Abstract
Background:
Diabetes mellitus and hypertension have a high prevalence of growth in all countries threatening to become a global epidemic risk, thus the quality of life this category of patients is extremely important. The aim of this study was to assess the socioeconomic determinants affecting the quality of life among diabetic and hypertensive patients.
Patient and Methods:
A descriptive cross-sectional study was conducted in a rural family health care center in El-Batanon village, in the delta region of Menoufia, Egypt. The recruited sample population was 401 participants over six month's context time frame (diabetic and hypertensive participants were 224 and 117 respectively). All participants were interviewed using a questionnaire to assess the demographic characteristics, socioeconomic status, type, duration and treatments of illness and the 36-Item Short Form Health Survey.
Results:
Patients with Diabetes presented a poorer health related quality of life than those with hypertension in perceived health in the areas of role-physical (RP) (P < 0.05), bodily pain (BP) (P < 0.001), general health (GH) (P < 0.05), vitality (VT) (P < 0.05), social functioning (SF) (P < 0.001) and role-emotional (RE) (P < 0.001). Age, Sex, Family size, socioeconomic score and occupation were the main Socioeconomic Determinants affecting the quality of life among diabetic and hypertensive patients.
Conclusion:
Diabetes and hypertension seem to comparably impair the health-related quality of life. There is a need to develop and implement effective targeted intervention to help the patients to cope with their life in a better way.
Keywords: Diabetes mellitus, hypertension, quality of life
Background
In 1948, the World Health Organization (WHO) had a new view for health, stating that health shouldn’t be defined not only the absence of disease and disability but also by the presence of physical, mental, and social well-being.[1] Recently, there has been a growing awareness in the quality of life (QoL) issues, and especially in health-related quality of life (HRQoL), fueled by numerous factors, including a growing body of evidence concerning the potent effect of psychosocial factors on physical health outcome and the burden of these morbidities on work productivity and performance.[2,3] In 2013, Nearly three hundred eighty two million people had diabetes; this number is expected to rise to reach 592 million by 2035.[4] The prevalence of diabetes mellitus (DM) and hypertension (HTN) is highest in the Eastern Mediterranean Region in comparison to other regions in the world accounting 11% and 29%, respectively.[5,6]
One of the most important goals of all health interventions is to improve the QoL of persons affected by disease.[3] In the domain of physical health and illness, QoL denotes the participant's self-evaluation of health or on their perceived functional status and well-being. In chronic conditions such as HTN and DM, health-related quality of life is a principally vital outcome, given their lifelong nature and the need for daily self-management.
HRQoL was found to be poorer in diabetic participants than in the general population,[3,7,8] particularly in the self-perceived physical health domain, while there was a diverse findings on psychosocial functioning between studies.[9] HTN has also been displayed to be related with negative outcomes in HRQoL, particularly in the domain of subjectively perceived general health (GH).[10] One of the strongest and dependable predictors of the individual's morbidity and mortality experience is the socioeconomic status (SES). This finding persists across all diseases with few exceptions, continues throughout the entire life span, and extends across numerous risk factors for disease.[11]
The primary objective of this paper was to assess the socioeconomic determinants affecting the QoL among patients with diabetes and hypertension patients in a rural area. These two chronic diseases were chosen because of their high prevalence in the community and similar hazard effect on the cardiovascular system and overall health.
Patients and Methods
This study was approved by the Ethical Committee of the Menoufia University, and informed written consent was obtained from all the participants.
Patients
A cross-sectional study was conducted in the primary health care unit (PHC) of El Batanon village, Shebin EL-Kom district, Menoufia governorate. It is a rural primary health care and was randomly selected out from all rural health-care units in Menoufia governorate. This study was conducted from May 2016 to October 2016. All the eligible patients with diabetes and hypertensionattending the PHC were offered to participate in the study. Eligible criteria for patients with diabetes were confirmed to have type 2 diabetes mellitus (DM) based on the American Diabetes Association criteria.[12] Hypertensive patient confirmed to have HTN based on the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure-7.[13] Exclusion criteria were the presence of complication of the illness or other chronic diseases such as co-morbidity with HTN or cardiovascular disease or renal failure or obesity or pulmonary diseases and being unavailable to complete the questionnaire.
The recruited participants were 224 patients with diabetes out of 235 diabetic attendees and 177 hypertensive patients out of 183 attendees.
Methods
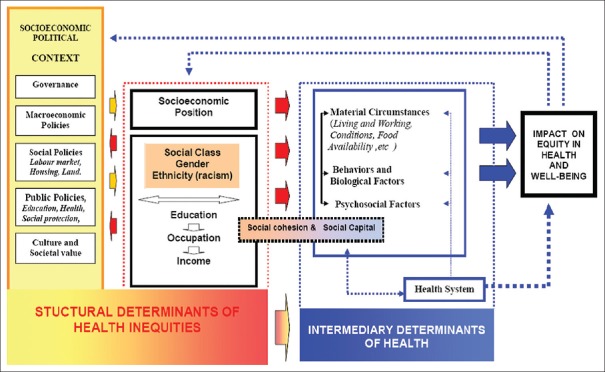
A registered analytic framework by the WHO Commission on Social Determinants of Health, 2008 that draws a structured view of the contextual drivers of changes in health structure functions, and their effects on health scheme goals was used.[14] The conceptual framework for the structural determinants was used for the health in the following dimensions; education, occupation, income, and socioeconomic position [Figure 1]. The participants were: recruited during their attendance to the family health center seeking treatment, follow-up, or coming with a patient. All the participants were subjected to a questionnaire: first part to collect sociodemographic and SES data regarding the respondents’ characteristics.[15] Second part Medical Outcome Study Short-Form Health Survey (SF-36). Psychometric characteristics of this instrument have shown its adequate reliability and validity.[16] The questionnaire contains 36 items integrated in multi-item scales measuring eight generic health concepts that physical functioning (PF), social functioning (SF), role physical (RP), bodily pain, mental health, role emotional (RE), vitality, and GH. Scoring included a transformation of raw scores for each subscale to a 0–100 scale, with higher scores representing better QoL. All participants were interviewed using the questionnaire which took early10 min to be filled.
Figure 1.
Framework by WHO commission on social determinants of health
Data entry and data analysis using (SPSS) took about 2 months. Results were analyzed using Statistical Package for the Social Sciences version 16 (SPSS Inc., Chicago, Il, USA). Qualitative data were described using number and percent. Quantitative data were described using range (minimum and maximum), mean, standard deviation, and median. Two types of statistics were performed; Student's t-test was used to compare normally distributed data for two groups for and Chi-squared (χ2) test was used to compare qualitative variable. The significance of the obtained results was judged at the 5% level and P ≤ 0.05 was considered statistically significant.
Results
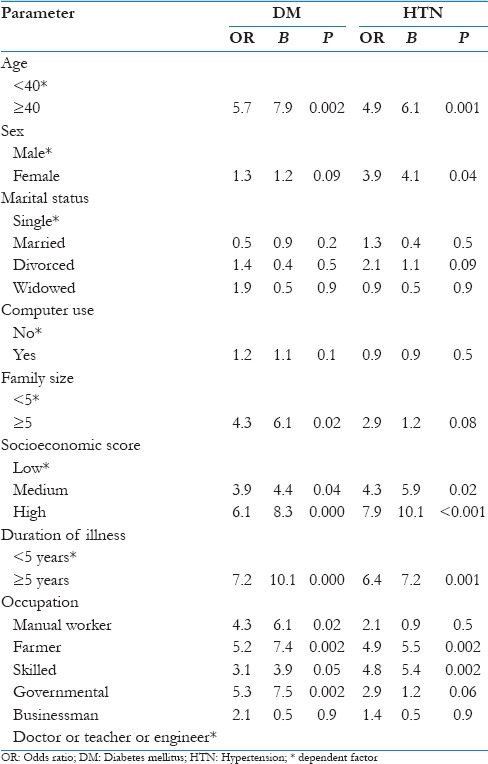
Participants’ sociodemographic characteristics are presented in Table 1 that showed the studied groups were mainly of the male gender, 46.2% in the diabetes mellitus group and 50.3% in HTN group. The average age of the studied group was 51.7 ± 8.5 years and 46.6 ± 8.2 years for diabetic and hypertensive patients, respectively. Criteria of illness are shown in Figure 2 where the majority of the patients were on oral drugs. Mean scores for the SF-36 subscales of the participants are shown in Table 2. Patients with HTN had significantly higher QoL scores than patients with diabetes for PF, RP, GH, SF, and RE. Table 3 showed the logistic regression for the determinants affecting the QoL of DM and HTN patients. Age, SES, illness duration, and occupation were strong risk predictors affecting the QoL for diabetes and HTN. The higher risk was associated with lower incomes.
Table 1.
Sociodemographic characteristics of the studied group
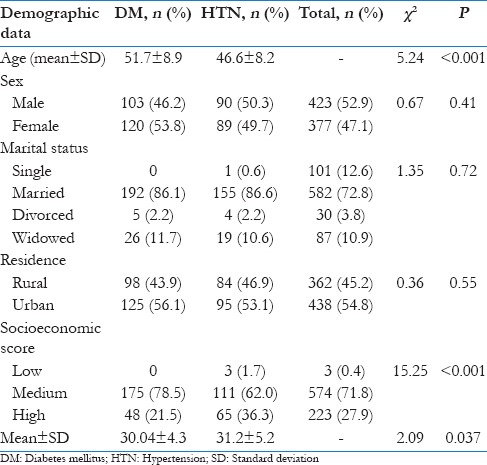
Figure 2.
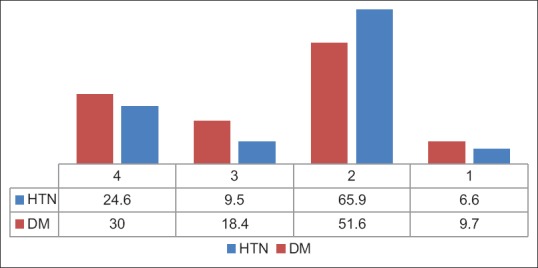
Criteria for illness. (1) Duration of illness. (2) Oral treatment %. (3) Insulin in diabetic%/Exercise in Hypertension. (4) Both 2 and 3
Table 2.
Diabetes mellitus and hypertension patients as regards health-related quality of life questionnaire
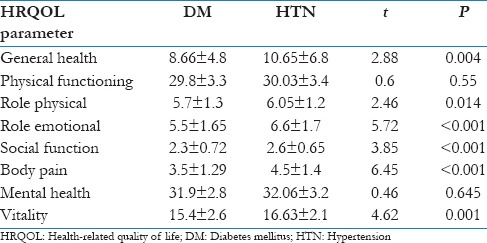
Table 3.
Logistic regression for the determinants affecting quality of life of diabetes mellitus and hypertension patients
Discussion
Our results suggest that DM and HTN have comparably negative effects on HRQoL, which supports the Assumption that both conditions impose similar self-perceived limitations in physical and mental functioning. Moreover, diabetic patients were affected more than the hypertensive patients.
However, available literature Rubin and Peyort[3] suggested that diabetes in its early stages has no impact on perceived HRQoL of the affected individuals, whereas our study found lower scores on the majority of SF-36 dimensions.
In our study, all dimensions of HRQoL were poorer in people with diabetes compared with HTN participants. This is in agreement with Hajian-Tilaki et al., despite different studied age groups.[17] However, our data didn’t embrace any information on potential nonvascular comorbidities, such as nephropathy, retinopathy, or musculoskeletal disease, which have been found to be essential predictors of HRQoL in diabetes.[3,7,18] It is possible that some individuals who had been categorized into the groups without cardiovascular comorbidities of HTN or DM had other comorbidities that possibly reduced their HRQoL. Former studies have yielded conflicting outcomes on the severity of the impact of DM and HTN on HRQoL,[19,20] without representing if the degree of impact of cardiovascular comorbidities in these two illnesses is comparable.
High SES represented a crucial risk factor as a determinant of the QoL in participants with diabetes and hypertension. This could be partly explained by the effect high SES on decreased physical activity. Another vital factor was growing in the age which is in agreement with Tailakh et al., who found it as a trend in most countries revised.[6] Similarly, females were prone nearly four times to develop HTN than males which is in concordance with many studies.[6,21]
Between-group comparisons of demographic characteristics; level of education, marital status, and employment status did not reveal statistically significant differences. Although those demographic factors influence HRQoL, their effect may be presumed to have been comparable in the studied group (DM and HTN). Taking into account the differences in sex between the studied group (DM and HTN).
Conclusion
Our results confirm preceding reports of the adverse influences of DM and HTN on participants’ well-being and operational functioning. The innovation of our study is that it displays these effect sizes are comparable. This is a useful finding for clinical practice, particularly in the early treatment of DM and HTN, at which point improvement in self-management and consequently HRQoL is still possible.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank the social research center in the American University in Cairo. Furthermore, we would like to thank all the interviewers for their patience and understanding during the data collection.
References
- 1.Callahan D. The WHO definition of ‘health’. Stud Hastings Cent. 1973;1:77–88. [PubMed] [Google Scholar]
- 2.Abu Salema M, Hegazy N, Mohamed S. The effect of diabetes and hypertension on work productivity and job satisfaction. Menoufia Med J. 2016;29:1106–11. [Google Scholar]
- 3.Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev. 1999;15:205–18. doi: 10.1002/(sici)1520-7560(199905/06)15:3<205::aid-dmrr29>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 4.Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103:137–49. doi: 10.1016/j.diabres.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Sherif S, Sumpio BE. Economic development and diabetes prevalence in Mena countries: Egypt and Saudi Arabia comparison. World J Diabetes. 2015;6:304–11. doi: 10.4239/wjd.v6.i2.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tailakh A, Evangelista LS, Mentes JC, Pike NA, Phillips LR, Morisky DE. Hypertension prevalence, awareness, and control in Arab countries: A systematic review. Nurs Health Sci. 2014;16:126–30. doi: 10.1111/nhs.12060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wändell PE. Quality of life of patients with diabetes mellitus. An overview of research in primary health care in the Nordic countries. Scand J Prim Health Care. 2005;23:68–74. doi: 10.1080/02813430510015296. [DOI] [PubMed] [Google Scholar]
- 8.Saito I, Inami F, Ikebe T, Moriwaki C, Tsubakimoto A, Yonemasu K, et al. Impact of diabetes on health-related quality of life in a population study in Japan. Diabetes Res Clin Pract. 2006;73:51–7. doi: 10.1016/j.diabres.2005.11.015. [DOI] [PubMed] [Google Scholar]
- 9.Stewart AL, Greenfield S, Hays RD, Wells K, Rogers WH, Berry SD, et al. Functional status and well-being of patients with chronic conditions. Results from the Medical Outcomes Study. JAMA. 1989;262:907–13. [PubMed] [Google Scholar]
- 10.Lawrence WF, Fryback DG, Martin PA, Klein R, Klein BE. Health status and hypertension: A population-based study. J Clin Epidemiol. 1996;49:1239–45. doi: 10.1016/s0895-4356(96)00220-x. [DOI] [PubMed] [Google Scholar]
- 11.Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: How education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992;82:816–20. doi: 10.2105/ajph.82.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Diabetes Association. (2) Classification and diagnosis of diabetes. Diabetes Care. 2015;38(Suppl 1):S8–16. doi: 10.2337/dc15-S005. [DOI] [PubMed] [Google Scholar]
- 13.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 14.Marmot M, Friel S, Bell R, Houweling TA, Taylor S. Commission on social determinants of health. Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet. 2008;372:1661–9. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- 15.Fahmy SI, Nofal LM, Shehata SF, El Kady HM, Ibrahim HK. Updating indicators for scaling the socioeconomic level of families for health research. J Egypt Public Health Assoc. 2015;90:1–7. doi: 10.1097/01.EPX.0000461924.05829.93. [DOI] [PubMed] [Google Scholar]
- 16.Ware JE., Jr SF-36 health survey update. Spine (Phila Pa 1976) 2000;25:3130–9. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- 17.Hajian-Tilaki K, Heidari B, Hajian-Tilaki A. Solitary and combined negative influences of diabetes, obesity and hypertension on health-related quality of life of elderly individuals: A population-based cross-sectional study. Diabetes Metab Syndr. 2016;10(2 Suppl 1):S37–42. doi: 10.1016/j.dsx.2016.01.018. [DOI] [PubMed] [Google Scholar]
- 18.Wändell PE, Brorsson B, Aberg H. Quality of life in diabetic patients registered with primary health care services in Sweden. Scand J Prim Health Care. 1997;15:97–102. doi: 10.3109/02813439709018495. [DOI] [PubMed] [Google Scholar]
- 19.Alonso J, Ferrer M, Gandek B, Ware JE, Jr, Aaronson NK, Mosconi P, et al. Health-related quality of life associated with chronic conditions in eight countries: Results from the International Quality of Life Assessment (IQOLA) Project. Qual Life Res. 2004;13:283–98. doi: 10.1023/b:qure.0000018472.46236.05. [DOI] [PubMed] [Google Scholar]
- 20.Smith DW. The population perspective on quality of life among Americans with diabetes. Qual Life Res. 2004;13:1391–400. doi: 10.1023/B:QURE.0000040785.59444.7c. [DOI] [PubMed] [Google Scholar]
- 21.Mirzajani M, Mirzaei M. Population Attributable Fraction of Ischemic Heart Disease Associated to Hypertension in the Middle East and North Africa. Journal of Community Health Research. 2015;4:38–46. [Google Scholar]