Abstract
Objective
To describe health-related quality of life (HRQOL) and psychological well-being of children and adolescents at enrolment in a multidisciplinary community-based obesity programme and to determine association with ethnicity. This programme targeted indigenous people and those from most deprived households. Further, this cohort was compared with other populations/normative data.
Methods
This study examines baseline demographic data of an unblinded randomised controlled clinical trial. Participants (recruited from January 2012-August 2014) resided in Taranaki, New Zealand, and for this study we only included those with a body mass index (BMI) ≥98th percentile (obese). HRQOL and psychological well-being were assessed using the Pediatric Quality of Life Inventory (PedsQL V.4.0TM) (parent and child reports), and Achenbach’s Child Behavior Checklist (CBCL)/Youth Self Report (YSR).
Results
Assessments were undertaken for 233 participants (45% Māori, 45% New Zealand European, 10% other ethnicities, 52% female, 30% from the most deprived household quintile), mean age 10.6 years. The mean BMI SD score (SDS) was 3.12 (range 2.01–5.34). Total PedsQL generic scaled score (parent) was lower (mean=63.4, SD 14.0) than an age-matched group of Australian children without obesity from the Health of Young Victorians study (mean=83.1, SD 12.5). In multivariable models, child and parental generic scaled scores decreased in older children (β=−0.70 and p=0.031, β=−0.64 and p=0.047, respectively). Behavioural difficulties (CBCL/YSR total score) were reported in 43.5% of participants, with the rate of emotional/behavioural difficulties six times higher than reported norms (p<0.001).
Conclusions
In this cohort, children and adolescents with obesity had a low HRQOL, and a concerning level of psychological difficulties, irrespective of ethnicity. Obesity itself rather than ethnicity or deprivation appeared to contribute to lower HRQOL scores. This study highlights the importance of psychologist involvement in obesity intervention programmes.
Trial registration number
Australian NZ Clinical Trials Registry ANZCTR 12611000862943; Pre-results.
Keywords: paediatric, obesity, adolescent, quality of life, lifestyle intervention, Whānau Pakari
Strengths and limitations of this study.
This study is the first to report health-related quality of life (HRQOL) in children and adolescents with obesity in New Zealand.
To our knowledge, there are very limited data regarding ethnicity and HRQOL. Due to the high participation rate from Māori, we were able to evaluate the impact of ethnicity on HRQOL.
Due to the lack of New Zealand HRQOL data, comparisons have been made with population groups of varying age ranges, which may have affected results.
The study participants were a referred cohort, which means our findings are not representative of the general population. The data from the Victorian cohort were collected in 2000, and the differences noted may have been impacted by the difference in dates of data collection.
Mean body mass index SD score for the Victorian cohort identified as obese was not available, which would be important if it was considerably lower than the Whānau Pakari participants.
There were no adjustments for multiple comparisons in our statistical analyses; due to the inflated likelihood of type 1 errors, our findings (particularly from exploratory analyses) need to be interpreted accordingly.
Introduction
Obesity in childhood and adolescence is known to be associated with weight-related comorbidities.1 Indigenous populations often have higher rates of obesity compared with non-indigenous counterparts where this information has been collated.2 3 In New Zealand, approximately 11% of New Zealand children aged 2–14 years are classed as obese, with Māori (New Zealand’s indigenous population) being 1.6 times more likely to be in the obese range compared with non-Māori counterparts.3 In addition, children living in households in the most socioeconomically deprived quintile for New Zealand are five times more likely to be in the obese range than children living in the least deprived areas.3 In the USA, while rates of children with obesity are not readily available for American Indian populations, rates of type 2 diabetes mellitus (a known weight-related comorbidity) are higher.2
Globally, indigenous populations that have experienced historical trauma secondary to colonisation are over-represented in socioeconomic household deprivation, and both experience the resultant health disparities.2 The social determinants of health, such as poverty, limited educational attainment and critically the loss of a traditional diet, all contribute to the impact on these population groups in terms of health and well-being.2 Overweight and obesity in adolescence have been shown to be strongly associated with medical complications, including an increase in cardiovascular mortality in adulthood.4 Emerging evidence suggests that obesity also affects the emotional health and well-being of children and adolescents, commonly referred to as health-related quality of life (HRQOL).5 However, little is known about the HRQOL of indigenous children and adolescents, especially as it pertains to weight. Previous research has found that Sami (the indigenous people of Sweden) children experience lower HRQOL in some domains compared with Swedish children in general.6 In relation to HRQOL as it pertains to weight, and the impact of ethnicity, it is acknowledged that information about the relationship between HRQOL and weight may not have transferability from one cultural context to another, given differing perceptions of body image cross-culturally.7 8
Quality of life is a broad construct that encompasses various aspects pertaining to health and well-being.9 The assessment of HRQOL is increasingly recognised as a necessary component of health and well-being evaluation, assessing physical, emotional and social health dimensions.10 11 Measurement of HRQOL has been shown to have utility in paediatric healthcare settings encompassing numerous chronic health conditions12–14 and in the assessment of health in young adults.9
Obesity during childhood is associated with impaired HRQOL. In one US study, 106 children and adolescents with severe obesity attending an obesity clinic reported significantly lower HRQOL than 401 healthy weight comparison children recruited through private practice paediatrician offices and health clinics, and similar HRQOL to 106 children and adolescents undergoing chemotherapy for cancer.15 The HRQOL of 9–12-year-old children enrolled in an Australian community-based longitudinal study was significantly lower among those with obesity versus those without obesity, with the differences not as marked as in the US study, but more likely to represent those of children with obesity not being seen in a specialised clinic setting.16 Pooled results from 22 cross-sectional and population-based studies report that children and adolescents with obesity have reduced overall HRQOL compared with normal weight counterparts, with 12 of these studies demonstrating an inverse relationship between overall HRQOL and weight status.5 Potential factors contributing to HRQOL in child and adolescent populations with obesity include treatment seeking versus community counterparts, gender, age and weight-related comorbidities.5
Alongside, and likely to be contributing to lower HRQOL, children and adolescents with obesity are at increased risk of behavioural and emotional difficulties. In addition to differences in HRQOL, studies have found concerning levels of internalising (anxiety/depression, social withdrawal and somatic complaints) and externalising behaviours (delinquency and rule-breaking behaviours) in children and adolescents with obesity.17 18 Others have identified higher rates of depression, behavioural problems and low self-esteem in adolescents with obesity attending obesity clinics compared with affected counterparts in the community.19 Children who are overweight and obese have also been shown to be at risk for psychosocial difficulties such as body image concerns, and emotional, social and school difficulties.20
Currently there are no published data on the HRQOL of children and adolescents with obesity in New Zealand. To our knowledge, there has only been quality of life data published on oral quality of life as it relates to dental caries,21 and Type 1 diabetes in New Zealand.14 In addition, there is an absence of cross-cultural evaluation of obesity and HRQOL. In this study, we aimed to describe the HRQOL (parent and child reports) and behavioural and emotional problems of children and adolescents with obesity at enrolment in a multidisciplinary obesity intervention programme. In addition, we compared this cohort to other populations or to normative data, and also examined potential ethnic differences between indigenous and non-indigenous children and adolescents. It was hypothesised that obesity is associated with lower HRQOL in New Zealand children and adolescents with obesity.
Methods
Children and adolescents were recruited into ‘Whānau Pakari’, a community-based, unblinded randomised controlled trial of a multidisciplinary obesity intervention programme,22 based in Taranaki (New Zealand). This region has a population of 23 139 children aged 0–15 years, of whom 81% identify as New Zealand European, 28% as Māori and 1% as other ethnicity.23 Eligibility was defined by residence in Taranaki, being aged 4.8–16.8 years, and either in obese (body mass index (BMI) ≥98th centile) or overweight (BMI >91st centile) categories with weight-related comorbidities.24 However, only obese participants were included in the study reported here. Referrals were received between January 2012 and August 2014 from a wide range of health professionals (including paediatricians, primary care providers and public health nurses), Māori health workers, school counsellors and self-referrals. This study examines elements of the baseline demographic data.
Assessments
Participants underwent a baseline assessment at home, which included taking anthropometric measurements, a medical history and weight-related physical examination, dietary history, physical activity questionnaire and completion of psychometric questionnaires. Questions pertaining to family structure, developmental history, presence/absence of headaches, difficulty getting to sleep and presence/absence of breathing pauses were all included in the weight-related medical history. Randomisation into six monthly assessments and advice or the intervention arm occurred if the participants indicated willingness to make healthy lifestyle change.22 The intervention consisted of weekly sessions delivered by a multidisciplinary team for 12 months including physical activity, dietary advice and psychology sessions (e.g., self-esteem, the importance of sleep, how to make and persist with healthy lifestyle change).
Measures
BMI percentile and SD score (SDS) were calculated using UK Cole normative data25 with the KIGS auxology software (Pfizer Endocrine CareTM). Socioeconomic deprivation was measured at the household level using the New Zealand Deprivation Index 2006.26 This area-level deprivation index is a well-validated measure of socioeconomic deprivation in New Zealand, which is derived from national census data on nine socioeconomic characteristics.
Quality of life was measured using the Pediatric Quality of Life Inventory (PedsQL), which has been specifically designed to evaluate HRQOL in children and adolescents. The PedsQL questionnaire has both parent-proxy and child self-report versions, which take approximately 5 min to administer. It consists of a 23-item Generic Core Scale that assesses problems over the preceding month related to Physical, Emotional, Social and School functioning.11 13 The reliability of this instrument has been demonstrated in ages 2–16 years as excellent (α=0.89 child; 0.92 parent report) with acceptable construct validity, in a large population survey in the USA (n=10 241), with white, Hispanic/Latino, black/African American, Asian/Pacific Islander, American Indian and Native Alaskan participants.27 A meaningful cut-off to identify those at risk of impaired HRQOL has been proposed as one SD below the population mean.27 Individual questions for each area are reverse scored and linearly transformed into a 0–100 scale, where higher scores indicate better HRQOL.
The existence of behavioural difficulties was assessed using Achenbach’s Child Behavior Checklist (CBCL) ages 1.5–5 and ages 6–18 (parent report) and Youth Self Report (YSR) for ages 11–18.28 The CBCL/YSR generate ratings of behavioural, emotional and social problems. The CBCL can be completed by parents, caregivers or others who see children in family contexts, or by the young person themselves in the case of the YSR. When the young person completed the YSR, no parent CBCL report was obtained in order to reduce the burden of assessment on the family. Subscale scores for the YSR and the CBCL are calculated for a number of behavioural and psychological problems such as aggressive behaviour, and somatic complaints. Subscales are then combined to obtain overall T-scores for internalising and externalising problems. Aggregate scores that represent normal, borderline or clinical behaviour are based on quartiles from a normative sample.28 The normative data for the CBCL/YSR have been derived from the 1999 National Survey of Children, Youth and Adults, a US population survey of 2029 children and adolescents of four ethnic groups (60% Latino white, 20% African American, 12% Mixed other and 9% Latino), of mixed socioeconomic status (33% ‘upper’, 16% ‘lower’), equal gender split and ranging in age from 6 to 18 years.29
Data analyses
PedsQL scores from the children and adolescents enrolled in this study were compared with three populations using two-sample t-tests. These comparison populations were:
A predominantly normal weight cohort of children from the Taranaki region (n=42) with a long-term chronic condition (Type 1 diabetes), with a mean age of 11.5 years (range 2–17 years), who were predominantly of New Zealand European (71%) or Māori (19%) ethnicity, and with representation from all levels of household deprivation.14 This cohort was used as they were resident in the same region as Whānau Pakari participants, and the only group of New Zealand children for which published HRQOL data using PedsQL exists. Recruitment period was May-July 2013.
A cohort of Australian children (n=63) from the Health of Young Victorians Study (follow-up data collected in 2000), who were identified as having obesity (from the total cohort of n=1456).16 We used Australian data due to the lack of New Zealand data available.
A cohort of Australian children from the above study (follow-up data collected in 2000), identified as having normal weight (n=1099, from the total cohort of n=1456). The children in the entire Health of Young Victorians cohort were aged 10.4 years (range 9–12 years), with representation from all quintiles of socioeconomic disadvantage, but ethnicity of participants was not reported.16 Given that developmental stage may be a contributing factor to HRQOL scores,5 30 the Whānau Pakari cohort comparison was limited to 9–12 years (n=91).
Exploratory analyses of the PedsQL data examined potential associations between a number of sociodemographic and clinical parameters with parental and child's generic scaled scores separately, using simple linear regressions and one-way analysis of variance. Further, multivariable models were used to examine possible associations between either parental or child’s generic scaled score and important confounding factors, namely age, sex, ethnicity and socioeconomic deprivation.
CBCL and YSR T-scores were used. One-tailed one-sample proportion tests were used to compare the rates of participants classified as borderline clinical or clinical in each CBCL/YSR subscale to the normative data (i.e., expected to be ≤7% of the population). Exploratory analyses using generalised linear regression models also examined the likelihood of displaying behavioural and emotional problems (i.e., having CBCL/YSR scores in the borderline or clinical ranges) in association with certain demographic parameters, adjusting only for source of test scores (i.e., parent or youth). A similarly constructed multivariable model was also run adjusting for age, sex, ethnicity and socioeconomic deprivation. These results are provided as relative risks (RR) and respective 95% CIs. Data were analysed in Minitab V.16 (Pennsylvania State University, State College, Pennsylvania, USA) and SAS V.9.4. All statistical tests (except one-sample proportion tests) were two-tailed. Significance level was maintained at p<0.05, with no adjustments for multiple comparisons.
Results
After exclusion of six participants who were in the overweight category, enrolled participants (n=233) had a mean age of 10.6 years (range 4.8–16.8 years), 52% were females and the sample was predominantly either of Māori (45%) or New Zealand European (45%) ethnicity. Nearly a third (30%) resided in households among the most deprived quintile (compared with 15% among the population of Taranaki).26 31 32 Forty-two per cent of Māori participants were from the most deprived quintile of household deprivation, compared with 20% of New Zealand European participants (p<0.001). BMI SDS at enrolment was 3.12 (SD 0.57, range 2.01–5.34 SDS). Demographics of family and medical history have been previously reported for the total cohort.33 In brief, among our 233 participants, living arrangements included a two-parent household for half of the participants (n=119, 52%), one-parent household (mother) for 38% (n=87), one-parent household (father) for 4% (n=10) and other arrangement for 6% (n=14). Headaches were prevalent in 32% (n=75), 32% of participants had difficulties getting to sleep (n=75), 20% had breathing pauses (n=47) and 9% had developmental concerns (n=20).
Quality of life
The PedsQL scores of our study’s participants and those of another study population in Taranaki are shown in table 1. There was a moderately positive correlation between overall quality of life scores derived from child compared with parental reports (r=0.55; p<0.001). However, for all three PedsQL measures, parents scored their children's HRQOL as being lower than that reported by the participants themselves (table 1).
Table 1.
Unadjusted Pediatric Quality of Life Inventory total generic scaled scores, as well as psychosocial and physical scaled scores (out of 100) for Whānau Pakari participants compared with other Taranaki children with Type 1 diabetes (predominantly normal weight)14
| Whānau Pakari | Type 1 diabetes | |
| Location | Taranaki, New Zealand | Taranaki, New Zealand |
| Source | This study | Mills et al 14 |
| n | 233 | 42 |
| Age range (years) | 4.8–16.8 | 2–17 |
| Child | ||
| Total generic scaled score | 72.2±16.2 (70.1 to 74.3)* | 74.6±15.3 |
| Psychosocial scaled score | 69.4±18.6 (67.0 to 71.8)* | 71.2±17.1 |
| Physical scaled score | 76.9±16.7 (74.8 to 79.1)* | 80.8±15.3 |
| Parent | ||
| Total generic scaled score | 65.1±16.0 (63.0 to 67.1) | 75.9±13.4† |
| Psychosocial scaled score | 64.1±17.3 (61.9 to 66.3) | 73.7±13.1† |
| Physical scaled score | 66.3±20.3 (63.6 to 68.9) | 79.9±17.9† |
Whānau Pakari data are mean ± SD (95% CI of the mean), while other data are mean ± SD.
*p<0.001 for a difference between child and parental scores
†p<0.001 for comparison with Whānau Pakari.
The Whānau Pakari participants reported similar HRQOL scores to Taranaki youth who were predominantly normal weight but with a chronic condition14 (table 1). However, youth with obesity in Whānau Pakari had consistently lower HRQOL scores than normal weight Australian children (p<0.001; table 2), and a community sample with obesity.16 Whānau Pakari parents reported that their children had lower HRQOL than those reported by the parents of all three of the comparison groups (p<0.001; tables 1 and 2).
Table 2.
Unadjusted Pediatric Quality of Life Inventory total generic scaled scores, as well as psychosocial and physical scaled scores (out of 100) for Whānau Pakari participants aged 9–12 years, compared with children and adolescents of two reference populations with a matching age range14 16
| Whānau Pakari | Normal weight | Obese | |
| Location | Taranaki, New Zealand | Victoria, Australia | Victoria, Australia |
| Source | This study | Williams et al 16 | Williams et al 16 |
| n | 91 | 1099 | 63 |
| Age range (years) | 9–12 | 9–12 | 9–12 |
| Child | |||
| Total generic scaled score | 69.0±15.9 (65.7 to 72.3)‡ | 80.5±12.2*** | 74.0±14.2* |
| Psychosocial scaled score | 65.8±18.4 (61.9 to 69.6)† | 77.7±14.1*** | 72.1±14.1* |
| Physical scaled score | 74.9±15.7 (71.6 to 78.2)‡ | 85.7±12.4*** | 77.5±17.9 |
| Parent | |||
| Total generic scaled score | 63.4±14.0 (60.5 to 66.3) | 83.1±12.5*** | 75.0±14.5*** |
| Psychosocial scaled score | 61.5±15.1 (58.4 to 64.7) | 77.6±14.5*** | 73.9±15.3*** |
| Physical scaled score | 66.7±17.7 (63.0 to 70.3) | 87.8±14.3*** | 76.3±17.6** |
*p<0.05, **p<0.01 and ***p<0.001 for comparison with Whānau Pakari
†p<0.05 and ‡p<0.001 for a difference between child and parental scores
Whānau Pakari data are mean±SD (95% CI of the mean), while other data are mean ± SD.
Exploratory analyses showed consistent associations between child and parent total generic scaled scores, and certain sociodemographic and clinical parameters, indicating worse overall quality of life with participants who had breathing pauses (p=0.0439 child and p<0.001 parent, respectively), reported difficulty getting to sleep (p=0.019 and p<0.001), history of headaches (p=0.023 and p=0.022), developmental problems (p<0.001 and p<0.001), and a father being identified as the sole/primary caregiver as opposed to children living in two-parent families (p=0.010 and p=0.031). In multivariable models, there was evidence that child and parental generic scaled scores decreased in older children (β=−0.70 and p=0.031, β=−0.64 and p=0.047, respectively), but there were no apparent associations with sex, ethnicity or household deprivation within our cohort.
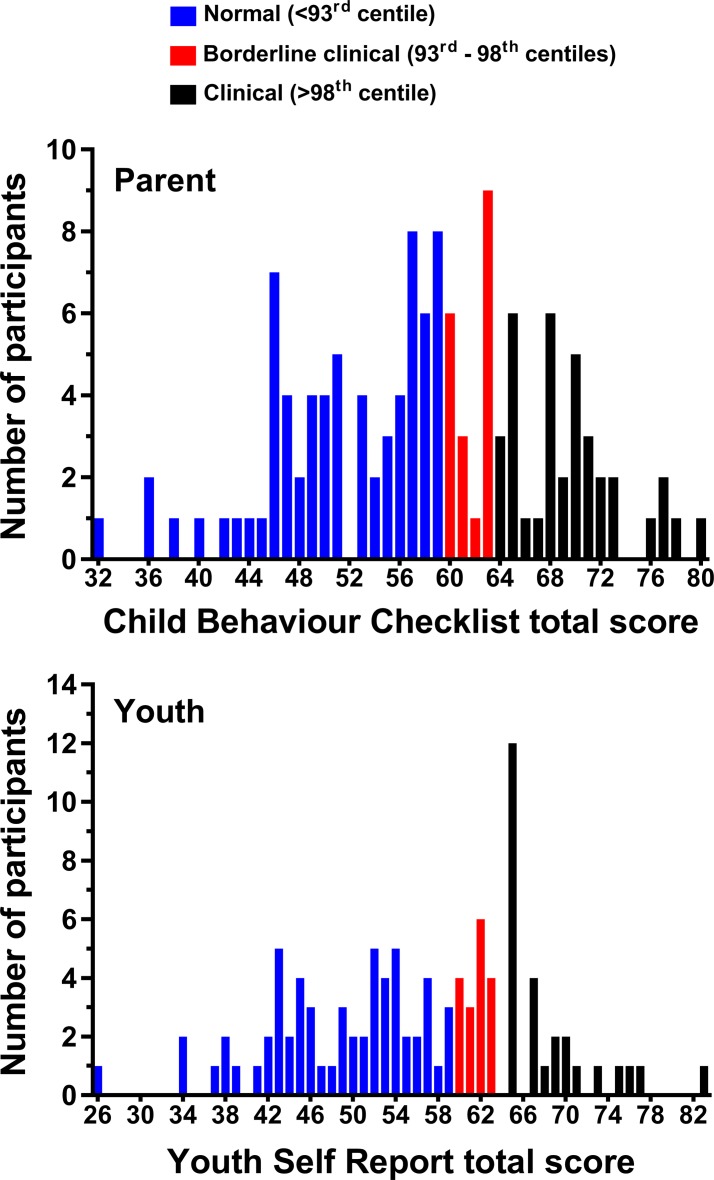
Child Behaviour Checklist
Of the total cohort for this study, 232 participants/parents completed the CBCL/YSR. The median CBCL/YSR total score was 58 (IQR 15.0). The distribution of participants’ scores is shown in figure 1.
Figure 1.
Frequency distribution of participants according to Achenbach's Child Behavior Checklist and Youth Self Report total scores.
Just over half of the participants had CBCL/YSR total scores in the normal range (56.5%), while the remaining 43.5% had scores in the borderline clinical (15.5%) and clinical (28.0%) ranges (figure 1 and table 3). From US normative data previously described, the overall proportion of population falling into the borderline clinical or clinical range is ≤7%.29 This means that children in our study had a prevalence of emotional and behavioural problems that was more than six times higher (p<0.001) than normative populations.
Table 3.
Proportion of participants with T-scores from Child Behaviour Checklist (CBCL)/Youth Self Report (YSR) falling into normal, borderline clinical and clinical ranges at baseline, as per parental and youth assessments
| Assessment | CBCL/YSR subscale | n | Normal* | Borderline clinical† | Clinical‡ |
| Parent | Anxious | 128 | 110 (85.9%)§ | 8 (6.3%) | 10 (7.8%) |
| Withdrawn | 128 | 92 (71.9%)§ | 26 (20.3%) | 10 (7.8%) | |
| Somatic complaints | 128 | 98 (76.6%)§ | 20 (15.6%) | 10 (7.8%) | |
| Social difficulties | 100 | 70 (7.0%)§ | 20 (20.0%) | 10 (10.0%) | |
| Thought problems | 100 | 80 (80.0%)§ | 7 (7.0%) | 13 (13.0%) | |
| Attention difficulties | 128 | 110 (85.9%)§ | 9 (7.0%) | 9 (7.0%) | |
| Rule breaking | 100 | 76 (76.0%)§ | 16 (16.0%) | 8 (8.0%) | |
| Aggressive | 128 | 102 (79.7%)§ | 18 (14.1%) | 8 (6.3%) | |
| Internalising | 128 | 68 (53.1%)§ | 22 (17.2%) | 38 (29.7%) | |
| Externalising | 128 | 72 (56.3%)§ | 24 (18.8%) | 32 (25.0%) | |
| Total | 128 | 71 (55.5%)§ | 19 (14.8%) | 38 (29.7%) | |
| Youth | Anxious | 104 | 88 (84.6%)§ | 12 (11.5%) | 4 (3.9%) |
| Withdrawn | 104 | 79 (76.0%)§ | 16 (15.4%) | 9 (8.7%) | |
| Somatic complaints | 104 | 79 (76.0%)§ | 15 (14.4%) | 10 (9.7%) | |
| Social difficulties | 104 | 84 (80.8%)§ | 11 (10.6%) | 9 (8.7%) | |
| Thought problems | 104 | 93 (89.4%)§ | 8 (7.7%) | 3 (2.9%) | |
| Attention difficulties | 104 | 81 (77.9%)§ | 15 (14.4%) | 8 (7.7%) | |
| Rule breaking | 104 | 86 (82.7%)§ | 16 (15.4%) | 2 (1.9%) | |
| Aggressive | 104 | 91 (87.5%)§ | 7 (6.7%) | 6 (5.8%) | |
| Internalising | 104 | 62 (59.6%)§ | 15 (14.4%) | 27 (26.0%) | |
| Externalising | 104 | 76 (73.1%)§ | 10 (9.6%) | 18 (17.3%) | |
| Total | 104 | 60 (57.7%)§ | 17 (16.4%) | 27 (26.0%) |
Data are n (%).
*<65 which is below 93rd centile.
†65–70 which is 93–98th centile (apart from internalising/externalising/total 60–63).
‡>70 which is 98th centile (apart from internalising/externalising/total >63).
§p<0.001 for comparison with normative data (i.e., expected ≤7% of participants in borderline clinical or clinical ranges combined).
The classification of participants according to individual CBCL/YSR subscales (both parent report and youth report) are shown in table 3. Missing data on subscales for parent report are due to the absence of these subscales in the questionnaire for those aged 1.5–5 years. Based on CBCL/YSR findings, children and adolescents in our cohort were significantly more likely to display emotional and behavioural difficulties than those in the general population. Compared with normative data, the proportion of participants in borderline clinical or clinical ranges was considerably greater for all subscales (table 3).
Exploratory analyses showed a higher probability of behavioural and emotional problems (as per CBCL/YSR total scores) in those who experienced breathing pauses (RR 1.52, 95% CI 1.13 to 2.04) or displayed developmental problems (RR 1.59, 95% CI 1.11 to 2.27). Multivariable analyses showed that older age at assessment was associated with higher CBCL/YSR total scores (ie, worse scores) (β=0.89; p=0.011), while males were more likely to display behavioural and emotional problems than females (RR 1.43, 95% CI 1.06 to 1.94).
Ethnic comparisons
There were no differences between Māori and New Zealand European participants with obesity with respect to the child’s reported overall PedsQL scores (p=0.09) or PedsQL psychosocial (p=0.14) scores, but Māori children reported higher PedsQL physical scores (80.1 vs 74.7, respectively, p=0.019). With respect to parental report, there were no ethnic differences in total quality of life (p=0.81), psychosocial (p=0.76) or physical (p=0.53) scores. There were no differences between Māori and New Zealand European participants on CBCL/YSR total (p=0.25), internalising (p=0.12) or externalising (p=0.71) scores.
Discussion
The main findings of this study were that children and adolescents with obesity in this region of New Zealand had lower HRQOL on parent report measures when compared with those with a chronic condition (i.e., diabetes that requires daily testing and treatment) and other samples with and without obesity. In addition, a large proportion (43.5%) obtained CBCL/YSR scores in the clinical and borderline range for experiencing psychological problems. The parent report quality of life scores were not dissimilar to those described in children with obesity attending a specialist clinic, and were similar to children and adolescents diagnosed with cancer.15 The degree to which HRQOL appeared to be affected in our cohort was not surprising, given that treatment-seeking parents of children with obesity are more likely to perceive their child as having a poorer HRQOL and more psychological difficulties when compared with parents of children with obesity in the community not seeking treatment.5 34 Our cohort consisted of participants referred to an obesity intervention programme, so were not a true community-based sample. Nor were they directly comparable to a hospital outpatient clinic population given that Whānau Pakari was specifically designed to address barriers to access which exist for hospital-based outpatient clinical care, particularly for indigenous children.22 Allowing for this not being a complete non-referred sample, the difference in HRQOL scores in our cohort compared with a large population-based study (n=10 241) of predominantly normal weight children aged 2–16 years (mean score 65.4 vs 81.3) is considerable.35
Differences between parent-proxy and child self-report on PedsQL questionnaires have been previously reported. A systematic review of the relationship between parents and children’s HRQOL scores found better agreement among parents and chronically sick children than between parents and their healthy children.36 It was argued that both parent and child reports should be obtained as they provide different perspectives. A further review noted differences in parent–child agreement in HRQOL across four different instruments.37 The authors suggested that the disagreement was a consequence of varying individual beliefs about the child’s health and well-being, rather than parent or child reports being wrong or right.37 A Norwegian study reviewed this in relation to children and adolescents seeking treatment for obesity versus a community sample of children of any BMI.34 Parents reported the quality of life of the children with obesity seeking treatment as lower than those in the community, which was not seen with the child self-report.34 Pooled analyses however showed that paediatric HRQOL can be accurately predicted from parent proxy reports with moderate to strong linear relationships between the two methods of report.5
We observed that psychological difficulties were prevalent in our cohort. Our participants aged 11–18 years reported a mean total YSR score of 55.9 (SD 10.6), which is similar to a small non-clinical group of adolescents with obesity from Turkey (n=30) with a total problem score of 58.2 (SD 7.7).19 We have no national data for comparison with CBCL/YSR, but there is nothing to suggest that scores in the Taranaki region would be higher than those nationally, and there is no known biological or environmental reason for this cohort to have higher rates of mental health problems outside of their obesity. The absence of paediatric psychology services at the time of this study is a notable issue in the region (child and adolescent mental health services were available), and it is unclear if this may contribute to these findings. The randomised clinical trial we are undertaking will be able to assess if the intervention can address the relationships between these variables over time.
Obesity in childhood is a major health concern in New Zealand, with the third highest prevalence of overweight and obesity in the Organisation for Economic Co-operation and Development.38 Recent studies in this cohort of children and adolescents with obesity have found suboptimal eating behaviour,39 suboptimal physical activity40 and a high prevalence of weight-related comorbidities, including hypertension and obstructive sleep apnoea.33 We were not surprised that breathing pauses were associated with poorer HRQOL and higher total scores on the CBCL/YSR. Breathing pauses in children and adolescents with obesity are associated with obstructive sleep apnoea,41 and children and adolescents with obesity with this condition have reported lower HRQOL total scores than peers with obesity without the condition.15 Moderate to severe obstructive sleep apnoea is associated with increased rates of aggressive behaviour, attention problems and internalising problems on the CBCL.42 These observations are important, given the considerable prevalence of breathing pauses reported in this cohort with obesity,33 and the wider impact of obstructive sleep apnoea on a child’s health, cognitive and behavioural functioning.43
Strengths of this study are that it is the first to report HRQOL in children and adolescents with obesity in the New Zealand population. Due to the high participation rate from Māori, we were also able to undertake evaluation of the impact of ethnicity. What was interesting and important about our findings in terms of ethnicity was the lack of disparity in HRQOL scores. This was despite a larger proportion of Māori participants being from the most deprived quintile of households. It therefore appears that obesity itself rather than factors such as deprivation is the main identified factor in our participants contributing to lower HRQOL scores. This finding is in contrast to previous research in Fiji and Kuwait, where there was no meaningful negative association between increased weight and HRQOL in children aged 12–18 in Fiji, irrespective of ethnicity, or Kuwaiti nationals, aged 10–14 years.7 8 The discrepancies in results may be explained by this study reviewing a treatment-seeking group, rather than population-based sample, and the different cultural values assigned to body size in Fiji and Kuwait compared with New Zealand (a predominantly westernised society).
A limitation of this study, as with all HRQOL assessments, is the use of an assessment tool to extrapolate one’s psychological health and well-being. Comparisons of our study have been made with population groups of varying age ranges, which may have affected results. Another limitation of this study is that this was a referred cohort, which means our findings are not necessarily representative of the general population, and therefore generalisability of findings to wider population groups is reduced. We compared our data with the Health of Young Victorians cohort from Australia, as this was the most comparable group we had access to. However, the data were collected in 2000, and the differences noted may have been impacted by the difference in dates of data collection. Mean BMI SDS for the Victorian cohort with obesity was not available, which would be important if it was considerably lower than the Whānau Pakari participants. Lastly, we made no adjustments for multiple comparisons in our statistical analyses, so that the findings (particularly from exploratory analyses) need to be interpreted accordingly.
In conclusion, this study highlights a lower HRQOL and a higher prevalence of psychological difficulties for this referred community-based group of children and adolescents with obesity compared with normative population data. No differences were found between Māori and New Zealand Europeans. This is despite Māori being represented in greater numbers in the more deprived households of the region compared with their non-Māori counterparts, suggesting that obesity itself rather than deprivation is the main contributor to lower HRQOL scores. This study highlights the importance of psychologist involvement and screening in the child and adolescent population with obesity as part of any multi-disciplinary team. Improvement in HRQOL should be considered a goal of all child and adolescent obesity intervention and management. Further research is required to ascertain how to maximise improvements in what is now recognised as an important health outcome.
Supplementary Material
Acknowledgments
The authors would like to acknowledge Dr John Doran (Taranaki District Health Board), Diana O’Neill and Dr Pat Tuohy (Ministry of Health) for their support of the trial; Taranaki District Health Board and Sport Taranaki for funding of the clinical service, and Gerard Dolan and Dr Rebecca Storey for their assistance with initial methodology surrounding psychology questionnaires. The Quality of Life study described in this paper was carried out using the PedsQL, developed by Dr James W. Varni.
Footnotes
Contributors: YCA designed the study, was involved with data interpretation and drafted this manuscript. LEW recruited participants and undertook assessments and data entry. KFT provided psychologist oversight and analysis of patient data. CCG is secondary supervisor for the research team and assisted with the design of the study. JMS was involved in study design. TLC assisted with data entry and analysis. TAW was involved in interpretation of data. JGBD analysed the data and drafted the manuscript. WSC contributed to study design. PLH contributed to study design and supervises the research team. All authors critically revised the manuscript, gave final approval for the version to be published and are accountable for all aspects of the work.
Funding: This work has been funded by grants from the Health Research Council of New Zealand, Royal Australasian College of Physicians, the Maurice and Phyllis Paykel Trust, Taranaki Medical Foundation and Lotteries Health Research.
Competing interests: YCA and PLH have been recipients of these grants to undertake clinical research in relation to Whānau Pakari, YCA has been paid in a fellowship capacity from the Health Research Council of New Zealand, TLC has been paid as a research assistant, JGBD has been paid for data analysis.
Patient consent: Obtained.
Ethics approval: Ethics approval for the programme was granted by the New Zealand Health and Disability Ethics Committee (CEN/11/09/054). Written and verbal informed consents were obtained from all participants or their guardians. The trial was registered with the Australian New Zealand Clinical Trials Registry (ANZCTR: 12611000862943).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Anonymised and deidentified data will be made available to other investigators upon request. Interested readers should contact the senior author PH (p.hofman@auckland.ac.nz) to obtain the data.
References
- 1. Lakshman R, Elks CE, Ong KK. Childhood obesity. Circulation 2012;126:1770–9. 10.1161/CIRCULATIONAHA.111.047738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Smylie J, Adomako P. Indigenous children's health report: Health assessment in action. Toronto: The Centre for Research on Inner City Health, 2009. http://www.stmichaelshospital.com/crich/wp-content/uploads/ichr_report-web.pdf (accessed 16 Nov 2014). [Google Scholar]
- 3. Ministry of Health, New Zealand. Annual Update of Key results 2014/2015: New New Zealand Health Survey. Wellington, New Zealand: Ministry of Health, 2015. http://www.health.govt.nz/system/files/documents/publications/annual-update-key-results-2014-15-nzhs-dec15-1.pdf (accessed 12 Apr 2016). [Google Scholar]
- 4. Twig G, Yaniv G, Levine H, et al. Body-Mass Index in 2.3 Million Adolescents and Cardiovascular Death in Adulthood. N Engl J Med 2016;374:2430–40. 10.1056/NEJMoa1503840 [DOI] [PubMed] [Google Scholar]
- 5. Tsiros MD, Olds T, Buckley JD, et al. Health-related quality of life in obese children and adolescents. Int J Obes 2009;33:387–400. 10.1038/ijo.2009.42 [DOI] [PubMed] [Google Scholar]
- 6. Omma L, Petersen S. Health-related quality of life in Indigenous Sami schoolchildren in Sweden. Acta Paediatr 2015;104:75–83. 10.1111/apa.12786 [DOI] [PubMed] [Google Scholar]
- 7. Petersen S, Moodie M, Mavoa H, et al. Relationship between overweight and health-related quality of life in secondary school children in Fiji: results from a cross-sectional population-based study. Int J Obes 2014;38:539–46. 10.1038/ijo.2013.212 [DOI] [PubMed] [Google Scholar]
- 8. Boodai SA, Reilly JJ. Health related quality of life of obese adolescents in Kuwait. BMC Pediatr 2013;13:105 10.1186/1471-2431-13-105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Varni JW, Limbers CA. The PedsQL 4.0 Generic Core Scales Young adult Version: feasibility, reliability and validity in a university student population. J Health Psychol 2009;14:611–22. 10.1177/1359105309103580 [DOI] [PubMed] [Google Scholar]
- 10. Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 2001;39:800–12. 10.1097/00005650-200108000-00006 [DOI] [PubMed] [Google Scholar]
- 11. Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care 1999;37:126–39. 10.1097/00005650-199902000-00003 [DOI] [PubMed] [Google Scholar]
- 12. Chan KS, Mangione-Smith R, Burwinkle TM, et al. The PedsQL: reliability and validity of the short-form generic core scales and Asthma Module. Med Care 2005;43:256–65. [DOI] [PubMed] [Google Scholar]
- 13. Varni JW, Seid M, Knight TS, et al. The PedsQL 4.0 generic core scales: sensitivity, responsiveness, and impact on clinical decision-making. J Behav Med 2002;25:175–93. 10.1023/A:1014836921812 [DOI] [PubMed] [Google Scholar]
- 14. Mills SA, Hofman PL, Jiang Y, et al. Health-related quality of life of Taranaki children with type 1 Diabetes. N Z Med J 2015;128:25–32. [PubMed] [Google Scholar]
- 15. Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. JAMA 2003;289:1813–9. 10.1001/jama.289.14.1813 [DOI] [PubMed] [Google Scholar]
- 16. Williams J, Wake M, Hesketh K, et al. Health-related quality of life of overweight and obese children. JAMA 2005;293:70–6. 10.1001/jama.293.1.70 [DOI] [PubMed] [Google Scholar]
- 17. Giel KE, Zipfel S, Schweizer R, et al. Eating Disorder pathology in adolescents participating in a lifestyle intervention for obesity: associations with weight change, general psychopathology and health-related quality of life. Obes Facts 2013;6:307–16. 10.1159/000354534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pervanidou P, Bastaki D, Chouliaras G, et al. Internalizing and externalizing problems in obese children and adolescents: associations with daily salivary cortisol concentrations. Hormones 2015;14:623–31. 10.14310/horm.2002.1602 [DOI] [PubMed] [Google Scholar]
- 19. Erermis S, Cetin N, Tamar M, et al. Is obesity a risk factor for psychopathology among adolescents? Pediatr Int 2004;46:296–301. 10.1111/j.1442-200x.2004.01882.x [DOI] [PubMed] [Google Scholar]
- 20. Lim CS, Espil FM, Viana AG, et al. Associations between anxiety symptoms and child and Family factors in Pediatric Obesity. J Dev Behav Pediatr 2015;36:664–72. 10.1097/DBP.0000000000000225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Foster Page LA, Thomson WM. Caries prevalence, severity, and 3-year increment, and their impact upon New Zealand adolescents' oral-health-related quality of life. J Public Health Dent 2012;72:287–94. 10.1111/j.1752-7325.2012.00336.x [DOI] [PubMed] [Google Scholar]
- 22. Anderson YC, Wynter LE, Moller KR, et al. The effect of a multi-disciplinary obesity intervention compared to usual practice in those ready to make lifestyle changes: design and rationale of Whanau Pakari. BMC Obes 2015;2 10.1186/s40608-015-0068-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Statistics New Zealand. Census 2013: ethnic group by age group and sex [Internet. Wellington: Statistics New Zealand; http://nzdotstat.stats.govt.nz/wbos/Index.aspx?DataSetCode=TABLECODE8021# (accessed 18 November 2014). [Google Scholar]
- 24. Cole TJ. A chart to link child centiles of body mass index, weight and height. Eur J Clin Nutr 2002;56:1194–9. 10.1038/sj.ejcn.1601473 [DOI] [PubMed] [Google Scholar]
- 25. Freeman JV, Cole TJ, Chinn S, et al. Cross sectional stature and weight reference curves for the UK, 1990. Arch Dis Child 1995;73:17–24. 10.1136/adc.73.1.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. University of Otago - School of Medicine and Health Science, New Zealand. NZ Deprivation Index. 2006. https://koordinates.com/layer/1066-nz-deprivation-index-2006/ (accessed 03 Nov 2014).
- 27. Varni JW, Burwinkle TM, Seid M, et al. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr 2003;3:329–41. [DOI] [PubMed] [Google Scholar]
- 28. Achenbach TM, Ruffle TM. The Child Behavior Checklist and related forms for assessing behavioral/emotional problems and competencies. Pediatr Rev 2000;21:265–71. 10.1542/pir.21-8-265 [DOI] [PubMed] [Google Scholar]
- 29. Achenbach TM, Rescorla LA. Manual for the ASEBA school-aged forms and profiles. Research Centre for Children, Youth & families. Burlington: University of Vermont, 2001. [Google Scholar]
- 30. Jansen PW, Mensah FK, Clifford S, et al. Bidirectional associations between overweight and health-related quality of life from 4-11 years: longitudinal Study of Australian Children. Int J Obes 2013;37:1307–13. 10.1038/ijo.2013.71 [DOI] [PubMed] [Google Scholar]
- 31. Ministry of Health, New Zealand. Population of Taranaki DHB. Wellington, New Zealand, 2015. http://www.health.govt.nz/new-zealand-health-system/my-dhb/taranaki-dhb/population-taranaki-dhb (accessed 26 Jan 2015). [Google Scholar]
- 32. Atkinson J, Salmond C, Crampton C. NZDep2013 Index of Deprivation. Wellington, New Zealand: University of Otago, 2014. http://www.otago.ac.nz/wellington/otago069936.pdf (accessed 03 Apr 2016). [Google Scholar]
- 33. Anderson YC, Wynter LE, Treves KF, et al. Prevalence of comorbidities in obese New Zealand children and adolescents at enrolment in a community-based obesity programme. J Paediatr Child Health 2016;52:1099–105. 10.1111/jpc.13315 [DOI] [PubMed] [Google Scholar]
- 34. Steinsbekk S, Jozefiak T, Ødegård R, et al. Impaired parent-reported quality of life in treatment-seeking children with obesity is mediated by high levels of psychopathology. Qual Life Res 2009;18:1159–67. 10.1007/s11136-009-9535-6 [DOI] [PubMed] [Google Scholar]
- 35. Seid M, Varni JW, Cummings L, et al. The impact of realized access to care on health-related quality of life: a two-year prospective cohort study of children in the California State Children's Health Insurance Program. J Pediatr 2006;149:354–61. 10.1016/j.jpeds.2006.04.024 [DOI] [PubMed] [Google Scholar]
- 36. Eiser C, Morse R. Can parents rate their child's health-related quality of life? Results of a systematic review. Qual Life Res 2001;10:347–57. 10.1023/A:1012253723272 [DOI] [PubMed] [Google Scholar]
- 37. Upton P, Lawford J, Eiser C. Parent-child agreement across child health-related quality of life instruments: a review of the literature. Qual Life Res 2008;17:895–913. 10.1007/s11136-008-9350-5 [DOI] [PubMed] [Google Scholar]
- 38. Organisation for Economic Co-operation and development (OECD. France: Secretary-General of the OECD, 2014. http://www.oecd.org/els/health-systems/Obesity-Update-2014.pdf (accessed 21 Feb 2015). [Google Scholar]
- 39. Anderson YC, Wynter LE, Butler MS, et al. Dietary intake and Eating Behaviours of obese New Zealand Children and Adolescents Enrolled in a Community-Based intervention Programme. PLoS One 2016;11:e0166996 10.1371/journal.pone.0166996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Anderson Y. C, Wynter L. E, Grant C. C, et al. Physical activity is low in obese New Zealand children and adolescents. Sci Rep 2017; 7:41822 10.1038/srep41822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Section on Pediatric Pulmonology, Subcommittee on Obstructive Sleep Apnea Syndrome. American Academy of Pediatrics. Clinical practice guideline: diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 2002;109:704–12. [DOI] [PubMed] [Google Scholar]
- 42. Bourke RS, Anderson V, Yang JS, et al. Neurobehavioral function is impaired in children with all severities of sleep disordered breathing. Sleep Med 2011;12:222–9. 10.1016/j.sleep.2010.08.011 [DOI] [PubMed] [Google Scholar]
- 43. Schechter MS. Section on Pediatric Pulmonology, Subcommittee on Obstructive Sleep Apnea syndrome. Technical report: diagnosis and management of childhood Obstructive sleep apnea syndrome. Pediatrics 2002;109:e69. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.