Abstract
Objective
Describe the ocular biometric parameters and their associations in a population of cataract surgery candidates.
Methods
A cross-sectional study of 13,012 eyes of 6,506 patients was performed. Biometric parameters of the eyes were measured by optical low-coherence reflectometry. The axial length (AL), mean keratometry (K) and astigmatism, anterior chamber depth (ACD) (epithelium to lens), lens thickness (LT), and Corneal Diameter (CD) were evaluated.
Results
The mean age was 69 ± 10 years (44–99 years). Mean AL, Km, and ACD were 23.87 ± 1.55 mm (19.8–31.92 mm), 43.91 ± 1.71 D (40.61–51.14 D), and 3.25 ± 0.44 mm (2.04–5.28 mm), respectively. The mean LT was 4.32 ± 0.49 mm (2.73–5.77 mm) and the mean CD was 12.02 ± 0.46 mm (10.50–14.15 mm). The mean corneal astigmatism was 1.08 ± 0.84 D (0.00–7.58 D) and 43.5% of eyes had astigmatism ≥ 1.00 D. Male patients had longer AL and ACDs (p < .001) and flatter corneas (p < .001). In regression models considering age, gender, Km, ACD, LT, and CD, a longer AL was associated with being male and having higher ACD, LT and CD.
Conclusions
These data represent normative biometric values for the Portuguese population. The greatest predictor of ocular biometrics was gender. There was no significant correlation between age and AL, ACD, or Km. These results may be relevant in the evaluation of refractive error and in the calculation of intraocular lens power.
Introduction
With the increase in life expectancy of populations, there has been a progressive increase in the volume of cataract surgery performed worldwide, and it is the most common elective surgery in many countries. The introduction of less invasive techniques, new intraocular lenses (IOLs), and the achievement of more predictable refractive outcomes have been accompanied by an increase in patients' expectations of good visual outcome without the use of spectacles. Accurate biometric measurements are therefore essential. Knowledge of these measures is fundamental for obtaining precise calculations for the IOL power, which is primarily based on formulas derived from normative ocular biometric parameters.
It is known that ocular biometric parameters such as axial length (AL), corneal power (K), and anterior chamber depth (ACD) (corneal epithelium to anterior lens) vary with gender, age, and ethnicity, and hence are different among different populations. [1–6] Although there are many studies that describe these mean parameters in the European Caucasian population, there has been little attention to those studies carried out in Asian, Black and Hispanic populations. [1, 2] In addition, many of the published studies were conducted using contact applanation ultrasound biometry, a method limited by several measurement errors limiting its use prior to cataract surgery, particularly when premium lenses are implanted. It is known that optical biometry offers several advantages even over immersion ultrasound biometry, including its non-contact method, greater reproducibility and accuracy, and application in particular cases such as posterior staphyloma and eyes filled with silicone oil. [7, 8] Published studies of ocular biometric parameters using optical biometry are scarce, and this technology is constantly evolving and allows the evaluation of new parameters, such as measurement of the crystalline lens thickness (LT). Among various optical biometry devices available, Lenstar (Haag-Streit AG, Koeniz, Switzerland) has proved to be highly accurate in biometry measurements. [9]
There has not before been a large study of biometric values for the Portuguese population. The objective of the present study is to characterize the ocular biometric parameters and their associations in a population of cataract surgery candidates in Portugal.
Material and methods
A retrospective study of 13,012 eyes of 6,506 patients who underwent cataract surgery was performed at the Hospital da Luz in Lisbon. The study was conducted in accordance with the principles of the declaration of Helsinki, and was approved by the center’s ethics committee (Hospital da Luz ethics committee). All patients provided written informed consent.
Ocular biometric parameters, including AL, mean corneal power K and astigmatism, ACD, LT, and corneal diameter (CD) were studied by optical low-coherence reflectometry using the Lenstar LS900 (Haag-Streit AG, Köniz, Switzerland). Examinations that yielded poor quality or uncertain results were excluded as were those of patients with previous ocular surgeries. Astigmatism was studied using the automatic keratometry of the same device. Keratometry with this system demonstrated high precision and repeatability and has been shown to produce better clinical results with toric IOLs than manual keratometry. [10]
Statistical analysis
One eye was randomly chosen for each patient. The biometric data measured were entered into an Excel spreadsheet (Microsoft Office 2010; Microsoft, Redmond, WA). The statistical analysis was performed according to E9 guidelines of the ICH principles of statistics for clinical trials, using SPSS for Mac (version 21.0, Chicago, IL). The normality of the data was accessed with the Kolmogorov–Smirnov test. Since none of the studied variables had a normal distribution, nonparametric statistics were used. The Mann–Whitney U test was used for comparisons between groups. Correlations were performed using the Spearman coefficient. Regression models considering age, gender, LT, and CD were constructed to determine associations with the most relevant ocular biometric parameters (AL, ACD, and K). The results are expressed as the parameter mean value ± standard deviation (SD), and those with a value of p < .05 were considered statistically significant.
Results
Demographic data and biometric parameters
The demographic data and ocular biometric parameters of the patients are presented in Table 1.
Table 1. Demographic data and mean ocular biometric parameters in Portuguese population.
| Parameter | Mean ± SD (range) | ||
| Eyes (n) | 6,506 | ||
| Patients (n) | 6,506 | ||
| Age (years-old) Range |
69 ± 10 (44–99) |
||
| Females, n (%) | 3,721 (57.2%) | ||
| Right eyes, n (%) | 1,678 (51.6%) | ||
| Total | Males | Females | |
| Axial length (mm) ± SD Range |
23.87 ± 1.55 (19.8–31.92) |
23.99 ± 1.47 (20.03–31.92) |
23.68 ± 1.46 (19.8–29.99) |
| Mean keratometry (D) ± SD Range |
43.91 ± 1.71 (40.61–51.14) |
43.46 ± 1.11 (40.93–51.14) |
44.20 ± 1.29 (40.61–49.93) |
| Mean corneal astigmatism (D) ± SD Range |
1.08 ± 0.84 (0–7.58) |
1.09 ± 0.92 (0–7.58) |
1.12 ± 0.86 (0–6.27) |
| Anterior chamber depth (mm) ± SD Range |
3.25 ± 0.44 (2.04–5.28) |
3.30 ± 0.40 (2.06–5.42) |
3.14 ± 0.43 (2.04–4.99) |
| Lens thickness (mm) ± SD Range |
4.32 ± 0.49 (2.73–5.77) |
4.35 ± 0.49 (2.75–5.77) |
4.38 ± 0.41 (2.73–5.42) |
| Corneal diameter (mm) ± SD Range |
12.02 ± 0.46 (10.50–14.15) |
12.03 ± 0.43 (10.51–14.15) |
11.98 ± 0.49 (10.50–14.09) |
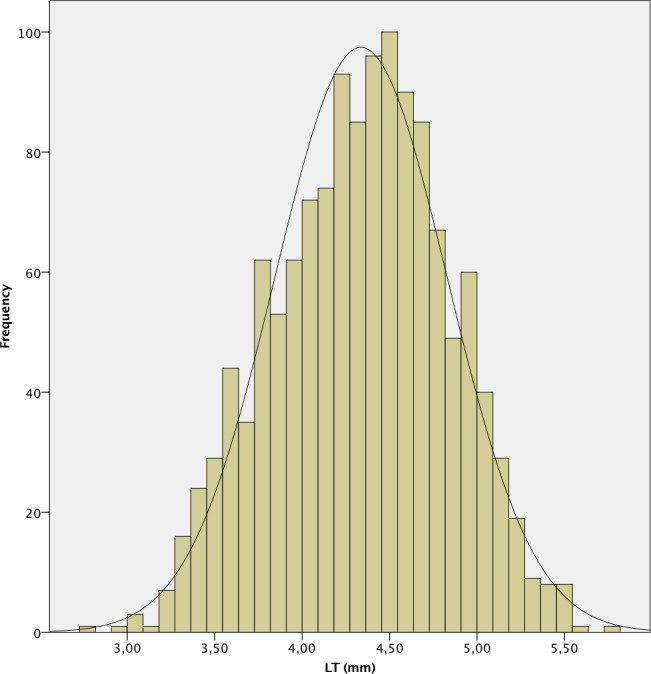
The mean AL was 23.87 ± 1.55 mm. 241 (7.4%) eyes had an AL < 22.0 mm, 2,111 (64.9%) between 22.0 and 24.5 mm, 612 (18.8%) between 24.5 and 26.0 mm and 289 (8.9%) > 26.0 mm. A positive deviation and a leptokurtic distribution (kurtosis 2.804) were observed, with a significant deviation from normality, as in the other measured parameters (p < .001 in all cases except for CD, p = .049). The histograms of the distribution of the measured values of AL, K, ACD, LT and CD are shown in Figs 1–6.
Fig 1. Histogram of axial length (AL) of the study population.
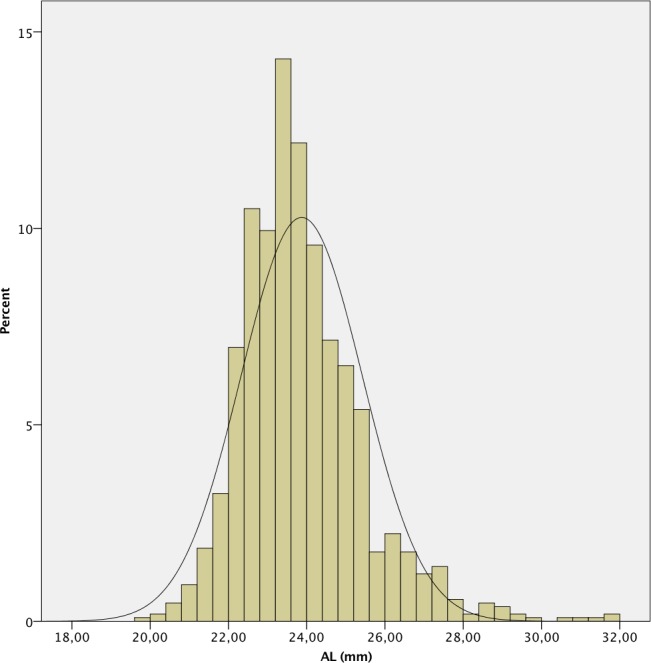
Fig 6. Histogram of corneal diameter (CD) of the study population.
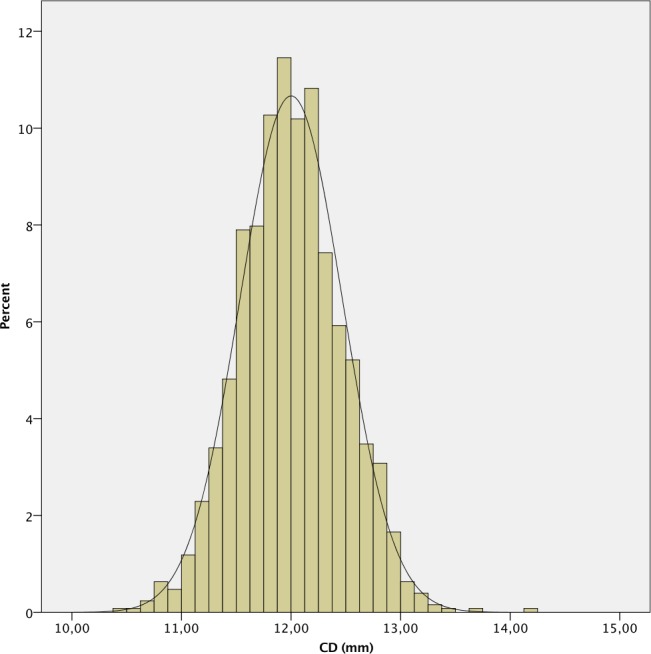
Fig 2. Histogram of mean keratometry (K) of the study population.
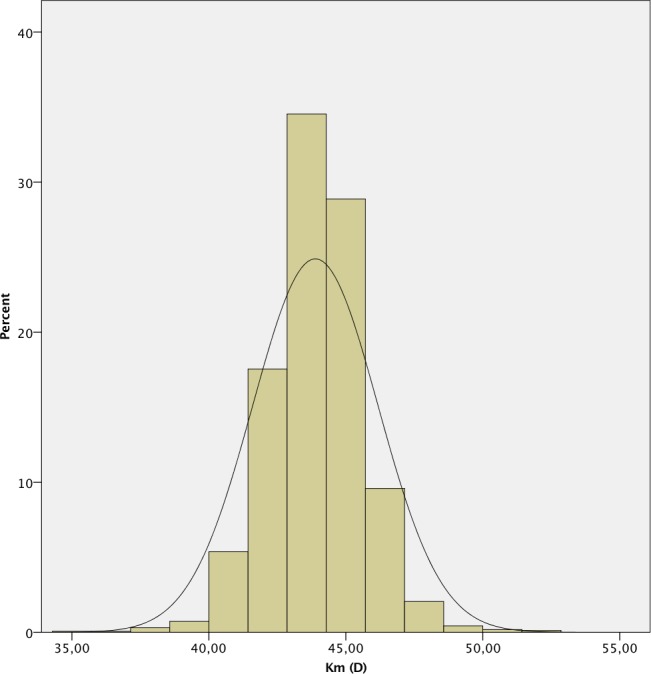
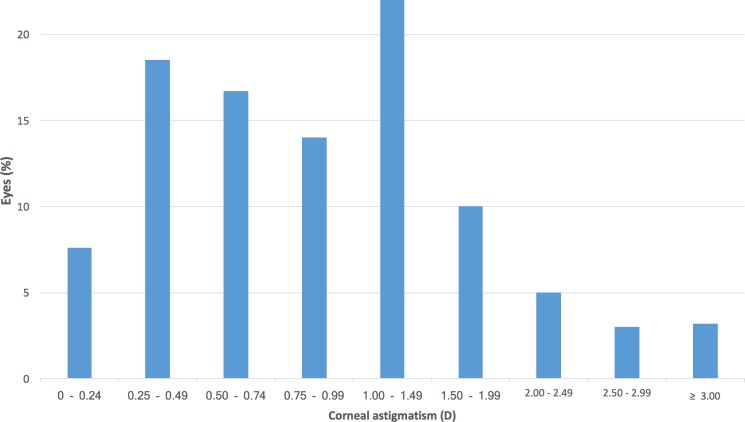
Fig 3. Histogram of corneal astigmatism of the study population.
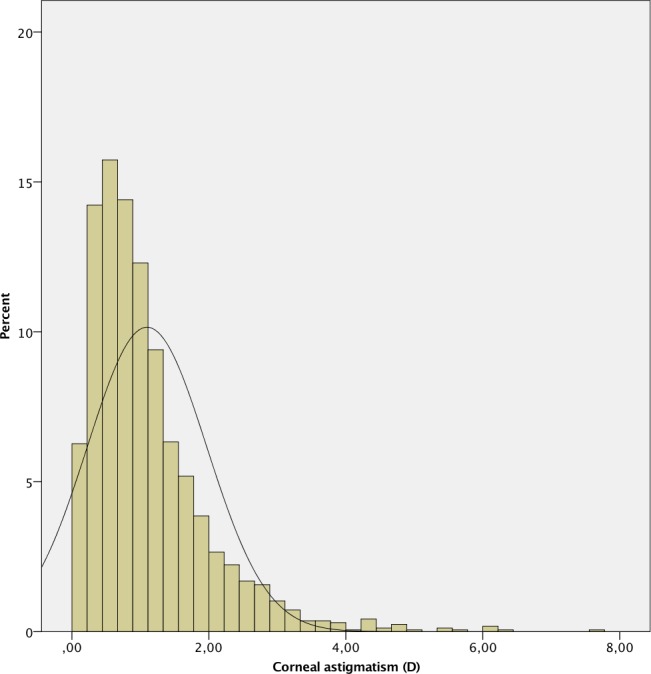
Fig 4. Histogram of anterior chamber depth (ACD) of the study population.
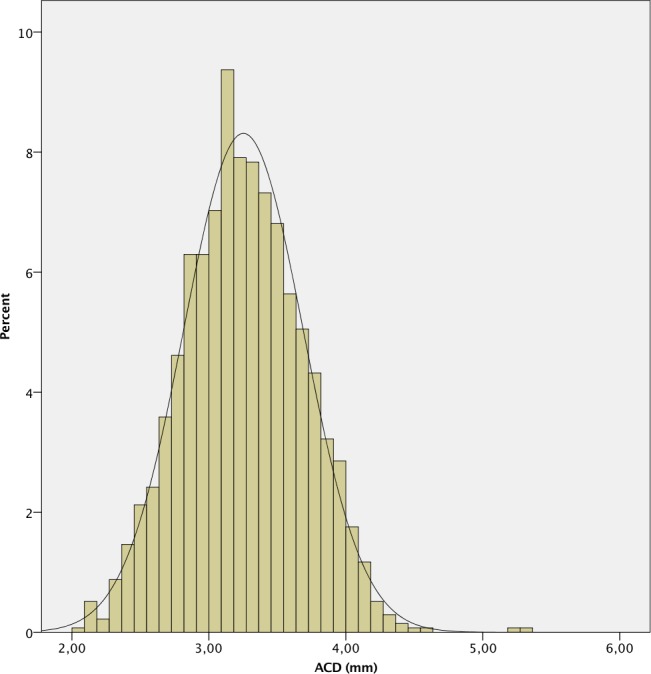
Fig 5. Histogram of lens thickness (LT) of the study population.
Male eyes had longer ALs, deeper ACDs and flatter corneas than female eyes (p < .001); however, there was no statistically significant differences in the other parameters evaluated.
The distribution of corneal astigmatism is shown in Fig 7. The mean corneal astigmatism was 1.08 ± 0.84 D (range 0–7.58), with 1415 (43.5%) eyes showing astigmatism ≥ 1 D. 1,513 (46.5%) eyes presented against-the-rule (ATR) astigmatism (steep meridian 0–30 degrees or 150–180 degrees), 1,077 (33.1%) eyes with-the-rule (WTR) (60 to 120 degrees), and 663 (20.4%) eyes were oblique (31–59 degrees or 121–149 degrees).
Fig 7. Distribution of corneal astigmatism in the study population.
Correlations
The AL, ACD, LT and CD were all significantly correlated between each other (p < .001). There was no significant correlation between age and any of the biometric parameters investigated (p > .05). The complete matrix of correlations is presented in Table 2.
Table 2. Matrix of correlations of ocular biometric parameters in Portuguese population.
| ACD | LT | CD | Mean K | Age | AL | |||
|---|---|---|---|---|---|---|---|---|
| Rho Spearman |
ACD | Correlation coefficient | 1,000 | -.633** | .484** | -.045 | -.018 | .571** |
| Sig. | . | < .001 | < .001 | .281 | .500 | < .001 | ||
| LT | Correlation coefficient | -.633** | 1.000 | -.245** | .032 | -.001 | -.334** | |
| Sig. | < .001 | . | < .001 | .256 | .979 | < .001 | ||
| CD | Correlation coefficient | .484** | -.245** | 1.000 | .048 | -.009 | .454** | |
| Sig. | < .001 | < .001 | . | .098 | .761 | < .001 | ||
| Mean K | Correlation coefficient | .040 | .032 | .048 | 1.000 | -.035 | .040 | |
| Sig. | .148 | .256 | .098 | . | .150 | .150 | ||
| Age | Correlation coefficient | -.018 | .012 | -.009 | -.035 | 1.000 | -.007 | |
| Sig. | .500 | .443 | .761 | .150 | . | .804 | ||
| AL | Correlation coefficient | .571** | -.334** | .454** | .040 | -.007 | 1.000 | |
| Sig. | < .001 | < .001 | < .001 | .150 | .804 | . | ||
**. Significant correlation (0.01).
Sig. = significance, ACD = anterior chamber depth (epithelium to lens), LT = lens thickness, CD = corneal diameter, Mean K = mean keratometry, AL = axial length.
Regression models
Regression models were constructed for AL, ACD, and K considering age, gender, K, ACD, LT, and CD. A longer AL was associated with male gender (β = .082, p = .018), and deeper ACD (β = 0.512, p < .001), LT (β = .105, p = .007), and CD (β = .171, p < .001). A deeper ACD was associated with male gender (β = .571, p < .001), longer AL (β = .298, p < .001), wider CD (β = .253, p < .001), and thinner LT (β = − .496, p < .001). For K, there was a significant association with male gender (β = .313, p < .001) and no significant associations with the other studied parameters.
Discussion
This study presents the normative values of the biometric parameters evaluated using optical biometry in a Portuguese population of candidates for cataract surgery. To our knowledge, this is the first study to characterize these parameters in this population.
Mean values of biometric parameters
The mean values of the biometric parameters published in the different studies in the literature are described in Table 3.
Table 3. Mean values of biometric parameters published in previous studies.
| Study | Country | Race | Measurement method |
AL (mm) | ACD (mm) | Km (D) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Males | Females | Total | Males | Females | Total | Males | Females | ||||
| Ferreira et al. | Portugal | Caucasian | Lenstar | 23.87 | 23.99 | 23.68 | 3.25 | 3.20 | 3.09 | 43.91 | 43.46 | 44.20 |
| The Tanjong Pagar Survey [1] | Singapore | Chinese | US Contact | 23.23 | 23.54 | 22.98 | 2.90 | 2.99 | 2.81 | 44.12 | 43.66 | 44.47 |
| Cao et al. [14] | China | Chinese | US Contact | 23.04 | - | - | 3.03 | - | - | 44.24 | - | - |
| Los Angeles Latino Eye Study [2] | USA | Hispanic | US Contact | 23.38 | 23.65 | 23.18 | 3.41 | 3.48 | 3.36 | 43.72 | 43.35 | 43.95 |
| Hoffer [15] | USA | Caucasian | US Immersion | 23.65 | - | - | 3.24 | - | - | 43.81 | - | - |
| Jivrajka et al. [16] | USA | Caucasian | US Immersion | 23.46 | 23.76 | 23.27 | 2.96 | 3.05 | 2.90 | - | - | - |
| The Reykjavik Study [11] | Finland | Caucasian | US Contact | - | 23.74 | 23.20 | - | 3.20 | 3.08 | - | 43.41 | 43.73 |
| The Singapore Malay Eye Study [12] | Singapore | Malay | IOLMaster | 23.55 | - | - | 3.10 | - | - | 44.12 | - | - |
| The Blue Mountains Eye Study [13] | Australia | Caucasian | IOLMaster | 23.44 | 23.75 | 23.20 | 3.10 | 3.16 | 3.06 | 43.42 | 43.01 | 43.74 |
| The Beaver Dam Eye Study [6] | USA | Caucasian | IOLMaster | 23.69 | 23.92 | 23.51 | 3.11 | 3.14 | 3.09 | 43.83 | 43.44 | 44.12 |
| Hoffmann et al. [17] | Germany | Caucasian | IOLMaster | 23.43 | 23.77 | 23.23 | 3.11 | 3.12 | 3.02 | 43.89 | 43.44 | 44.12 |
| Knox Cartwright et al. [18] | United Kingdom |
Caucasian | IOLMaster | 23.40 | 23.76 | 23.20 | - | - | - | 43.90 | 43.45 | 44.18 |
| Siahmed et al. [19] | France | Caucasian | IOLMaster | 23.46 | - | - | - | - | - | 43.97 | - | - |
| Olsen [20] | Denmark | Caucasian | IOLMaster | 23.45 | - | - | - | - | - | - | - | - |
US = A-scan ultrasound biometry, AL = axial length, ACD = anterior chamber depth, Km = mean keratometry (values converted to D using the given refractive index)
In our study, we found that AL had a non-normal distribution with positive deviation and high kurtosis. This deviation and kurtosis are in accordance with the findings described in the Reykjavik Eye study, [11] Singapore Malay Eye study, [12] and the Blue Mountains Eye Study. [13]The normality of the distribution is variable in several studies. The mean AL in our study (23.87 ± 1.55 mm) is longer than the one reported in the Singapore and Chinese populations using applanation contact ultrasound. [5, 14] It is still slightly longer than that reported in the Hispanic population of Los Angeles and Singapore Malay [12] and in the studies of Hoffer [15] and Jivrajka et al [16] both in the USA and using immersion ultrasound. When compared with studies using optical biometry, the mean AL in our population is longer than that of the Caucasian population in Australia [13] and USA. [6] Using optical biometry, the mean AL in our study is longer than that published in several studies of European populations. [17–20] Although there may be differences explained by the AL measurement method, the AL in our study is longer than that published in the literature for different populations in studies using optical biometry, being closer to that reported in the Caucasian population of the USA [6, 15] than in European Caucasian populations. [17–20] In the latter populations, there is great similarity in the AL values reported in different countries; hence, in our study is longer than all of them, with a difference in mean values of about 0.40 mm. Although the majority of these studies used the IOLMaster 500 (Carl Zeiss AG, Jena, Germany) and our study used the Lenstar, this does not explain the differences found, since it was demonstrated by Hoffer et al. [9] that the IOLMaster and Lenstar AL biometry are not significantly different. The mean difference found is relevant, since a 1 mm error in AL results in a residual postoperative refractive error of 2.35 D in a 23.5 mm eye, 1.75 D in a 30.0 mm eye and 3.75 D in a 20 mm eye or about 2.0–4.0 D in the power of the implanted IOL. [21]
The mean keratometry in our study did not follow a normal distribution, with negative deviation and high kurtosis. These findings are similar to both the Singapore Malay Eye study [12] and the Blue Mountains Eye Study. [13] The mean keratometry in our study was 43.91 ± 1.71 D. This value is lower than that reported in the Chinese [2] and Singaporean [12] populations, being closer to those reported in the Caucasian population in Europe [18, 19] and USA. [15] Although the keratometry evaluation methods are different, there is a close relationship between the values reported in Caucasian populations, which are generally lower than in the Far Eastern populations. The difference observed with respect to Far Eastern populations is significant, representing a potential difference in the refractive error greater than 0.50 D. [21]
It is known that about 29 to 40% of patients undergoing cataract surgery have corneal astigmatism greater than 1 D, which is enough to prevent optimal visual acuity without optical correction. [22] In our series, the mean corneal astigmatism was 1.08 ± 0.84 D, with 43.5% of the eyes showing astigmatism ≥ 1 D. These values are higher than those reported in most studies, such as those by Ferrer-Blasco et al. [22] (34.8%) in Spain and by Hoffmann et al. [17] in Germany (36%). It is known that corneal astigmatism varies significantly with age, increasing the prevalence of ATR astigmatism. [23] In our study, the majority of eyes (46.5%) had ATR astigmatism, which is in agreement with the age range of the evaluated population, with a mean of 69 years-old.
The mean ACD in our population (3.25 ± 0.44 mm) was higher than that reported in most studies in Eastern [2, 12, 14] and in Western populations [6, 11, 13, 17], and it is comparable with that reported by Hoffer in the USA [15]. The differences found may be partly because of the measurement method used, since Lenstar uses laser optical biometry to measure ACD, while the IOLMaster 500, uses an optical slit image. Hoffer et al [9] have reported that ACD values with Lenstar are higher than those measured with IOLMaster 500.
In our series, the mean LT was 4.32 ± 0.49 mm, and it was directly proportional to age and inversely proportional to AL. These findings confirm those of the studies by Jivrajka et al. [16] and Hoffer [15, 24], although LT in our study was thinner than those studies reported.
The mean CD in our study (12.02 ± 0.46 mm) was similar to that reported in other series in the literature. [13, 17]
Relationship with gender and age
In this study, male eyes had longer ALs, deeper ACDs and flatter corneas than female patients did, and a gender difference with respect to the other investigated parameters was not statistically significant. These results are in accordance with those in the literature, especially in populations from Germany, [17] Australia, [13] USA, [6, 16] and Iceland. [11] It is interesting to note that in a paper to be published, Hoffer et al. found a constant 0.50 mm difference in AL between genders, much higher than the 0.31 mm we found in this study. According to the Beaver Dam Eye Study [6] the height adjustment of individuals can explain all the differences found between the genders, however other studies have adjusted for height and weight and found that the differences still existed. Since gender and race appear to be important determinants of ocular biometric parameters, it may be important to consider them in the calculation of the IOL for cataract surgery, as shown by the appearance of the first 5th-generation formula, the Hoffer-H-5, which uses the same basic structure as the Holladay 2 formula but considers gender and ethnicity to reduce the error associated with the use of generalized population regression factors.
In contrast with most studies, [13, 17] there was no significant correlation between age and AL, ACD, or K. In the study by Hoffmann et al., [17] the results were similar to those observed in our series, and no correlation was found between age and AL. The interpretation of these differences is complex and would require adjustments for the refraction, height, age, and even educational level of the studied population.
Correlations between parameters
In this series, there was a positive correlation between AL and ACD, and K (not statistically significant) and CD, and a negative correlation between AL and LT. These results are in agreement with those reported in the literature [13, 15, 16] except for K, whose correlation with AL is inverse in most series, showing the emmetropic relationship between AL and corneal curvature. [15] Although there may be population differences and the correlation with refractive error has not been addressed in this study, the different published studies in the literature reported keratometry evaluated with manual, automatic, or IOLMaster keratometry, and these values cannot be directly compared with ours because of the different methods of measurement and refractive indices used.
Regression models
In regression models for AL, ACD, and K considering age, gender, K, ACD, LT, and CD, the major determinants of AL were ACD and CD, and gender was not significant. Unlike the finding in other series, age was not a significant determinant. [6, 12] An association between ACD and CD and LT was also observed.
In conclusion, the present study presents normative biometric parameters and their relationships in a Portuguese population. These results may be relevant not only in the evaluation of the refractive error but also in the IOL calculation for cataract surgery. The obtained AL, ACD, and mean K values were closer to the US population than most published series in different European Caucasian populations, and the disparities found could represent differences greater than 1 D in both the refractive error and the IOL power. Corneal astigmatism in the present study was higher than that in most published series, which may affect the type of IOL to be implanted.
Acknowledgments
Financial interests: Hoffer licenses the registered trademark name Hoffer® to all ultrasound and optical biometer manufacturers for the commercial use of the Hoffer Q and Hoffer H-5 formulas to ensure accuracy of their programming. This does not alter our adherence to PLOS ONE policies on sharing data and materials.
Funding information: Fundação para a Ciência e a Tecnologia—PEst-OE/FIS/UI0068/2011 and UID/FIS/00068/2013 - Prof Paulo Ribeiro.
Sociedade Portuguesa de Oftalmologia—N/A—Dr Tiago Ferreira.
No other author has a financial relationship with anything in this paper.
Financial support: Portuguese research Grant numbers PEst-OE/FIS/UI0068/2011 and UID/FIS/00068/2013 through the FCT-MEC, the “Plurianual” financial contribution of “Fundação para a Ciência e Tecnologia”, Portugal and Sociedade Portuguesa de Oftalmologia PhD Grant.
Data Availability
Data cannot be made publicly available to protect patient privacy. Data are available upon request from the corresponding author. For additional information about the data, please contact Comissão Nacional de Proteção de Dados Rua de São Bento at geral@cnpd.pt.
Funding Statement
This work was supported by Portuguese research Grant numbers PEst-OE/FIS/UI0068/2011 and UID/FIS/00068/2013 through the FCT-MEC, the “Plurianual” financial contribution of “Fundação para a Ciência e Tecnologia”, Portugal and Sociedade Portuguesa de Oftalmologia PhD Grant.
References
- 1.Wong TY, Foster PJ, Ng TP, Tielsch JM, Johnson GJ, Seah SK. Variations in ocular biometry in an adult Chinese population in Singapore: the Tanjong Pagar Survey. Invest Ophthalmol Vis Sci. 2001;42:73–80. [PubMed] [Google Scholar]
- 2.Shufelt C, Fraser-Bell S, Ying-Lai M, Torres M, Varma R. Refractive error, ocular biometry, and lens opalescence in an adult population: the Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci. 2005;46:4450–4460. doi: 10.1167/iovs.05-0435 [DOI] [PubMed] [Google Scholar]
- 3.Grosvenor T. Reduction in axial length with age: an emmetropizing mechanism for the adult eye? Am J Optom Physiol Opt. 1987;64:657–663. [PubMed] [Google Scholar]
- 4.Ip JM, Huynh SC, Kifley A, Rose KA, Morgan IG, Varma R et at. Variation of the contribution from axial length and other oculometric parameters to refraction by age and ethnicity. Invest Ophthalmol Vis Sci. 2007;48:4846–4853. doi: 10.1167/iovs.07-0101 [DOI] [PubMed] [Google Scholar]
- 5.Saw SM, Chua WH, Hong CY, Wu HM, Chia KS, Stone RA et al. Height and its relationship to refraction and biometry parameters in Singapore Chinese children. Invest Ophthalmol Vis Sci. 2002;43:1408–1413. [PubMed] [Google Scholar]
- 6.Lee KE, Klein BK, Klein R, Quandt Z, Wong TY. Age, Stature, and Education Associations with Ocular Dimensions in an Older White Population. Arch Ophthalmol. 2009;127:88–93. doi: 10.1001/archophthalmol.2008.521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Santodomingo-Rubido J, Mallen EA, Gilmartin B, Wolffsohn JS. A new non-contact optical device for ocular biometry. Br J Ophthalmol. 2002;86:458–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lege BA, Haigis W. Laser interference biometry versus ultrasound biometry in certain clinical conditions. Graefes Arch Clin Exp Ophthalmol. 2004;242:8–12. doi: 10.1007/s00417-003-0672-2 [DOI] [PubMed] [Google Scholar]
- 9.Hoffer KJ, Shammas HJ, Savini G. Comparison of 2 laser instruments for measuring axial length. J Cataract Refract Surg. 2010;36(4):644–648, Erratum 2010;36(6):1066. doi: 10.1016/j.jcrs.2009.11.007 [DOI] [PubMed] [Google Scholar]
- 10.Laursen JV, Jeppesen P, Olsen T. Precision of 5 different keratometry devices. Int Ophthalmol. 2016;36:17–20. doi: 10.1007/s10792-015-0069-3 [DOI] [PubMed] [Google Scholar]
- 11.Olsen T, Arnarsson A, Sasaki H, Sasaki K, Jonasson F. On the ocular refractive components: the Reykjavik Eye Study. Acta Ophthalmol Scand. 2007;85:361–366. doi: 10.1111/j.1600-0420.2006.00847.x [DOI] [PubMed] [Google Scholar]
- 12.Lim LS, Saw SM, Jeganathan SE, Tay WT, Aung T, Tong L et al. Distribution and determinants of ocular biometric parameters in an Asian population: the Singapore Malay Eye Study. Invest Ophthalmol Vis Sci. 2010;51:103–109. doi: 10.1167/iovs.09-3553 [DOI] [PubMed] [Google Scholar]
- 13.Fotedar R, Wang JJ, Burlutsky G et al. Distribution of axial length and ocular biometry measured using partial coherence laser interferometry (IOLMaster) in an older white population. Ophthalmology. 2010;117:417–423. doi: 10.1016/j.ophtha.2009.07.028 [DOI] [PubMed] [Google Scholar]
- 14.Cao X, Hou X, Bao Y. The ocular biometry of adult cataract patients on lifeline express hospital eye train in rural China. J Ophthalmol. 2015. 5;2015:171564 doi: 10.1155/2015/171564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoffer KJ. Biometry of 7,500 cataractous eyes. Am J Ophthalmol. 1980;90:360–368 Erratum: 1980;90(6):890. [DOI] [PubMed] [Google Scholar]
- 16.Jivrajka R, Shammas MC, Boenzi T, Swearingen M, Shammas HJ. Variability of axial length, anterior chamber depth, and lens thickness in the cataractous eye. J Cataract Refract Surg. 2008;34:289–294. doi: 10.1016/j.jcrs.2007.10.015 [DOI] [PubMed] [Google Scholar]
- 17.Hoffmann PC, Hütz WW. Analysis of biometry and prevalence data for corneal astigmatism in 23,239 eyes. J Cataract Refract Surg. 2010;36:1479–1485. doi: 10.1016/j.jcrs.2010.02.025 [DOI] [PubMed] [Google Scholar]
- 18.Knox Cartwright NE, Johnston RL, Jaycock PD, Tole DM, Sparrow JM. The Cataract National Dataset electronic multicentre audit of 55,567 operations: when should IOLMaster biometric measurements be rechecked? Eye (Lond). 2010;24:894–900. [DOI] [PubMed] [Google Scholar]
- 19.Siahmed K, Muraine M, Brasseur G. Optic biometry in intraocular lense calculation for cataract surgery. Comparison with usual methods. J Fr Ophtalmol. 2001;24:922–926. [PubMed] [Google Scholar]
- 20.Olsen T. Improved accuracy of intraocular lens power calculation with the Zeiss IOLMaster. Acta Ophthalmol Scand. 2007;85:84–87. doi: 10.1111/j.1600-0420.2006.00774.x [DOI] [PubMed] [Google Scholar]
- 21.Ribeiro F, Castanheira-Dinis A, Dias JM. Refractive error assessment: influence of different optical elements and current limits of biometric techniques. J Refract Surg. 2013;29:206–212. [DOI] [PubMed] [Google Scholar]
- 22.Ferrer-Blasco T, Montes-Mico R, Peixoto-de-Matos SC, González-Méijome JM, Cerviño A. Prevalence of corneal astigmatism before cataract surgery. J Cataract Refract Surg. 2009;35:70–75. doi: 10.1016/j.jcrs.2008.09.027 [DOI] [PubMed] [Google Scholar]
- 23.Anstice J. Astigmatism–its components and their changes with age. Am J Optom Arch Am Acad Optom. 1971;48:1001–1006. [DOI] [PubMed] [Google Scholar]
- 24.Hoffer KJ. Axial dimension of the human cataractous lens. Arch Ophthalmol 1993;111(7):914–918, Erratum 1993;111(12):1626. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data cannot be made publicly available to protect patient privacy. Data are available upon request from the corresponding author. For additional information about the data, please contact Comissão Nacional de Proteção de Dados Rua de São Bento at geral@cnpd.pt.