development of acute respiratory distress syndrome. Open Access Emerg Med. 2011;3:49–53. doi: 10.2147/OAEM.S22802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim JJ, Shin JH, Jin W, et al. The value of grading of pulmonary contusion by the chest CT scanning. J Korean Soc Emerg Med. 2004;15:452–5. [Google Scholar]
- 8.Baker SP, O’Neill B, Haddon W, Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96. doi: 10.1097/00005373-197403000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Antonelli M, Moro ML, Capelli O, et al. Risk factors for early onset pneumonia in trauma patients. Chest. 1994;105:224–8. doi: 10.1378/chest.105.1.224. [DOI] [PubMed] [Google Scholar]
- 10.Sagarin MJ, Barton ED, Chng YM, Walls RM National Emergency Airway Registry Investigators. Airway management by US and Canadian emergency medicine residents: a multicenter analysis of more than 6,000 endotracheal intubation attempts. Ann Emerg Med. 2005;46:328–36. doi: 10.1016/j.annemergmed.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 11.Demirhan R, Onan B, Oz K, Halezeroglu S. Comprehensive analysis of 4205 patients with chest trauma: a 10-year experience. Interact Cardiovasc Thorac Surg. 2009;9:450–3. doi: 10.1510/icvts.2009.206599. [DOI] [PubMed] [Google Scholar]
- 12.Clark GC, Schecter WP, Trunkey DD. Variables affecting outcome in blunt chest trauma: flail chest vs. pulmonary contusion. J Trauma. 1988;28:298–304. doi: 10.1097/00005373-198803000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Wardhan R. Assessment and management of rib fracture pain in geriatric population: an ode to old age. Curr Opin Anaesthesiol. 2013;26:626–31. doi: 10.1097/01.aco.0000432516.93715.a7. [DOI] [PubMed] [Google Scholar]
- 14.Richards MJ, Edwards JR, Culver DH, Gaynes RP. Nosocomial infections in medical intensive care units in the United States. National Nosocomial Infections Surveillance System. Crit Care Med. 1999;27:887–92. doi: 10.1097/00003246-199905000-00020. [DOI] [PubMed] [Google Scholar]
- 15.Rodriguez JL, Gibbons KJ, Bitzer LG, Dechert RE, Steinberg SM, Flint LM. Pneumonia: incidence, risk factors, and outcome in injured patients. J Trauma. 1991;31:907–12. doi: 10.1097/00005373-199107000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Lively MW. Early onset pneumonia following pulmonary contusion: the case of Stonewall Jackson. Mil Med. 2012;177:315–7. doi: 10.7205/MILMED-D-11-00272. [DOI] [PubMed] [Google Scholar]
- 17.Odell DD, Peleg K, Givon A, et al. Sternal fracture: isolated lesion versus polytrauma from associated extra-sternal injuries: analysis of 1,867 cases. J Trauma Acute Care Surg. 2013;75:448–52. doi: 10.1097/TA.0b013e31829e227e. [DOI] [PubMed] [Google Scholar]
- 18.Cohn SM. Pulmonary contusion: review of the clinical entity. J Trauma. 1997;42:973–9. doi: 10.1097/00005373-199705000-00033. [DOI] [PubMed] [Google Scholar]
- 19.Wagner RB, Jamieson PM. Pulmonary contusion: evaluation and classification by computed tomography. Surg Clin North Am. 1989;69:31–40. doi: 10.1016/S0039-6109(16)44732-8. [DOI] [PubMed] [Google Scholar]
- 20.Pape HC, Remmers D, Rice J, Ebisch M, Krettek C, Tscherne H. Appraisal of early evaluation of blunt chest trauma: development of a standardized scoring system for initial clinical decision making. J Trauma. 2000;49:496–504. doi: 10.1097/00005373-200009000-00018. [DOI] [PubMed] [Google Scholar]
- 21.Martinez Casas I, Amador Marchante MA, Paduraru M, Fabregues Olea AI, Nolasco A, Medina JC. Thorax trauma severity score: is it reliable for patient’s evaluation in a secondary level hospital? Bull Emerg Trauma. 2016;4:150–5. [PMC free article] [PubMed] [Google Scholar]