Abstract
Introduction
China has pioneered advances in primary health care (PHC) and public health for a large and diverse population. To date, the current state of PHC in China has not been subjected to systematic assessments. Understanding variations in primary care services could generate opportunities for improving the structure and function of PHC.
Methods and analysis
This paper describes a nationwide PHC study (PEACE MPP Primary Health Care Survey) conducted across 31 provinces in China. The study leverages an ongoing research project, the China Patient-centered Evaluative Assessment of Cardiac Events (PEACE) Million Persons Project (MPP). It employs an observational design with document acquisition and abstraction and in-person interviews. The study will collect data and original documents on the structure and financing of PHC institutions and the adequacy of the essential medicines programme; the education, training and retention of the PHC workforce; the quality of care; and patient satisfaction with care. The study will provide a comprehensive assessment of current PHC services and help determine gaps in access and quality of care. All study instruments and documents will be deposited in the Document Bank as an open-access source for other researchers.
Ethics and dissemination
The central ethics committee at the China National Centre for Cardiovascular Disease (NCCD) approved the study. Written informed consent has been obtained from all patients. Findings will be disseminated in future peer reviewed papers, and will inform strategies aimed at improving the PHC in China.
Trial registration number
NCT02953926
Keywords: public health, primary care, health services administration & management
Strengths and limitations of this study:
This large scale up-to-date study will collect comprehensive and in-depth data of primary health care (PHC) across 31 provinces in China; it will assess the PHC services from three domains of information: structure, process and outcome.
The study is supported and funded by the National Development and Reform Commission of China; the regional health authorities are responsible for facilitating this study. This type of support, with involvement of local government officials and local practitioners as part of the effort, promotes a high response rate.
This study employs a cross-sectional designed survey in conjunction with the collection of 10 types of documents. As such, as a result of document collection, it provides a perspective not only on current practice, but also on features of care in the recent past.
The questionnaires are designed for three participant roles: PHC institution, healthcare provider, and patient; further specific questionnaires are being developed for the village clinics and village doctors.
This study is built on the China Patient-centered Evaluative Assessment of Cardiac Events (PEACE) Million Persons Project (MPP); the data from this study can be linked to the data of the MPP that has information on social economics, disease history, lifestyle, physical measurements and health outcome from 2.1 million participants; it is also linked with the national census data that allows us to extend our findings at the national level.
We will deposit all assessment instruments used in the survey in a Document Bank that will become an open access data source for researchers who want to study PHC in China.
Introduction
China has pioneered advances in primary health care (PHC) and public health for an immense, diverse population. Since the 1950s, the government has established a multi-tiered rural health service delivery system and a national network of healthcare providers to bring medical care to rural populations. Barefoot doctors and groups of villagers and farmers with limited medical training provide most of the healthcare services in rural areas (online supplementary appendix 1: China PHC healthcare providers and main responsibilities). With emphasis on prevention and self-care, the barefoot doctor-based system proved effective in improving overall health outcomes and earned praise from the international community.1
bmjopen-2017-016195supp001.pdf (324.7KB, pdf)
The healthcare system in China began to weaken following the 1980s market-oriented economic reforms.2 3 The healthcare system faced substantial challenges such as high health care costs, low quality of care, high patient out-of-pocket expenditure, and inequalities between and within urban and rural areas. In the late 1990s and early 2000s, the national government addressed the problems in the healthcare system with an emphasis on PHC. China initiated healthcare reform in 2009 to expand insurance coverage, establish a national system of essential medicines, provide essential public health services for all, pilot public hospital reform, and emphasise the central role of primary care services.2
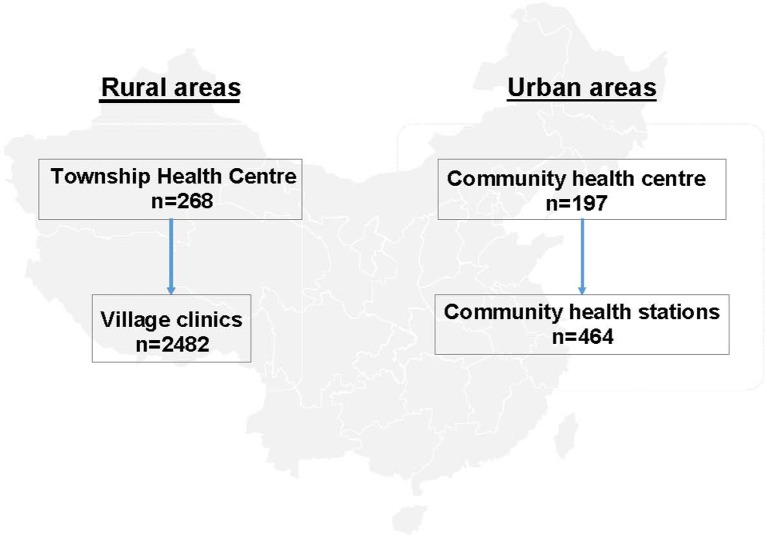
To ensure that China could achieve its goals for efficient, effective and affordable primary care, a national network of PHC has been established. This network includes community health centres and health stations in urban areas as well as township health centres and village clinics in rural areas (figure 1). The PHC institutions are responsible for health education, disease prevention, basic public health services, clinical inpatient services for minor diseases and health conditions, outpatient treatment, family planning, communicable and non-communicable disease (NCD) management, and rehabilitation services to the residents.4 The central and provincial governments fund PHC institutions for basic public health service, facility infrastructure and human resources. The government paid 45 RMB per capita in 2016 for primary healthcare providers to deliver a defined package of basic public health services, thereby serving vulnerable populations and addressing substantial challenges from NCDs.
Figure 1.
Basic structure of primary health care institutions in China.
NCDs, which include cardiovascular disease (CVD), cancer, diabetes and chronic respiratory illnesses, now account for about 80% of China’s annual deaths.5 It is estimated that NCDs currently comprise 71.5% of the total economic burden for all disease-based healthcare in China. PHC providers are expected to serve as healthcare gatekeepers, assuming responsibility for referring patients to hospitals and managing patients with diagnosed NCDs.
Since the 2009 health care reforms, China has achieved almost universal insurance coverage. Studies show considerable improvements in access, range of services, and patient satisfaction.6 7 However, PHC is not widely available in western rural areas of the country and the impact of the essential medicines list (EDL) on the availability of medicines remains unclear.8 9 The selection criteria and the adequacy of the national essential medicines list are still the subject of debate.10 Most prior studies of primary care in China faced limitations such as small sample sizes, restrictive geographic areas, and lack of direct data collection from healthcare providers and patients.6 8 9 11
Few data are available on the characteristics of the PHC workforce, health insurance reimbursement policies, effect of insurance on health outcomes, financial investment at different levels of PHC institutions, extent of geographic variation, utilisation of services, and patient satisfaction with clinical care. There has been no systematic effort to document whether variations in primary care services exist or to understand gaps in the structure and function of primary care. To assess PHC services, China needs independent and evidence-based instruments. Systematic data collection and evaluation will yield insight into factors of both the successes and persistent challenges in PHC.
This nationwide PHC study across 31 provinces in China employs an observational design and will collect data and original documents on the structure and financing of PHC institutions; adequacy of the essential medicines programme; education, training and retention of the PHC workforce; and quality of care and patient satisfaction. The study findings will serve as a critical source for a comprehensive assessment of current PHC services and help determine what gaps remain in access, quality and equity in PHC.
The study was developed with funding from the National Development and Reform Commission of China and builds on an ongoing project, the China Patient-centered Evaluative Assessment of Cardiac Events (PEACE) Million Persons Project (MPP).12 The China PEACE MPP is a nationwide population-based project aiming to identify subjects with high CVD risk and investigate their treatment, management, and outcomes. The collaborators of the MPP network include PHC institutions, secondary and tertiary hospitals, and Centers of Disease Control and Prevention (CDCs) across 31 provinces in mainland China. The survey will be conducted based on PHC institutions of the MPP network.
As part of this study, we plan to create a Document Bank of PHC in China, where we will deposit all of the assessment instruments used in the study with all patient identifiers removed. We have committed to a policy of open science to allow other investigators access to the data being collected in this survey. The Document Bank will eventually become an open access data source for researchers who want to study PHC in China. We anticipate the findings and results will be valuable for health policymakers in China, and knowledge learnt from the study may also benefit other countries that face challenges similar to China.
Methods
Study overview
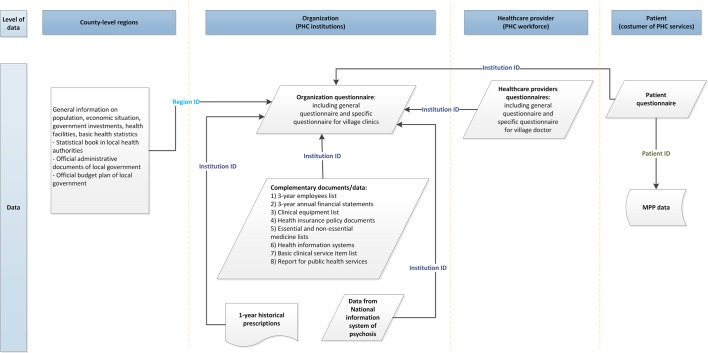
This study is a cross-sectional assessment and document collection initiative conducted in 31 provinces and municipalities directly under the central government, and autonomous regions across mainland China. We employ multiple methods of data collection. First, a cross-sectional survey is used to collect data on three levels: system (PHC institutions), service provision (healthcare providers), and users of PHC service (patients who receive PHC services). The survey assessment involves about 3400 PHC institutions (Figure 1), 20 000 health providers, and more than 35 000 patients. This multi-level design is able to link information on PHC institutions to information on service providers, as well as to patient information. Second, we will collect objective data on financing, workforce, essential public health services, health insurance policies, essential medicines, electronic health systems, and 1-year historical prescription records from all participating PHC institutions. We will also obtain registry data of patients with severe mental illnesses. Thirdly, we will link patient survey data to the MPP study database to assess diagnoses, management and outcomes of CVD. Figure 2 shows the types of data and documents collected by the study and their relationship. All study instruments will be deposited in the Document Bank as an open access source for other researchers. As part of this paper, we will place the main survey instruments into a web-based electronic appendix.
Figure 2.
Relationship of data and documents collected by the study. MPP, Patient-centered Evaluative Assessment of Cardiac Events Million Persons Project. PHC, primary health care.
Data sources
Survey assessment
The cross-sectional survey uses questionnaires to collect comprehensive data on the PHC system, service provision, and the perspectives of health professionals and consumers of services to form a database that will enable studies on a wide range of PHC research questions.
Setting and sampling
The survey leverages the ongoing MPP study in China.12 The MPP is a national population-based screening project across China to identify subjects aged from 35 to 75 years with high risk of CVD. All PHC institutions of the MPP network will be enrolled in the survey, including township hospital and village clinics in rural areas and community health centres and stations in urban areas (online supplementary appendix 2 describes the PHC institutions and their function in more detail). The selection criteria of the study sites in the MPP network have been described in the published protocol.12 Briefly, the MPP enrolled the eligible study sites according to the size of residents of the catchment area, population stability, local economic condition and geographic location. All healthcare providers who work in the participating PHC institution are recruited in the survey. The healthcare providers include physicians, nurses, public health professionals, village doctors and their assistants. More details of healthcare providers are available in Appendix 1 (online supplementary appendix 1: China PHC healthcare providers and main responsibilities). From the MPP high-risk CVD population, we will use the stratified random sampling method to sample patients 35 to 75 years of age who live in the catchment areas of participating PHC institutions. We will link the participating patients to the MPP health data for additional health information, such as self-reported disease history, medication use and measured blood pressure, glucose and cholesterol. The MPP defines a participant with high risk CVD using the following criteria: (1) history of established CVD; (2) high blood pressure; (3) dyslipidaemia; and (4) expected 10 year risk of CVD ≥20%.12 Written consent has been obtained from all MPP study participants.
Questionnaire development
To prepare for the questionnaire development, we obtained the perspectives of people associated with PHC through meetings with frontline practitioners, international experts, domestic policymakers, and a review of prior literature, questionnaires, and policy documents. Before the study, we visited 20 PHC institutions in six provinces and consulted with local PHC healthcare providers to obtain their opinions on PHC. Next, to understand healthcare policies and regulations at a central government level, we reviewed official policy documents on health care from 1984 to 2016 that were provided by the Legislative Affairs Office of the State Council (online supplementary appendix 3: National policy documents on health care in Chinese). In addition, we reviewed published questionnaires of other observational studies and population surveys on primary care in China and other countries.13 We emphasised questionnaires on known and potential measurements for PHC that are or will be important for China’s PHC. Authors of this paper and other national and international experts have reviewed the finalised version of the questionnaires (online supplementary appendix 4: List of questionnaire reviewers).
Questionnaire scope and sampling design
Three types of questionnaires were developed: (1) organisational questionnaire; (2) healthcare provider questionnaire; and (3) patient questionnaire. The English versions of these questionnaires are available in online supplementary appendix 5. The Chinese version of all the questionnaires is available on request. The survey questions can be categorised into three broad domains: the organisational structure of the PHC, its processes and outcomes14 (table 1). Data will be collected on elements such as financing, the workforce, essential drug supply, availability of essential medical and public health services, patients’ experience and satisfaction with the PHC system.
Table 1.
Main outcomes of interest covered by the survey questionnaires
| Aspects | Outcomes of interest | Organisation questionnaire | Provider questionnaire | Patient questionnaire |
| Structure | Governance | ✓ | ✓ | |
| Financing | ✓ | |||
| Workforce | ✓ | ✓ | ||
| Facility infrastructure | ✓ | |||
| Health information system | ✓ | |||
| Drug supply | ✓ | ✓ | ||
| Process | Access | ✓ | ✓ | ✓ |
| Comprehensiveness | ✓ | |||
| Continuity | ✓ | ✓ | ✓ | |
| Coordination | ✓ | ✓ | ✓ | |
| Outcome | Quality | ✓ | ✓ | |
| Equity | ✓ | ✓ | ||
| Efficiency | ✓ | ✓ |
Organisational questionnaire
This questionnaire is collecting system-level data on PHC institutions, focusing on financing, resources, and regulatory aspects. Questions have been included on infrastructure, staff employment, employees’ social benefits, income and expenditure in 2015, basic medical and public health services, essential medical equipment, and supply of essential medicine. These questions were mostly based on government policies and regulations for PHC and consultation with local healthcare providers. The amount of funding also varies between village clinics and other types of PHC institutions. We have developed specific questions for village clinics with respect to their financing, revenue sources and expenditure flows. We piloted the questionnaires in about 90 PHC institutions. The questions were revised and updated based on the feedback of the local PHC health professionals and senior managers. The final version of the questionnaire is considered reasonable and well understood by the participating PHC institutions.
Healthcare provider questionnaire
This questionnaire collects information on education and training, provider services, career development and training opportunities, working responsibilities and tasks, workload, psychological status and satisfaction with work. The questions were mainly sourced and adapted from large surveys on primary care (ie, the QUALICOPC study on general practice and general partitions in 34 European countries) which have been used extensively on large and diverse study populations.15 16 We also used the Maslach Burnout Inventory for Human Services Survey (MBI-HSS) to assess the burnout status of PHC healthcare providers.17 Chinese researchers have commonly used the MBI questionnaire to assess professional burnout.18 19 We compared the existing Chinese and English versions of MBI-HSS questionnaires and independently verified that the translation of BMI-HSS questions was accurate. The full Chinese version of the BMI-HSS questionnaire is included in the healthcare providers questionnaires.
The village doctor is a unique PHC healthcare provider in China. They are not considered a conventionally defined physician, who is typically trained in medical school for at least 5 years and has completed a residency programme in a hospital. Instead, most village doctors graduate from middle school or high school, and attend adult education or remote education programmes to learn basic medical knowledge for up to 2 years. They provide essential medical care and public health services to villagers and farmers in rural areas. The government has issued a specific salary policy which provides a specific budget plan to retain village doctors in their post and motivate them to provide basic public health services. As such, we developed specific questions to assess the impact of policies on village doctors and their services. We collected information on education and training, incomes, whether they held other jobs in the community in addition to their role as village doctor, and their level of job satisfaction. This questionnaire was also developed with reference to a survey on village clinics and village doctors in Ningxia province, China.20
Patient questionnaire
This questionnaire examines reasons for visiting a PHC institution and using its services, measures out-of-pocket expenditure on health care, reimbursement experiences, satisfaction and accessibility to PHC. The questions are adapted from various validated survey instruments,21–23 and are mainly designed to assess the user’s experience of those services. The data can be linked to the MPP health database where information on medical history, physical examination and laboratory test results are available.
Questionnaire administration
A computerised direct data entry method is used for all questionnaires. The IT technology of the direct data entry method has been specially developed for the PHC survey. To ensure feasibility, comprehension, and to recognise the time needed to complete the questionnaire, this self-administered method is used for the organisation and healthcare provider questionnaire and a face-to-face interview method is used for the patient questionnaire. The director of a participating PHC institution takes responsibility for accurate answers to the questions in the organisation questionnaire. The institution director facilitates the human resource department,the financing department and senior manager input to provide the relevant information for the organisation questionnaire. The organisation questionnaire takes about 60 min to complete, and the healthcare provider and patient questionnaires typically require an average of 30 min to complete.
Objective documents
In addition to the questionnaires, we will collect objective documents from each participating PHC institution. Table 2 summarises the main data elements of each document (online supplementary appendix 6: Contents of each document). The provincial and regional policy documents will be analysed systematically to quantify the impact of regional policy on PHC services. The collection of documents in the survey was considered with respect to availability, reliability and relevance. As such, the included documents are usually readily available within PHC institutions, and are able to be provided without additional work. With respect to reliability, the documents are produced within certain quality assurance control. They are initially generated for a management purpose or required by health authorities. For example, the employee list is an essential document for the human resources department to register all employees of an organisation, and the financial statement is an essential document within the finance and accounting department of a PHC organisation. For relevance, the documents collected by the survey were dependent on the other studies that indicated they were useful for understanding and assessing specific aspects of PHC services in China. For example, we collect the national and provincial essential medication lists (EMLs) for assessing the availability of essential drugs and regional variation of EMLs. The health insurance policy documents can be used to assess variation of the reimbursement policy across provinces and economic regions.
Table 2.
Data elements in the objective documents
| Name | Main data elements covered |
| Employee roster (3 year records) | Age, gender, ethnicity, first high education degree, highest education degree, seniority, qualification, licence, government quota post, year of working, department |
| Annual financial statement (3 year records) | Funding/income (funding/income sources and amount of funding/income), expenditure (expense flow and amount of expense) |
| Clinical equipment list | Type of equipment (physical measurement, laboratory, imaging and clinical treatment), name, manufacturer, model, amount of the equipment, unit price, year of start use |
| Health insurance policy document | Funding sources (government, patients and employers), deducible, reimbursement ration, ceiling, co-payment, reimbursement for hypertension patient, reimbursement for diabetes patients |
| Medicine lists | Type of drug list (ie, national essential medicine list (EML), provincial EMLs, insurance reimbursement medicine list), name of drug, dosage, package size, manufacturer, price |
| Health information systems | Type of system, name, software developers, maximum coverage, year of installation, purchase price, annual maintenance fee |
| Essential clinical services item list | Name of service, description, price of service, unit of service |
| Report for essential public health service packages* | Name of public health service, defined indicators and their values for each public health service |
*Essential public health service packages include mainly established health archives, health education/promotion, planned immunisation and vaccination, child health management, maternal care management, geriatric care, chronic disease management (including hypertension and diabetes), and management for patients with severe mental illness.2
Employee rosters in preceding 3 years
The participating PHC institutions provide anonymous employee rosters for the preceding 3 years. The information includes employees’ educational background, seniority, professional qualifications and job title, which can be used to assess the education level and work experience of the workforce. The 3-year employee rosters allow us to calculate the retention rates of employees.
Annual financial statements in preceding 3 years
Participating PHC institutions will provide annual financial statements from the last 3 years. We will extract the information on funding, income sources and expense on personnel, medical services, public health services, equipment, and medicines (including Traditional Chinese Medicine (TCM), Chinese herbal medicine and western drugs). The financial statements allow us to study the trends of funding sources and expenditure flows.
Clinical equipment list
Each participating institution provides a list of the types of clinical equipment used routinely for physical examinations, laboratory tests, imaging studies and clinical treatments, as well as the unit price and starting use year. We will be able to assess the availability of clinical equipment by four groups: physical examination, laboratory test, imaging examination and clinical treatment. They allow us to assess whether the equipment meets the needs of the routine work of the PHC.
Health insurance policy documents
These relate to all three basic medical insurance systems, including the Urban Employees’ Basic Medical Insurance (UEBMI), the Urban Residents’ Basic Medical Insurance (URBMI), and the New Rural Cooperation Medical Scheme (NRCMS). The UEBMI and URBMI provide reimbursements to urban residents for both inpatient and outpatient expenses. NRCMS is largely dedicated to the reimbursement of inpatient and catastrophic outpatient expenses for rural residents. Health insurance and reimbursement policies vary across regions and disease categories. We will collect regional health insurance policy documents and extract the information on funding sources (government and public source), and reimbursement policies for inpatient, outpatient and NCDs.
Medication list
The Chinese central government has implemented the National Essential Medicines policy in PHC institutions and hospitals to ensure that essential medicines are available and affordable. The latest version of the National Essential Medicine List (EML) for the PHC has 307 medicines, including 102 TCM. In addition, each province has its own supplement list (ie, provincial EMLs), which varies largely across China. In addition, health insurance schemes have their own specified drug lists for reimbursement purposes (ie, national reimbursement medicine lists). The insurance reimbursement medicine is further grouped into two categories, List A and List B. List A includes most drugs from EMLs that are 100% reimbursed by the insurance scheme. List B includes newer and innovative drugs that are partly reimbursed. The data allow us to assess the availability of essential medications and assess this accessibility across the various regions of China. We will also be able to assess the impact of the regional variation of EML due to different selection criteria for provincial and insurance reimbursement medication lists across provinces.24 Lastly, we will collect the in-stock medication list from the participating PHC institutions to study the availability of essential medicines.
Health information systems
The health information systems can be grouped as follows: hospital information systems, public health information systems, health insurance information systems, healthcare expenditure information platforms, and health administration platforms. We will collect information on the names of the systems, system developers, year of implementation, purchase price and annual maintenance fees.
Essential clinical service item list
We will collect the data on routine clinical service items provided by participating PHC instructions and the level of fee charged.
Report on national essential public health services
The PHC institutions provide 12 essential public health service packages for free. The service packages can be grouped into three categories: services for the general population; services for children, maternal needs and the elderly; and services for communicable and non-communicable disease prevention and control.4 The PHC institutions are required by the health authority to submit a report on the delivered public health services using pre-defined indicators/benchmarks, such as the proportion of residents who have electronic health records in their catchment area and the proportion of patients with hypertension or diabetes.2 The health authority compares the reported indicators/benchmarks to pre-existing target values (e.g. at least 95% of residents will have electronic health records) to assess whether the institution meets the target. In addition to the purposes of quality control, these reports are also used for pay-for-performance purposes. In 2016, about 45 RMB per capita was paid to the PHC institutions to provide these public health services. We will collect the official reports and extract the self-reported values of indicators/benchmarks from the reports.
Historical prescription records
We will scan up to 300 hard copies of prescriptions per month from all participating PHC institutions from April 2015 to March 2016, depending on the number of patients who visited the institutions each month. Prescriptions will be randomly selected for scanning based on the 10 day interval of the month. For example, 100 prescriptions will be randomly selected from the first 10 days of the month, 100 prescriptions will be randomly selected from the second 10 days of the month, and the remaining 100 copies will be selected from the remaining days of the month. It is possible that no prescriptions may be available in a typical month at some rural township health stations and village clinics, due to lack of activity. According to regulations issued by China’s provincial health administrative departments, a prescription is limited to one patient and up to five medicines. In the first instance, we will abstract the data on diagnoses, prices if available, date of diagnoses, medication formula, dosage and use frequency, focusing on antibiotics, antihypertensive and hypoglycaemic agents, and lipid-lowering drugs (see online supplementary appendix 7: Example of a scanned prescription without identifiers).
Anonymised data from the national information system of psychosis
China faces a challenge with meeting the mental health needs of its population, for which the resources and services fall short of the needs of its vast population.25 The government has initiated an essential public health programme that registers and follows up psychosis patients in communities, and builds a national information system for these patients.26 The data from the National Information System of Psychosis are important for the assessment of psychosis patient management—one of the essential public health services in the PHC system. We will extract the anonymised baseline data and the last wave data for each follow-up year in the past 3 years from the surveillance information system of the participating PHC institutions. The baseline dataset includes information on diagnoses, dates of episodes, and dates of hospital admissions. The follow-up dataset will include data on date of follow-up interview, date of hospital admission, drug use (formula, dosage, frequency and compliance), outcome of treatment and vital status (online supplementary appendix 8: Data elements of the anonymised data from the National Information System of Psychosis).
General information on county-level regions where participating PHC institutions locate
In this study, ‘county’ refers to the county-level administrative divisions. There are five levels of hierarchical administrative divisions in China: provincial, prefecture, county, township, and village. Township- and village-level regions are positioned under the county level. This study collects data on economic development, population size, insurance population size, and health statistics from county-level regions where the participating PHC institutions are located. It is facilitated by the county health authorities, the health and economic departments of county governments and local Centers for Disease Control and Prevention (CDCs). The general information obtained from counties can be linked to other datasets by a unique regional ID number (online supplementary appendix 9: General information on population, economic and health statistics of the county where participating PHC institutions locate).
MPP health data
The MPP is a large-scale population-based screening project to identify a population with high CVD risk.12 It collects detailed information from study participants and biological samples for further risk assessment. The information collected by the PHC patient questionnaire can be linked to the MPP health data by a unique ID number. MPP study health data are used to inform the current status of NCD diagnoses and management in China. At this stage, the MPP project has screened about 1.2 million residents in 16 provinces and identified about 0.27 million high-risk CVD patients. We anticipate assessment in the other 15 provinces will be finished in the second quarter of 2017. The participants are interviewed using structured questionnaires for sociodemographic, lifestyle and self-reported disease history and medication use history. A physical examination is conducted for each participant, and further information collected such as blood pressure, heart rate, weight and height. Meanwhile, a blood and urine sample is taken from each participant for future investigation. Data on laboratory test results, including blood lipid, glucose, glycated haemoglobin (HbA1c) and creatinine, are available for all high CVD risk participants. Table 3 Table 3 shows the main characteristics of the 0.27 million screened high CVD risk MPP population.
Table 3.
Main characteristics of the China PEACE MPP high CVD risk population
| Rural | Urban | Total | |
| (n=167 144) | (n=108 457) | (n=275 601) | |
| Male, n (%) | 72 690 (43.5) | 49 025 (45.2) | 121 715 (44.2) |
| Age group, n (%) | |||
| 35–39 | 3 347 (2.0) | 2 268 (2.1) | 5 615 (2.0) |
| 40–49 | 27 830 (16.7) | 19 398 (17.9) | 47 228 (17.1) |
| 50–59 | 52 876 (31.6) | 33 659 (31.0) | 86 535 (31.4) |
| 60–69 | 63 245 (37.8) | 40 251 (37.1) | 103 496 (37.6) |
| 70–75 | 19 846 (11.9) | 12 881 (11.9) | 32 727 (11.9) |
| Mean (SD) | 58.4 (9.1) | 58.2 (9.3) | 58.3 (9.2) |
| Current smoker, n (%) | 35 125 (21.0) | 22 380 (20.6) | 57 505 (20.9) |
| BMI (kg/m2) | |||
| <18.5 | 2 364 (1.4) | 1 026 (1.0) | 3 390 (1.2) |
| 18.5–24.9 | 76 945 (46.3) | 47 564 (44.2) | 124 509 (45.2) |
| 25.0–29.9 | 71 109 (42.8) | 48 708 (45.2) | 119 817 (43.5) |
| ≥30.0 | 15 883 (9.6) | 10 426 (9.7) | 26 309 (9.6) |
| Mean (SD) | 25.4 (3.5) | 25.6 (3.3) | 25.5 (3.4) |
| SBP (mm Hg), mean (SD) | 159.9 (22.0) | 156.6 (22.3) | 158.6 (22.2) |
| DBP (mm Hg), mean (SD) | 90.3 (12.8) | 89.1 (13.0) | 89.8 (12.9) |
| TC, mean (SD) | 5.0 (1.3) | 5.0 (1.3) | 5.0 (1.3) |
| HDL, mean (SD) | 1.4 (0.5) | 1.3 (0.5) | 1.4 (0.5) |
| LDL, mean (SD) | 2.8 (1.1) | 2.8 (1.1) | 2.8 (1.1) |
| Self-reported diseases, n (%) | |||
| Hypertension | 74 818 (44.8) | 47 037 (43.4) | 121 855 (44.2) |
| Diabetes | 14 275 (8.5) | 12 341 (11.4) | 26 616 (9.7) |
| MI | 4 214 (2.5) | 3 579 (3.3) | 7 793 (2.8) |
| Stroke | 16 735 (10.0) | 12 489 (11.5) | 29 224 (10.6) |
BMI, body mass index; CVD, cardiovascular disease; DBP, diastolic blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; MI, myocardial infarction; SBP, systolic blood pressure; TC, total cholesterol.
Document bank and IT system architecture
A fully integrated IT system has been developed for data collection, repository and archiving, involving local assessment sites and a central coordinating centre, based at China’s National Clinical Research Center of Cardiovascular Disease (NCCD), in Beijing.
The IT system for assessment sites includes the hardware (Universal Serial Bus (USB) memory key) and software applications (offline electronic data collection). Each participating PHC institution will be issued with a USB memory key with a unique ID number at the start of data collection. The USB memory key acts as a storage device for collecting various data types. The original policy documents, such as health insurance policy documents, are collected and saved directly onto the USB memory key. All data on the USB key will be removed after the transfer of the data to the central repositories within the NCCD. Meanwhile, controlled access to the system will be implemented by the local coordinating centre staff and will prevent unauthorised access. The staff members must use the account and authorised passwords to log into the system and gain entry to the data collection platform. The passwords are used not only to ensure data security, but also to create an audit trail of all data entered, saved or changed.
The software applications have been specifically developed for the PHC study, including electronic questionnaires, Excel template tables, and a scanning plugin. The electronic questionnaires have built-in basic rules for data entry—for example, a pre-defined format and range for variables, single or multiple choice for questions, and blank entries cannot be uploaded. The Excel template tables are designed to collect data using standardised methods that enable collected data to be more usable. The scanning plugin application is designed for scanning hard copies of prescriptions and depositing them in the USB.
The assessment sites securely pass all collected data and documents to the central repositories at the NCCD in Beijing. The NCCD deposits collected raw and health data from the MPP study in central highly-secured repositories that will form the document bank for the China PHC data. Repository data will be transformed, processed, extracted and validated before being used for any research purposes.
Data management
Data transfer and access
As the PHC institutions are scattered widely throughout China, it is important to return the data and documents to the national coordinating centre (NCCD, Beijing) on schedule to provide timely and regular audits, to ensure that the data and documents are being collected correctly and then to provide necessary feedback to the local coordinating centres. The regional data collection systems will securely transfer encrypted data on the USB memory key to the core database at the NCCD for storing and data validation via a secured network every 3 days. This will enable the NCCD to provide rapid responses and implement any necessary improvements for the smooth running of the local coordinating centre and PHC institution. The NCCD project team will manually check the uploaded documents and assess the quality of scanned documents for clarity, completeness and correctness (figure 3).
Figure 3.
Flowchart of data processing procedure. PHC, primary health care; QA, quality assurance.
All data and documents will be de-identified and stored on secure servers at the NCCD in Beijing. The confidential identifier—for example, name, date of birth, contact information and address—will not appear in the analytic dataset. Only authorised staff and researchers will be able to access the database.
Data quality assurance and quality control (QA/QC)
We have developed a set of policies and procedures to ensure data quality. Specifically, for the data collection phase, we focused on four precautions: (1) software design; (2) proper training; (3) central and on-site monitoring visits; and (4) real-time data monitoring.
Software design
The e-questionnaire module in the offline electronic data collection system has been designed with capabilities for quality control. First, instructions and explanations for questions have been listed within questionnaires alongside each question. Second, logical data checks have been embedded to verify that the questions are answered completely and that the values entered meet the predefined range and formats. The system displays a warning message for users to correct or re-enter data if answers violate the pre-defined rules. Thirdly, a standardised coding system is adopted using organisation ID, file type, year/month, and file sequence number as a combination for naming all data files. Lastly, we will ensure data security during the transfer of data by using encrypted data transmission from local study sites to the NCCD.
Training
Before data collection starts, all regional coordinating centre staff and key personnel of PHC institutions undergo training at a 2 day conference. The training has been organised by the NCCD and delivered by specialised trainers. The training programme covers the sections of introduction, questionnaire, original documents collection and processing, scanning and practice sessions (online supplementary appendix 10: Core training programme). Meanwhile, the NCCD provided the fieldwork staff a package of training materials, including standard operating protocols, training videos, and slides of the presentations given during the training conference. In addition, the NCCD sent trainers to participating PHC institutions and delivered on-site training. The NCCD also provided remote training as an alternative training method for participants. Telephone and web-based hotlines are available for any queries during the data collection through the NCCD. We also provided additional training material for people who participate in the anonymous questionnaires (general staff and village doctors) to ensure data quality.
Central and on-side monitoring visits
We conducted central and on-site monitoring visits. The central monitoring aims to review collected data and documents that are stored in the document bank in the NCCD. Data were uploaded daily and were inspected manually for completeness and clarity of documents by five full-time data quality specialists.
Real-time data monitoring
Moreover, we have developed an SAS QA/QC package to conduct real-time data checks on both questionnaire and structured document data. Specifically, the package runs at midnight of every day and identifies records with data errors or potential data errors. These records will be reviewed by data specialists who will make necessary corrections. The SAS package focuses on the following aspects at each PHC institution.
Progress status tracking: for example, this was done by comparing numbers of provider questionnaires finished with the total number of employees confirmed by the PHC institution to identify any potential issues with the operation of the survey.
Missing data tracking: the number of questions missed in a questionnaire is used to assess the completeness of questionnaires; the number of documents missing will be used to identify operational weaknesses.
Data validation: predefined logic verification standard was applied for data quality checks. For example, the number of outliers for each continuous variable or illogic association between variables will be used to identify the process failure of data collection and help to identify staff requiring additional training if appropriated.
Once data issues have been identified, through manual check or through the real-time SAS QA/QC package, the NCCD staff will contact the local coordinating centres to clarify or correct these issues. Any major issues identified during the data review will be followed up by an on-site monitoring visit by the NCCD’s project team. In addition, the NCCD and regional coordinating teams will conduct regular on-site visits in the participating PHC institutions. The goal of an on-site visit is to monitor staff compliance with the operations manual, installation and maintenance of software applications, data collection flowchart, interview protocol, as well as checking the completeness and quality of documents.
Data analyses
Given the comprehensive information collected by the survey, a wide range of measurement tools and analytic methods can be applied to the data. We describe part of the primary analysis methods in this paper. We will conduct the Cronbach's α test to assess reliability of key questionnaires. Descriptive analyses will be used to illustrate PHC institutions, PHC healthcare professionals and population characteristics, and to compare the observed differences in outcomes across PHCs. We will investigate the key outcome indicators (such as access to care) across institutions, healthcare providers and patients. We will use standard parametric and non-parametric techniques for observational data. More specifically, we will use the Χ2 test for comparing categorical variables and the t-test or Wilcoxon rank sum tests for comparing continuous variables. Given that the PHC survey data are hierarchical, we will use a mixed methods modelling approach for most of the analyses. We will fit a mixed model with a Poisson link function to model the number of PHCs as a function of the PHC's characteristics, the population's socioeconomic status, health risk factors, lifestyle, and area-specific demographic and geographic characteristics. This model will allow us to identify important characteristics that are associated with PHC services. We will also include region-specific random intercepts in the model to account for within-region and between-region variations, and the area-specific population will be used as an offset within the model. We will use a multiple imputation approach to handling missing data problems for those variables to be included in a regression model. The region-specific and institute/provider-specific variations are important for this study. We will calculate the population-weighted coefficient of dispersion to assess the variation between PHCs.
To assess geographic variation in the availability of PHC services nationwide, we will calculate province-specific risk-standardised rates availability of PHCs per 100 000 population for each of the 31 provinces in the study, using the method developed by Krumholz et al.27–29 We will include a spherical covariate structure in models to account for the spatial autocorrelation. Weighted adjustment will be applied to analyses as needed. All analyses will be conducted using SAS version 9.4, 64-bit (SAS Institute Inc, Cary, North Carolina). All statistical testing will be two-sided, at a significance level of 0.05.
Discussion
We present the methods of a massive survey and document collection of PHC in China that is configured to build the foundation for a learning health system. To achieve notable improvements in the effectiveness, efficiency and equity of healthcare delivery requires a thorough understanding of current performance, an identification of targets for improvement, and a means of linking specific processes with outcomes. Moreover, ideally research into performance and improvement ought to integrate perspectives of practitioners, policymakers and, most importantly, patients. We have constructed a broad ranging survey, with the input of patients, practitioners and policymakers, and an extensive effort to collect documents that will enable a full picture of contemporary primary care in China to emerge—and to lead to a system of continual improvement. Ultimately the goal is to integrate assessment and learning into everyday practice, and to make performance clear and accountability routine. Moreover, the assessment is designed to lead to policy improvements that promote high-quality, affordable care that best serves patients, the medical workforce, and society.
To the best of our knowledge, there has been no systematic effort to collect comprehensive and in-depth data to understand the current status of PHC in China since 2009. This study is the most recent nationwide study on PHC in China, providing independent and evidence-based instruments for PHC research. It is likely to have a large sample size as it will assess more than 3 400 PHC institutions, 20 000 healthcare providers, and 35 000 patients in 31 provinces. The data will represent the ‘real life’ of PHC as data are collected in routine primary care. As the local health authorities will facilitate this study, we are likely to have high engagement by respondents and a high response rate. The idea is that the survey will be seen as part of an ongoing collaboration with them to improve care, rather than a singular research project. Furthermore, the study will link with national census data that allows us to analyse the results in the context of information about local population characteristics. This study will allow researchers to address many important issues of PHC in partnership with key stakeholders—for example, a detailed profile of the workforce, the current situation of rural PHC services and village doctors, the availability and affordability of essential drugs, and regional variations in health insurance policy.
The study does have some limitations. First, we use self-administered questionnaires to assess the PHC institutions, healthcare providers and patients, which may introduce recall bias and reporting bias. However, we collect objective documents in conjunction with the questionnaires. Meanwhile, we have worked with partners to develop the content and improve the administration of the survey and data collection. In order to improve the ability to understand the self-administered questionnaires, we have tested the wording of the questions with groups to ensure they are interpreted correctly. We also provide the interviewees with instructions to explain the questions. Second, the study provides estimates at one point in time. However, the comprehensive and in-depth data of this study can provide thoughtful descriptive analyses of PHC to identify the current achievement and knowledge gaps. Moreover, we collect documents that provide a perspective on recent history. Third, the study does not collect information about other sectors of the healthcare system—for example, hospitals. The focus is on PHC and future efforts can expand data collection to these other sectors.
In conclusion, we describe an effort to create a rich PHC-specific database that will reflect the contemporary pattern of China's PHC system, that will provide an opportunity for researchers, in partnership with stakeholders, to characterise and improve PHC in China, and that will become an important milestone in supporting China's modern healthcare reform efforts.
Ethics and dissemination
Central ethics approvals have been obtained from the China National Center for Cardiovascular Disease (NCCD) Ethical Committee. All patients will be asked to provide written informed consent. The survey central coordinating centre NCCD will be responsible for doing the analyses and drafting the main reports of the survey. The results from this study will be disseminated at international conferences and in peer reviewed journals.
Supplementary Material
Acknowledgments
We appreciate all participating PHC institutions, healthcare providers and patients of the survey. We thank all staff of provincial and regional coordinating centres for their support and coordinating assistance. We are grateful for the support provided by the Chinese government. We appreciate the advice from Professor Qingyue Meng, Professor Dong Xu, and Professor Richard Peto. We appreciate the contribution of the project team and fieldwork staff at the NCCD central coordinating centre. We thank Claire Masters and Tianna Zhou for proof reading.
Footnotes
Contributors: LJ and HMK initially designed the study. MS and QZ wrote the first draft. YW provided data management and statistical expertise. JL, XL, NT, YW, WY, KC, GAM, RIH and EM provided comments and suggestions in critical revision of the article. All authors approved the final version of the article.
Funding: This project was supported by the Major Public Health Service Project from the Ministry of Finance of China and National Health and Family Planning Commission of China; the Entrusted Project from the China National Development and Reform Commission; the CAMS Innovation Fund for Medical Sciences (CIFMS) (20164I2M414006); the China WHO Biennial Collaborative Projects 201642017 (2016/66442440); Research Special Fund for Public Welfare Industry of Health (201502009) from the National Health and Family Planning Commission of China; the National Key Technology R&D Program (2013BAI09B01, 2015BAI12B01, 2015BAI12B02) from the Ministry of Science and Technology of China; and the 111 Project (B16005).
Competing interests: None declared.
Patient consent: Obtained, using the MPP's template consent form.
Ethics approval: The central ethics committee at the China National Center for Cardiovascular Disease (NCCD) approved the study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: When the survey is finished, data requests can be sent to the NCCD central coordinating center, Beijing. Research proposal based on the survey data must be approved by the NCCD Central Coordinating Centre and Expert committee.
References
- 1. Zhang S, Zhang W, Zhou H, et al. . How China's new health reform influences village doctors' income structure: evidence from a qualitative study in six counties in China. Hum Resour Health 2015;13:26 10.1186/s12960-015-0019-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yip WC, Hsiao WC, Chen W, et al. . Early appraisal of China's huge and complex health-care reforms. Lancet 2012;379:833–42. 10.1016/S0140-6736(11)61880-1 [DOI] [PubMed] [Google Scholar]
- 3. Wagstaff A, Yip W, Lindelow M, et al. . China's health system and its reform: a review of recent studies. Health Econ 2009;18:S7–S23. 10.1002/hec.1518 [DOI] [PubMed] [Google Scholar]
- 4. Meng Q. People's Republic of China Health System Review. 2015. [Google Scholar]
- 5. Watts J. Chen Zhu: from barefoot doctor to China's Minister of Health. Lancet 2008;372:1455 10.1016/S0140-6736(08)61561-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Li J, Wang P, Kong X, et al. . Patient satisfaction between primary care providers and hospitals: a cross-sectional survey in Jilin Province, China. Int J Qual Health Care 2016;28:346–54. 10.1093/intqhc/mzw038 [DOI] [PubMed] [Google Scholar]
- 7. Hu R, Liao Y, Du Z, et al. . Types of health care facilities and the quality of primary care: a study of characteristics and experiences of Chinese patients in Guangdong Province, China. BMC Health Serv Res 2016;16:335 10.1186/s12913-016-1604-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Han Y, Wei J, Song X, et al. . Accessibility of primary health care workforce in rural China. Asia Pac J Public Health 2012;24:833–47. 10.1177/1010539511403801 [DOI] [PubMed] [Google Scholar]
- 9. Yao Q, Liu C, Ferrier JA, et al. . Urban-rural inequality regarding drug prescriptions in primary care facilities - a pre-post comparison of the National Essential Medicines Scheme of China. Int J Equity Health 2015;14:58 10.1186/s12939-015-0186-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tian X, Song Y, Zhang X. National Essential Medicines list and policy practice: a case study of China's health care reform. BMC Health Serv Res 2012;12:401 10.1186/1472-6963-12-401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wei X, Li H, Yang N, et al. . Changes in the perceived quality of primary care in Shanghai and Shenzhen, China: a difference-in-difference analysis. Bull World Health Organ 2015;93:407–16. 10.2471/BLT.14.139527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lu J, Xuan S, Downing NS, et al. . Protocol for the China PEACE (Patient-centered Evaluative Assessment of Cardiac events) Million Persons Project pilot. BMJ Open 2016;6:e010200 10.1136/bmjopen-2015-010200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kringos DS, Boerma WG, Hutchinson A, et al. . The breadth of primary care: a systematic literature review of its core dimensions. BMC Health Serv Res 2010;10:65 10.1186/1472-6963-10-65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Donabedian A. Evaluating the quality of medical care. Milbank Mem Fund Q 1966;44:166–206. 10.2307/3348969 [DOI] [PubMed] [Google Scholar]
- 15. Schäfer WL, Boerma WG, Kringos DS, et al. . QUALICOPC, a multi-country study evaluating quality, costs and equity in primary care. BMC Fam Pract 2011;12:115 10.1186/1471-2296-12-115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yang H, Shi L, Lebrun LA, et al. . Development of the Chinese primary care assessment tool: data quality and measurement properties. Int J Qual Health Care 2013;25:92–105. 10.1093/intqhc/mzs072 [DOI] [PubMed] [Google Scholar]
- 17. Maslach C, Jackson SE, Leiter MP. The Maslach Burnout Inventory Manual Zalaquett ECW RJ, Evaluating stress: a book of Resources. the Scarecrow Press, 1997. [Google Scholar]
- 18. Li Y. Brief introduction to Maslach Burnout Inventory. J Envion Occup Med 2004;21:506–7. [Google Scholar]
- 19. Li YY, Li LP. [An investigation on job burnout of medical personnel in a top three hospital]. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2016;34:357–60. [DOI] [PubMed] [Google Scholar]
- 20. Yip W. Re-alignment of Health System incentives to improve affordable and effective Healthcare Project. http://www.bsg.ox.ac.uk/research/projects/re-alignment-health-system-incentives.
- 21. Schäfer WL, Boerma WG, Kringos DS, et al. . Measures of quality, costs and equity in primary health care instruments developed to analyse and compare primary care in 35 countries. Qual Prim Care 2013;21:67–79. [PubMed] [Google Scholar]
- 22. Canadian Institute for Health Information. CIHI-Canada: primary health care practice-based surveys. https://www.cihi.ca/en/types-of-care/primary-health-care (accessed 6 Dec 2016).
- 23. Johns Hopkins University. PCAT: Primary Care Assessment Tools. http://www.jhsph.edu/research/centers-and-institutes/johns-hopkins-primary-care-policy-center/pca_tools.html (accessed 5 Dec 2016).
- 24. Barber SL, Huang B, Santoso B, et al. . The reform of the essential medicines system in China: a comprehensive approach to universal coverage. J Glob Health 2013;3:010303 10.7189/jogh.03.010303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Liu J, Ma H, He YL, et al. . Mental health system in China: history, recent service reform and future challenges. World Psychiatry 2011;10:210–6. 10.1002/j.2051-5545.2011.tb00059.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zhou W, Xiao S. Existing public health surveillance systems for mental health in China. Int J Ment Health Syst 2015;9:3 10.1186/1752-4458-9-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Krumholz HM, Normand SL, Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke, 1999-2011. Circulation 2014;130:966–75. 10.1161/CIRCULATIONAHA.113.007787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Krumholz HM, Nuti SV, Downing NS, et al. . Mortality, hospitalizations, and expenditures for the medicare population aged 65 years or older, 1999-2013. JAMA 2015;314:355–65. 10.1001/jama.2015.8035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Spatz ES, Beckman AL, Wang Y, et al. . Geographic variation in trends and disparities in acute myocardial infarction hospitalization and mortality by income levels, 1999-2013. JAMA Cardiol 2016;1:255–65. 10.1001/jamacardio.2016.0382 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-016195supp001.pdf (324.7KB, pdf)