Abstract
Background
There is increasing evidence questioning the use of warfarin for atrial fibrillation (AF) among older adults with end stage renal disease (ESRD). We assessed the patterns and determinants of warfarin utilization among these patients in the US.
Methods
We assembled a cohort of older adults (age ≥65) undergoing dialysis with incident AF from July 2007 to November 2011 from the US Renal Data System (USRDS). We used descriptive statistics to characterize warfarin utilization within 30 days of AF discharge, and logistic regression to quantify patient characteristics associated with warfarin initiation.
Results
Among 5730 older adults undergoing dialysis with incident AF, 15.5% initiated warfarin. Among 2906 patients with high risk of bleeding, 12.7% initiated warfarin; whereas 14.9% initiated warfarin among 4824 patients with high risk of stroke. After adjustment for patient characteristics, warfarin initiation was lower among patients who were older [odds ratio (OR) = 0.74 per 10-year increase, 95% confidence interval (CI) 0.66–0.83] and those with a history of diabetes (OR = 0.75, 95% CI 0.63–0.90), myocardial infarction (OR = 0.64, 95% CI 0.50–0.80), or bleeding (OR = 0.63, 95% CI 0.50–0.80). There was no association between sex, race, or dialysis modality and warfarin initiation. Among patients who initiated warfarin, 46.8% discontinued warfarin use after a median treatment length of 8.6 months.
Conclusion
Despite the unclear benefit and increased bleeding risk of warfarin treatment in patients with ESRD, 1 in 8 older adults undergoing dialysis with incident AF in the US who had high risk of bleeding used warfarin. Changes to warfarin therapy due to discontinuation were common after initiation.
Keywords: End stage renal disease, Atrial fibrillation, Anticoagulants, Warfarin, Drug utilization
Introduction
More than one in ten patients with end stage renal disease (ESRD) also has comorbid atrial fibrillation (AF) [1]. The prevalence of AF is greater among older adults on dialysis, ranging from 13.2% among those aged 65 to 74 years to 22.5% among those 85 years or older [2]. Patients with comorbid ESRD and AF are at high risk of poor outcomes such as ischemic stroke, all-cause mortality, myocardial infarction and heart failure compared to patients with ESRD but without AF [3]. In the general population, older patients have a higher risk of thromboembolism, but they derive a greater net clinical benefit from warfarin in terms of protection of thromboembolic events [4].
While warfarin is recommended for prevention of stroke and thromboembolism in the general population with AF who have one or two risk factors for stroke [5–9], experts have raised concerns about the Effectiveness of warfarin treatment in patients with ESRD and AF [10–13]. Recently published systematic reviews and observational studies suggest that warfarin is not beneficial in reducing stroke risk but is associated with increased bleeding risk in patients with AF undergoing dialysis [14–17], especially among older dialysis patients [18, 19]. However, there was some emerging evidence suggesting that warfarin use is associated with a reduction in mortality, even in the absence of a reduction in stroke incidence [20–24].
Given the unclear survival benefit, lack of association with stroke reduction, and increased risk of bleeding associated with warfarin use in patients with ESRD [14–17], clinicians are faced with uncertainty about this treatment decision in this population [25]. Little is known about the use of warfarin in older adults with ESRD, especially about which patients are most likely to initiate this therapy after AF diagnosis and how their utilization changes after initiation. In order to quantify warfarin use and understand the clinical determinants of warfarin treatment in this population, we evaluated the characteristics of warfarin initiation and utilization using a comprehensive national registry of older adults undergoing hemodialysis (HD) and peritoneal dialysis (PD) in the US.
Subjects and methods
Study population and data
We determined the study sample from all available patients in the US Renal Data System (USRDS). We began with a cohort of 9784 older adults aged 65 years or older with ESRD who had an incident AF diagnosis from July 1, 2007 to November 30, 2011. We identified AF by 1 inpatient or 2 outpatient diagnosis codes within 30 days of each other indicating AF (International Classification of Diseases, Ninth Revision [ICD-9] code 427.31) [26]. The study population was limited to patients who: (1) were without pre-existing AF diagnosis from January 1, 1999 to June 30, 2007; (2) had continuous Part A, B, and D coverage from 6 months before through 30 days after AF discharge; (3) had no valvular disease associated with AF in 6 months prior to AF diagnosis [22]; (4) were undergoing HD or PD at the time of AF diagnosis; and (5) had no history of warfarin prescription in 6 months prior to AF diagnosis. After excluding 84 patients with missing Medical Evidence Report (Centers for Medicare & Medicaid Services [CMS] form 2728), the final analytic sample included 5730 older adults with ESRD and incident AF (Appendix Fig. 1). This study was exempted from the full institutional review because the sample was comprised of de-identified secondary data.
Patient characteristics
We gleaned information regarding patients' demographics and dialysis modality from the Medical Evidence Report (Centers for Medicare & Medicaid Services [CMS] form 2728). We ascertained medication history in the 6 months before AF diagnosis from the Medicare prescription claims data. We identified comorbidities from the Medical Evidence Report or previously published ICD-9 based algorithms [27–29] using all available Medicare inpatient claims data [30] (i.e. from January 1, 1999 to AF diagnosis).
Stroke and bleeding risk scores
We calculated the CHA2DS2-VASc [31] and HAS-BLED [32] scores for risk stratification. The CHA2DS2-VASc score (ranges 0 to 9) was calculated by assigning 1 point for the presence of congestive heart failure, hypertension, diabetes mellitus, vascular disease, age 65–74 years, sex category (i.e. female gender), and assigning 2 points to age ≥75 years, and history of stroke/transient ischemic attack/thromboembolism [31]. Since our study population only included older adults, all patients had a minimum CHA2DS2-VASc score of 1 for age.
The HAS-BLED score (ranges 0 to 9) was calculated by assigning 1 point for the presence of hypertension, abnormal renal function, abnormal liver function, stroke, bleeding history, elderly (>65 years), concomitant drug use, and alcohol abuse [32]. Since labile international normalized ratio (INR) information was not available from the USRDS database, this factor was not included in our calculation [33]. Additionally, our study population included older adults undergoing dialysis; therefore, all patients had a minimum score of 2 for age and abnormal kidney function, and a maximum score of 8 due to lack of INR information.
We modified both the CHA2DS2-VASc and HAS-BLED risk categories, whereby a score of 1 corresponded to low, 2–3 corresponded to intermediate, and 4–8 corresponded to high risk. We adjusted the score cut points, because no older adult dialysis patients had a CHA2DS2-VASc score of 0 due to age, or a HAS-BLED score of 0–1 due to age and abnormal kidney function.
Warfarin initiation
We identified claims for warfarin using Medicare Part D claims of filled prescriptions. We defined warfarin initiation as any warfarin prescription claims within 30 days of AF discharge (i.e. date of discharge for patients who had a one inpatient diagnosis of AF or date of first diagnosis for patients who had two or more diagnoses of AF), and non-initiation as the absence of a warfarin prescription claims within 30 days of AF discharge. We then calculated the proportion of dialysis patients with warfarin initiation among the cohort of older adults undergoing dialysis with newly diagnosed AF, and by CHA2DS2-VASc and HAS-BLED risk categories.
Warfarin utilization
We described medication utilization characteristics including number of warfarin prescriptions per user, total quantity dispensed per user, and total days of supply per user for those who initiated warfarin between AF discharge and the end of follow-up (the earliest day of death date, first kidney transplantation date, loss of Medicare coverage, or December 31, 2011).
We also assessed medication utilization measures such as discontinuation and switching. For these analyses, we excluded patients who were diagnosed with AF on or after October 1, 2011 to ensure patients analyzed had enough follow up to assess discontinuation or switching. We defined discontinuation as no additional refill for warfarin within 60 days after the end of days of supply of warfarin prescription. We defined switching as any dabigatran, rivaroxaban, or apixaban prescription between the initial warfarin prescription date and the end of follow-up for those who initiated warfarin, and as any warfarin prescription between 30 days after AF discharge and the end of follow-up for those who did not initiate warfarin.
Statistical analysis for association of patient characteristics with warfarin initiation
We described patient characteristics using median and interquartile range (IQR) for continuous variables, and counts and proportions for categorical variables. We compared the patient characteristics of warfarin initiators and non-warfarin initiators, and tested the difference using the two-sample t-test for continuous variables and the Pearson Chi square test for categorical variables. We calculated the proportion of warfarin initiators by CHA2DS2-VASc and HAS-BLED risk categories. We tested the independent associations of demographic, dialysis, and clinical factors with warfarin initiation by fitting multiple logistic regression models and reported the odds ratio (OR) and 95% confidence interval (CI). We selected the most parsimonious model by backward stepwise selection based on lowest the Akaike information criterion, and assessed the model fit by the Hosmer–Lemeshow goodness-of-ft test. We performed similar analyses among the older PD patients with incident AF. All statistical analyses were performed using Stata 14.0 (StataCorp, College Station, TX).
Sensitivity analysis
We conducted two sensitivity analyses using alternate definition of initiation and discontinuation. First, we defined warfarin initiation as any prescription within 60 days of AF discharge instead of 30 days. Second, we defined warfarin discontinuation using a gap of 30 days instead of 60 days for no refill after the end of days' supply. We also conducted an additional sensitivity analysis to assess the determinants of warfarin initiation excluding patients identified by a single inpatient diagnosis of AF.
Results
Study population
We identified 5730 older adults undergoing HD or PD who were newly diagnosed with AF from July 1, 2007 to November 30, 2011 (Table 1). These patients had a median age of 74 years (IQR 69–80) at AF diagnosis and had a median time on dialysis of 3.9 years (IQR 2.3–5.9); 56.8% were female and 62.7% were white. A history of comorbid conditions was common: 21.6% had cerebrovascular disease, 71.5% had diabetes mellitus, 68.8% had congestive heart failure, and 98.6% had hypertension.
Table 1. Characteristics of older adults (≥ 65 years) undergoing dialysis with newly diagnosed atrial fibrillation by warfarin initiation.
| Patient characteristics | Total (N = 5730) | Non-initiators (n = 4842) | Warfarin initiators (n = 888) | P-value1 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Demographics | ||||||||||
| Age at AF diagnosis, median (IQR) | 74 (69–80) | 74 (69–80) | 73 (69–78) | <0.001 | ||||||
| Year of AF diagnosis, n (%) | 0.76 | |||||||||
| 2007 | 1,352 (23.6) | 1,150 (23.8) | 202 (22.8) | |||||||
| 2008 | 1,564 (27.3) | 1,315 (27.2) | 249 (28.0) | |||||||
| 2009 | 1,211 (21.1) | 1,021 (21.1) | 190 (21.4) | |||||||
| 2010 | 1,029 (18.0) | 873 (18.0) | 156 (17.6) | |||||||
| 2011 | 574 (10.0) | 483 (10.0) | 91 (10.2) | |||||||
| Female sex, n (%) | 3,252 (56.8) | 2,752 (56.8) | 500 (56.3) | 0.77 | ||||||
| Race, n (%) | 0.03 | |||||||||
| White | 3,593 (62.7) | 3,008 (62.1) | 585 (65.9) | |||||||
| Non-white | 2,137 (37.3) | 1,834 (37.9) | 303 (34.1) | |||||||
| Hispanic, n (%) | 1,081 (18.8) | 914 (18.9) | 167 (18.8) | 0.96 | ||||||
| Geographic region, n (%) | 0.003 | |||||||||
| Northeast | 1,011 (17.6) | 837 (17.3) | 174 (19.6) | |||||||
| Midwest | 1,199 (20.9) | 982 (20.3) | 217 (24.4) | |||||||
| South | 2,531 (44.2) | 2167 (44.8) | 364 (41.0) | |||||||
| West | 989 (17.3) | 856 (17.7) | 133 (15.0) | |||||||
| Dialysis factors | ||||||||||
| Dialysis vintage, median (IQR) | 3.9 (2.3–5.9) | 3.9 (2.3–5.9) | 3.8 (2.3–5.9) | 0.51 | ||||||
| Modality, n (%) | ||||||||||
| Hemodialysis | 5,539 (96.7) | 4,686 (96.8) | 853 (96.1) | 0.34 | ||||||
| Peritoneal dialysis | 191 (3.3) | 156 (3.2) | 35 (3.9) | |||||||
| History of medication use | ||||||||||
| Anticoagulant agent | 36 (0.6) | 28 (0.6) | 8 (0.9) | 0.26 | ||||||
| Antiplatelet agent | 1,452 (25.3) | 1,221 (25.2) | 231 (26.0) | 0.62 | ||||||
| Beta-Blocker | 2,499 (43.6) | 2,116 (43.7) | 383 (43.1) | 0.75 | ||||||
| Calcium channel blocker | 2,721 (47.5) | 2,282 (47.1) | 439 (49.4) | 0.21 | ||||||
| Calcium acetate | 1,818 (31.7) | 1,542 (31.8) | 276 (31.1) | 0.65 | ||||||
| Central acting agonist | 939 (16.4) | 804 (16.6) | 135 (15.2) | 0.30 | ||||||
| Diuretic | 1,172 (20.4) | 996 (20.6) | 176 (19.8) | 0.61 | ||||||
| Lipid-lowering agent, nonstatin | 453 (7.9) | 381 (7.9) | 72 (8.1) | 0.81 | ||||||
| Nitrate | 1,335 (23.3) | 1,135 (23.4) | 200 (22.5) | 0.55 | ||||||
| NSAID | 519 (9.1) | 446 (9.2) | 73 (8.2) | 0.34 | ||||||
| PPI or H2-blocker | 2,744 (47.9) | 2,353 (48.6) | 391 (44.0) | 0.01 | ||||||
| Sevelamer | 2,449 (42.7) | 2,065 (42.6) | 384 (43.2) | 0.74 | ||||||
| Statin | 2,634 (46.0) | 2,204 (45.5) | 430 (48.4) | 0.11 | ||||||
| History of comorbid conditions, n (%) | ||||||||||
| Alcohol dependence | 47 (0.8) | 40 (0.8) | 7 (0.8) | 0.91 | ||||||
| Concomitant use of antiplatelets or NSAIDs | 916 (16.0) | 771 (15.9) | 145 (16.3) | 0.76 | ||||||
| Tobacco use | 693 (12.1) | 597 (12.3) | 96 (10.8) | 0.20 | ||||||
| Cancer (excl. non-melanoma skin cancer) | 893 (15.6) | 764 (15.8) | 129 (14.5) | 0.34 | ||||||
| Cerebrovascular disease | 1,235 (21.6) | 1,073 (22.2) | 162 (18.2) | 0.01 | ||||||
| Ischemic heart disease | 3,793 (66.2) | 3,230 (66.7) | 563 (63.4) | 0.06 | ||||||
| Diabetes mellitus | 4,096 (71.5) | 3,498 (72.2) | 598 (67.3) | 0.003 | ||||||
| Congestive heart failure | 3,942 (68.8) | 3,366 (69.5) | 576 (64.9) | 0.01 | ||||||
| Hypertension | 5,651 (98.6) | 4,780 (98.7) | 871 (98.1) | 0.14 | ||||||
| Peripheral vascular disease | 2,413 (42.1) | 2,053 (42.4) | 360 (40.5) | 0.30 | ||||||
| Pulmonary disease | 2,089 (36.5) | 1,786 (36.9) | 303 (34.1) | 0.12 | ||||||
| Liver disease | 443 (7.7) | 402 (8.3) | 41 (4.7) | <0.001 | ||||||
| Myocardial infarction | 908 (15.8) | 812 (16.8) | 96 (10.8) | <0.001 | ||||||
| Ischemic stroke/TIA/TE history | 757 (13.2) | 668 (13.8) | 89 (10.0) | 0.002 | ||||||
| Bleeding history | 1,691 (29.5) | 1,505 (31.1) | 186 (21.0) | <0.001 | ||||||
| Risk scores | ||||||||||
| CHA2DS2-VASc2 | 0.03 | |||||||||
| Low | 10 (0.2) | 8 (0.2) | 2 (0.2) | |||||||
| Intermediate | 896 (15.6) | 730 (15.1) | 166 (18.7) | |||||||
| High | 4,824 (84.2) | 4,104 (84.8) | 720 (81.1) | |||||||
| HAS-BLED2 | <0.001 | |||||||||
| Low | 0 | 0 | 0 | |||||||
| Intermediate | 2,824 (49.3) | 2,306 (47.6) | 518 (58.3) | |||||||
| High | 2,906 (50.7) | 2,536 (52.4) | 370 (41.7) | |||||||
P-value is calculated from two-sample t-test for continuous variables and from Pearson Chi square test for categorical variables
Low corresponds to CHA2DS2-VASc or HAS-BLED score 1; intermediate corresponds to CHA2DS2-VASc or HAS-BLED score 2–3; high corresponds to CHA2DS2-VASc 4–9 or HAS-BLED score 4–8
Warfarin initiation patterns
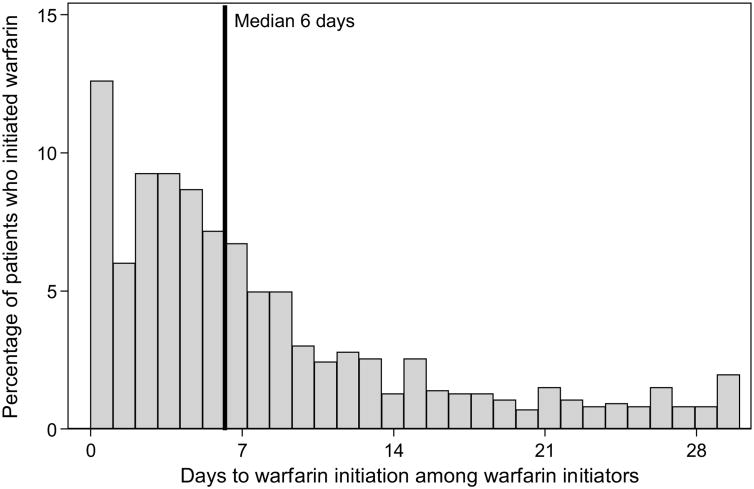
Among these 5730 patients, 15.5% initiated warfarin within 30 days of AF discharge. Half of those who initiated warfarin did so in the first week after AF discharge (median 6 days, IQR 3–11) (Fig. 1). Warfarin initiators tended to be healthier than non-initiators, with lower median age at AF diagnosis (73 vs 74 years, P < 0.001), lower rates of liver disease (4.7 vs 8.3%, P < 0.001), myocardial infarction (10.8 vs 16.8%, P < 0.001), ischemic stroke/TIA/TE history (10.0 vs 13.8%, P = 0.002) and bleeding history (21.0% vs 31.1%, P < 0.001) (Table 1).
Fig. 1.
Time to warfarin initiation among older adults (≥65 years) undergoing dialysis within 30 days of atrial fibrillation discharge
Warfarin initiation by CHA2DS2-VASc and HAS-BLED risk categories
The CHA2DS2-VASc and HAS-BLED scores were statistically different between warfarin initiators and non-initiators (Table 1). Among 4824 patients with high risk of stroke predicted by CHA2DS2-VASc score, 14.9% were warfarin initiators (Table 2). Among 2906 patients with high risk of bleeding predicted by HAS-BLED score, 12.7% were warfarin initiators.
Table 2. Warfarin initiation by CHA2DS2-VASc and HAS-BLED risk score categories among older adults (≥65 years) undergoing dialysis with newly diagnosed atrial fibrillation.
| CHA2DS2-VASc category1 | HAS-BLED category1 | Total | ||
|---|---|---|---|---|
|
| ||||
| Low (n = 0) | Intermediate (n = 2824) | High (n = 2906) | ||
| Low (n = 10) | 0 | 20.0 | 0 | 20.0 |
| Intermediate (n = 896) | 0 | 20.5 | 15.2 | 18.5 |
| High (n = 4,824) | 0 | 17.8 | 12.4 | 14.9 |
| Total | 0 | 18.3 | 12.7 | 15.5 |
Numbers in the table are cell percentage (%)
Low corresponds to CHA2DS2-VASc or HAS-BLED score 1; intermediate corresponds to CHA2DS2-VASc or HAS-BLED score 2–3; high corresponds to CHA2DS2-VASc 4–9 or HAS-BLED score 4–8
Independent association of patient characteristics with warfarin initiation
After adjustment for other patient characteristics, age (OR 0.745 per 10-year increase, 95% CI 0.66–0.83), but not sex (OR 1.00, 95% CI 0.85–1.17), race (OR 0.88, 95% CI 0.75–1.03) or dialysis modality (OR 1.05, 95% CI 0.72–1.54), was independently associated with warfarin initiation (Table 3). Patients with diabetes (OR 0.75, 95% CI 0.63–0.90), liver disease (OR 0.58, 95% CI 0.41–0.83), myocardial infarction (OR 0.64, 95% CI 0.50–0.80), stroke history (OR 0.76, 95% CI 0.58-1.00) and bleeding history (OR 0.63, 95% CI 0.50–0.80) were significantly less likely to initiate warfarin. Among PD patients, 18.3% initiated warfarin within 30 days of AF diagnosis. None of the patient characteristics was independently associated with warfarin initiation in the subset of 178 patients. (Appendix Table 1).
Table 3. Adjusted association of patient characteristics with warfarin initiation among older adults (≥65 years) undergoing dialysis, who initiated warfarin within 30 days of atrial fibrillation discharge.
| Patient characteristics | Warfarin initiation (OR, 95% CI) |
|---|---|
| Age at AF diagnosis, per 10-year increase | 0.74 (0.66–0.83) |
| Year of AF diagnosis | |
| 2007 | Ref |
| 2008 | 1.19 (0.97–1.46) |
| 2009 | 1.24 (1.00–1.55) |
| 2010 | 1.24 (0.98–1.57) |
| 2011 | 1.46 (1.10–1.93) |
| Sex | |
| Male | Ref |
| Female | 1.00 (0.85–1.17) |
| Race | |
| White | Ref |
| Non-white | 0.88 (0.75–1.03) |
| Dialysis modality | |
| Hemodialysis | Ref |
| Peritoneal dialysis | 1.05 (0.72–1.54) |
| Geographic region | |
| Northeast | Ref |
| Midwest | 1.04 (0.83–1.30) |
| South | 0.78 (0.64–0.96) |
| West | 0.70 (0.54–0.90) |
| History of medication use | |
| Anticoagulant agent | 1.82 (0.81–4.08) |
| PPI or H2-blocker | 0.87 (0.75–1.01) |
| Statin | 1.20 (1.03–1.39) |
| History of comorbid conditions | |
| Tobacco use | 0.81 (0.64–1.02) |
| Diabetes mellitus | 0.75 (0.63–0.90) |
| Liver disease | 0.58 (0.41–0.83) |
| Myocardial infarction | 0.64 (0.50–0.80) |
| Stroke/TIA/TE history | 0.76 (0.58-1.00) |
| Bleeding history | 0.63 (0.50–0.80) |
| Risk scores | |
| CHA2DS2-VASc risk category | |
| Low and Intermediate | Ref |
| High | 1.07 (0.84–1.36) |
| HAS-BLED risk category | |
| Intermediate | Ref |
| High | 0.95 (0.76–1.18) |
Warfarin utilization patterns
Warfarin initiators had a median of 6 (IQR 2–14) warfarin prescriptions, covering a median of 231 (IQR 90–532) days of supply (Table 4). Among warfarin initiators, 46.8% discontinued warfarin after a median duration of 257 days (IQR 165–444) after the initial warfarin prescription (Table 4). Only 0.5% warfarin initiators switched to dabigatran, and 15.4% patients who did not used warfarin initially started warfarin use after a median duration of 149 days (IQR 66–358).
Table 4. Warfarin utilization among older adults (≥65 years) undergoing dialysis with newly diagnosed atrial fibrillation, who initiated warfarin within 30 days of atrial fibrillation discharge.
| Warfarin initiators | |
|---|---|
| Medication utilization characteristics | |
| Number of warfarin prescriptions per user, median (IQR) | 6 (2–14) |
| Total quantity dispensed per user, median (IQR) | 231 (90–532) |
| Total days of supply per user, median (IQR) | 180 (63–460) |
| Medication utilization measures | |
| Discontinuation, % | 46.8 |
| Median time to discontinuation, days, median (IQR) | 257 (165–444) |
| Switching to dabigatran, rivaroxaban, apixaban, % | 0.5 |
Sensitivity analysis
In the sensitivity analysis of warfarin initiation using 60 day for initiation period, we excluded 44 patients diagnosed with AF between November 1 and November 30, 2011. Among 5,686 older adults on dialysis, 17.3% initiated warfarin prescription within 60 days of AF discharge. Similar to the primary analysis, patient age and year of AF diagnosis were significantly associated with warfarin initiation (Appendix Table 2). In the sensitivity analysis of discontinuation using 30 days instead of 60 days as discontinuation window, 60.1% of warfarin initiators discontinued warfarin after a median duration of 194 days (IQR 125–335). In the sensitivity analysis excluding 408 patients with a single diagnosis of AF, 16.5% initiated warfarin within 30 days after AF discharge and 45.8% of them discontinued warfarin after a median of 166 days (IQR 259–446). Similar to the main analysis, patients age (OR 0.73, 95% CI 0.64–0.82), diabetes (OR 0.76, 95% CI 0.64–0.92), liver disease (OR 0.61, 95% CI 0.43–0.87), myocardial infarction (OR 0.60, 95% CI 0.48–0.76) and bleeding history (OR 0.61, 95% CI 0.48–0.77) were negatively associated with warfarin initiation, whereas CHA2DS2-VASc and HAS-BLED scores were not associated (Appendix Table 3).
Discussion
In this national study of older adults with ESRD and newly diagnosed AF, nearly one in six initiated warfarin prescription within 30 days of their discharge. Patient characteristics such as age and geographic region, as well as comorbid conditions including diabetes, liver disease, myocardial infarction, and bleeding history, were independently associated with warfarin initiation. Half of warfarin initiators discontinued use of warfarin after a median treatment length of 8.6 months.
Although several studies have examined the characteristics of patients using warfarin for AF in the US, these studies tended to focus on the general population [34] or older adults with AF not on dialysis [35, 36]. We found the overall proportion of warfarin initiation was 15.5%, which was the same as that (15%) among US adults with AF on HD reported by Shen et al. [22]. We found that bleeding history was inversely associated with warfarin initiation, but bleeding risk score and stroke risk score were not associated after adjustment for other patient characteristics. Genovesi et al. found that previous bleedings and hemorrhagic risk score was inversely related to warfarin use, but stroke risk score was not associated with warfarin use [37]. Such discrepancy might be due to differences in the study population and the definition of warfarin use: Genovesi et al. studied a mixed population of new and chronic warfarin among chronic HD patients with AF in Italy [37], whereas we studied new users among older adults undergoing HD or PD with incident AF in the US.
We found that several predictors of stroke risk including advanced age, history of diabetes and myocardial infarction were inversely associated with warfarin initiation, which differed from Genovesi et al.'s observation that these factors were not significantly associated with warfarin prescription [37]. The magnitude of these factors reported by Genovesi et al. were in the same direction as ours (i.e. OR < 1), but they may lacked statistical power to detect significant associations due to small sample size (N = 290). Given the high prevalence of frailty among HD patients [38, 39], and the high risk of adverse outcomes such as falls in this population [40, 41], physicians are reluctant to prescribe warfarin [25].
Among PD patients, we observed that warfarin was used among 18.3% older patients on PD, higher than that (15.4%) among older patients on HD; however, dialysis modality was not a significant predictor of warfarin initiation. In addition to warfarin initiation, we extended the previous findings by assessing utilization measures such as discontinuation and switching. We found that 46.8% warfarin initiators discontinued use, which was higher than that in the general population with AF (41.5%) reported by Nelson et al. [34].
Our study has several limitations. First, we determined warfarin treatment based on prescription claims, which indicates how medications were dispensed rather than how patients consumed the medications. Due to inherent limitations of claims analysis, we could not rule out the presence of unmeasured confounding such as factors affecting physicians' prescribing behaviors, other indications for warfarin use, or over-the-counter medication use. Secondly, information such as the type of AF (persistent or paroxysmal) and INR values was lacking due to inherent limitations of administrative claims, so we were not able to study how these factors influence warfarin prescription. Although the presence of AF was not directly documented, we tried to minimize the misclassification bias by using a previously validated algorithm to identify AF [22, 26]. Finally, we used a dummy variable approach instead of a multilevel model to examine factors associated with warfarin initiation. We did not assess whether such relationships vary across group-level factors because we were mainly interested in individual-level factors.
Our study has strengths in that we studied the patterns and determinants of warfarin initiation among a national cohort of older adults with AF undergoing dialysis. To our knowledge, our study is the first to describe the detailed utilization characteristics of warfarin initiation after AF diagnosis in this vulnerable population. Identifying the initiation and utilization patterns of warfarin among older adults with AF undergoing dialysis is a first step in understanding the real world practice of stroke prophylaxis in this under-studied population, which could help inform future studies in evaluating the benefits and risks of warfarin treatment.
Our findings suggest that warfarin was initiated among 15.5% older adults undergoing dialysis within 30 days of AF discharge, even among 12.7% of those with high bleeding risk. Patients' age, history of diabetes, liver disease, myocardial infarction, or bleeding were significantly associated with warfarin initiation. Warfarin was discontinued among 46.8% of those who initiated warfarin after 8.6 months, reflecting the challenges in warfarin management requiring careful monitoring and dosage adjustment. In light of the increasing number of older dialysis patients with AF and the unclear clinical benefit of warfarin treatment, more research is needed to determine the complex interplay of factors that affect AF epidemiology, warfarin use, and outcomes in this vulnerable population.
Supplementary Material
Acknowledgments
The data reported here have been supplied by the United States Renal Data System (USRDS). The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy or interpretation of the U.S. government. This research was supported by the National Heart, Lung, and Blood Institute (T32HL007024) pre-doctoral training grant and the doctoral dissertation fund provided by the Johns Hopkins Bloomberg School of Public Health Department of Epidemiology. Jodi B. Segal was supported by the National Institute on Aging (K24AG049036). Mara McAdams-DeMarco was supported by the American Society of Nephrology Carl W. Gottschalk Research Scholar Grant and Johns Hopkins University Claude D. Pepper Older Americans Independence Center, and the National Institute on Aging (P30AG021334 and K01AG043501). Dorry Segev was supported by the National Institute for Diabetes and Digestive and Kidney Disorders (K24DK101828). The funding sources had no role in the design and conduct of the study, analysis, or interpretation of the data; and preparation or final approval of the manuscript prior to publication.
Abbreviations
- ESRD
End stage renal disease
- AF
Atrial fibrillation
- CI
Confdence interval
- OR
Odds ratio
- IQR
Interquartile range
- INR
International normalized ratio
Footnotes
Electronic supplementary material: The online version of this article (doi:10.1007/s40620-016-0374-6) contains supplementary material, which is available to authorized users.
Compliance with Ethical Standards: Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest: G. Caleb Alexander is Chair of the FDA's Peripheral and Central Nervous System Advisory Committee; serves as a paid consultant to PainNavigator, a mobile startup to improve patients' pain management; serves as a paid consultant to IMS Health; and serves on an IMS Health scientific advisory board. This arrangement has been reviewed and approved by Johns Hopkins University in accordance with its conflict of interest policies.
Statement of human rights: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: For this type of retrospective study using anonymous registry data, formal consent is not required.
References
- 1.Zimmerman D, Sood MM, Rigatto C, Holden RM, Hiremath S, Clase CM. Systematic review and meta-analysis of incidence, prevalence and outcomes of atrial fibrillation in patients on dialysis. Nephrol Dial Transplant. 2012;27(10):3816–3822. doi: 10.1093/ndt/gfs416. [DOI] [PubMed] [Google Scholar]
- 2.Winkelmayer WC, Patrick AR, Liu J, Brookhart MA, Setoguchi S. The increasing prevalence of atrial fibrillation among hemodialysis patients. J Am Soc Nephrol. 2011;22(2):349–357. doi: 10.1681/ASN.2010050459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shih CJ, Ou SM, Chao PW, Kuo SC, Lee YJ, Yang CY, Tarng DC, Lin CC, Huang PH, Li SY, et al. Risks of death and stroke in patients undergoing hemodialysis with new-onset atrial fibrillation: a competing-risk analysis of a nationwide cohort. Circulation. 2016;133(3):265–272. doi: 10.1161/CIRCULATIONAHA.115.018294. [DOI] [PubMed] [Google Scholar]
- 4.Singer DE, Chang Y, Fang MC, Borowsky LH, Pomernacki NK, Udaltsova N, Go AS. The net clinical benefit of warfarin anticoagulation in atrial fibrillation. Ann Intern Med. 2009;151(5):297–305. doi: 10.7326/0003-4819-151-5-200909010-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fuster V, Ryden LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, Halperin JL, Kay GN, Le Huezey JY, Lowe JE, et al. 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2011;123(10):e269–e367. doi: 10.1161/CIR.0b013e318214876d. [DOI] [PubMed] [Google Scholar]
- 6.You JJ, Singer DE, Howard PA, Lane DA, Eckman MH, Fang MC, Hylek EM, Schulman S, Go AS, Hughes M, et al. Antithrombotic therapy for atrial fibrillation: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e531S–e575 S. doi: 10.1378/chest.11-2304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC, Jr, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):e199–e267. doi: 10.1161/CIR.0000000000000041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Atrial fibrillation: the management of atrial fibrillation. http://guidance.nice.org.uk/CG180.
- 9.Verma A, Cairns JA, Mitchell LB, Macle L, Stiell IG, Gladstone D, McMurtry MS, Connolly S, Cox JL, Dorian P, et al. 2014 focused update of the Canadian Cardiovascular Society Guidelines for the management of atrial fibrillation. Can J Cardiol. 2014;30(10):1114–1130. doi: 10.1016/j.cjca.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 10.Bennett WM. Should dialysis patients ever receive warfarin and for what reasons? Clin J Am Soc Nephrol. 2006;1(6):1357–1359. doi: 10.2215/CJN.01700506. [DOI] [PubMed] [Google Scholar]
- 11.Sood MM, Komenda P, Sood AR, Rigatto C, Bueti J. The intersection of risk and benefit: is warfarin anticoagulation suitable for atrial fibrillation in patients on hemodialysis? Chest. 2009;136(4):1128–1133. doi: 10.1378/chest.09-0730. [DOI] [PubMed] [Google Scholar]
- 12.Shen JI, Turakhia MP, Winkelmayer WC. Anticoagulation for atrial fibrillation in patients on dialysis: are the benefits worth the risks? Curr Opin Nephrol Hypertens. 2012;21(6):600–606. doi: 10.1097/MNH.0b013e32835856fd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang F, Chou D, Schweitzer P, Hanon S. Warfarin in haemodialysis patients with atrial fibrillation: what benefit? Europace. 2010;12(12):1666–1672. doi: 10.1093/europace/euq387. [DOI] [PubMed] [Google Scholar]
- 14.Li J, Wang L, Hu J, Xu G. Warfarin use and the risks of stroke and bleeding in hemodialysis patients with atrial fibrillation: a systematic review and a meta-analysis. Nutr Metab Cardiovasc Dis. 2015 doi: 10.1016/j.numecd.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 15.Liu G, Long M, Hu X, Hu CH, Liao XX, Du ZM, Dong YG. Effectiveness and safety of warfarin in dialysis patients with atrial fibrillation: a meta-analysis of observational studies. Medicine (Baltimore) 2015;94(50):e2233. doi: 10.1097/MD.0000000000002233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee M, Saver JL, Hong KS, Wu YL, Huang WH, Rao NM, Ovbiagele B. Warfarin use and risk of stroke in patients with atrial fibrillation undergoing hemodialysis: a meta-analysis. Medicine (Baltimore) 2016;95(6):e2741. doi: 10.1097/MD.0000000000002741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tan J, Liu S, Segal JB, Alexander GC, McAdams-DeMarco M. Warfarin use and stroke, bleeding and mortality risk in patients with end stage renal disease and atrial fibrillation: a systematic review and meta-analysis. BMC Nephrol. 2016;17(1):157. doi: 10.1186/s12882-016-0368-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shah M, Avgil Tsadok M, Jackevicius CA, Essebag V, Eisenberg MJ, Rahme E, Humphries KH, Tu JV, Behlouli H, Guo H, et al. Warfarin use and the risk for stroke and bleeding in patients with atrial fibrillation undergoing dialysis. Circulation. 2014;129(11):1196–1203. doi: 10.1161/CIRCULATIONAHA.113.004777. [DOI] [PubMed] [Google Scholar]
- 19.Winkelmayer WC, Liu J, Setoguchi S, Choudhry NK. Effectiveness and safety of warfarin initiation in older hemodialysis patients with incident atrial fibrillation. Clin J Am Soc Nephrol. 2011;6(11):2662–2668. doi: 10.2215/CJN.04550511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carrero JJ, Evans M, Szummer K, Spaak J, Lindhagen L, Edfors R, Stenvinkel P, Jacobson SH, Jernberg T. Warfarin, kidney dysfunction, and outcomes following acute myocardial infarction in patients with atrial fibrillation. JAMA. 2014;311(9):919–928. doi: 10.1001/jama.2014.1334. [DOI] [PubMed] [Google Scholar]
- 21.Bonde AN, Lip GY, Kamper AL, Hansen PR, Lamberts M, Hommel K, Hansen ML, Gislason GH, Torp-Pedersen C, Olesen JB. Net clinical benefit of antithrombotic therapy in patients with atrial fibrillation and chronic kidney disease: a nationwide observational cohort study. J Am Coll Cardiol. 2014;64(23):2471–2482. doi: 10.1016/j.jacc.2014.09.051. [DOI] [PubMed] [Google Scholar]
- 22.Shen JI, Montez-Rath ME, Lenihan CR, Turakhia MP, Chang TI, Winkelmayer WC. Outcomes after warfarin initiation in a cohort of hemodialysis patients with newly diagnosed atrial fibrillation. Am J Kidney Dis. 2015 doi: 10.1053/j.ajkd.2015.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brancaccio D, Neri L, Bellocchio F, Barbieri C, Amato C, Mari F, Canaud B, Stuard S. Patients' Characteristics Affect the Survival Benefit of Warfarin Treatment for Hemodialysis Patients with Atrial Fibrillation. A Historical Cohort Study. Am J Nephrol. 2016;44(4):258–267. doi: 10.1159/000448898. [DOI] [PubMed] [Google Scholar]
- 24.Genovesi S, Rebora P, Gallieni M, Stella A, Badiali F, Conte F, Pasquali S, Bertoli S, Ondei P, Bonforte G, et al. Effect of oral anticoagulant therapy on mortality in end-stage renal disease patients with atrial fibrillation: a prospective study. J Nephrol. 2016 doi: 10.1007/s40620-016-0364-8. [DOI] [PubMed] [Google Scholar]
- 25.Juma S, Thomson BK, Lok CE, Clase CM, Blake PG, Moist L. Warfarin use in hemodialysis patients with atrial fibrillation: decisions based on uncertainty. BMC Nephrol. 2013;14:174. doi: 10.1186/1471-2369-14-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jensen PN, Johnson K, Floyd J, Heckbert SR, Carnahan R, Dublin S. A systematic review of validated methods for identifying atrial fibrillation using administrative data. Pharmacoepidemiol Drug Saf. 2012;21(1):141–147. doi: 10.1002/pds.2317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chronic Conditions Data Warehouse. https://www.ccwdata.org/web/guest/condition-categories.
- 28.Cunningham A, Stein CM, Chung CP, Daugherty JR, Smalley WE, Ray WA. An automated database case definition for serious bleeding related to oral anticoagulant use. Pharmacoepidemiol Drug Saf. 2011;20(6):560–566. doi: 10.1002/pds.2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kokotailo RA, Hill MD. Coding of stroke and stroke risk factors using international classification of diseases, revisions 9 and 10. Stroke. 2005;36(8):1776–1781. doi: 10.1161/01.STR.0000174293.17959.a1. [DOI] [PubMed] [Google Scholar]
- 30.Brunelli SM, Gagne JJ, Huybrechts KF, Wang SV, Patrick AR, Rothman KJ, Seeger JD. Estimation using all available covariate information versus a fixed look-back window for dichotomous covariates. Pharmacoepidemiol Drug Saf. 2013;22(5):542–550. doi: 10.1002/pds.3434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137(2):263–272. doi: 10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- 32.Pisters R, Lane DA, Nieuwlaat R, De Vos CB, Crijns HJGM, Lip GYH. A novel user-friendly score to assess one-year risk of major bleeding in atrial fibrillation patients: the Euro Heart-Survey. Eur Heart J. 2010;31:923. doi: 10.1378/chest.10-0134. [DOI] [PubMed] [Google Scholar]
- 33.Abraham NS, Singh S, Alexander GC, Heien H, Haas LR, Crown W, Shah ND. Comparative risk of gastrointestinal bleeding with dabigatran, rivaroxaban, and warfarin: population based cohort study. Bmj. 2015;350:h1857. doi: 10.1136/bmj.h1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nelson WW, Song X, Coleman CI, Thomson E, Smith DM, Damaraju CV, Schein JR. Medication persistence and discontinuation of rivaroxaban versus warfarin among patients with non-valvular atrial fibrillation. Curr Med Res Opin. 2014;30(12):2461–2469. doi: 10.1185/03007995.2014.933577. [DOI] [PubMed] [Google Scholar]
- 35.Choudhry NK, Soumerai SB, Normand SL, Ross-Degnan D, Laupacis A, Anderson GM. Warfarin prescribing in atrial fibrillation: the impact of physician, patient, and hospital characteristics. Am J Med. 2006;119(7):607–615. doi: 10.1016/j.amjmed.2005.09.052. [DOI] [PubMed] [Google Scholar]
- 36.Raji MA, Lowery M, Lin YL, Kuo YF, Baillargeon J, Goodwin JS. National utilization patterns of warfarin use in older patients with atrial fibrillation: a population-based study of Medicare Part D beneficiaries. Ann Pharmacother. 2013;47(1):35–42. doi: 10.1345/aph.1R515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Genovesi S, Rossi E, Pogliani D, Gallieni M, Stella A, Badiali F, Conte F, Pasquali S, Bertoli S, Ondei P, et al. The nephrologist's anticoagulation treatment patterns/regimens in chronic hemodialysis patients with atrial fibrillation. J Nephrol. 2014;27(2):187–192. doi: 10.1007/s40620-013-0030-3. [DOI] [PubMed] [Google Scholar]
- 38.Salter ML, Gupta N, Massie AB, McAdams-DeMarco MA, Law AH, Jacob RL, Gimenez LF, Jaar BG, Walston JD, Segev DL. Perceived frailty and measured frailty among adults undergoing hemodialysis: a cross-sectional analysis. BMC Geriatr. 2015;15:52. doi: 10.1186/s12877-015-0051-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McAdams-DeMarco MA, Tan J, Salter ML, Gross A, Meoni LA, Jaar BG, Kao WH, Parekh RS, Segev DL, Sozio SM. Frailty and cognitive function in incident hemodialysis patients. Clin J Am Soc Nephrol. 2015;10(12):2181–2189. doi: 10.2215/CJN.01960215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McAdams-DeMarco MA, Law A, Salter ML, Boyarsky B, Gimenez L, Jaar BG, Walston JD, Segev DL. Frailty as a novel predictor of mortality and hospitalization in individuals of all ages undergoing hemodialysis. J Am Geriatr Soc. 2013;61(6):896–901. doi: 10.1111/jgs.12266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McAdams-DeMarco MA, Suresh S, Law A, Salter ML, Gimenez LF, Jaar BG, Walston JD, Segev DL. Frailty and falls among adult patients undergoing chronic hemodialysis: a prospective cohort study. BMC Nephrol. 2013;14:224. doi: 10.1186/1471-2369-14-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.