Abstract
The adoption and implementation of evidence-based interventions (EBIs) are end goals of translational research, however, potential end-users’ perceptions of an EBI’s value have contributed to low rates of adoption. In this article, we describe our application of emerging dissemination and implementation science theoretical perspectives, community engagement, and systems science principles to develop a novel EBI dissemination approach. Using consumer-driven, graphics-rich simulation, the approach demonstrates predicted implementation effects on health and employment outcomes for socioeconomically disadvantaged women at the local level, and is designed to increase adoption interest of county program managers accountable for improving these outcomes in their communities.
Introduction
“Evidence, like beauty, may be in the eye of the beholder.”
- Kerner (2006)
Despite significant progress in developing effective evidence-based interventions (EBIs), low adoption and implementation rates in practice settings have precluded most from having a positive effect on the public’s health.1,2 This ‘high supply, low demand’ pattern with respect to EBI implementation has been consistently observed across a range of disease states, health-related disciplines, and practice settings.3,4 In 2006, the National Institutes of Health (NIH) responded to this pattern by committing over $3.2 billion to increase fiscal and intellectual investments in translational research through the initiation of the Clinical and Translational Research Award (CTSA) Program.5,6 Translational research is concerned with knowledge translation (KT), with efforts typically reflecting three pathways through which knowledge must be translated to be useful at the next stage. These include translating basic science findings to humans (T1), translating initial findings in humans to patients and/or populations in clinical practice settings (T2), and, finally, translating interventions found effective in the T2 studies into routine care provided in clinical and community settings (T3).7 As indicated by the fact that there are at least 31 scientific journals currently dedicated to translational research, the CTSA investment has stimulated a great deal of scientific productivity in the field.
In the remainder of this article, we first describe an EBI that improves health and employment outcomes for socioeconomically disadvantaged women participating in a Welfare Transition Program (WTP). The EBI was both developed and tested by a nurse scientist, and is currently being disseminated through the Agency for Healthcare Quality and Research (AHRQ) Innovations Exchange website8 (see Figure 1). We then describe existing and emerging theoretical perspectives in dissemination and implementation (D&I) research that have informed a pilot study underway that will test a novel, consumer-driven, graphics-rich simulation of the effects of EBI implementation at the local level as a dissemination approach. Finally, we argue that, given the practice-embedded nature of nursing as a discipline, nurse scientists are poised to make important contributions to advancing the field D&I research.
Figure 1.
Screen shot of EBI Dissemination format via the Agency for Healthcare Quality & Research Innovations Exchange (at: https://innovations.ahrq.gov/profiles/public-health-nurses-provide-case-management-low-income-women-chronic-conditions-leading).
An EBI to Improve Health & Employment Outcomes for Disadvantaged Women
Comprised of >90% women, health problems present greater obstacles to employment for women in Welfare Transition Programs (WTPs) than does low education, lack of work experience, or having very young children.9 Within this group, 27% to 53% screen positive for depression10-13; 25% report fair or poor health; and 60% report a health-related functional limitation has interfered with their ability to work.14 Despite numerous study findings documenting the health-related barriers to employment among women in WTPs, there had been an absence of EBIs to address the health-related needs of this group until 2010. From 2005-2010, using a community-based participatory research (CBPR) approach the primary author collaborated with women enrolled in a WTP, WTP administrators, public health nurse representatives, and other stakeholders to develop an intervention that placed public health nurses on site at the WTP to conduct comprehensive health screening, referral for needed health-related services, and case management for women in WTPs with one or more chronic health conditions (defined broadly).12 The intervention was tested against an attenuated wait-control condition using a randomized controlled trial (RCT) design with 432 women. In 2011, the findings demonstrated reduced depressive symptoms, improved health-related functioning, and improved employment-entry (by 35 days) for women in WTP programs. Details of the EBI development and study findings are available elsewhere.12,15-18
Within six months of publishing the study findings, the intervention was selected for inclusion on the Agency for Healthcare Research and Quality (AHRQ) Innovations Exchange website (henceforth referred to as the Exchange). The purpose of the Exchange is to “speed the implementation of new and better ways of delivering health care.”19 The site allows health professionals to search for EBI innovations; provides practical tools to help them assess, promote, and improve the quality of care delivered; directly connects potential adopters to the EBI innovator; and provides resources for providers to learn more about effective adoption and implementation strategies. A standardized information delivery format is applied to describe each innovation on the Exchange, with an emphasis on section brevity, the use of lay language, and walking potential adopters step-by-step through understanding both the resources needed for adoption and key factors that facilitate implementation (see Table 1).
Table 1.
Standardized Format of the Agency for Healthcare Research and Quality (AHRQ) Innovations Exchange Innovation Description Content.
| Innovation Snapshot |
| Summary |
| Evidence Rating |
| Date First Implemented |
| Problem Addressed |
| What They Did |
| Description of the Innovative Activity |
| Context of the Innovation |
| Did it Work? |
| Results |
| Evidence Rating |
| How They Did It |
| Planning and Development Process |
| Resources Used and Skills Needed |
| Funding Sources |
| Tools and Resources |
| Adoption Considerations |
| Sustaining This Innovation |
| More Information |
| Contact the Innovator |
| Innovator Disclosures |
| References/Related Articles |
| Footnotes |
| Back Story |
| Client/Patient Example |
With the EBI originally published on the Exchange in February 2012, there was little evidence over the course of the following two years to suggest disseminating it’s findings through this mechanism had led or would lead to increased adoption. The PI/Innovator had not been contacted by a single potential adopter over that period of time. As website traffic statistics are not provided to innovators who feature their EBI’s on the Exchange, it is difficult to interpret what was responsible for the lack of inquiry. Given the nature of the primary outcomes (both health and employment), and the setting in which the EBI is intended to be applied (WTP offices, rather than health care clinics), a reasonable explanation was that there was a misalignment of motivations between the audience to whom the Exchange was marketing, and the audience that would likely benefit most from EBI implementation. That is, health care professionals in traditional direct-care delivery settings have had few incentives to address the chronic health condition management needs of disadvantaged women outside those settings. Meanwhile, descriptive statistics of Exchange users, by role, suggest WTP managers may be unlikely users of this dissemination platform: less than 1% of users over a 1-year period were from the social service sector.19 Although nurses and nurse practitioners comprise the largest Exchange utilizer group (at 36%), there is no differentiation of utilization by nurse licensure type or setting, limiting the conclusions that can be drawn about the extent to which public health nurses utilize the Exchange to find EBIs for their practice setting.19
Recognizing this misalignment required a new approach for disseminating the EBI if it were ever going to have a meaningful impact for the population of disadvantaged women it was intended to serve. With a strong base of D&I research expertise and mentoring available through The University of North Carolina at Chapel Hill’s CTSA program (i.e., The North Carolina Translational and Clinical Sciences (NC TraCS) Institute), we reframed this EBI dissemination dilemma as an opportunity to generate a new approach. Specifically, we were looking to develop this approach by synthesizing emerging theoretical perspectives in D&I research and systems science with the working knowledge the first author had of the WTP population’s health needs, the WTP policy-driven goals to facilitate employment, and the receptivity of public health nursing leadership in North Carolina to innovative ideas and collaboration. A brief overview of D&I science, and a description of how we synthesized emerging theory and methods to design the new approach, follow.
Dissemination and Implementation (D&I) Science
Considered one form of translational research, dissemination and implementation (D&I) science focuses on the T3 pathway, where moving EBI’s into the health care services routinely delivered in acute care, outpatient or primary care, and/or public health practice is the end goal. Although the frequently used term dissemination and implementation science might leave the impression that the “dissemination” and “implementation” aspects of translational research are indistinguishable, the foci of each are rather distinct. In general, dissemination research focuses on understanding how to effectively package and transmit information about an EBI to a targeted audience.20 Outcomes of effective dissemination include increasing awareness of, interest in, and potential adoption of an EBI. Implementation research, on the other hand, focuses on understanding how to most effectively facilitate adopting and implementing the EBI in practice settings.20 Outcomes of effective implementation include changed practice patterns that reflect the full integration of the EBI into the given setting, and, ultimately, observing improvements in the health of the patients and/or population served at the local level.
Knowledge Translation – in Context
Much of the earlier work in D&I science focused on the largely passive dissemination of health-related research findings21,22 with the expectation that print and mass media dissemination alone would lead to the adoption and implementation of new EBI’s into practice settings. In part, this assumption was rooted in the notion that the ethos of health professionals to care for the individuals or populations for whom they were responsible would drive EBI uptake.23 As such, there has been a great deal of effort focused on compiling and synthesizing the vast quantity of new research findings and then widely disseminating the resulting guidelines and recommendations. Findings from a decade of knowledge translation research, however, have shown that passive dissemination strategies are highly ineffective for eliciting the adoption and implementation of EBI’s into practice settings.24 Practitioners report they have difficulty interpreting information about EBIs and have concerns that EBIs are not relevant or feasible within their practice context. Moreover, the proliferation of research dissemination sites and products has exacerbated the “signal-to-noise” ratio problem21 that occurs for practitioners when confronted with information overload.25
Although there are several other reasons that passive dissemination strategies are believed to have failed in increasing EBI implementation in practice, a major consideration that has been “lost in translation” is the degree to which context counts.22 Information about an EBI needs to be customized to feature the specific advantages it offers based on the context in which it is to be implemented.26 Customizing an EBI’s advantages and feasibility to a specific audience, within a specific context, is not always an easy task – particularly when EBI implementation and impact varies across different contexts. This is particularly true when EBIs are multicomponent and designed to be implemented within complex systems, in which a web of interconnected factors shape system outcomes, delays between cause and effect make it hard to accurately intuit what is working, and the effects of components of interventions might not be linear or additive when combined.27 In this circumstance, the impact of EBIs will likely vary in the configuration of resources required to implement and the populations affected.28 Systems science methods offer new opportunities for customizing information about an EBI’s potential benefits and cost to fit a specific context. Systems science-based models, for example, can be used to simulate how an intervention will perform differently across different contexts29 – such as those depicting infectious disease spread30,31 and traffic flow patterns,32,33 among others.
Marketing & Community Engagement Perspectives
From the business literature, several have argued that marketing EBIs as products using a commercial business-oriented, customer-centered distribution perspective is a promising dissemination strategy in the health care sector.1,34,35 From this perspective, the ultimate goal of commercial marketing is to positively influence consumers’ decisions to purchase a product.36,37 When applied to serve the purpose of dissemination, an EBI represents the product, and a purchase is reconceived as EBI adoption. Recent findings suggest applying customer-driven marketing principles to disseminate EBIs is effective in both reaching target end-users24,38-40 and increasing their EBI adoption intentions.36
To apply consumer-driven marketing, however, one must “know thy consumer” (i.e., the potential adopter).35 Fundamentally, this means having a comprehensive understanding of what drives the potential adopter – that is, what shapes the potential adopter group’s perceptions of reality? What are the potential adopter’s individual self-interests and motivations, as well as the interests, motivations, and mission of his or her agency? In the EBI dissemination example discussed here, this required having a clear understanding of the Temporary Assistance for Needy Families (TANF) policy that mandates moving individuals from welfare receipt into employment.41 Under TANF mandates, if agencies responsible for WTP delivery in each county (typically Department of Social Services agencies) do not meet specific welfare-to-employment benchmarks, there are significant funding reduction repercussions at both the state and county level.41 Thus, the motivation to meet ‘welfare-to-employment’ benchmarks becomes a central feature of the organizational environment within which WTPs are delivered, with management and staff efforts focused on this goal. It was also critical for us to recognize the extent to which TANF policy constructs how WTP managers and staff interpret ‘reality’ in terms of the problems relevant to, and the needs of, the WTP population in moving into employment – and how to solve them.42 For example, TANF policy encourages local WTPs to screen for domestic violence, mental health conditions, and drug abuse as ‘known’ barriers to employment, but is silent with regard to the growing body of findings indicating physical health conditions also act as equally, if not more, significant barriers to employment.9,14,43-48 A perhaps unintended consequence of this omission is a narrowly-constructed, partial reality for WTP administrators and staff that domestic violence, mental health conditions, and drug abuse are the sole health concerns limiting employment in the WTP population.
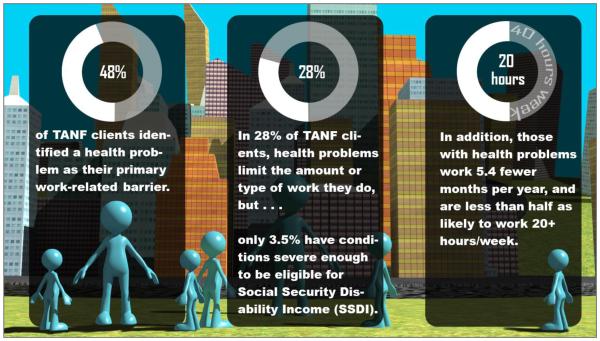
A more narrowly-defined reality of the intersections between health and employment for the WTP population described above has implications for the knowledge and persuasion phases of the EBI adoption example presented here. In designing the novel dissemination approach, we took a social constructivist perspective of potential adopters’ knowledge proposed by Thomas and colleagues, where knowledge of the need for, and other aspects of, EBI adoption “can be regarded as an active learning process … a fluid set of understandings shaped by those who produce [evidence] and those who use it.”42(p.2) As such, recognizing WTP managers may have a limited, or partial, understanding of the full range of health conditions that can impede employment, we incorporate a “tutorial” of findings that outline the prevalence of different health conditions in the WTP population and the magnitude of impact they are estimated to have on employability. The prevalence of select conditions, and the effect they have on impeding employment for this group, will be simulated to reflect each county-level WTP population. For our potential adopters, this information provides critical foreknowledge of the problem that may not have been previously understood, yet must be understood for a description of the EBI and its implementation effects to have any persuasive influence on potential EBI adopters.
Finally, although emerging from two entirely different fields (public health and business, respectively), community-engaged research and consumer-driven marketing share key attributes that are relevant to D&I research.35 One such attribute is incorporating collaborative processes to ensure the end products (be it an EBI dissemination approach, an item designed for sale in the commercial market, or a study design) are relevant to the end-user. While we had a strong working knowledge of many core motivational factors that would drive interest in EBI adoption from the first author’s prior community-engaged research, we have included representatives of our potential adopter group as members of the research team to inform the dissemination approach and pilot study design.
Our community partners have emphasized that an effective dissemination approach must make the effects of adopting an EBI readily observable in the populations that potential adopters are directly responsible for, and present these effects in a format that facilitates understanding of the need for, and favorable appraisal of, the EBI. Details of the novel dissemination approach they have advised the team on include aesthetics (animation graphics, background music), messaging content, and length. The public health nurse and WTP manager community partners on the research team (the third and seventh author, respectively) also assume the role of dissemination/pilot study liaisons to our study sample of potential adopters across North Carolina. Having networked with managers from many other counties across the state, they lend a level of practice-oriented credibility to both the dissemination approach and the pilot study that the academic members on the team would not be able to achieve alone. As they enact these critical roles, our community partners on the team will encourage potential adopters to complete the pilot study survey to which they have been randomly assigned; and will provide written endorsements of the importance to consider the EBI and of their personal experiences in implementing a version of it through faculty-led student clinical practicum courses.
Diffusion of Innovation Theory
Considered one of the more familiar theories for dissemination research, the Diffusion of Innovation (DOI) theory provides an explanatory framework of the antecedents to, and processes of, innovation adoption. These include characteristics of the potential adopter and the social context of the organization, and the potential adopter’s perceptions of the innovation’s attributes (relative advantage, complexity, compatibility, observability, and trialability). It also provides a stage-ordered framework to understand phases of the adoption and implementation process.49 Given the dissemination-focused purpose of our approach, where the outcome is to increase EBI adoption interest, we focus on the knowledge and persuasion phases of the DOI theory, which have been found to predict adoption interest and decisions to adopt.49
In considering the characteristics of the most likely potential adopters, the first author’s many years of experience conducting participatory research with public health organizations and the WTP program suggested that public health nurse and WTP managers should fill the potential adopter role. During both the RCT conducted originally to test the EBI case study described here, and in implementing the EBI on a smaller scale with students during their public health nursing clinical experience, the WTP staff and public health nurse managers successfully negotiated study implementation across both upper level administration and front-line staff. This inclination ran counter to the potential adopter groups identified in the vast majority of health-related dissemination research, where individuals in positions of the highest authority (e.g., those in executive, top managerial, or physician roles) have generally been presumed to most readily adopt, and most effectively implement EBIs. This presumption has recently been challenged by Birken and colleagues,50,51 however, who point out there is little evidence to suggest those in positions of highest authority are the most likely to facilitate EBI adoption or implementation. Rather, they argue that middle managers are more likely to understand both the value and implementation implications of adopting innovative EBIs in healthcare contexts. This was consistent with our prior experience, where we observed public health nurse and WTP managers firmly having their feet in two different worlds within their respective agencies: both being accountable to meeting higher-level, organizational objectives, and responsible for orchestrating the everyday service delivery carried out by front-line personnel. As such, middle managers are in ideal positions to (1) readily assess the potential value of adopting and implementing an EBI relative to the organization’s objectives, and (2) convince those with decision-making authority within the agency to adopt an EBI based on this value. In the D&I research arena, middle managers are frequently overlooked; yet, as recent evidence suggests, and as we anticipate in selecting this group as our target potential adopters, they can be key “brokers” of the dissemination and implementation (i.e., the T3 translational science) process.52
Systems Science Methods
Complexity is a hallmark of the systems used to deliver individual health services, social services, and public health services in the U.S.29 Complexity can be readily observed when services are delivered within each of these systems; however, in the post-Affordable Care Act (ACA) era, where service coordination across systems to address social determinants of health is becoming an embedded part of the delivery landscape, complexity abounds. While there has been a productive stream of healthcare systems research conducted by nurse scientists and others over the past few decades,53-55 that line of inquiry differs in important respects from what is now emerging as a new area of “systems science” research.56 Notably, while healthcare systems research to date has made important contributions to our understanding of associations among the many, complex factors that can affect health outcomes (using both cross-sectional and longitudinal data), the analytic methods applied to these studies have not fully empirically captured the iterative, or dynamic, nature of the interactions that occur in complex, dynamic systems. With new graphics-based software such as MatLab, AnyLogic, NetLogo, and others, systems science methods are not only able to estimate the many interactions that occur over time, but are able to convey the effects of change using micro time-sequenced animation to visually demonstrate the effect of these dynamics to support learning about how the system functions, and the effect of alternate strategies for improving it. As noted previously, simulations developed from a systems science perspective have been successfully applied in other contexts to influence decision-making at the organizational and policy levels.30-32,57 Systems science methods are also beginning to inform the methods and analytics applied in D&I research, as well58 -- for example, to understand the network influences on dissemination practices among tobacco control networks,59 and to understand the brokering role of cardiovascular foundations and interorganizational relationships in disseminating EBIs in communities.60
A Novel, Consumer-Driven, Graphics-Rich Simulation Approach to Dissemination
Drawing from the existing and emergent theory and methods in the D&I research arena described above, we are pilot testing the effect of a novel dissemination approach on increasing EBI adoption interest compared to the existing AHRQ Innovations Exchange EBI dissemination format in a sample of potential adopters. In the new approach, we integrate marketing science with computer simulation principles and modeling technologies from the systems science arena that have successfully conveyed complex information, facilitated understanding, and improved decision-making in other contexts. Our target potential adopters – public health nurse and WTP managers at the county level – comprise the pilot study population.
The dissemination approach features simulations to increase potential adopter’s knowledge of the prevalence, and impact of health conditions on the ability to work within the TANF population. A first (preliminary) rendering, or draft, of this graphics component is presented in Figure 2. A subsequent part of the simulation will be customized to reflect the expected health and employment transitions of WTP populations over a 3-year period under two conditions within each manager’s county: with and without EBI implementation. The simulations will reflect the WTP county caseload dynamics in the 50 North Carolina counties that were randomly selected for inclusion in the pilot study, and are representative of both rural and urban areas. The model is parameterized to project the health status and employment outcomes for county-level WTP caseloads into the future using the rates and intervention effect data derived from the EBI RCT.12,15 To generate these projections, we have created synthetic populations matching the real, county-level WTP population by the distributions of select demographics (race, age, education level, prior TANF receipt) and environmental factors (local unemployment rates, rural/urban county designation, primary care access for vulnerable populations). Parameters will be estimated using hierarchical linear models to describe the differences in the expected health and employment outcomes that would be expected between synthetic populations with and without EBI implementation. Currently, our team is in the process of making iterative revisions to the graphics and messaging content in consultation with the community partners who represent the potential adopter group.
Figure 2.
First Rendering of Simulation Storyboard with Example Content to Increase Potential Adopter Knowledge.
The novel, simulation-supported dissemination approach will be tested against the existing AHRQ Innovations Exchange format using a two-group counterbalanced, mixed (within- and between-group) experimental design. Each dissemination approach will be embedded within a survey using Qualtrics software for our potential adopter sample to view, with the order of presentation randomly assigned. We will assess sociodemographic characteristics, innovative work behavior attributes, evidence-based practice knowledge, and WTP population health knowledge at baseline. WTP population health knowledge, EBI attribute appraisal, and adoption interest (our primary outcome of interest) will be assessed following the potential adopters’ review of each dissemination approach. The simulation is theoretically- and empirically-driven to make the effect of the EBI more visually tangible for, and more ‘locally’ relevant to, potential adopters.
Advancing D&I Research Through and For the Nursing Discipline
The theory, methods, and perspectives that we have applied in designing this novel dissemination approach are likely to have intuitive appeal to many nurse scientists, and be familiar to others who have applied nuanced or related versions of them in different research contexts. Increasing the involvement of nurse scientists in conducting D&I research should have two-way, or bidirectional, benefits – both by advancing the field of D&I science through innovation and discovery, and by offering a return on investment (ROI) to more effectively promote the adoption and implementation of the many existing EBI’s that can directly inform nursing practice and benefit the health of the populations we serve.
Applying marketing principles, for example, should come easily for many nurse scientists for several reasons. First, given nursing is a practice discipline, a working knowledge of organizational mission, and potential adopters’ self-interests and motivations often comes from nurse investigators maintaining a presence in practice settings for research, teaching, and/or clinical practice purposes. Second, many nurse scientists routinely engage members of their target populations in the formative research phase when designing interventions – either through community-based participatory research (CBPR) or other participatory processes.61 In essence, EBI-focused dissemination research is intervention research by another name – whereby dissemination is an intervention (i.e., containing both content and processes for delivery), as it is intended to alter an outcome. What does differ between what nurse researchers have tended to focus on in terms of intervention research relative to dissemination research is the outcomes of interest (i.e., outcomes focused on health-related phenomenon versus EBI adoption-related phenomenon).
Engaging potential adopters when conducting dissemination research relies on lines of inquiry that are similar to those used to understand the target population when designing an intervention intended to change health outcomes.37 This might include, for example, incorporating advisory committee input or incorporating findings from qualitative studies conducted using focus groups, into the intervention or study design, among other aspects of the study. For nurse scientists who have developed interventions using CBPR, it is likely that some of the marketing principles that facilitate D&I are already “built in” – such as already having made the intervention relevant to multiple end-user groups (i.e., target populations, potential adopters, and other key stakeholders), and practical or feasible in terms of implementation. Burgio62 has argued one extreme of this benefit, stating “interventions found to be effective through CBPR render the term translation meaningless … One does not need to translate an intervention for community use when all aspects of the intervention’s design were developed in the community.”(p.61) While we agree using a CBPR framework for developing interventions has distinct advantages for knowledge translation efforts, and likely portends a less difficult journey through the T3 translational pathway, there are a unique set of challenges related to dissemination that cannot be preemptively addressed during EBI development and testing. These include several of the factors described in our case example that can be addressed through the use of marketing and community engagement principles, such as how to design the dissemination approach in a way that conveys the EBI’s key findings in a format that is customized to potential adopters so that it is highly relevant, aesthetically pleasing, and secures their attention in a way that makes them curious to learn more. Nurse scientists already using participatory methods can extend their work into the D&I research arena without requiring a seismic shift in focus, and can contribute their expertise in the use of participatory methods to advance the field. Likewise, as systems science methods become increasingly familiar to nurse scientists,61,63 they can be readily applied to advance D&I research.
Finally, the nursing discipline itself has a great deal to gain by having more nurse scientists involved in conducting D&I research. There is a long and fruitful history of nurse investigators developing interventions that have demonstrated efficacy in improving health, reducing healthcare costs, and generating other desirable outcomes across a wide array of populations. Some examples include interventions to reduce HIV risk behaviors among racial and ethnic minority adolescents64; and to improve parenting skills across culturally and ethnically diverse populations,65,66 disease self-management skills among adolescents and teens with Type I diabetes mellitus,67 and coping and psychosocial health responses of parents of hospitalized/critically ill children or premature infants.68 Each of these exemplar EBI’s have demonstrated outcomes using rigorous study designs; hence, they represent EBIs with high evidence ratings for implementation in practice settings and could greatly improve healthcare and population health if implemented on a large scale nationwide. Similar to the case study EBI presented in this article, however, these nurse scientist-developed and -tested EBI’s are currently disseminated via designated internet sites – with one featured on the Centers for Disease Control and Prevention (CDC) High Impact Prevention website,69 another featured on the AHRQ Innovations Exchange website,70 and the others on individually-maintained websites. Although it is difficult to ascertain the extent to which these exemplar EBIs have been adopted based on the limited amount of information available on the dissemination websites, as noted previously, dissemination formats that are predominantly comprised of making EBI information available reflect passive dissemination strategies, which have not generally been effective in facilitating the adoption or implementation of EBIs.21,22
If we, as a community of nurse scientists, are relying primarily on passive dissemination strategies to move EBIs into practice, it could reasonably be argued that this reliance may have negative consequences for the nursing discipline and society as a whole moving forward. That is, as less effective dissemination strategies hamper moving EBIs into practice, nurses in practice settings are less able to provide the most effective care available, where clearly, the patients and populations we serve suffer as a result. From a nursing education perspective, our task of teaching the next generation of nurses the importance of using EBIs is made far more difficult when students repeatedly encounter clinical practice settings where EBIs are not routinely implemented. Finally, from a science ‘landscape’ view, it is not sufficient to demonstrate the impact of nurse scientist-developed interventions solely in terms of their clinical, statistical, or potential cost-savings significance. As NIH and other national research agencies are dependent on Congressional action to fund a productive research enterprise into the future, they are increasingly pressed to demonstrate how past investments in research have resulted in health improvements at the population level, and have generated a return on investment in terms of cost-savings to the nation. Realizing the promise of translational research for transforming clinical practice remains within our reach, and nurse scientists have much not only to give, but also to gain, by advancing the science to inform more effective dissemination and implementation.
Acknowledgments
“The project described was supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number 1UL1TR001111. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.”
References
- 1.Kreuter MW, Bernhardt JM. Reframing the dissemination challenge: a marketing and distribution perspective. Am. J. Public Health. 2009;99(12):2123–2127. doi: 10.2105/AJPH.2008.155218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lenfant C. Shattuck lecture--clinical research to clinical practice--lost in translation? N. Engl. J. Med. 2003;349(9):868–874. doi: 10.1056/NEJMsa035507. [DOI] [PubMed] [Google Scholar]
- 3.Hannon PA, Maxwell AE, Escoffery C, et al. Colorectal Cancer Control Program grantees' use of evidence-based interventions. Am J Prev Med. 2013;45(5):644–648. doi: 10.1016/j.amepre.2013.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stevens KR, Staley JM. The Quality Chasm reports, evidence-based practice, and nursing's response to improve healthcare. Nurs Outlook. 2006;54(2):94–101. doi: 10.1016/j.outlook.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 5.Institute of Medicine . The CTS Program at NIH: Opportunities for advancing clinical and translational research. Washington, DC: 2013. [PubMed] [Google Scholar]
- 6.U.S. Department of Health and Human Services . National Center for Research Resources (NCRR) FY 2011 Budget. National Institutes of Health; Bethesda, MD: 2011. p. 33. [Google Scholar]
- 7.Institute of Medicine . The CTSA Program at NIH: Opportunities for advancing clinical and translational research. Washington, DC: 2013. [PubMed] [Google Scholar]
- 8.Agency for Healthcare Research & Quality (AHRQ) Public Health Nurses Provide Case Management to Low-Income Women with Chronic Conditions, Leading to Improved Mental Health and Functional Status. 2015 https://innovations.ahrq.gov/profiles/public-health-nurses-provide-case-management-low-income-women-chronic-conditions-leading-more. Accessed January 10, 2015.
- 9.Zedlewski S. Work-Related Activities and Limitations of Current Welfare Recipients. The Urban Institute; Washington, DC: 1999. [Google Scholar]
- 10.Polit DF, London AS, Martinez JM. The Health of Poor Urban Women: Findings from the Project on Devolution and Urban Change. Manpower Demonstration Research Corporation; 2001. [Google Scholar]
- 11.Coiro MJ. Depressive symptoms among women receiving welfare. Women Health. 2001;32:1–23. doi: 10.1300/J013v32n01_01. [DOI] [PubMed] [Google Scholar]
- 12.Kneipp SM, Kairalla J, Lutz BJ, et al. Effectiveness of Public Health Nursing Case-Management on the Health of Women Receiving Temporary Assistance for Needy Families: Findings from a Randomized Controlled Trial using Community Based Participatory Research. Am. J. Public Health. 2011;101(9):1759–1768. doi: 10.2105/AJPH.2011.300210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kalil A, Born CE, Kunz J, Caudill PJ. Life stressors, social support, and depressive symptoms among first-time welfare recipients. Am. J. Community Psychol. 2001;29:355–369. doi: 10.1023/A:1010351302196. [DOI] [PubMed] [Google Scholar]
- 14.Loprest P, Maag E. Disabilities Among TANF Recipients: Evidence from the NHIS. The Urban Institute; Washington, D. C.: 2009. [Google Scholar]
- 15.Kneipp SM, Kairalla JA, Sheely AL. A randomized controlled trial to improve health among women receiving welfare in the U.S.: The relationship between employment outcomes and the economic recession. Soc. Sci. Med. 2013;80:130–140. doi: 10.1016/j.socscimed.2012.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kneipp SM, Lutz BJ, Cook C, Levonian C, Hamilton J, Roberson D. Women’s experiences as participants in a community-based participatory research randomized controlled trial. Qual. Health Res. 2013;23(6):847–860. doi: 10.1177/1049732313483924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kneipp SM, Lutz BJ, Means D. Reasons for enrollment, the informed consent process, and trust among low-income women participating in a community-based participatory research study. Public Health Nurs. 2009;26:362–369. doi: 10.1111/j.1525-1446.2009.00791.x. [DOI] [PubMed] [Google Scholar]
- 18.Lutz BJ, Kneipp S, Means D. Developing a health screening questionnaire for women in welfare transition programs in the United States. Qual. Health Res. 2009;19:105–115. doi: 10.1177/1049732308327347. [DOI] [PubMed] [Google Scholar]
- 19.Agency for Healthcare Research & Quality (AHRQ) About the AHRQ Health Care Innovations Exchange. 2015 https://innovations.ahrq.gov/about-us. Accessed January 10, 2015.
- 20.U.S. Department of Health and Human Services . National Institutes of Health; Bethesda, MD: 2009. Dissemination and Implementation Research in Health (R01) [Google Scholar]
- 21.Kerner J, Rimer B, Emmons K. Introduction to the special section on dissemination: dissemination research and research dissemination: how can we close the gap? Health Psychol. 2005;24(5):443–446. doi: 10.1037/0278-6133.24.5.443. [DOI] [PubMed] [Google Scholar]
- 22.Kerner JF. Knowledge translation versus knowledge integration: a "funder's" perspective. J. Contin. Educ. Health Prof. 2006;26(1):72–80. doi: 10.1002/chp.53. [DOI] [PubMed] [Google Scholar]
- 23.Best A, Hiatt RA, Norman CD. Knowledge integration: conceptualizing communications in cancer control systems. Patient Educ Couns. 2008;71(3):319–327. doi: 10.1016/j.pec.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 24.Harris JR, Cheadle A, Hannon PA, et al. A framework for disseminating evidence-based health promotion practices. Prev Chronic Dis. 2012;9:E22. [PMC free article] [PubMed] [Google Scholar]
- 25.Leeman J, Teal R, Jernigan J, Reed JH, Farris R, Ammerman A. What evidence and support do state-level public health practitioners need to address obesity prevention. Am J Health Promot. 2014;28(3):189–196. doi: 10.4278/ajhp.120518-QUAL-266. [DOI] [PubMed] [Google Scholar]
- 26.Dearing JW, Maibach EW, Buller DB. A convergent diffusion and social marketing approach for disseminating proven approaches to physical activity promotion. Am J Prev Med. 2006;31(4 Suppl):S11–23. doi: 10.1016/j.amepre.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 27.Sussman S, Levy D, Lich KH, et al. Comparing effects of tobacco use prevention modalities: need for complex system models. Tobacco induced diseases. 2013;11(1):2. doi: 10.1186/1617-9625-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lich KH, Ginexi EM, Osgood ND, Mabry PL. A call to address complexity in prevention science research. Prevention science : the official journal of the Society for Prevention Research. 2013;14(3):279–289. doi: 10.1007/s11121-012-0285-2. [DOI] [PubMed] [Google Scholar]
- 29.Luke DA, Stamatakis KA. Systems science methods in public health: dynamics, networks, and agents. Annu. Rev. Public Health. 2012;33:357–376. doi: 10.1146/annurev-publhealth-031210-101222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee BY, Wong KF, Bartsch SM, et al. The Regional Healthcare Ecosystem Analyst (RHEA): a simulation modeling tool to assist infectious disease control in a health system. J. Am. Med. Inform. Assoc. 2013;20:e139–146. doi: 10.1136/amiajnl-2012-001107. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shang Y. Modeling epidemic spread with awareness and heterogeneous transmission rates in networks. J Biol Phys. 2013;39(3):489–500. doi: 10.1007/s10867-013-9318-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arasan VT, Vedagiri P. Simulating heterogeneous traffic flow on roads with and without bus lanes. Journal of Infrastructure Systems. 2009;15(4):305–312. [Google Scholar]
- 33.Hu M, Jiang R, Wang R, Wu Q. Urban traffic simulated from the dual representation: Flow, crisis and congestion. Physics Letters A. 2009;373:2007–2011. [Google Scholar]
- 34.Bernhardt JM, Mays D, Kreuter MW. Dissemination 2.0: closing the gap between knowledge and practice with new media and marketing. J Health Commun. 2011;16(Suppl 1):32–44. doi: 10.1080/10810730.2011.593608. [DOI] [PubMed] [Google Scholar]
- 35.Maibach EW, Van Duyn MA, Bloodgood B. A marketing perspective on disseminating evidence-based approaches to disease prevention and health promotion. Prev Chronic Dis. 2006;3(3):A97. [PMC free article] [PubMed] [Google Scholar]
- 36.Luck J, Hagigi F, Parker LE, Yano EM, Rubenstein LV, Kirchner JE. A social marketing approach to implementing evidence-based practice in VHA QUERI: the TIDES depression collaborative care model. Implementation science : IS. 2009;4:64. doi: 10.1186/1748-5908-4-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Andreasen AR. Social Marketing in the 21st Century. SAGE Publications; London: 2006. [Google Scholar]
- 38.Estrada CA, Krishnamoorthy P, Smith A, et al. Using onling marketing to increase participation in a web-based continuing medical education cultural competence curriculum. Journal of Continuing Education in Health Professions. 2011;31(1):21–27. doi: 10.1002/chp.20097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Santucci LC, McHugh RK, Barlow DH. Direct-to-consumer marketing of evidence-based psychological interventions: introduction. Behav Ther. 2012;43(2):231–235. doi: 10.1016/j.beth.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 40.Szymanski J. Using direct-to-consumer marketing strategies with obsessive-compulsive disorder in the nonprofit sector. Behavior Therapy. 2012;43:251–256. doi: 10.1016/j.beth.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 41.Tanf Reauthorization Act TANF Reauthorization Act of 2001. 2001 [Google Scholar]
- 42.Thomas A, Menon A, Boruff J, Rodriguez AM, Ahmed S. Applications of social constructivist learning theories in knowledge translation for healthcare professionals: a scoping review. Implementation science : IS. 2014;9:54. doi: 10.1186/1748-5908-9-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pavetti L, Derr MK, Kauff JF, Barrett A. Mental disorders and service use among welfare and disability program participants in fee-for-service Medicaid. Psychiatr. Serv. 2010;61:495–499. doi: 10.1176/ps.2010.61.5.495. Journal Article. [DOI] [PubMed] [Google Scholar]
- 44.Anderson SG, Halter AP, Gryzlak BM. Difficulties after leaving TANF: Inner-city women talk about reasons for returning to welfare. Soc. Work Res. 2004;49:185–194. doi: 10.1093/sw/49.2.185. Journal Article. [DOI] [PubMed] [Google Scholar]
- 45.Fagnoni C. Welfare Reform Outcomes for TANF Recipients with Impairments. United States General Accounting Office; Washington, DC: 2002. GAO-02-884. [Google Scholar]
- 46.Kneipp SM, Welch DP, Wood CE, Yucha CB, Yarandi H. Psychosocial and physiological stress among women leaving welfare. West. J. Nurs. Res. 2007;29(7):864–883. doi: 10.1177/0193945906297378. discussion 884-895. [DOI] [PubMed] [Google Scholar]
- 47.Zedlewski S. Work and Barriers to Work among Welfare Recipients in 2002. The Urban Institute; Washington, D.C.: 2003. [Google Scholar]
- 48.Zedlewski SR. Work Activity and Obstacles to Work Among TANF Recipients. The Urban Institute; Washington, DC: 1999. (Series B, No. B-2). [Google Scholar]
- 49.Dearing JW. Applying Diffusion of Innovation Theory to Intervention Development. Res Soc Work Pract. 2009;19(5):503–518. doi: 10.1177/1049731509335569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Birken SA, Lee SY, Weiner BJ. Uncovering middle managers' role in healthcare innovation implementation. Implementation science : IS. 2012;7:28. doi: 10.1186/1748-5908-7-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Birken SA, Lee SY, Weiner BJ, Chin MH, Schaefer CT. Improving the effectiveness of health care innovation implementation: middle managers as change agents. Med. Care Res. Rev. 2013;70(1):29–45. doi: 10.1177/1077558712457427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Birken S. How Middle Managers Can Influence Innovation Implementation. 2015 https://innovations.ahrq.gov/perspectives/how-middle-managers-can-influence-innovation-implementation-3. Accessed January 10, 2015.
- 53.Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheney T. Effects of hospital care environment on patient mortality and nurse outcomes. J. Nurs. Adm. 2009;39(7-8 Suppl):S45–51. doi: 10.1097/NNA.0b013e3181aeb4cf. [DOI] [PubMed] [Google Scholar]
- 54.Mark BA, Jones CB, Lindley L, Ozcan YA. An examination of technical efficiency, quality, and patient safety in acute care nursing units. Policy, politics & nursing practice. 2009;10(3):180–186. doi: 10.1177/1527154409346322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Aiken LH, Shang J, Xue Y, Sloane DM. Hospital use of agency-employed supplemental nurses and patient mortality and failure to rescue. Health Serv. Res. 2013;48(3):931–948. doi: 10.1111/1475-6773.12018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mabry PL, Milstein B, Abraido-Lanza AF, Livingood WC, Allegrante JP. Opening a window on systems science research in health promotion and public health. Health Educ. Behav. 2013;40(1 Suppl):5S–8S. doi: 10.1177/1090198113503343. [DOI] [PubMed] [Google Scholar]
- 57.Hu XH, Golden W, Bolge SC, et al. Predictability of future attacks by migraineurs: a prospective observational study. Headache. 2010;50(8):1296–1305. doi: 10.1111/j.1526-4610.2010.01630.x. [DOI] [PubMed] [Google Scholar]
- 58.Burke JG, Lich KH, Neal JW, Meissner HI, Yonas M, Mabry PL. Enhancing Dissemination and Implementation Research Using Systems Science Methods. International journal of behavioral medicine. 2014 doi: 10.1007/s12529-014-9417-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Luke DA, Wald LM, Carothers BJ, Bach LE, Harris JK. Network influences on dissemination of evidence-based guidelines in state tobacco control programs. Health Educ. Behav. 2013;40(1 Suppl):33S–42S. doi: 10.1177/1090198113492760. [DOI] [PubMed] [Google Scholar]
- 60.Yessis J, Riley B, Stockton L, Brodovsky S, Von Sychowski S. Interorganizational relationships in the Heart and Stroke Foundation's Spark Together for Healthy Kids: insights from using network analysis. Health Educ. Behav. 2013;40(1 Suppl):43S–50S. doi: 10.1177/1090198113490724. [DOI] [PubMed] [Google Scholar]
- 61.Kneipp S, Gilleskie D, Sheely A, Schwartz T, Gilmore RM, Atkinson D. Nurse scientists overcoming challenges to lead transdisciplinary research teams. Nurs. Outlook. 2014;62:352–361. doi: 10.1016/j.outlook.2014.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Burgio LD. Disentangling the translational sciences: a social science perspective. Research and theory for nursing practice. 2010;24(1):56–63. doi: 10.1891/1541-6577.24.1.56. [DOI] [PubMed] [Google Scholar]
- 63.Lee KA, Dziadkowiec O, Meek P. A systems science approach to fatigue management in research and health care. Nurs. Outlook. 2014;62(5):313–321. doi: 10.1016/j.outlook.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 64.Jemmott JB, 3rd, Jemmott LS, Braverman PK, Fong GT. HIV/STD risk reduction interventions for African American and Latino adolescent girls at an adolescent medicine clinic: a randomized controlled trial. Arch. Pediatr. Adolesc. Med. 2005;159(5):440–449. doi: 10.1001/archpedi.159.5.440. [DOI] [PubMed] [Google Scholar]
- 65.Breitenstein SM, Gross D, Fogg L, et al. The Chicago Parent Program: comparing 1-year outcomes for African American and Latino parents of young children. Res. Nurs. Health. 2012;35(5):475–489. doi: 10.1002/nur.21489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gross D, Garvey C, Julion W, Fogg L, Tucker S, Mokros H. Efficacy of the Chicago parent program with low-income African American and Latino parents of young children. Prevention science : the official journal of the Society for Prevention Research. 2009;10(1):54–65. doi: 10.1007/s11121-008-0116-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Grey M, Boland EA, Davidson M, Li J, Tamborlane WV. Coping skills training for youth with diabetes mellitus has long-lasting effects on metabolic control and quality of life. J. Pediatr. 2000;137(1):107–113. doi: 10.1067/mpd.2000.106568. [DOI] [PubMed] [Google Scholar]
- 68.Melnyk BM, Feinstein N, Fairbanks E. Two decades of evidence to support implementation of the COPE program as standard practice with parents of young unexpectedly hospitalized/critically ill children and premature infants. Pediatr. Nurs. 2006;32(5):475–481. [PubMed] [Google Scholar]
- 69.The Centers for Disease Control and Prevention Sister to Sister: An HIV Risk Reduction Intervention “Respect yourself, protect yourself, because you are worth it!”. 2015 [Google Scholar]
- 70.(AHRQ) AfHRQ Coping Skills Training Helps Adolescents Improve Quality of Life and Ability to Manage Their Diabetes. 2015 [Google Scholar]