Abstract
Objective
α-Synuclein is critical to the pathogenesis of Parkinson’s disease (PD). Few studies examined the plasma levels of α-synuclein due to the exceptionally low level of α-synuclein in plasma compared with cerebrospinal fluid. We aimed to investigate plasma α-synuclein in patients with PD of different disease severity.
Methods
There were total 114 participants, including 80 patients with PD and 34 controls, in the study. Participants received a complete evaluation of motor and non-motor symptoms, including cognitive function. We applied immunomagnetic reduction-based immunoassay to measure plasma levels of α-synuclein.
Results
Plasma levels of α-synuclein were significantly higher in patients with PD compared with controls (median: 1.56 pg/mL, 95% CI 1.02 to 1.98 pg/mL vs 0.02 pg/mL, 95% CI 0.01 to 0.03 pg/mL; p<0.0001). Although there was a significant increase in plasma α-synuclein levels in PD patients with a higher Hoehn-Yahr (H-Y) stage, there was no correlation with motor symptom severity, as assessed by Unified Parkinson’s Disease Rating Scale part III scores, after confounders (age, gender, and disease duration) were taken into account. However, plasma α-synuclein levels were significantly higher in PD patients with dementia (PDD) than in PD patients with mild cognitive impairment (PD-MCI) or normal cognition (0.42 pg/mL, (95% CI 0.25 to 0.93) for PD with normal cognition; 1.29 pg/mL (95% CI 0.76 to 1.93) for PD-MCI and 4.09 pg/mL (95% CI 1.99 to 6.19) for PDD, p<0.01) and were negatively correlated with Mini-Mental State Examination scores (R2-adjusted=0.3004, p<0.001), even after confounder adjustment.
Conclusions
Our data suggest that plasma α-synuclein level correlates with cognitive decline but not motor severity in patients with PD. Plasma α-synuclein could serve as a surrogate biomarker for patients at risk of cognitive decline.
Keywords: Parkinson’s disease, Biomarker, α-synuclein, cognitive decline, dementia
Introduction
Parkinson’s disease (PD) is one of the most common neurodegenerative disorders affecting more than 1% of the global population over the age of 65, with an incidence rate likely to double by 2030.1 The diagnosis of PD is primarily based on clinical presentations, while the pathology stage of Lewy body deposition has already advanced,2 with more than 50% of dopaminergic neurons have been lost when motor symptoms are evident.3 Additionally, non-motor symptoms, for example rapid eye movement (REM) stage sleep behaviour disorder, constipation, depression and olfactory loss, can precede motor symptoms by decades.4 Unfortunately, reliable biomarkers to support an early PD diagnosis at this premotor stage are not yet available. Although dopaminergic treatments provide symptomatic benefit for some of the motor symptoms of the disease, their long-term use is problematic. As the disease progresses, patients with PD deteriorate in their motor aspects and in cognitive function,5 which is one of the most disabling non-motor features of PD. Therefore, there is a currently unmet need to identify biomarkers that could identify these patients at earlier disease stages to better predict disease progression and possible early therapeutic interventions.
PD is characterised by the presence of Lewy bodies containing aggregated α-synuclein, which is also present in human body fluids including cerebrospinal fluid (CSF) and blood plasma.6 Accordingly, the majority of body fluid biomarker studies have studied CSF samples of patients with PD, either to assess disease risk or to predict cognitive deterioration.5 7 However, thus far, results have been inconsistent other than to identify a consistently lower level of amyloid-ß in PD patients with dementia (PDD) versus PD patients with normal cognition.8–10 The relatively invasive procedure for collecting CSF has led to investigations of serum or plasma as alternatives. Currently, CSF, serum or plasma biomarkers are mainly analysed using ELISA, or similar immunoassay techniques. These assays are often performed manually and are therefore difficult to standardise, which has resulted in substantial variability in measurements between clinical centres and laboratories.11 Plasma levels of α-synuclein are also exceptionally low compared with CSF, which has hampered the use of ELISA in accurately detecting plasma α-synuclein.12 Consequently, studies exploring plasma levels of α-synuclein and their association with disease risk and progression in patients with PD are lacking.
We previously developed an ultra-sensitive immunoassay utilising immunomagnetic reduction (IMR),13 14 which could quantitatively detect biomolecules at ultra-low concentrations with a fg/mL limit of detection. This would theoretically facilitate measurements of plasma α-synuclein from control subjects and patients with PD.15 IMR uses antibody-functionalised magnetic nanoparticles that are well dispersed in reagent and that can attach to target biomolecules over a large total binding area due to their nano-scaled particle sizes, contributing to an ultra-high sensitivity when compared with traditional immunoassay. In this study, we aimed to utilise this IMR-based immunoassay to investigate plasma levels of α-synuclein in healthy control subjects and in patients with PD of varying motor and cognitive status. This would allow us to evaluate the plausibility of using this easily accessible plasma marker to predict both disease risk and severity of PD.
Methods
Study participants
Patients with PD were recruited from the movement disorder clinics of the National Taiwan University Hospital, a tertiary referral centre in Taiwan. PD was diagnosed according to the United Kingdom PD Society Brain Bank clinical diagnostic criteria.3 We excluded subjects who had any of the following signs or symptoms, as these would suggest atypical or secondary parkinsonism syndromes: multiple system atrophy, progressive supranuclear palsy, corticobasal ganglionic degeneration, vascular parkinsonism and neuroleptic agent-related parkinsonism. None of the subjects had a parental consanguineous marriage. Mutations of previously reported PD causative genes were excluded, including SNCA, Parkin, PINK1, DJ-1, ATP13A2, PLA2G6, FBXO7, LRRK2, HtrA2 and CHCHD2. 16 17 Healthy control subjects, who were neurologically normal patients visiting our clinics, or spouses and accompanied friends of the PD patients, were recruited from the same institute. Our research protocols were reviewed by the institutional ethics board committee of the National Taiwan University Hospital, with all subjects having provided informed consent.
Evaluation of motor and non-motor symptoms
Motor symptom severity was evaluated using the motor subscale of the Unified Parkinson’s Disease Rating Scale (UPDRS part III)18 and Hoehn-and-Yahr (H-Y) staging.19 Cognition was examined with the Mini-Mental State Examination (MMSE).20 PDD was diagnosed according to the recommended diagnostic criteria of the Movement Disorder Society (MDS) task force,21 with an MMSE score of 25 or less was the cut-off for identifying significant cognitive impairment in patients with PD, as well as impairment of instrumental activities of daily living (eg, inability to manage finances and cope in social situations).21 22 We also evaluated clinical dementia rating (CDR) scale for all the participated subjects.23 The CDR rates the severity of dementia using a five-point scale that rates the severity of signs and symptoms in the six cognitive categories of memory, orientation, judgement and problem solving, community affairs, home life and hobbies, and personal care. The CDR is completed by a neuropsychiatrist after performing a face-to-face, semi-structured interview with the patient and a reliable caregiver. In each cognitive category, the patient receives a score of 0 (no cognitive impairment) to 3 (severe cognitive impairment). We excluded patients with severe dementia, defined as CDR scale more than 3,23 to make sure the recruited PDD patients can understand the oral instructions and complete the non-motor symptoms evaluations. PD with mild cognitive impairment (PD-MCI) was diagnosed according to the MDS task force diagnostic criteria using the level I global cognitive function test.24 We applied MMSE score of 26 to 28 as a possible PD-MCI diagnostic feature with reported sensitivity and specificity rates of 0.92 and 0.42, respectively,25 together with a preservation of instrumental activities of daily living. Other non-motor symptoms of patients with PD were assessed by the Non-Motor Symptom Assessment Scale (NMSS)26 and the Autonomic Scale for Outcomes in PD (SCOPA-AUT).27
Measurement of plasma α-synuclein
Ten millilitres of venous blood was drawn from each participant at enrollment. Blood samples were centrifuged (2500 g for 15 min) within 1 hour of collection, and the plasma was aliquoted into cryotubes and stored at −80°C for less than 3 months before IMR testing. The reagent for assaying α-synuclein consists of magnetic Fe3O4 nanoparticles (MF-DEX-0060, MagQu) bio-functionalised with monoclonal antibodies (sc-12767, Santa Cruz Biotech) against monomers of α-synuclein. Eighty microlitres of reagent was mixed with 40 µL of plasma for the measurement of α-synuclein concentration via IMR. Details of the methodologies to immobilise antibodies onto magnetic Fe3O4 nanoparticles, to measure the magnetic concentration of the immunocomplex, and validation assay have been published previously.15 In brief, the reagent for IMR consists of magnetic nanoparticles functionalised with antibodies against α-synuclein was dispersed in pH 7.2 phosphate-buffered saline (MF-ASC-0060, MagQu). The reagent was superparamagnetic with the saturated magnetisation of 0.3 emu/g. After mixing the reagent and the tested plasma sample, each mixture was put into a superconducting-quantum-interference-device (SQUID)-based alternative current (ac) magnetosusceptometer (XacPro-S, MagQu) to determine the time-dependent ac magnetic susceptibility, which approximates the association between magnetic nanoparticles and α-synuclein molecules in the plasma.15 Because of the association between the antibody-functionalised magnetic nanoparticles and the target biomarkers, the ac magnetic susceptibility of the mixture was reduced. This reduction in the magnetic susceptibility due to the association between magnetic nanoparticle and α-synuclein molecule can be sensed by high-Tc SQUID magnetometer and is referred to as the IMR signal. The IMR signal is therefore a function of the concentration of α-synuclein. We previously have performed a standard curve analysis to examine the robustness of the IMR method to detect plasma α-synuclein.15 We tested the dynamic range of plasma α-synuclein level using the IMR signals, which were denoted by φα-syn,IMR. The correlation between φα-syn,IMR and the concentration of α-synuclein was examined. Duplicate measurements were performed for IMR signals at each concentration of α-synuclein solution. We observed that among the concentration range of α-synuclein between 0.3 fg/mL and 310 pg/mL, the slop of the correlation line is 0.93 and the coefficient of determination R2 is 0.999, indicating that the IMR assay is a sensitive and robust method to detect plasma α-synuclein level.
Statistical analyses
Numerical variables were expressed as the mean±SD of the mean or median with 95% CI. For variables following a Gaussian distribution, data were compared using the two-tailed t-test, and multiple comparisons were performed using analysis of variance (ANOVA). To control for possible confounders (eg, age, gender and disease duration), ANOVA was used for group comparisons, including, as covariates, any demographic variable that differed significantly between groups. For variables not following a normal distribution, data was compared using the Mann-Whitney test, which is the non-parametric equivalent of the independent samples t-test, and Kruskal-Wallis test was used when there are more than two groups. Correlations between variables were graphically analysed using the slope of the regression line including the 95% CI. The correlation between variables was explored with multiple linear regression analyses, with the covariance of the model (R2) and the standardised correlation coefficient presented. We performed all analyses using the Stata software, version 9. A p value <0.05 was considered significant.
Results
Clinical characteristics
A total of 114 study participants comprising 80 patients with PD and 34 normal control subjects were enrolled. Table 1 summarises the demographic and clinical information for all participants. While the mean age of the PD group was higher than that of the control (69.6±12.3 vs 61.9±9.5, p<0.01), there were no significant differences in either gender or education levels between the two groups. However, there was a larger proportion of male PD participants than male controls (52% PD; 48% controls). Patients with PD were classified into three groups according to their cognitive function: PD with normal cognition (defined as MMSE >28, n=30), PD-MCI (defined as MMSE >25 but ≦28, n=21) or PDD (defined as MMSE≦25, n=29). Mean UPDRS part III scores and H-Y stages during the ‘on’ and ‘off’ state are detailed in table 1.
Table 1.
Clinical characteristics of study participants
| Normal control (n=34) |
PD (n=80) |
PD (n=80) | ||||
| PD with normal cognition (n=30) |
PD-MCI (n=21) |
PDD (n=29) |
p Value | |||
| Age (years) | 61.9±9.5 | 69.6±12.3 | 60.7±10.6 | 68.9±11.1 | 79.9±5.5 | p<0.01** |
| Gender (male, %) | 48.5 | 52.2 | 48.3 | 57.2 | 57.8 | p=0.10 |
| Education (years) | 11.8±1.8 | 13.1±2.2 | 13.1±2.2 | 13.4±1.8 | 12.8±2.6 | p=0.46 |
| Disease duration (years) | N.A. | 7.5±5.2 | 4.6±2.3 | 8.1±6.3 | 9.2±7.3 | p=0.03* |
| MMSE | 29.2±0.8 | 24.3±5.7 | 28.7±0.9 | 25.3±1.8 | 17.8±5.4 | p<0.01** |
| Hoehn-Yahr stage (on) | N.A. | 1.8±0.9 | 1.4±0.8 | 1.6±0.8 | 2.3±1.0 | p=0.01* |
| Hoehn-Yahr stage (off) | N.A. | 2.6±1.1 | 2.3±1.1 | 2.5±0.9 | 3.3±1.1 | p=0.01* |
| UPDRS part III (on) | N.A. | 17.4±9.6 | 13.9±7.5 | 17.6±10.1 | 21.8±9.9 | p=0.02* |
| UPDRS part III (off) | N.A. | 32.4±13.9 | 27.7±12.8 | 32.8±15.3 | 38.3±12.5 | p=0.03* |
| NMSS (on) | N.A. | 32.4±13.9 | 36.9±7.4 | 31.5±6.2 | 32.1±14.3 | p=0.55 |
| SCOPA-AUT (on) | N.A. | 10.7±6.8 | 12.4±2.1 | 9.9±5.6 | 10.9±6.90.7 | p=0.49 |
Numbers are expressed as mean±SD.
*p<0.05; **p<0.01. The p values were analysed by parametric t-test.
MCI, mild cognitive impairment; MMSE, Mini-Mental Status Examination; N.A., not available; NMSS, Non-Motor Symptom Assessment Scale; PD, Parkinson’s disease; PDD, Parkinson’s disease with dementia; SCOPA-AUT, The Scale for Outcomes in PD for Autonomic Symptoms; UPDRS, Unified Parkinson’s Disease Rating Scale.
Plasma α-synuclein measurements
Plasma levels of α-synuclein were significantly higher in patients with PD compared with controls (figure 1, median level of plasma α-synuclein: PD vs controls: 1.56 pg/mL (95% CI 1.02 to 1.98 pg/mL) vs 0.02 pg/mL (95% CI 0.01 to 0.03 pg/mL) (p<0.0001 by Mann-Whitney test). With regard to the possible influence of age on plasma concentrations of α-synuclein,28 we examined plasma α-synuclein levels in control subjects of varying age. Consistent with our previous data,15 we did not find any significant correlation between age and plasma α-synuclein levels in control subjects (correlation coefficient r=0.1602, p=0.195, online supplementary figure 1).
Figure 1.
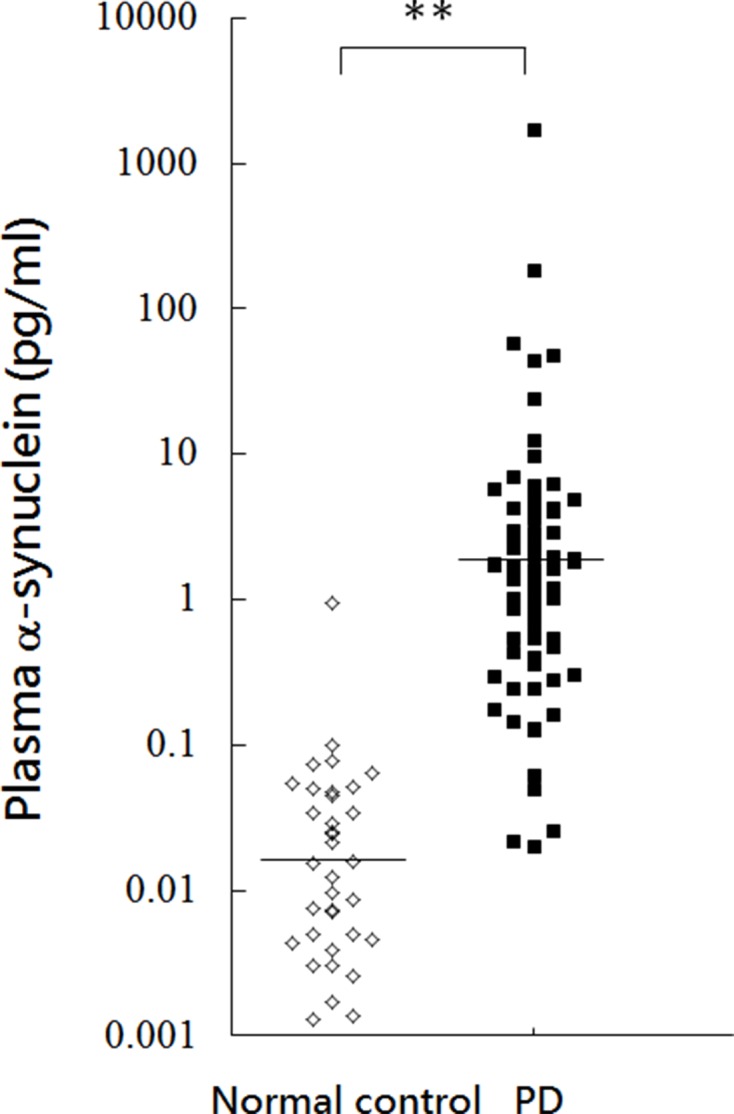
Plasma α-synuclein levels for all participants in the study. Plasma α-synuclein levels of normal controls and patients with PD. The plasma α-synuclein level was significantly increased in patients with PD compared with normal control subjects (p<0.001). PD, Parkinson’s disease. *, p<0.05; **, p<0.01.
jnnp-2016-314857supp001.jpg (45.9KB, jpg)
Correlation between plasma α-synuclein levels and motor severity
We next examined whether the plasma levels of α-synuclein correlated with disease severity, either in terms of motor or non-motor symptoms. For the motor symptom severity evaluation, we observed that plasma α-synuclein levels were higher in PD patients with a higher H-Y stage (figure 2). Specifically, the median plasma α-synuclein levels were 1.06 pg/mL (95% CI 0.52 to 1.62), 0.73 pg/mL (95% CI 0.36 to 1.84), 1.48 pg/mL (0.41–15.70) and 1.64 pg/mL (0.71–11.19) for H-Y stage I–IV, respectively (p<0.01 by Kruskal-Wallis test). However, the simultaneous inclusion of age, gender and disease duration in the multivariate linear regression model resulted in a significant correlation between motor symptom severity (as assessed by UPDRS part III scores) and disease duration only; no significant correlation was found between motor symptom severity and plasma levels of α-synuclein (table 2).
Figure 2.
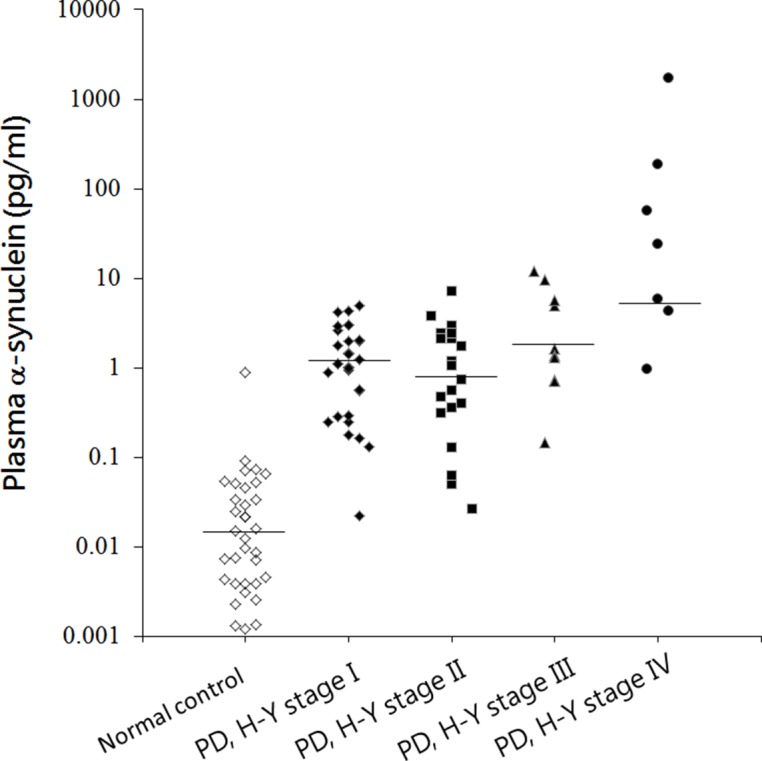
Plasma α-synuclein levels in PD patients with variable motor severity. The plasma α-synuclein level was markedly increased in PD patients with more severe motor disability as assessed by Hoehn-Yahr stage (p<0.01). PD, Parkinson’s disease; H-Y stage, Hoehn-Yahr stage.
Table 2.
Multivariate linear regression models for motor symptom severity in patients with PD as assessed by UPDRS part III scores
| Independent variables | Coefficient | SE | r | t | p Value |
| Constant | −0.530 | ||||
| Disease duration (years) | 0.361 | 0.177 | 0.303 | 2.038 | 0.048* |
| Age (years) | 0.173 | 0.107 | 0.246 | 1.625 | 0.112 |
| Gender (male) | 4.021 | 2.688 | 0.228 | 1.496 | 0.142 |
| Plasma α-synuclein level | 0.213 | 0.176 | 0.186 | 1.213 | 0.232 |
In this model, the motor score of UPDRS (part III) in the on state was set as the dependent variable, with age, gender, disease duration and plasma level of α-synuclein set as independent variables. r: correlation coefficient based on the model of multiple linear regression; t: t value for the coefficient of each parameter in the model; p: for r or t; R2-adjusted=0.1998, p=0.01 for the model. *: statistically significant, p<0.05; **: p<0.01.
PD, Parkinson’s disease; UPDRS, Unified Parkinson’s Disease Rating Scale.
Correlation between plasma α-synuclein levels and the severity of non-motor symptoms
As cognitive decline is one of the most disturbing non-motor symptoms of PD, we then examined the relationship between plasma levels of α-synuclein and PD patients with various levels of cognitive ability. While there were no robust correlations between α-synuclein levels and NMSS or SCOPA-AUT data (data not shown), we observed that plasma α-synuclein levels were significantly higher in PD patients with more severe cognitive dysfunction than in PD patients with normal cognition (figure 3). The median plasma α-synuclein levels were 0.42 pg/mL (95% CI 0.25 to 0.93) for PD with normal cognition, 1.29 pg/mL (95% CI 0.76 to 1.93) for PD-MCI and 4.09 pg/mL (95% CI 1.99 to 6.19) for PDD, respectively (p<0.0001 by Kruskal-Wallis test). When simultaneously considering the effects of age, gender and disease duration in the multivariate linear regression model, plasma levels of α-synuclein were found to negatively correlate with MMSE scores (R2-adjusted=0.3004, p<0.001, table 3), suggesting that a higher plasma α-synuclein level was associated with a lower cognitive performance in patients with PD.
Figure 3.
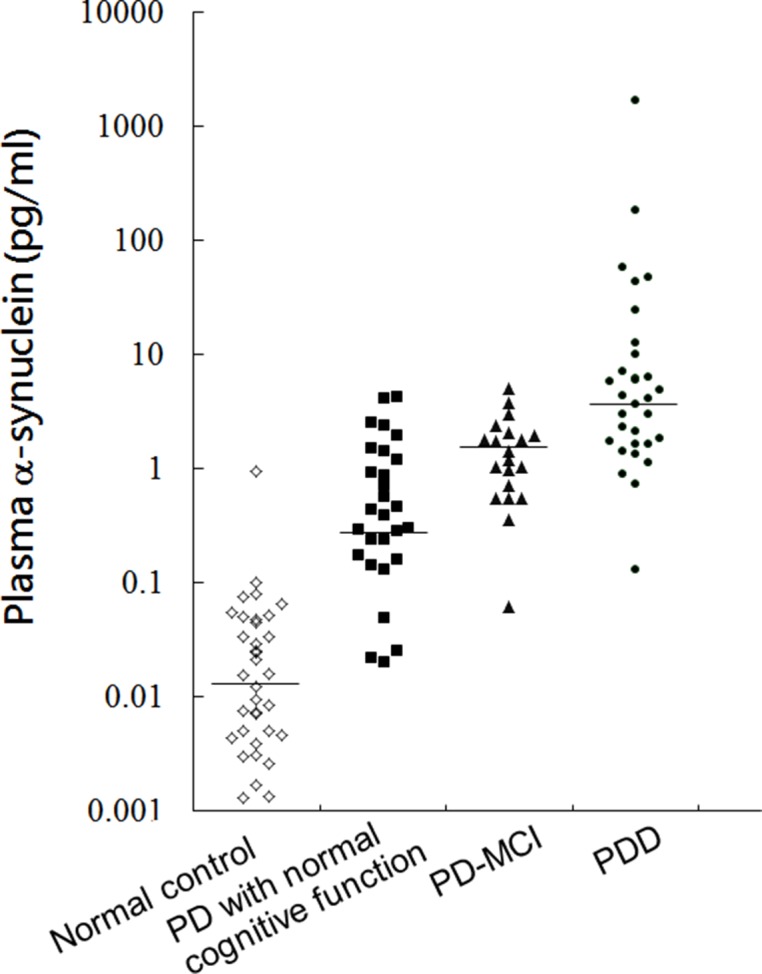
Plasma α-synuclein levels in PD patients with varying cognitive function. The plasma α-synuclein level was significantly higher in PD patients with more severe cognitive dysfunction than in PD patients with normal cognition (p<0.01). PD, Parkinson’s disease; PD-MCI, Parkinson’s disease with mild cognitive impairment; PDD, Parkinson’s disease with dementia.
Table 3.
Multivariate linear regression models for cognitive symptom severity in patients with PD as assessed by MMSE scores
| Independent variables | Coefficient | SE | r | t | p Value |
| Constant | 39.526 | ||||
| Disease duration (years) | 0.0612 | 0.095 | 0.097 | 0.650 | 0.519 |
| Age (years) | −0.223 | 0.056 | −0.512 | −4.003 | <0.001** |
| Gender (male) | 0.208 | 1.422 | 0.022 | 0.147 | 0.884 |
| Plasma α-synuclein level | −0.226 | 0.096 | −0.331 | −2.351 | 0.023* |
In this model, the MMSE score of patients with PD was set as the dependent variable, with age, gender, disease duration and plasma level of α-synuclein set as independent variables. r: correlation coefficient based on the model of multiple linear regression; t: t value for the coefficient of each parameter in the model; p: for r or t; R2-adjusted=0.3004, p<0.001 for the model. *: statistically significant, p<0.05; **: p<0.01.
MMSE, Mini-Mental State Examination; PD, Parkinson’s disease.
Discussion
The results of this study demonstrate several major advances with regard to a plasma α-synuclein assay that exploits ultra-sensitive IMR analyses for patients with PD. Comparing patients with PD with healthy controls revealed PD-associated differences in the plasma levels of α-synuclein. We have, for the first time, demonstrated that plasma levels of α-synuclein are associated with motor dysfunction and cognitive decline in patients with PD. Additional analyses revealed a significant negative correlation between plasma α-synuclein levels and MMSE scores in patients with PD after considering the confounders of age, gender and disease duration. Our observations suggest that plasma α-synuclein could serve as a surrogate biomarker for cognitive decline in PD patients, and our results may assist clinicians in identifying patients at risk of cognitive dysfunction in the future.
α-Synuclein is the pathognomonic protein associated with PD. Mutations or multiplications of the α-synuclein gene (SNCA) are known to be causative in some familial forms of PD,29 and genome-wide association studies have also confirmed that common variants of SNCA modulate the risk of sporadic PD.30 Experimental data have shown that α-synuclein would be released from neurons by exocytosis into body fluids, including the CSF and plasma, which contribute to cell-to-cell transmission of α-synuclein pathology in the brain.31 In this regard, numerous studies have attempted to compare levels of total or oligomeric α-synuclein in CSF samples from patients with PD compared with healthy controls, although results, thus far, have been inconsistent.5 7 However, there is a trend that the level of ‘total α-synuclein’ is, on average, lower in samples of CSF taken from patients with PD than in groups of normal controls.7 A large multicentre Parkinson’s Progression Markers Initiative study showed the decreased CSF α-synuclein level in early-stage, drug-naive PD patients compared with healthy controls.32 With regard to the role of CSF α-synuclein level in PD with cognitive decline, a recent large cohort study who participated in the deprenyl and tocopherol antioxidative therapy of parkinsonism (DATATOP) study, with an 8-year follow-up period, observed that higher CSF levels of total α-synuclein predicted worse cognitive function in patients with PD.33 Similarly, another longitudinally follow-up study observed that higher CSF levels of total α-synuclein were associated with progression of both motor symptoms and cognitive decline in PD over 2 years.34 The mechanisms why the concentrations of plasma α-synuclein showed a biphasic pattern, decreased in early stage of PD compared with controls and then increased as disease severity deteriorated, remain elusive. One possible explanation is that the decreased level of CSF α-synuclein in early-stage PD may be the result of cellular compensatory mechanisms for sequestering pathological soluble α-synuclein and, therefore, resulting in lower level of CSF α-synuclein compared with controls.33 As the disease severity increased with loss of cellular compensatory ability to sequester the toxic species of α-synuclein with forming of Lewy bodies, the CSF levels of α-synuclein increased.33 Since obtaining CSF is an invasive procedure, recent studies have instead focused on assessing plasma α-synuclein levels as a potential surrogate biomarker from the much more accessible, peripheral blood. Few studies have shown an increased level of this protein in plasma samples from patients with PD versus healthy controls.35 36 Consistent with these observations, our results also demonstrate a significantly higher plasma α-synuclein level in patients with PD compared with controls. One recent study that used an intracerebroventricular injection of radiolabelled α-synuclein into mouse brain demonstrated that CSF α-synuclein could be diverted to the blood via exosome efflux.35 Subsequent studies in patients with PD confirmed that the levels of plasma exosomal α-synuclein were substantially higher in PD patients than in control subjects, suggesting an increased efflux of α-synuclein to the peripheral blood in the disease state.35 Although we could not differentiate exosomal and non-exosomal α-synuclein in the plasma by the IMR method used in the current study, the results of increased plasma exosomal α-synuclein in patients with PD compared with controls35 are consistent with our findings. The compensatory increased clearance of excess, potentially toxic α-synuclein species from the PD brain to the peripheral blood through exoxomes release into the extracellular environment may partly contribute to the increased plasma levels of α-synuclein. Although further studies are clearly needed to elucidate the mechanism involved in the transport of α-synuclein from the central nervous system to the peripheral blood, our results suggest that plasma levels of α-synuclein would be a feasible biomarker with which to predict disease progression, as this marker partly reflects the escalation of α-synuclein pathology in the brains of patients with PD.
Our study also observed that plasma α-synuclein levels were associated with motor severity and cognitive dysfunction in patients with PD. The correlations between α-synuclein levels and motor severity (as assessed by UPDRS part III scores) and non-motor severity (as assessed by NMSS scores) were, however, found to be insignificant after confounders (age, gender and disease duration) were taken into account. However, we found that levels of plasma α-synuclein negatively correlated with MMSE scores, even after considering confounder effects. These data suggest that higher levels of plasma α-synuclein are associated with poor cognitive performance in patients with PD. Few studies have examined the relationships between plasma α-synuclein levels and cognitive function in patients with PD. Cortical Lewy body/neuritic pathology is more extensive in PDD than in PD without dementia, which implies that the α-synuclein burden in plasma is more severe in PDD than in PD with normal cognition. Our results support this hypothesis, in that plasma levels of α-synuclein were significantly higher in patients with PDD than in PD-MCI and PD patients with normal cognition. Consistent with our findings, recent technically more advanced analyses show that PDD patients express a greater quantity of the oligomeric forms of α-synuclein than PD patients without dementia.37 Furthermore, a higher CSF total α-synuclein concentration was associated with a faster decline in cognitive performance in de novo patients with PD, with no correlation with motor progression.33 In addition to a recent study showing that a specific genetic haplotype in intron 4 of SNCA is associated with a risk of PDD,38 our results suggest that α-synuclein may serve as a plasma biomarker for cognitive decline in PD. However, as plaques of amyloid-β and tau neurofibrillary tangles, the hallmark pathologies of Alzheimer’s dementia, are also observed, and correlate with cognitive status in patients with PDD,31 future longitudinal follow-up studies concomitantly incorporating assessing α-synuclein, amyloid-β protein, total and phospho-tau in plasma levels of PDD are needed to better understand the pathophysiology of cognitive deterioration in PD.
In our study, a negative, but important observation, is that although plasma α-synuclein levels increase as motor symptoms progress (figure 2), their values did not correlate with UPDRS part III scores after considering confounders (age, gender and disease duration (table 2)). This observation suggests that, in contrast to PD-related cognitive decline, there is not a straightforward relationship between plasma α-synuclein and motor symptoms. Similar findings have been observed in previous cross-sectional investigations that examined patients’ levels of α-synuclein in CSF.39 40 One possible explanation is that the UPDRS part III scores primarily reflect deficits arising from nigrostriatal degeneration, whereas plasma or CSF α-synuclein levels are influenced by whole brain α-synuclein loading. However, the reason why plasma α-synuclein level correlates cognitive decline but not motor symptoms severity remains unclear. Further studies are warranted to decipher the pathophysiology behind motor and cognitive symptoms of PD.
The major advantage of this study is the use of the IMR-based method to detect plasma levels of α-synuclein, as well as enrolling control subjects, and PD patients with varying levels of disease severity. In plasma samples, heterophilic antibodies commonly interfere with immunoassays and are major confounders when assaying low-level target proteins using the traditional ELISA method.41 Previous studies have shown that IMR manifests a low-interference and high-specificity for detecting target proteins comparing with ELISA.13 15 When IMR signals are measured, the magnetic particles oscillate, which establishes centrifugal forces. Should these forces exceed the binding forces that couple an antibody to a non-specific target, selective removal of weakly bound antibody/antigen targets will occur. This selection diminishes the interference effects of both heterophile antibody action, and naturally occurring plasma biomolecules derived from frequently used drugs that can bind to magnetic nanoparticles.13 These characteristics feature IMR a novel and sensitive assay to detect plasma level of α-synuclein. However, our study has some limitations. First, we only assessed cognitive function using MMSE, a simple measurement for global cognitive function. Detailed neuropsychological tests evaluating individual cognitive domains are warranted for further assessing the correlation between plasma α-synuclein level and individual cognitive domain decline in patients with PD. Second, the relatively small number of enrolled subjects and the cross-sectional design of this study may limit the extent to which our data can be extrapolated to all patients with PD. Future, large cohort studies with a long follow-up period are needed to validate our results. Third, the mean age of control subjects was younger than the mean age of patients with PD in the current study. Although we did not find any significant correlation between age and plasma α-synuclein levels in control subjects of varying age (online supplementary figure 1), further studies with age-matched control subjects are needed. Finally, we did not check plasma levels of amyloid-β and tau in this study. As plaques of amyloid-β and tau neurofibrillary tangles are also observed in the postmortem findings of patients with PDD,31 future longitudinal follow-up studies concomitantly incorporating assessing α-synuclein, amyloid-β protein, total and phospho-tau in plasma levels of patients with cognitive decline are warranted to have a better understanding of the pathophysiology of PDD.
In summary, our findings suggest that plasma levels of α-synuclein could serve as a non-invasive biomarker for PD risk and severity. Furthermore, plasma α-synuclein levels, which correlated with cognitive decline in patients with PD, may help clinicians to identify patients at risk of cognitive impairment in the future.
Acknowledgments
We would like to thank all the subjects that participated in this study, and we are grateful to The National Taiwan University Hospital (NTUH 105-002942) for their support of this work.
Footnotes
Contributors: Study concept and design: CHL and MJC.
Acquisition of data: CHL, SYY, HEH, CCY, JJC, HHC and BHL.
Analysis and interpretation of data: CHL, SYY and MJC.
Drafting of the manuscript: CHL.
Critical revision of the manuscript for important intellectual content: CHL, SYY and MJC.
Statistical analysis: CHL.
Obtained funding: CHL and MJC.
Study supervision: MJC.
Funding: The authors are grateful to the National Taiwan University Hospital for their support of this work (NTUH 105-002942).
Competing interests: None declared.
Ethics approval: Institutional Review Board of National Taiwan University Hospital.
Provenance and peer review: Not commissioned; externally peer reviewed.
Correction notice: Since this notice was first published online figure 1 has been updated.
References
- 1. Dorsey ER, Constantinescu R, Thompson JP, et al. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology 2007;68:384–6. 10.1212/01.wnl.0000247740.47667.03 [DOI] [PubMed] [Google Scholar]
- 2. Del Tredici K, Braak H. Review: sporadic Parkinson’s disease: development and distribution of α-synuclein pathology. Neuropathol Appl Neurobiol 2016;42:33–50. 10.1111/nan.12298 [DOI] [PubMed] [Google Scholar]
- 3. Hughes AJ, Daniel SE, Kilford L, et al. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 1992;55:181–4. 10.1136/jnnp.55.3.181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Munhoz RP, Moro A, Silveira-Moriyama L, et al. Non-motor signs in Parkinson’s disease: a review. Arq Neuropsiquiatr 2015;73:454–62. 10.1590/0004-282X20150029 [DOI] [PubMed] [Google Scholar]
- 5. Lin CH, Wu RM. Biomarkers of cognitive decline in Parkinson’s disease. Parkinsonism Relat Disord 2015;21:431–43. 10.1016/j.parkreldis.2015.02.010 [DOI] [PubMed] [Google Scholar]
- 6. El-Agnaf OM, Salem SA, Paleologou KE, et al. Alpha-synuclein implicated in Parkinson’s disease is present in extracellular biological fluids, including human plasma. FASEB J 2003;17:1945–7. 10.1096/fj.03-0098fje [DOI] [PubMed] [Google Scholar]
- 7. Delgado-Alvarado M, Gago B, Navalpotro-Gomez I, et al. Biomarkers for dementia and mild cognitive impairment in Parkinson’s disease. Mov Disord 2016;31:861–81. 10.1002/mds.26662 [DOI] [PubMed] [Google Scholar]
- 8. Compta Y, Pereira JB, Ríos J, et al. Combined dementia-risk biomarkers in Parkinson’s disease: a prospective longitudinal study. Parkinsonism Relat Disord 2013;19:717–24. 10.1016/j.parkreldis.2013.03.009 [DOI] [PubMed] [Google Scholar]
- 9. Siderowf A, Xie SX, Hurtig H, et al. CSF amyloid β 1-42 predicts cognitive decline in Parkinson disease. Neurology 2010;75:1055–61. 10.1212/WNL.0b013e3181f39a78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Liu C, Cholerton B, Shi M, et al. CSF tau and tau/Aβ42 predict cognitive decline in Parkinson's disease. Parkinsonism Relat Disord 2015;21:271–6. 10.1016/j.parkreldis.2014.12.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mattsson N. CSF biomarkers in neurodegenerative diseases. Clin Chem Lab Med 2011;49:345–52. 10.1515/CCLM.2011.082 [DOI] [PubMed] [Google Scholar]
- 12. Atik A, Stewart T, Zhang J. Alpha-synuclein as a biomarker for Parkinson’s disease. Brain Pathol 2016;26:410–8. 10.1111/bpa.12370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yang CC, Yang SY, Chieh JJ, et al. Biofunctionalized magnetic nanoparticles for specifically detecting biomarkers of Alzheimer’s disease in vitro. ACS Chem Neurosci 2011;2:500–5. 10.1021/cn200028j [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chiu MJ, Chen YF, Chen TF, et al. Plasma tau as a window to the brain-negative associations with brain volume and memory function in mild cognitive impairment and early Alzheimer’s disease. Hum Brain Mapp 2014;35:3132–42. 10.1002/hbm.22390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yang SY, Chiu MJ, Lin CH, et al. Development of an ultra-high sensitive immunoassay with plasma biomarker for differentiating Parkinson disease dementia from Parkinson disease using antibody functionalized magnetic nanoparticles. J Nanobiotechnology 2016;14:41 10.1186/s12951-016-0198-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wu RM, Bounds R, Lincoln S, et al. Parkin mutations and early-onset parkinsonism in a Taiwanese cohort. Arch Neurol 2005;62:82–7. 10.1001/archneur.62.1.82 [DOI] [PubMed] [Google Scholar]
- 17. Lin CH, Tan EK, Chen ML, et al. Novel ATP13A2 variant associated with Parkinson disease in Taiwan and Singapore. Neurology 2008;71:1727–32. 10.1212/01.wnl.0000335167.72412.68 [DOI] [PubMed] [Google Scholar]
- 18. Goetz CG, Tilley BC, Shaftman SR, et al. Movement disorder society-sponsored revision of the unified Parkinson’s disease rating scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord 2008;23:2129–70. 10.1002/mds.22340 [DOI] [PubMed] [Google Scholar]
- 19. Hoehn MM, Yahr MD. Parkinsonism: onset, progression and mortality. Neurology 1967;17:427–42. 10.1212/WNL.17.5.427 [DOI] [PubMed] [Google Scholar]
- 20. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–98. [DOI] [PubMed] [Google Scholar]
- 21. Emre M, Aarsland D, Brown R, et al. Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Mov Disord 2007;22:1689–707. 10.1002/mds.21507 [DOI] [PubMed] [Google Scholar]
- 22. Poewe W, Gauthier S, Aarsland D, et al. Diagnosis and management of Parkinson’s disease dementia. Int J Clin Pract 2008;62:1581–7. 10.1111/j.1742-1241.2008.01869.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Berg L. Clinical dementia rating (CDR). Psychopharmacol Bull 1988;24:637–9. [PubMed] [Google Scholar]
- 24. Litvan I, Goldman JG, Tröster AI, et al. Diagnostic criteria for mild cognitive impairment in Parkinson’s disease: Movement disorder society task force guidelines. Mov Disord 2012;27:349–56. 10.1002/mds.24893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hoops S, Nazem S, Siderowf AD, et al. Validity of the MoCA and MMSE in the detection of MCI and dementia in parkinson disease. Neurology 2009;73:1738–45. 10.1212/WNL.0b013e3181c34b47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chaudhuri KR, Martinez-Martin P, Brown RG, et al. The metric properties of a novel non-motor symptoms scale for Parkinson’s disease: results from an international pilot study. Mov Disord 2007;22:1901–11. 10.1002/mds.21596 [DOI] [PubMed] [Google Scholar]
- 27. Visser M, Marinus J, Stiggelbout AM, et al. Assessment of autonomic dysfunction in Parkinson’s disease: the SCOPA-AUT. Mov Disord 2004;19:1306–12. 10.1002/mds.20153 [DOI] [PubMed] [Google Scholar]
- 28. Koehler NK, Stransky E, Meyer M, et al. Alpha-synuclein levels in blood plasma decline with healthy aging. PLoS One 2015;10:e0123444 10.1371/journal.pone.0123444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Polymeropoulos MH, Lavedan C, Leroy E, et al. Mutation in the α-synuclein gene identified in families with Parkinson’s disease. Science 1997;276:2045–7. 10.1126/science.276.5321.2045 [DOI] [PubMed] [Google Scholar]
- 30. Simón-Sánchez J, Schulte C, Bras JM, et al. Genome-wide association study reveals genetic risk underlying Parkinson’s disease. Nat Genet 2009;41:1308–12. 10.1038/ng.487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Irwin DJ, Lee VM, Trojanowski JQ. Parkinson’s disease dementia: convergence of α-synuclein, tau and amyloid-β pathologies. Nat Rev Neurosci 2013;14:626–36. 10.1038/nrn3549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kang JH, Irwin DJ, Chen-Plotkin AS, et al. Association of cerebrospinal fluid β-amyloid 1-42, T-tau, P-tau181, and α-synuclein levels with clinical features of drug-naive patients with early parkinson disease. JAMA Neurol 2013;70:1277–87. 10.1001/jamaneurol.2013.3861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Stewart T, Liu C, Ginghina C, et al. Cerebrospinal fluid α-synuclein predicts cognitive decline in parkinson disease progression in the DATATOP cohort. Am J Pathol 2014;184:966–75. 10.1016/j.ajpath.2013.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hall S, Surova Y, Öhrfelt A, et al. CSF biomarkers and clinical progression of Parkinson disease. Neurology 2015;84:57–63. 10.1212/WNL.0000000000001098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Shi M, Liu C, Cook TJ, et al. Plasma exosomal α-synuclein is likely CNS-derived and increased in Parkinson’s disease. Acta Neuropathol 2014;128:639–50. 10.1007/s00401-014-1314-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lee PH, Lee G, Park HJ, et al. The plasma α-synuclein levels in patients with Parkinson’s disease and multiple system atrophy. J Neural Transm 2006;113:1435–9. 10.1007/s00702-005-0427-9 [DOI] [PubMed] [Google Scholar]
- 37. Hansson O, Hall S, Ohrfelt A, et al. Levels of cerebrospinal fluid α-synuclein oligomers are increased in Parkinson’s disease with dementia and dementia with Lewy bodies compared to Alzheimer’s disease. Alzheimers Res Ther 2014;6:25 10.1186/alzrt255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Guella I, Evans DM, Szu-Tu C, et al. α-synuclein genetic variability: a biomarker for dementia in Parkinson disease. Ann Neurol 2016;79:991–9. 10.1002/ana.24664 [DOI] [PubMed] [Google Scholar]
- 39. Mollenhauer B, Locascio JJ, Schulz-Schaeffer W, et al. α-Synuclein and tau concentrations in cerebrospinal fluid of patients presenting with parkinsonism: a cohort study. Lancet Neurol 2011;10:230–40. 10.1016/S1474-4422(11)70014-X [DOI] [PubMed] [Google Scholar]
- 40. van Dijk KD, Bidinosti M, Weiss A, et al. Reduced α-synuclein levels in cerebrospinal fluid in Parkinson’s disease are unrelated to clinical and imaging measures of disease severity. Eur J Neurol 2014;21:388–94. 10.1111/ene.12176 [DOI] [PubMed] [Google Scholar]
- 41. Ishii R, Tokuda T, Tatebe H, et al. Decrease in plasma levels of α-synuclein is evident in patients with Parkinson’s disease after elimination of heterophilic antibody interference. PLoS One 2015;10:e0123162 10.1371/journal.pone.0123162 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jnnp-2016-314857supp001.jpg (45.9KB, jpg)


