Abstract
Vertebrobasilar insufficiency (VBI) provoked by physiological head rotation is known as rotational vertebral artery syndrome (RVAS) or Bow Hunter syndrome. RVAS most often occurs at C1–2 level with head rotation and presents with symptoms of VBI. Several previously published studies have reported RVAS at subaxial sites (V2 segment), however, tumor-induced RVAS has never been reported. The authors report the first case of RVAS at V2 segment due to compression from a spinal tumor. A 71-year-old man presented with symptoms of dizziness provoked by head rotation or neck extension. computed tomography (CT) angiography and dynamic cerebral angiography revealed circumferential stenosis with neutral neck position and complete occlusion of the left dominant vertebral artery (VA) at C5 level with his neck extended or rotated to the left. Complete neurological recovery was achieved after removal of a spinal osteochondroma and surgical decompression of the left VA via an anterior approach. Spinal tumors should be included in the differential diagnosis in cases of RVAS. Spinal degenerations or sarcomatous transformation of the tumor could lead to clinical manifestations of RVAS in cases with spinal osteochondroma. Complete removal of the tumor with or without spinal fusion would be the treatment of choice, in addition to medical treatment in the cases of acute stroke.
Keywords: rotational vertebral artery syndrome, vertebrobasilar insufficiency, spinal osteochondroma, subaxial spine, anterior approach
Introduction
Rotational vertebral artery syndrome (RVAS), also known as Bow Hunter syndrome, is the clinical presentation of vertebrobasilar insufficiency (VBI) produced by reversible occlusion of the vertebral artery (VA) during head rotation. Typically, the dominant VA is transiently compressed at the C1-2 level, but there are multiple reports indicating that RVAS can occur in the subaxial cervical spine. The majority of these cases were secondary to spondylotic changes, such as osteophytes of the uncovertebral joint, disc herniation, and spondylolisthesis.1–5) Here, we report a rare case of RVAS caused by a compressive spinal osteochondroma that occurred at the C5 transverse foramen. To our knowledge, a RVAS case triggered by spinal tumor has not been previously reported. The case was successfully treated with total removal of the tumor via an anterior approach. We discuss the surgical and pathological findings of this rare entity in detail.
Case Report
A 71-year-old male presented to Nagoya University Hospital complaining of a 2-year history of dizziness, without loss of consciousness, provoked by neck extension or rotation of his head nearly 90° toward the left. The symptom always resolved immediately after he returned his head to the neutral position. He had never suffered from any pathology of the cervical spine and had a negative family history. Neurological examination was otherwise normal without myelopathy, motor weakness or sensory disturbance.
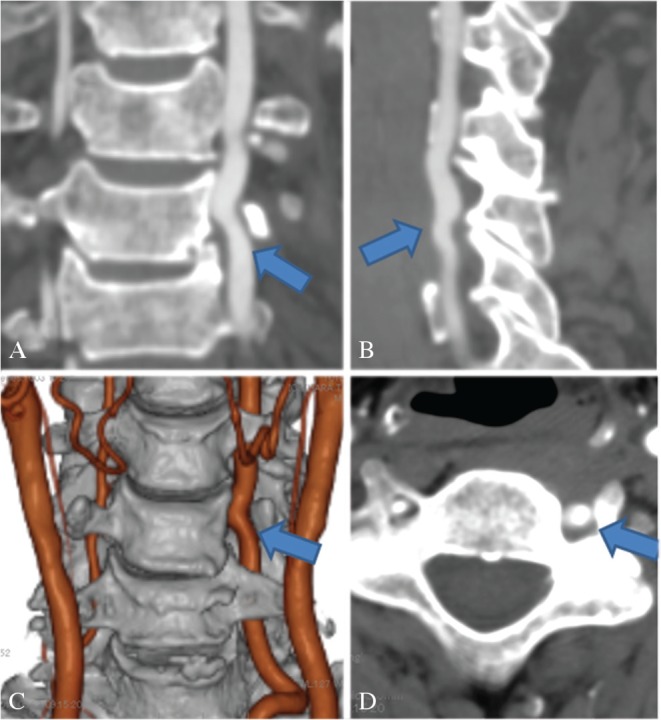
Cervical spine x-rays showed degenerative change with collapsed disc space (Fig. 1A) and segmental hypermobility of the index level on flexion and extension X-ray (Figs. 1B, and 1C) compared with other levels, while there was not significant spinal instability. Computed tomographic angiography (CTA) of the VA obtained with his head maintained in neutral position showed severe circumferential stenosis of the left VA with medial displacement by an exophytic bony structure as well as with lateral intervertebral disc bulging at the C5 transverse foramen (Figs. 2A, 2B, and 2D–2G). The bony mass was presumed to be arising from the C5/6 facet joint on computed tomography (CT) (Figs. 2A, 2B, and 2D). Spinal degenerations, such as lateral disc bulging, multilevel facet joint osteoarthritis and osteophyte formation, were also confirmed on CT and magnetic resonance image (MRI) (Figs. 2C, 2F, and 2G). Cerebral angiography demonstrated stenosis of the left VA at the C5/6 level with his head maintained neutral (Fig. 3A) and a right VA terminating at the posterior inferior cerebellar artery (PICA) (Fig. 3C). However, on dynamic cerebral angiography with his head rotated to the left or extended, the left VA was completely occluded and the distal VA flow was weakly filled by collateral circulation from muscular branches (Fig. 3B).
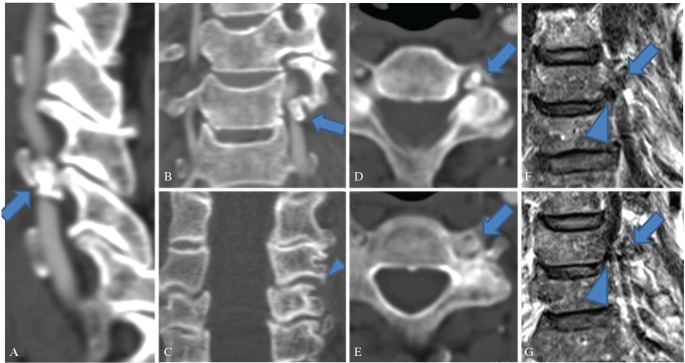
Fig. 1.
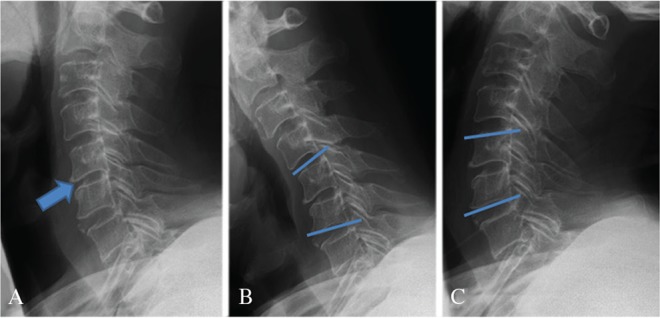
Preoperative cervical spine x-rays showed mild degenerative changes and collapse of the disc space at C5/6 level (Fig. 1A arrow). Although there was no clear spinal instability, neck flexion created kyphotic angle at C5/6 level, indicating hypermobility, compared with other levels (Fig. 1B). Extension x-ray revealed well-aligned C5/6 segment (Fig. 1C). A: neutral x-ray, B: flexion x-ray, C: extension x-ray.
Fig. 2.
Preoperative computed tomographic angiography (CTA) of the vertebral artery (VA) (A: sagittal view, B and C: coronal view, D and E: axial view) and coronal image of MRI (T2WI) obtained with his head maintained neutral showed severe circumferential stenosis of the dominant left VA with medial displacement by an exophytic bony structure (arrow; Figs. 2A, 2B, and 2D–2G) and compression toward lateral direction by lateral disc bulging (arrowhead; Figs. 2F, and 2G) at the C5 transverse foramen. Osteophyte formation and osteoarthritis of C5/6 facet joint are showed (arrowhead; Fig. 2C), indicating spinal degenerations.
Fig. 3.
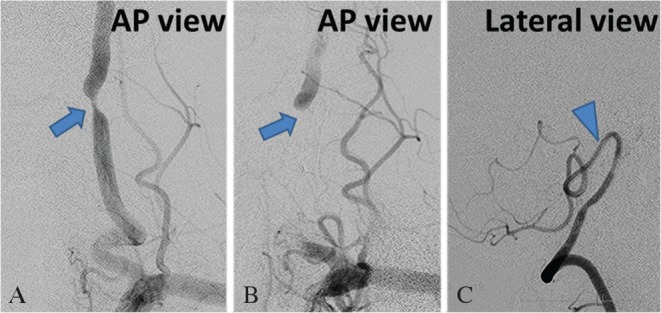
Preoperative cerebral angiography with neutral neck position demonstrated severe stenosis (arrow) of the left vertebral artery (VA) at the C5/6 level (Fig. 3A) and a right VA terminating at the posterior inferior cerebellar artery (PICA) (arrowhead) (Fig. 3C). Dynamic cerebral angiography with his head rotated to the left or extended showed the left VA was completely occluded at the C5/6 level and the distal VA flow was weakly filled by collateral circulation from muscular branches (Fig. 3B). AP view: (Anterior-Posterior view).
Surgery was recommended to remove the bony mass and decompress the left VA. A left-sided anterior approach was adopted. The longus colli muscle was dissected off the vertebral body at the C4 to C6 levels on the left side and mobilized laterally. The muscle was divided transversely at the index level with the fascia of the muscle left intact to preserve sympathetic nerves. The anterior surface of the C5 transverse process was exposed, then unroofed. Cartilage-like solid tissue was noted inside the transverse foramen, compressing the VA towards the medial direction (Fig. 4A). The lesion was adherent slightly to the VA at the medial aspect and heavily to the C5/6 facet joint, therefore, it was gently separated circumferentially and successfully removed en bloc. VA nicely expanded and pulsated immediately after removal of the mass lesion. Medial aspect of VA was not explored since we were concerned additional maneuver of severely squeezed VA could cause arterial dissection. The floor of cavity created after removal was carefully investigated.
Fig. 4.
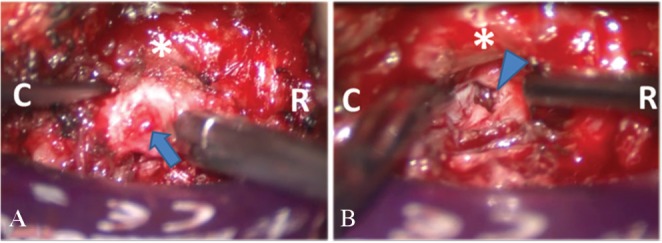
Intraoperative pictures demonstrated cartilage-like tissue (arrow) compressing the left vertebral artery (asterisk) was encountered after removing the anterior wall of C5 transverse foramen (Fig. 4A). The floor of the cavity created after removal of the lesion was breached facet capsule and facet cartilage was exposed. (Fig. 4B arrowhead). The tumor appeared to be connected to the C5/6 facet joint. R: rostral direction, C: caudal direction.
The facet capsule was breached and articular cartilage was exposed. Judging from these intraoperative findings, the lesion appeared to be directly connected to the C5/6 facet joint. Therefore, we concluded that it had arisen from the facet joint (Fig. 4B). Spinal fusion was deemed unnecessary because of lack of significant spinal instability. Histological examination revealed a benign osteochondroma with mature bony trabeculae and bone marrow capped by cartilage tissue. Sarcomatous transformation was absent. Endochondral ossification intervened between the bone and cartilage (Figs. 5A–5C).
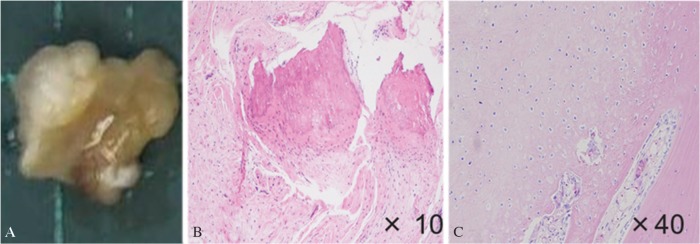
Fig. 5.
(A) An actual photograph of surgical specimen. (B and C) Histological examination revealed a benign osteochondroma with mature bony trabeculae and bone marrow capped by cartilage tissue. Endochondral ossification intervened between the bone and cartilage.
The patient recovered well and his neurological symptoms completely resolved immediately after surgery. CTA obtained 6 months after surgery showed no focal stenosis of the left VA and no residual or recurrent tumor (Figs. 6A–6D).
Fig. 6.
Good flow of left dominant vertebral artery was confirmed on computed tomographic angiography (CTA) obtained 6 months after surgery. There was no residual tumor and marked restoration of caliber of left vertebral artery (arrow). (A: AP view, B: lateral view, C: 3D image, D: axial view).
Discussion
VBI is rarely symptomatic because most patients have adequate collateral flow compensation.6) To be symptomatic, the contralateral VA and anterior cerebral circulation must be insufficient to provide compensatory flow.7) In the present case, dynamic DSA demonstrated that the left dominant VA was completely occluded at the C5 level with the leftward head rotation or extension. Distal blood flow after occlusion supplied by muscular branches was considered to be insufficient in light of the contralateral hypoplastic VA terminating in the PICA.
RVAS, also known as Bow Hunter syndrome, is VBI induced by physiological head rotation. Typically, head rotation may provoke mechanical stretching and kinking of the contralateral VA at the C1–2 level (V3 segment), which is followed by external compression of the VA by ligamentous insertions or deep fascia at the scalenovertebral angle (V1 segment).8,9) Other less frequent causes include osteophytes of the uncovertebral joint, disc herniation, and spondylolisthesis at the C3–6 level where the VA passes through the transverse foramen (V2 segment).1–3,10,11) Neurological symptoms of V2 RVAS are provoked by ipsilateral head rotation or neck extension in most cases, contrary to classic RVAS at the C1/2 level. To the best of our knowledge, a spinal tumor has never been implicated as the cause of RVAS in the V2 segment. In the present case, the tumor seemed to originate from facet joint and its mobility might have led to intermittent symptoms related to head rotation or neck extension. For RVAS at the V2 segment, anterior cervical decompression with or without fusion is a reasonable approach.12,13) Resection of osteophyte or disc herniation compressing VA and unroofing of the transverse foramen are key maneuvers.
Osteochondroma is the most common benign osseous tumor and usually arises at the metaphysis of the long bone.14) It basically grows in line with bone growth and stops increasing in size with skeletal maturity. The tumor, therefore, tends to be symptomatic with an average age of around 30 years15) In several previous reports, the appearance of symptoms at a much later age and progression of symptoms are explained by possible growth of the tumor beyond skeletal maturity,16,17) however, this abnormal tumor growth is unlikely. At the same time, we need to consider the possibility of sarcomatous transformation if we detect continuous growth of the tumor, however, this was ruled out in the present case based on histological assessment.17) Given the fact that the present case became symptomatic at older age with symptoms triggered by neck motion, we have to consider spinal degenerations and spinal mobility as a static and dynamic factor other than the presence of spinal tumor. VA was circumferentially squeezed by the combination of osteochondroma and lateral disc bulging on preoperative angiography, 3DCTA and MRI even with neutral neck position, which was static compression and completely different from past reports of RVAS describing the flow of the VA with neutral neck position as normal. Furthermore, the tumor location of facet joint has to be directly affected by facet joint mobility associated with spinal degenerations including disc bulging and osteophyte formation. Therefore, we conclude the static compression from both of osteochondroma arising from facet joint and lateral disc bulging was dynamically influenced by spinal mobility, resulting in the production of motion-related symptoms in the 71-year-old patient.16,17)
Approximately, 50% of spinal osteochondromas arise in the cervical spine, particularly from the posterior arch followed by the vertebral body, the pedicle, the articular facet or the transverse process.15) As far as we know, there have been only four reports describing the association of spinal osteochondromas with VBI (Table 1).18–21) Three out of four cases presented with neurological symptoms under the age of thirty. One case reported by Fadili was a 59-year-old male, who developed acute occlusion of ipsilateral VA at the tumor location.21) The VA dissection may have been triggered by a combination of neck motion and long-lasting compression from the tumor, which was occupying most of the C4 transverse foramen. Only one case reported by Zhang et al. demonstrated a dynamic change of the VA flow on neck motion during dynamic angiography like the present case.20) However, a clear relationship between neck movement and clinical deterioration was not revealed. The other three cases presented with complete irreversible VA occlusion.18,19),21) Therefore, RVAS induced by osteochondroma is first described in this report. Early exploration and detection of the tumor are essential once VBI becomes symptomatic. Presence of a tumor should be considered as a potential cause of VBI for prevention of stroke or irreversible VA occlusion. Conservative, surgical and more recently endovascular intervention have been generally proposed for RVAS.22–24) However, surgical intervention has to be considered as a treatment of choice for tumor-induced RVAS. Two slowly-progressive VBI cases caused by osteochondromas were effectively treated surgically (Table 1).18,20) As VBI-related osteochondroma is usually located ventrally to the spinal canal, either of anterior or anterolateral approach is conveniently adopted. Complete removal of the tumor should be aimed for in light of the possibility of sarcomatous transformation. Spinal fusion has to be planned if tumor-induced spinal instability is suspected, depending on the extent of bone destruction by the tumor. Two other cases reportedly developed acute neurological deficits provoked by VA dissections (Table 1). In these unstable conditions, medical treatment should precede surgery. Out of these two unstable cases, one case reported by Altaf showed a VA dissection on the contralateral side to the incidentally-found tumor and only antiplatelet medication was given.19) The other unstable case reported by Fadili received treatment for stroke without tumor removal because of a complete irreversible VA occlusion as a result of dissection.21)
Table 1.
Summary of reported cases of vertebrobasilar insufficiency associated with spinal osteochondroma
| Authors & Year | Age & Sex | Tumor type | Involved spinal elements | Presenting symptoms (VA-related symptoms) | State of VA | Effect of head rotation on VA | Treatment | Surgical outcome |
|---|---|---|---|---|---|---|---|---|
| George et al., 198918) | 30, male | multiple hereditary | C2 transverse process, lamina, articular facet | C2 neuralgia, tinnitus, dizziness, blurred vision (tinnitus, dizziness) | Ipsi; complete occlusion, Con; dominant and good filling to brain stem | No | Tumor removal via anterolateral approach without fusion | Complete recovery |
| Altaf et al., 201319) | 14, male | multiple hereditary | C1 lateral mass | dizziness, headache, transient motor weakness and facial droop (all symptoms) | Ipsi; complete occlusion, Con; acute dissection | No | No surgery and antiplatelet medication for acute dissection | Complete recovery |
| Zhang et al., 201520) | 19, female | solitary | C1 lateral mass | vertigo, nausea, vomiting, headache (all symptoms) | Ipsi; narrowing by 50%, Con; good filling to brain stem | Yes | Tumor removal, otherwise no description provided | No progression |
| Fadili et al., 201421) | 59, male | solitary | C4 posterior arch | Coma due to bilateral cerebellar infarction and hydrocephalus (all symptoms) | Ipsi; complete occlusion, Con; dominant and intact | No | Ventriculostomy and posterior fossa decompression | Complete recovery |
| Present case | 71, male | solitary | C5–6 articular facet | Dizziness on neck rotation & extension (all symptoms) | Ipsi; complete occlusion, Con; hypoplastic terminating in the PICA | Yes | Anterior approach without fusion | Complete recovery |
Con: Contralateral, Ipsi: Ipsilateral, PICA: posterior inferior cerebellar artery, VA: vertebral artery.
The cause of VBI in the present case was a compressive osseous tumor associated with spinal degenerations and spinal mobility in the subaxial cervical spine. Complete surgical resection of the tumor and decompression of the VA without fusion was curative. The treatment modality should be selected by careful evaluation of pathology, such as the cause of compression, location, or spinal stability.
Conclusion
We reported a rare case of RVAS associated with spinal osteochondroma arising from the C5/6 facet joint. Imaging studies localized the lesion and the dynamic changes of the vertebrobasilar circulation were clearly revealed. Histological evaluation was necessary for the diagnosis. After surgical resection, the patient neurologically recovered well without tumor recurrence.
Footnotes
Conflicts of Interest Disclosure
The authors have no conflicts of interests.
References
- 1).Yoshimura K, Iwatsuki K, Ishihara M, Onishi Y, Umegaki M, Yoshimine T: Bow hunter’s stroke due to instability at the uncovertebral C3/4 joint. Eur Spine J 20 Suppl 2: S266–S270, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2).Vates GE, Wang KC, Bonovich D, Dowd CF, Lawton MT: Bow hunter stroke caused by cervical disc herniation. Case report. J Neurosurg 96: 90–93, 2002 [DOI] [PubMed] [Google Scholar]
- 3).Piñol I, Ramirez M, Saló G, Ros AM, Blanch AL: Symptomatic vertebral artery stenosis secondary to cervical spondylolisthesis. Spine 38: E1503–E1505, 2013 [DOI] [PubMed] [Google Scholar]
- 4).Bakay L, Leslie EV: Surgical treatment of vertebral artery insufficiency caused by cervical spondylosis. J Neurosurg 23: 596–602, 1965 [DOI] [PubMed] [Google Scholar]
- 5).Nagashima C: Surgical treatment of vertebral artery insufficiency caused by cervical spondylosis. J Neurosurg 32: 512–521, 1970 [DOI] [PubMed] [Google Scholar]
- 6).Yang PJ, Latack JT, Gabrielsen TO, Knake JE, Gebarski SS, Chandler WF: Rotational vertebral artery occlusion at C1–C2. AJNR Am J Neuroradiol 6: 96–100, 1985 [PMC free article] [PubMed] [Google Scholar]
- 7).Spetzler RF, Hadley MN, Martin NA, Hopkins LN, Carter LP, Budny J: Vertebrobasilar insufficiency. Part 1: Microsurgical treatment of extracranial vertebrobasilar disease. J Neurosurg 66: 648–661, 1987 [DOI] [PubMed] [Google Scholar]
- 8).Zaidi HA, Albuquerque FC, Chowdhry SA, Zabramski JM, Ducruet AF, Spetzler RF: Diagnosis and management of bow hunter’s syndrome: 15-year experience at barrow neurological institute. World Neurosurg 82: 733–738, 2014 [DOI] [PubMed] [Google Scholar]
- 9).Kojima N, Tamaki N, Fujita K, Matsumoto S: Vertebral artery occlusion at the narrowed “scalenovertebral angle”: mechanical vertebral occlusion in the distal first portion. Neurosurgery 16: 672–674, 1985 [DOI] [PubMed] [Google Scholar]
- 10).Kawaguchi T, Fujita S, Hosoda K, Shibata Y, Iwakura M, Tamaki N: Rotational occlusion of the vertebral artery caused by transverse process hyperrotation and unilateral apophyseal joint subluxation. Case report. J Neurosurg 86: 1031–1035, 1997 [DOI] [PubMed] [Google Scholar]
- 11).Ujifuku K, Hayashi K, Tsunoda K, et al. : Positional vertebral artery compression and vertebrobasilar insufficiency due to a herniated cervical disc. J Neurosurg Spine 11: 326–329, 2009 [DOI] [PubMed] [Google Scholar]
- 12).Miele VJ, France JC, Rosen CL: Subaxial positional vertebral artery occlusion corrected by decompression and fusion. Spine 33: E366–E370, 2008 [DOI] [PubMed] [Google Scholar]
- 13).Lu DC, Zador Z, Mummaneni PV, Lawton MT: Rotational vertebral artery occlusion-series of 9 cases. Neurosurgery 67: 1066–1072, 2010 [DOI] [PubMed] [Google Scholar]
- 14).Khosla A, Martin DS, Awwad EE: The solitary intraspinal vertebral osteochondroma. An unusual cause of compressive myelopathy: features and literature review. Spine 24: 77–81, 1999 [DOI] [PubMed] [Google Scholar]
- 15).Albrecht S, Crutchfield JS, SeGall GK: On spinal osteochondromas. J Neurosurg 77: 247–252, 1992 [DOI] [PubMed] [Google Scholar]
- 16).Sakai D, Mochida J, Toh E, Nomura T: Spinal osteochondromas in middle-aged to elderly patients. Spine 27: E503–E506, 2002 [DOI] [PubMed] [Google Scholar]
- 17).Gille O, Pointillart V, Vital JM: Course of spinal solitary osteochondromas. Spine 30: E13–E19, 2005 [PubMed] [Google Scholar]
- 18).George B, Atallah A, Laurian C, Tayon B, Mikol J: Cervical osteochondroma (C2 level) with vertebral artery occlusion and second cervical nerve root irritation. Surg Neurol 31: 459–464, 1989 [DOI] [PubMed] [Google Scholar]
- 19).Altaf F, Movlik H, Brew S, Rezajooi K, Casey A: Osteochondroma of C1 causing vertebral artery occlusion. Br J Neurosurg 27: 130–131, 2013 [DOI] [PubMed] [Google Scholar]
- 20).Zhang Y, Ilaslan H, Hussain MS, Bain M, Bauer TW: Solitary C1 spinal osteochondroma causing vertebral artery compression and acute cerebellar infarct. Skeletal Radiol 44: 299–302, 2015 [DOI] [PubMed] [Google Scholar]
- 21).Fadili S, Clarençon F, Bonneville F, Savatovsky J, Deltour S, Dormont D: Occlusion of vertebral artery due to transverse canal osteochondroma. Clin Neuroradiol 24: 395–397, 2014 [DOI] [PubMed] [Google Scholar]
- 22).Choi KD, Choi JH, Kim JS, et al. : Rotational vertebral artery occlusion: mechanisms and long-term outcome. Stroke 44: 1817–1824, 2013 [DOI] [PubMed] [Google Scholar]
- 23).Matsuyama T, Morimoto T, Sakaki T: Comparison of C1–2 posterior fusion and decompression of the vertebral artery in the treatment of bow hunter’s stroke. J Neurosurg 86: 619–623, 1997 [DOI] [PubMed] [Google Scholar]
- 24).Anene-Maidoh TI, Vega RA, Fautheree GL, Reavey-Cantwell JF: An unusual case of pediatric bow hunter’s stroke. Surg Neurol Int 4: 148, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]