Abstract
Introduction:
Anemia is a condition, in which the number of red blood cells (RBC) and the hemoglobin (Hb) is insufficient to meet the body's physiologic needs. Hypoferritinemia without anemia (HWA) could cause masked clinical manifestations as general weakness, easy fatigability, depressed mode, and hair loss but with normal complete blood count (CBC) parameters. HWA is deferent from iron deficiency anemia (IDA) because there is no reduction in the RBC, Hb, or any of the other parameters of the CBC. In HWA, the hypoferritinemia could be missed because serum ferritin not always requested by general practitioners.
Materials and Methods:
A retrospective study conducted on 6993 patients of hypoferritinemia patients from our computerized database from 2010 to 2016. The parameters investigated to detect HWA disorder were serum ferritin, RBC, Hb, hematocrit, mean corpuscular volume, and mean corpuscular hemoglobin.
Results:
HWA is found in 130 (0.018%) hypoferritinemia patients, in a ratio 1.7–1 females to male.
Conclusion:
HWA is a masked hematology disorder which needs new nomenclature to distinguish it from IDA because they are two deferent disorders although both of them have low serum ferritin. HWA is not a latent IDA because it could happen in patients whom will not get anemia as in polycythemia patients on recurrent veinesection treatement.
Keywords: Anemia, ferritin, hypoferritinemia, iron
Introduction
Anemia according to the WHO is a condition, in which the number of red blood cell (RBC) is insufficient to meet the body's physiologic needs. Hemoglobin (Hb) concentration alone cannot be used to diagnose the cause of anemia.[1] Anemia also refers to a less than normal mean for age and sex of the RBC mass, amount of Hb, and/or volume of packed RBCs. Hypoferritinemia means low iron storage in the ferritin form, which could manifest as general weakness, easy fatigability, depressed mode, palpitation, and hair loss.[2] Iron is present in all cells in the human body and has several vital functions, such as: carrying oxygen to the tissues from the lungs as a key component of the Hb molecule, facilitating oxygen use and storage in the muscles as a component of myoglobin, and acting as a transport medium for electrons within the cells in the form of cytochromes and as an integral part of enzyme reactions in various tissues. Too little iron can interfere with these vital functions and lead to morbidity.[3]
Hypoferritinemia diagnosed when the level of serum ferritin reduced below 11 ng/ml in females and below 23 ng/ml in males in our institute's reference range. Hypoferritinemia caused by decreased iron intake, as part of the general poor diet, or due to low gastrointestinal absorption that happens to postbariatric surgery. It also happens in Crohn's disease, ulcerative colitis and celiac disease, hemorrhoids, colon cancer, peptic ulcer, menorrhagia, and hematuria. It also could be due to increase iron demands in pregnancy and puberty.[4] Rarely, hypoferritinemia may be due to disorders of iron metabolism.[5] The aim of this study is to highlight the importance of hypoferritinemia without anemia (HWA) and to distinguish it by the nomenclature HWA to make it known disorder among general practitioners and other physicians because it is easy to be missed while the patient has long-standing suffering of obscure general weakness.
Materials and Methods
The data gathered from our institute Amiri Hospital and its regional polyclinics electronic database. The period of this cross-sectional retrospective study was from 2010 to 2016. The total number of the samples 4370 females and 2623 males. Age of the patients was from 15 to 88 years old. The inclusion criteria were adult patients with hypoferritinemia and with normal complete blood counts (CBCs) parameters. The exclusion criteria were normal or high serum ferritin. The CBC performed in Coulter LH-750/755 analyzer. Serum ferritin level was done by Beckman Coulter, UniCel DXI 800 Access immunoassay system. Normal range of serum ferritin for adult female participants is 11–306.8 ng/ml and for adult male is 23.9–336.2 ng/ml according to our laboratory's reference range.
Results
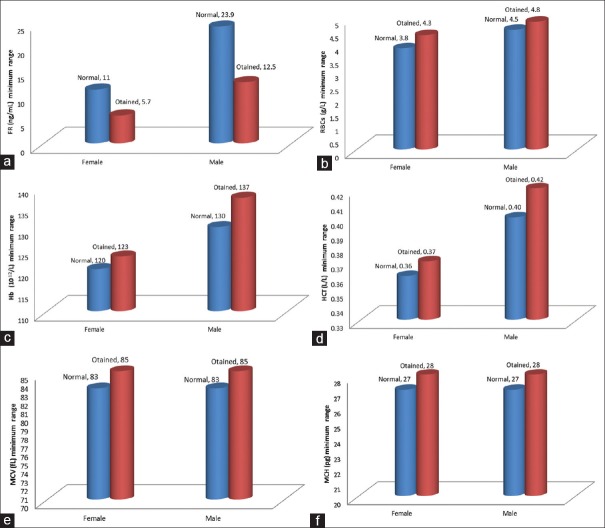
A total of 4370 hypoferritinemia females were tested, 80 found to have HWA (low ferritin with normal RBC, Hb, mean corpuscular volume [MCV], and mean corpuscular hemoglobin [MCH]). In the male group 2623 patients were tested, 50 found to have HWA. All HWA patients had low serum ferritin, but they had normal CBC parameters (RBC, Hb, hematocrit [Hct], MCV, and MCH); the results are shown in Table 1 and Figure 1.
Table 1.
Female hypoferritinemia without anemia and male hypoferritinemia without anemia normal complete blood count referral ranges
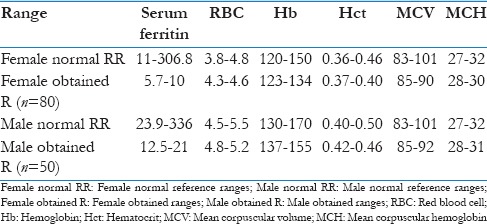
Figure 1.
(a) Low Serum Ferritin level in HWA. (b-f) Normal RBC, Hb, Hct, MCV and MCH Levels in HWA
Discussion
This study results showed hypoferritinemia in the presence of normal RBC, Hb, MCV, and MCH [Table 1]. Hence, HWA is a masked disorder because serum ferritin test is not performed routinely when the CBC parameters are normal. Furthermore, serum ferritin is never done in the family clinics or in the primary care Centers in many countries. Serum iron, total iron-binding capacity, and transferrin saturation are easily available tests, but it is reported in the literature that they are less sensitive than serum ferritin in assessing iron status;[6] low serum ferritin with normal CBC was discussed in the literature; as a latent iron deficiency anemia (IDA), it was considered an early stage or masked form of IDA.[7] This study is to classify the phenomena of normal CBC in the presence of low serum ferritin as an independent disorder entity because patients could present in HWA status but never proceed to IDA as in polycythemia cases on recurrent veinesection treatement.[8] This study which was conducted on a total of 6993 patients with low serum ferritin, 4370 females and 2623 males, HWA found in 130 (0.018%) of the cases. It was 80 (62%) cases in female and 50 (38%) cases in male patients. HWA is a hypoferritinemia with normal reference range of RBC, Hb, Hct, MCV, and MCH, or even Hb could be high [Table 2]. HWA patients usually complain of chronic undiagnosed signs and symptoms of feeling general weakness, depressed mode, and hair loss.[9] However, HWA and IDA considered in this study as two different disorders, as IDA has an anemia with changes in the CBC parameters and characteristic hematological morphological changes in the peripheral blood film, while HWA does not have anemia, nor any morphological or CBC parameters changes. Furthermore, IDA is an easily diagnosed with its microcytic hypochromic anemia while HWA is a masked disorder with normal CBC parameters and with normocytic normochromic picture under the light microscope. Both the physicians and patients must be more aware and oriented about HWA for better diagnosis, management, and follow-up. HWA disorder has its own entity as a disorder which could cause long-standing undiagnosed signs and symptoms of feeling weak and unwell. Latent IDA is a status proceed IDA while HWA could stay as HWA without proceeding to IDA as in myeloproliferative neoplasms in Polycythema rubra vera, kessential thrombocythemia, early myelofibrosis, and other myeloproliferative neoplasms disorders.[10] HWA should be involved more in the public and in community health teaching programs. HWA is an area of hot research work in the presence of the new tool research implemented in IDA investigations as hepcidin and transferrin receptor, which are key regulators of iron metabolism, absorption, and serum ferritin level.[11]
Table 2.
The differences between iron deficiency anemia and hypoferritinemia without anemia disorders

Limitation
In this retrospective study, we do not know about patients whom on iron treatment which could affect the level of serum ferritin and the CBC status.
Conclusion
HWA is a masked hematology disorder because RBC, Hb, MCV, and MCH are all within normal ranges, but the patient could complain of the long-standing undiagnosed status of feeling unwell. HWA disorder could be missed when serum ferritin is not checked. HWA could happen in myeloproliferative disorders as polycythemia without being a latent IDA; HWA is a deferent disorder entity, so we need to distinguish this disorder with a special nomenclature to make it known to the general practitioners, which will help for its detection and treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Great thankful for the hematology and biochemistry laboratories staff in Amiri Hospital for facilitating this work.
References
- 1.World Health Organization. Haemoglobin Concentrations for the Diagnosis of Anemia and Assessment of Severity.Vitamin, and Mineral Nutrition Information System. (WHO/NMH/NHD/MNM/11.1) Geneva: World Health Organization; 2011. [Google Scholar]
- 2.Pavord S, Myers B, Robinson S, Allard S, Strong J, Oppenheimer C. UK Guidelines on the Management of Iron Deficiency in Pregnancy. British Committee for Standards in Haematology; 2011;156:588–600. doi: 10.1111/j.1365-2141.2011.09012.x. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Recommendations to prevent and control iron deficiency in the United States. MMWR Morb Mortal Wkly Rep. 1998;47:1. [Google Scholar]
- 4.Abbaspour N, Hurrell R, Kelishadi R. Review on iron and its importance for human health. J Res Med Sci. 2014;19:164–74. [PMC free article] [PubMed] [Google Scholar]
- 5.Kotze MJ, van Velden DP, van Rensburg SJ, Erasmus R. Pathogenic mechanisms underlying iron deficiency and iron overload: New insights for clinical application. EJIFCC. 2009;20:108–23. [PMC free article] [PubMed] [Google Scholar]
- 6.Wish JB. Assessing iron status: Beyond serum ferritin and transferrin saturation. Clin J Am Soc Nephrol. 2006;1(Suppl 1):S4–8. doi: 10.2215/CJN.01490506. [DOI] [PubMed] [Google Scholar]
- 7.Raza M, Amanat ST, Hussain T, Shakoor HA, Asghar M. Latent iron deficiency and iron deficiency anaemia in hypoferritinemic patients. J Rawalpindi Med Coll. 2014;18:139–41. [Google Scholar]
- 8.Pearson TC, Messinezy M, Westwood N, Green AR, Bench AJ, Green AR, et al. A polycythemia vera update: Diagnosis, pathobiology, and treatment. ASH Edu Book. 2000;2000:51–68. doi: 10.1182/asheducation-2000.1.51. [DOI] [PubMed] [Google Scholar]
- 9.Rushton DH, Dover R, Sainsbury AW, Norris MJ, Gilkes JJ, Ramsay ID. Why should women have lower reference limits for haemoglobin and ferritin concentrations than men? BMJ. 2001;322:1355–7. doi: 10.1136/bmj.322.7298.1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Derossi SS, Garfunkel A, Greenberg MS. Hematologic Disease. Principles of Medicine: Diagnosis & treatment. 10th Ed. Hamilton, Ontario: BC Decker; 2003. pp. 429–453. [Google Scholar]
- 11.Pasricha SR, McQuilten Z, Westerman M, Keller A, Nemeth E, Ganz T, et al. Serum hepcidin as a diagnostic test of iron deficiency in premenopausal female blood donors. Haematologica. 2011;96:1099–105. doi: 10.3324/haematol.2010.037960. [DOI] [PMC free article] [PubMed] [Google Scholar]