Abstract
Objective
Patient decision aids are important tools for facilitating balanced, evidence-based decision making. However, the potential of decision aids to lower health care utilization and costs is uncertain; few studies have investigated the cost-effectiveness of decision aids that change patient behavior. Using an example of a decision aid for colorectal cancer screening, we provide a framework for analyzing the cost-effectiveness of decision aids.
Methods
A decision-analytic model with two strategies (decision aid or no decision aid) was used to calculate expected costs in U.S. dollars and benefits measured in life-years saved (LYS). Data from a systematic review of ten studies about decision aid effectiveness was used to calculate the percentage increase in the number of people choosing screening instead of no screening. We then calculated the incremental cost per LYS with the use of the decision aid.
Results
The no decision aid strategy had an expected cost of $3,023 and yielded 18.19 LYS. The decision aid strategy cost $3,249 and yielded 18.20 LYS. The incremental cost-effectiveness ratio for the decision aid strategy was $36,126 per LYS. Results were sensitive to the cost of the decision aid and the percentage change in behavior caused by the decision aid.
Conclusions
This study provides proof-of-concept evidence for future studies examining the cost-effectiveness of decision aids. The results suggest that decision aids can be beneficial and cost-effective.
Keywords: Patient decision aids, Decision making, Colorectal cancer, Screening, Cost and cost analysis
Introduction
Patient decision aids are tools designed to provide unbiased, comprehensive, evidence-based information health care options to help patients participate in health care decision making (Alston et al., 2014). These tools support shared decision making among patients and their health care providers by promoting the deliberation and exploration of patients’ values, with the goal of arriving at a shared decision that is consistent with the informed preferences of the patient (Volk et al., 2013). Past research and experience have shown that the use of decision aids reduces decision conflict in patients, increases their knowledge, and bolsters their participation in decision making (Stacey et al., 2014; Walsh et al., 2014). In addition, decision aids can reduce the overuse of procedures that are questionably effective or highly preference-sensitive (Arterburn et al., 2012). However, few studies have investigated whether decision aids can improve clinical outcomes by helping patients choose strategies that prolong survival or enhance quality of life.
There is ongoing debate about the role patient decision aids have in reducing health care costs (Walsh et al., 2014). Reductions in overtreatment and unwarranted practice variation are cited as principle vehicles through which health care savings from the adoption of a shared decision making approach, and by extension the patient decision aids used to support shared decision making, might be realized (Oshima Lee and Emanuel, 2013). One study’s findings suggest that the use of decision aids causes patients to choose less invasive, less expensive alternatives, thereby reducing the number of patients who undergo elective surgery as well as overall healthcare costs (Wennberg, 2011). However, systematic reviews have shown that such studies yield little definitive evidence that decision aids reduce costs or push patients towards the least expensive option (Katz and Hawley, 2013; Walsh et al., 2014). Furthermore, none of the studies that have evaluated the potential savings of using a decision aid (Katz, 2014; Walsh et al., 2014) have considered cost-effectiveness in terms of an incremental cost-effectiveness ratio (ICER), which makes it difficult to compare these studies’ outcomes.
Because the benefits of decision aids are not typically expressed in an outcome measure such as life-years saved (LYS), the cost-effectiveness of decision aids has not been frequently examined. Rather than determining whether a decision aid will save money, a cost-effectiveness analysis, which incorporates a predefined willingness-to-pay threshold, determines whether a decision aid will change patient behavior and improve outcomes enough to warrant its cost. Although using a decision aid adds to the cost of screening initially, this additional cost may be worthwhile if the decision aid changes behavior enough to decrease the total long-term costs and/or increase the screening’s effectiveness in terms of LYS or quality-adjusted LYS. Assessing the cost-effectiveness of decision aids could provide useful information for payers and policy makers and potentially increase the dissemination and acceptability of aids found to be cost-effective.
Because it has been shown to be effective in detecting early-stage disease and prolonging patients’ lives, colorectal cancer screening presents a good opportunity to evaluate the cost-effectiveness of decision aids. Patients’ preferences for colorectal cancer screening vary greatly, with many patients choosing no screening (Meissner et al., 2006; Sheikh et al., 2004). Decision aids have the potential to change this trend by prompting patients to choose among several recommended screening options that will improve their outcomes and thus the overall outcomes for a population. This paper presents a framework for assessing the cost-effectiveness of decision aids using colorectal cancer screening as an example. A decision-analytic model that incorporated the decision aid as an intervention was used to assess the aid’s potential influence on economic costs and clinical benefits.
Methods
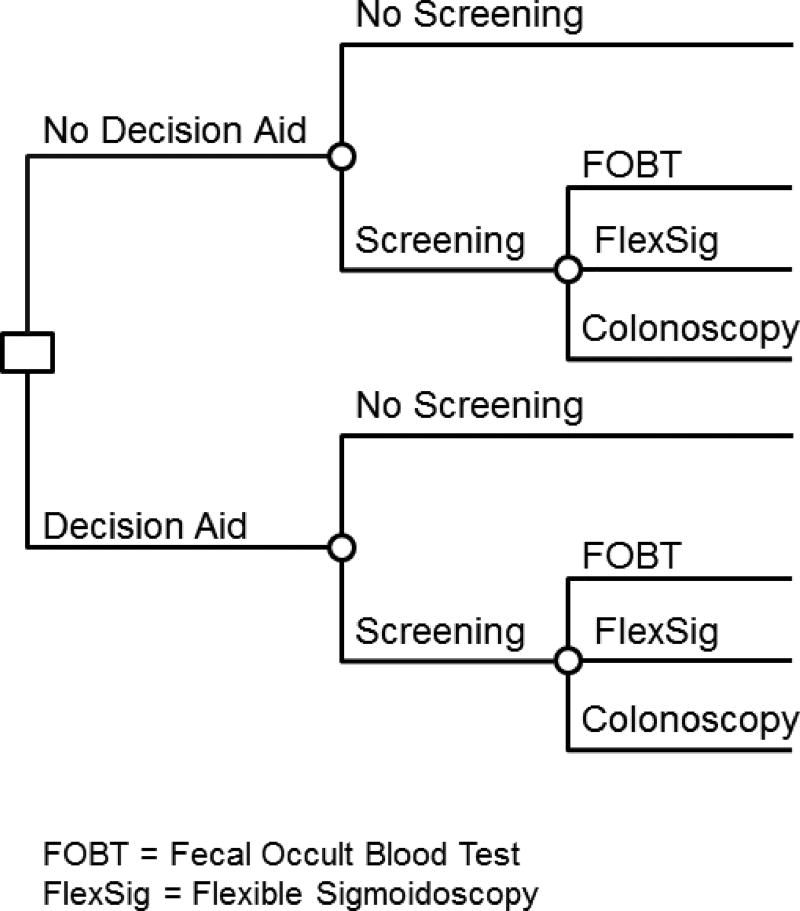
In this study, a simple decision-analytic model was used to incorporate the costs and effectiveness of two potential strategies: decision aid use and no decision aid use. The structure of the model is shown in Figure 1.
Figure 1.
Decision-analytic model
The model is relatively simple: the decision tree begins with a decision node indicating whether a decision aid is used. All patients then decide whether to undergo some type of colorectal cancer screening. Patients who elect to undergo screening then choose among three screening strategies: fecal occult blood testing (FOBT), flexible sigmoidoscopy, or colonoscopy. Outcomes are the fraction of participants who choose each of the screening strategies. Each strategy is associated with a cost and an effectiveness. Costs, measured in 2013 U.S. dollars, include the cost of administering screening and the cost of clinician time; the decision aid strategy has the added cost of administering the decision aid. Each strategy’s effectiveness, measured in LYS, is calculated from life tables of colorectal cancer patients and varies according to how well a given screening test can identify the disease (Khandker et al., 2000). In the present study, both the cost and the effectiveness were discounted by 3%, as recommended by the U.S. Panel on Cost Effectiveness in Health and Medicine (Lipscomb et al., 1996). The cost per LYS was the outcome measure.
Model parameters
The results of previously published analyses that evaluated colorectal cancer screening strategies (Frazier et al., 2000; Khandker et al., 2000; Ladabaum et al., 2010; Lansdorp-Vogelaar et al., 2010; O'Leary et al., 2004; Pignone et al., 2002; Sonnenberg and Delco, 2002; Telford et al., 2010; Tsoi et al., 2008; Vijan et al., 2001; Zauber et al., 2008) were used to identify the expected cost and effectiveness of each screening strategy in the present study. The previously published analyses were normative strategies, i.e., they sought to determine the expected costs and benefits of screening. To be considered in the present study, the studies had to evaluate the cost-effectiveness of colorectal cancer screening strategies, including colonoscopy, FOBT, and flexible sigmoidoscopy, and publish results in the form of dollars per LYS or dollars per quality-adjusted LYS. Because it provided the cost parameters and effectiveness parameters separately, the study by Khandker et al., an economic evaluation of a variety of screening strategies for colorectal cancer, was used as the source of data input in the present study (Khandker et al., 2000). Only four of the strategies that Khandker et al. evaluated were assessed in the present study: 1) no screening, 2) annual FOBT, 3) flexible sigmoidoscopy every 5 years, and 4) colonoscopy every 10 years. Since the decision tree divides the screening decision into only screening or no screening, the three screening strategies were combined. Data about patients’ preference for individual screening strategies were adjusted accordingly by calculating the conditional probabilities of each strategy.
Time frame
In keeping with the Panel for Cost-Effectiveness in Health and Medicine guidelines for analyzing cost-effectiveness, the costs associated with colorectal cancer and each of the screening strategies were estimated using a lifetime analytic horizon to ensure that the long-term benefits of the interventions were included in the analysis (Lipscomb et al., 1996).
Costs
Each screening strategy’s cost to the healthcare provider was derived from the study by Khandker et al. and adjusted to be expressed in 2013 dollars (Khandker et al., 2000). Khandker et al. used Medicare and private insurance claims data to identify the costs to the healthcare provider rather than those to the patients; however, they did not take into account patient or physician time, which would provide a more accurate estimate of cost in a decision aid analysis.
The cost of the decision aid on a per-use basis was $22.90. Table 1 shows the breakdown of these costs in 2013 dollars. Patient and healthcare costs were calculated using estimates of the average hourly wage from the Bureau of Labor Statistics. The total patient time costs included 20 minutes to view the decision aid and 2.5 minutes to consult with a healthcare provider. Healthcare provider consultation time costs included the time that clinicians spent with the patient and were calculated using the average wage for healthcare providers estimated by the Bureau of Labor Statistics. The median increase in consultation time due to using a decision aid was 2.5 minutes, which was the base case for the study (Stacey et al., 2014). The fixed costs required to develop and design the decision aid were calculated in a study by Kennedy et al. and amounted to $0.26 per patient (Kennedy et al., 2002). These costs were spread over 3 years since Kennedy et al. predicted that this would be the active life of the intervention. Finally, the per-patient cost to disseminate the decision aids was $12.81 (van Peperstraten et al., 2010). It was assumed that all patients received the decision aid and that all patients used the aid only once, at 50 years of age. Thus, the results of a cost-effectiveness analysis served as input parameters in the decision-analysis model (Table 2).
Table 1.
Fixed and variable per-patient costs of using a decision aid.
| Cost type | Per-patient cost, 2013 USD |
Source |
|---|---|---|
| Patient time to use decision aid (20 min) | 7.46 | BLS, 2013 |
| Patient consultation (2.5 min) | 0.93 | BLS, 2013 |
| Healthcare provider consultation (2.5 min) | 1.50 | BLS, 2013 |
| Development of decision aid | 0.26 | Kennedy et al., 2002 |
| Dissemination of decision aid | 12.77 | van Peperstraten et al., 2010 |
| Total | 22.90 |
USD, U.S. dollars; BLS, Bureau of Labor Statistics.
Table 2.
Cost and effectiveness of screening strategies according to Khandker et al., 2002.
| Strategy | Cost, USDa | Effectiveness, LYS |
|---|---|---|
| No screening | 1,287 | 18.14 |
| Flex-sig | 3,428 | 18.23 |
| FOBT | 4,119 | 18.24 |
| Colonoscopy | 5,208 | 18.25 |
USD, U.S. dollars; LYS, life-years saved; Flex-sig, flexible sigmoidoscopy; FOBT, fecal occult blood testing.
Costs were adjusted and are expressed in 2013 USD.
Effectiveness
A decision aid’s effectiveness is measured in terms of its impact on patient behavior. Thus, the change in patient selection of the screening strategy after use of the decision aid was estimated. Data from a systematic review of ten studies about decision aid effectiveness was used to calculate the increase in the number of people choosing screening instead of no screening (Stacey et al., 2014). This percentage change was identified by calculating the difference across all 10 studies between the percentage of patients who chose some screening option in the experimental groups (39.82%) and in the control groups (33.87%) Previously published analyses were used to determine the participants’ screening patterns; data about patients’ screening strategy preferences were obtained from the study by Meissner et al. (Meissner et al., 2006), who compiled data from 5 years’ worth of National Health Interview Surveys to illustrate patients’ preferences for colorectal cancer screening among FOBT, flexible sigmoidoscopy, colonoscopy, and no screening (Meissner et al., 2006). In the present study, these survey data were used as the base case (Table 3).
Table 3.
Preference changes caused by decision aids according to (Meissner et al., 2006)
| Strategy | Fraction of cohort opting for strategy before decision aid |
Fraction of cohort opting for strategy after decision aid |
|---|---|---|
| No screening | 0.49 | 0.43 |
| Flex-sig | 0.05 | 0.06 |
| FOBT | 0.16 | 0.18 |
| Colonoscopy | 0.30 | 0.34 |
Flex-sig, flexible sigmoidoscopy; FOBT, fecal occult blood testing.
Analysis
Weighted averages of each strategy’s expected cost and expected effectiveness were calculated. The cost per LYS for both strategies was derived and used to calculate a comparative ICER that described the cost-effectiveness of the decision aids. The ICER was calculated by dividing the incremental cost of using the decision aids by the incremental effectiveness, in LYS, of using the decision aids. The analysis was modeled using TreeAge Pro, a decision analysis software program. Sensitivity analyses were performed to determine the degree to which the conclusions of the base case analysis were sensitive to changes in the model parameters. One-way sensitivity analyses were performed to determine the sensitivity of the ICER to the cost of the decision aid and the percentage change in behavior caused by the decision aid.. In addition, a tornado diagram was used to illustrate the relative impact of changes in uncertain parameters on the ICER as compared to a willingness-to-pay threshold of $50,000/LYS. The sensitivity analysis had a lower bound of half the value of the base case and an upper bound of twice the value of the base case.
Results
Cost-effectiveness analysis
The no–decision aid strategy had an expected cost of $3,023.37 and yielded 18.19 LYS. The decision aid strategy had an expected cost of $3,248.86 and yielded 18.20 LYS. The assumed 5.95% change in preferences from no screening to screening resulted in a marginal increase in both the cost and effectiveness of the decision aid. The decision aid had an incremental cost of $225.49 and an incremental benefit of 0.01 LYS, which resulted in an ICER of $36,125.79 per LYS.
Uncertainty and sensitivity analysis
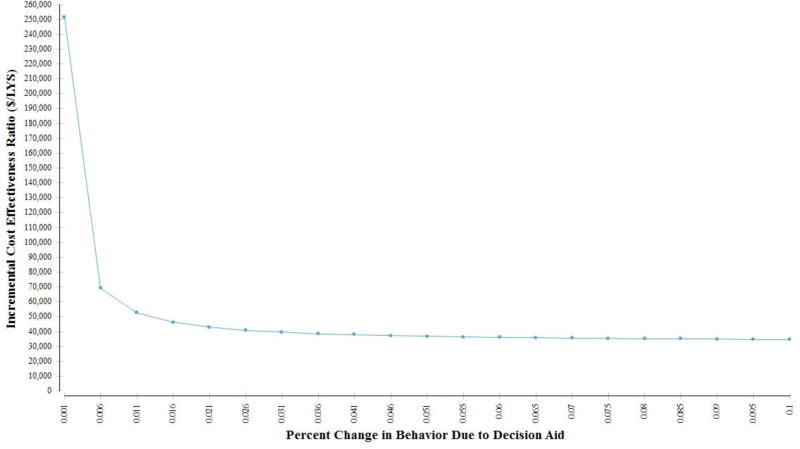
The sensitivity analysis revealed the ways in which variations in key parameters affected the ICER. For example, the ICER was affected by variation in the percentage of people who changed from no screening to screening (Figure 2).
Figure 2.
One-way sensitivity analysis of the percentage change from no screening to screening.
The decision aid was cost-effective for all but minimal change rates. The cost-effectiveness exceeded the willingness-to-pay threshold only if the decision aid caused less than 1.4% of patients to change their behavior.
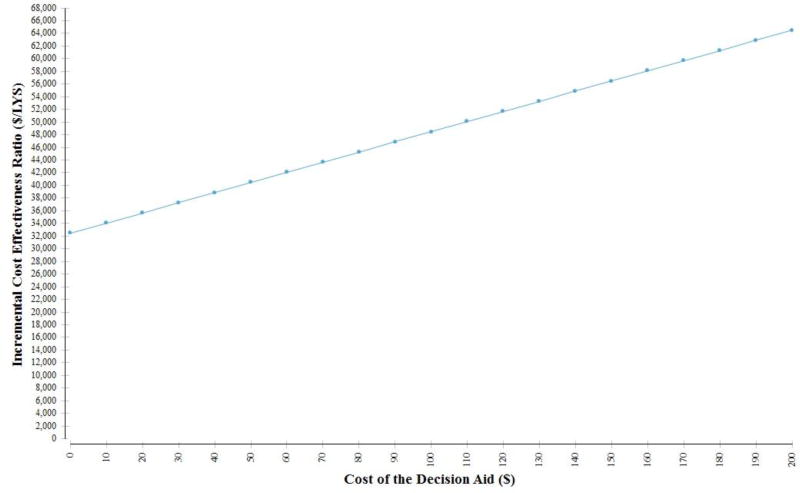
The effect of variation in decision aid cost on the ICER is shown in Figure 3.
Figure 3.
One-way sensitivity analysis of decision aid cost.
The decision aid strategy was not cost-effective if the cost of using it exceeded $110. If the variable costs and patient time costs were more than 5 times higher than those estimated, the decision aid was not cost-effective.
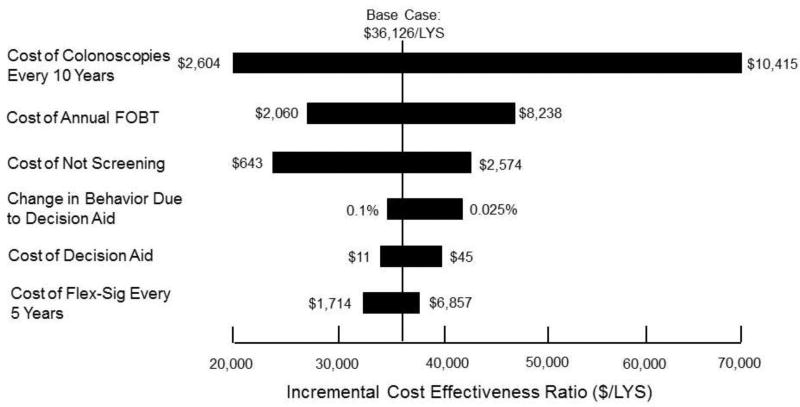
The effect of changing various model parameters is shown in the tornado diagram in Figure 4.
Figure 4.
Sensitivity of ICER to variation in model parameters.
The ICER was most sensitive to variation in the cost of each strategy, especially colonoscopy, FOBT, and no screening. Of the parameters shown, the cost of colonoscopies every 10 years had the greatest effect on the ICER. The ICER was moderately sensitive to changes in behavior due to the decision aid and to the cost of the decision aid in the interval shown.
Discussion
The present study’s findings suggest that using a decision aid to influence patient behavior regarding colorectal cancer screening is generally a cost-effective strategy. The ICER of $36,125.79 per LYS was below the willingness-to-pay threshold and was sensitive to the change in behavior caused by the decision aids as well as variation in the cost of distributing and using the aids.
In the present study, it was estimated that the decision aid would change the screening preferences of 5.95% of the patients. However, even if the decision aid were much less effective at changing patients’ behavior, it would still be fairly cost-effective. If the decision aid caused more than a 5.95% change in behavior, its cost effectiveness would grow incrementally. However, if the change in behavior were closer to 1%, the decision aid would be much less cost-effective, costing more than $50,000 per LYS. In their study, Schroy et al. (Schroy 3rd et al., 2012) found that decision aids caused about an 8% change from no screening to screening. This is similar to the 5.95% change assumed in the present study and lends credence to the study’s estimates of the decision aid’s influence on patient behavior. Moreover, the sensitivity results are encouraging: The decision aid failed to be a viable strategy only if it was extremely ineffective at changing patient preferences.
The intervention worked well and was cost-effective as long as the cost of the decision aid was less than $110 per patient. This per-patient cost did not include the cost of developing the decision aid or periodically updating it to reflect the most recent evidence, but rather the cost of using it. Omitting the cost of developing the decision aid from the analysis is reasonable if the aid is produced and placed in the public domain and no other costs are associated with adopting it. In addition, the costs of developing and updating the decision aid would be spread among a large number of patients who interact with it, which would make the per-patient costs very small. In fact, the majority of the decision aid’s cost came from the valuation of patient time. If these costs are low, the decision aid strategy is cost-effective.
In addition, sensitivity analyses of other parameters showed that the cost-effectiveness of the decision aid was sensitive to the cost of each screening strategy. Thus, if the decision aid actually caused a change in behavior that resulted in patients selecting lower-cost screening strategies, its cost-effectiveness would greatly increase. The cost-effectiveness of the decision aid would continue to improve as the costs of these screening strategies are reduced through technological advancements.
The present study had several potential limitations. For one, many of the numbers used to calculate the cost-effectiveness ratio were estimates based on values given in previous studies. The lack of accurate measurements of the effectiveness of decision aids would no doubt change their overall cost-effectiveness. In addition, for simplicity, it was assumed that the decision aid would create a 5.95% change in patient preference from no screening to screening and that this increase in screening would be distributed among all three screening strategies based on current patient preferences. However, an actual decision aid could create a more complicated change in screening preferences, perhaps by encouraging patients to favor one screening option over others. Based on the findings of previous studies, these more complex changes in behavior (e.g., moving patients’ preference from FOBT or flexible sigmoidoscopy to colonoscopy) would actually push patients to a more cost-effective pattern of preferences, thereby lowering the ICER of the decision aid (Leard et al., 1997; Pignone et al., 1999; Schroy 3rd et al., 2012). Finally, the impact of patient noncompliance was not considered in the present study. There is very little data about how decision aids affect long-term compliance with colorectal cancer screening standards. In the present study, we made the simplifying assumption that a one-time interaction with the decision aid would permanently change patient behavior. This is not always the case, however. Although a decision aid could encourage patients to undergo FOBT once, they might not return for the FOBT annually thereafter. The model in the present study did not consider this scenario, which may have led to a slight overestimation of the effectiveness of each screening strategy as compared to the no screening option. However, compliance rates with and without the use of decision aids should be similar, with some studies suggesting higher compliance rates after using decision aids (Ling et al., 2009; Menon et al., 2011). Such an effect on compliance would improve the effectiveness of decision aids.
This study used an estimate of the decision aid cost in the decision analysis. This was mainly because there is little research on the cost of decision aids, which makes it difficult to identify an exact value. However, the sensitivity analysis tested the validity of the estimates using a range of different decision aid costs. The study also did not take into account any one-time development costs or continuing maintenance costs because it was assumed that these costs would be amortized over the life of the decision aid to the point of negligibility. Of course, if development and dissemination costs were high, the decision aid cost would increase and its cost-effectiveness would decrease; however, this situation seems unlikely in the colorectal cancer screening setting because a single decision aid could be used by multiple patients and would not have to be replaced often. Thus, the addition of development costs should not dramatically reduce the cost-effectiveness of the decision aid.
The analysis in the present study modeled cost-effectiveness in terms of LYS. However, one major focus in evaluating decision support tools that was not included in the present study was the role decision aids have in increasing decision quality (O'Connor et al., 2007). Decision quality is a measurement of how well a patient’s decision matches both clinical knowledge and the patient’s own goals and concerns. Although scales to quantify this increase are being developed, such scales were not included in the present study’s analysis mainly because evaluating the non-standardized outcome of such a model would be difficult. For example, the present analysis could have revealed that improving decision quality by one point on the scale would cost an additional $10, but no existing standard is available to tell help determine whether that increase in cost would be acceptable to policy makers and healthcare providers. Thus, a cost-effectiveness model that evaluates dollars per LYS is preferred because the use of established willingness-to-pay thresholds has been documented in previous studies and because this metric can be compared across diseases and interventions.
The results of the present study are promising because they provide proof-of-concept evidence for future studies examining the cost-effectiveness of decision aids in promoting behavioral change. For decisions for which strategies associated with increased life expectancy are underutilized, such as screening for colorectal cancer, examining the cost-effectiveness of using patient decision aids seems warranted. For other clinical decisions for which overutilization of a certain strategy is a concern, the same approach may be justified. By no means does the present study provide a perfect estimation of the value of decision aids. However, the present study’s most compelling evidence supporting the use of decision aids is that even in the sensitivity analysis, the ICER of the decision aid strategy was below the willingness-to-pay threshold for most values. This paper lays out a framework for conducting studies of decision aids, and the results presented here suggest that such aids are cost-effective. With more accurate estimations of costs, life expectancies, behavior patterns, and utilities, this model can be adjusted to produce results that are much more accurate than those presented here. If anything, the findings of the present study indicate that additional research in this relatively new area is warranted so that policy makers and healthcare providers can evaluate the benefits of adding more decision aids in clinical and preventive settings.
Highlights.
We provide a framework for analyzing the cost-effectiveness of decision aids.
A decision analysis evaluated use of a decision aid for colorectal cancer screening.
Use of the decision aid strategy was shown to be cost-effective.
Results were sensitive to cost and percentage change in behavior caused by the aid.
The results suggest that decision aids can be beneficial and cost-effective.
Acknowledgments
The authors thank Joe Munch in MD Anderson’s Department of Scientific Publications for editing the manuscript.
Funding
Financial support for this study was provided in part by a grant from the Informed Medical Decisions Foundation, now a division of Healthwise (#0169-1); the funding agreement ensured the authors’ independence in designing the study, interpreting the data, and writing and publishing the report. The findings and conclusions reported in this paper do not necessarily reflect those of the sponsor. The sponsor had no role in the study design; collection, analysis, and interpretation of data; the writing of this manuscript; or the decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement
The authors have no conflicts of interest to declare.
References
- Alston C, Berger Z, Brownlee S, Elwyn G, Fowler F, Jr, Kelly Hall L, Montori V, Moulton B, Paget L, et al. Shared decision-making strategies for best care: patient decision aids, Discussion Paper. Institute of Medicine; Washington DC: 2014. [Google Scholar]
- Arterburn D, Wellman R, Westbrook E, Rutter C, Ross T, McCulloch D, Handley M, Jung C. Introducing decision aids at Group Health was linked to sharply lower hip and knee surgery rates and costs. Health Aff. (Millwood) 2012;31:2094–104. doi: 10.1377/hlthaff.2011.0686. [DOI] [PubMed] [Google Scholar]
- Frazier AL, Colditz GA, Fuchs CS, Kuntz KM. Cost-effectiveness of screening for colorectal cancer in the general population. JAMA. 2000;284:1954–61. doi: 10.1001/jama.284.15.1954. [DOI] [PubMed] [Google Scholar]
- Katz SJ. Treatment decision aids are unlikely to cut healthcare costs. BMJ. 2014;348:g1172. doi: 10.1136/bmj.g1172. [DOI] [PubMed] [Google Scholar]
- Katz SJ, Hawley S. The value of sharing treatment decision making with patients: expecting too much? JAMA. 2013;310:1559–60. doi: 10.1001/jama.2013.278944. [DOI] [PubMed] [Google Scholar]
- Kennedy AM, Sculpher MJ, Coulter A, et al. Effects of decision aids for menorrhagia on treatment choices, health outcomes, and costs: A randomized controlled trial. JAMA. 2002;288:2701–08. doi: 10.1001/jama.288.21.2701. [DOI] [PubMed] [Google Scholar]
- Khandker RK, Dulski JD, Kilpatrick JB, Ellis RP, Mitchell JB, Baine WB. A decision model and cost-effectiveness analysis of colorectal cancer screening and surveillance guidelines for average-risk adults. Int. J. Technol. Assess. Health Care. 2000;16:799–810. doi: 10.1017/s0266462300102077. [DOI] [PubMed] [Google Scholar]
- Ladabaum U, Ferrandez A, Lanas A. Cost-effectiveness of colorectal cancer screening in high-risk Spanish patients: use of a validated model to inform public policy. Cancer Epidemiol. Biomarkers Prev. 2010;19:2765–76. doi: 10.1158/1055-9965.EPI-10-0530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansdorp-Vogelaar I, Kuntz KM, Knudsen AB, Wilschut JA, Zauber AG, van Ballegooijen M. Stool DNA testing to screen for colorectal cancer in the Medicare population: a cost-effectiveness analysis. Ann. Intern. Med. 2010;153:368–77. doi: 10.1059/0003-4819-153-6-201009210-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leard LE, Savides TJ, Ganiats TG. Patient preferences for colorectal cancer screening. J. Fam. Pract. 1997;45:211–8. [PubMed] [Google Scholar]
- Ling BS, Schoen RE, Trauth JM, et al. Physicians encouraging colorectal screening: A randomized controlled trial of enhanced office and patient management on compliance with colorectal cancer screening. Arch. Intern. Med. 2009;169:47–55. doi: 10.1001/archinternmed.2008.519. [DOI] [PubMed] [Google Scholar]
- Lipscomb J, Weinstein MC, Torrance GW. Time Preference. In: Gold MR, Siegel JE, Russell LB, Weinstein MC, editors. Cost-Effectiveness in Health and Medicine. Oxford University Press; USA: 1996. pp. 214–35. [Google Scholar]
- Meissner HI, Breen N, Klabunde CN, Vernon SW. Patterns of colorectal cancer screening uptake among men and women in the United States. Cancer Epidemiol. Biomarkers Prev. 2006;15:389–94. doi: 10.1158/1055-9965.EPI-05-0678. [DOI] [PubMed] [Google Scholar]
- Menon U, Belue R, Wahab S, Rugen K, Kinney AY, Maramaldi P, Wujcik D, Szalacha LA. A randomized trial comparing the effect of two phone-based interventions on colorectal cancer screening adherence. Ann. Behav. Med. 2011;42:294–303. doi: 10.1007/s12160-011-9291-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor AM, Wennberg JE, Legare F, Liewehyn-Thomas HA, Moulton BW, Sepucha KR, Sodano AG, King JS. Toward the 'tipping point': decision aids and informed patient choice. Health Aff. (Millwood) 2007;26:716–25. doi: 10.1377/hlthaff.26.3.716. [DOI] [PubMed] [Google Scholar]
- O'Leary BA, Olynyk JK, Neville AM, Platell CF. Cost-effectiveness of colorectal cancer screening: comparison of community-based flexible sigmoidoscopy with fecal occult blood testing and colonoscopy. J. Gastroenterol. Hepatol. 2004;19:38–47. doi: 10.1111/j.1440-1746.2004.03177.x. [DOI] [PubMed] [Google Scholar]
- Oshima Lee E, Emanuel EJ. Shared decision making to improve care and reduce costs. N. Engl. J. Med. 2013;368:6–8. doi: 10.1056/NEJMp1209500. [DOI] [PubMed] [Google Scholar]
- Pignone M, Bucholtz D, Harris R. Patient preferences for colon cancer screening. J. Gen. Intern. Med. 1999;14:432–37. doi: 10.1046/j.1525-1497.1999.00018.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pignone M, Saha S, Hoerger T, Mandelblatt J. Cost-effectiveness analyses of colorectal cancer screening: a systematic review for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2002;137:96–104. doi: 10.7326/0003-4819-137-2-200207160-00007. [DOI] [PubMed] [Google Scholar]
- Schroy PC, 3rd, Emmons KM, Peters E, Glick JT, Robinson PA, Lydotes MA, Mylvaganam SR, Coe AM, Chen CA, et al. Aid-assisted decision making and colorectal cancer screening: a randomized controlled trial. Am. J. Prev. Med. 2012;43:573–83. doi: 10.1016/j.amepre.2012.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheikh RA, Kapre S, Calof OM, Ward C, Raina A. Screening preferences for colorectal cancer: a patient demographic study. South. Med. J. 2004;97:224–30. doi: 10.1097/01.SMJ.0000078619.39604.3D. [DOI] [PubMed] [Google Scholar]
- Sonnenberg A, Delco F. Cost-effectiveness of a single colonoscopy in screening for colorectal cancer. Arch. Intern. Med. 2002;162:163–8. doi: 10.1001/archinte.162.2.163. [DOI] [PubMed] [Google Scholar]
- Stacey D, Legare F, Col NF, Bennett CL, Barry MJ, Eden KB, Holmes-Rovner M, Llewellyn-Thomas H, Lyddiatt A, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst. Rev. 2014;1:CD001431. doi: 10.1002/14651858.CD001431.pub4. [DOI] [PubMed] [Google Scholar]
- Telford JJ, Levy AR, Sambrook JC, Zou D, Enns RA. The cost-effectiveness of screening for colorectal cancer. CMAJ. 2010;182:1307–13. doi: 10.1503/cmaj.090845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsoi KK, Ng SS, Leung MC, Sung JJ. Cost-effectiveness analysis on screening for colorectal neoplasm and management of colorectal cancer in Asia. Aliment. Pharmacol. Ther. 2008;28:353–63. doi: 10.1111/j.1365-2036.2008.03726.x. [DOI] [PubMed] [Google Scholar]
- van Peperstraten A, Nelen W, Grol R, Zielhuis G, Adang E, Stalmeier P, Hermens R, Kremer J. The effect of a multifaceted empowerment strategy on decision making about the number of embryos transferred in in vitro fertilisation: randomised controlled trial. BMJ. 2010;341:c2501. doi: 10.1136/bmj.c2501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vijan S, Hwang EW, Hofer TP, Hayward RA. Which colon cancer screening test? A comparison of costs, effectiveness, and compliance. Am. J. Med. 2001;111:593–601. doi: 10.1016/s0002-9343(01)00977-9. [DOI] [PubMed] [Google Scholar]
- Volk R, Llewellyn-Thomas H, Stacey D, Elwyn G. Ten years of the International Patient Decision Aid Standards Collaboration: evolution of the core dimensions for assessing the quality of patient decision aids. BMC Med. Inform. Decis. Mak. 2013;13:S1. doi: 10.1186/1472-6947-13-S2-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh T, Barr PJ, Thompson R, Ozanne E, O'Neill C, Elwyn G. Undetermined impact of patient decision support interventions on healthcare costs and savings: systematic review. BMJ. 2014;348:g188. doi: 10.1136/bmj.g188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wennberg JE. Time to tackle unwarranted variations in practice. BMJ. 2011;342:d1513. doi: 10.1136/bmj.d1513. [DOI] [PubMed] [Google Scholar]
- Zauber AG, Lansdorp-Vogelaar I, Knudsen AB, Wilschut J, van Ballegooijen M, Kuntz KM. Evaluating test strategies for colorectal cancer screening: a decision analysis for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2008;149:659–69. doi: 10.7326/0003-4819-149-9-200811040-00244. [DOI] [PMC free article] [PubMed] [Google Scholar]