Abstract
Background
Organ failure increases mortality in patients with liver cirrhosis. Data about resuscitated cardiac arrest patients with liver cirrhosis are missing. This study aims to assess aetiology, survival and functional outcome in patients after successful cardiopulmonary resuscitation (CPR) with and without liver cirrhosis.
Methods
Analysis of prospectively collected cardiac arrest registry data of consecutively hospital-admitted patients following successful CPR was performed. Patient’s characteristics, admission diagnosis, severity of disease, course of disease, short- and long-term mortality as well as functional outcome were assessed and compared between patients with and without cirrhosis.
Results
Out of 1068 patients with successful CPR, 47 (4%) had liver cirrhosis. Acute-on-chronic liver failure (ACLF) was present in 33 (70%) of these patients on admission, and four patients developed ACLF during follow-up. Mortality at 1 year was more than threefold increased in patients with liver cirrhosis (OR 3.25; 95% CI 1.33–7.96). Liver cirrhosis was associated with impaired neurological outcome (OR for a favourable cerebral performance category: 0.13; 95% CI 0.04–0.36). None of the patients with Child–Turcotte–Pugh (CTP) C cirrhosis survived 28 days with good neurological outcome. Overall nine (19%) patients with cirrhosis survived 28 days with good neurological outcome. All patients with ACLF grade 3 died within 28 days.
Conclusion
Cardiac arrest survivors with cirrhosis have worse outcome than those without. Although one quarter of patients with liver cirrhosis survived longer than 28 days after successful CPR, patients with CTP C as well as advanced ACLF did not survive 28 days with good neurological outcome.
Electronic supplementary material
The online version of this article (doi:10.1186/s13613-017-0322-1) contains supplementary material, which is available to authorized users.
Keywords: Cardiac arrest, Cirrhosis, Acute-on-chronic liver failure, Multiple organ failure, Intensive care unit
Background
Patients with liver cirrhosis [1] and organ failure admitted to intensive care units (ICU) have high morbidity and mortality [2, 3]. Mortality rates of up to 80% are reported in critically ill cirrhotic patients, progressively increasing with the number of organs failing [4–6]. Recently, chronic liver failure-SOFA (CLIF-SOFA) score [3] was developed as a tool for risk stratification in patients with cirrhosis and acute-on-chronic liver failure (ACLF) [2, 3].
Cardiac arrest (CA) can be the consequence of or lead to multiple organ failure. It is one of the leading causes of death in many parts of the world. Every year estimated 375,000–700,000 citizens are suffering CA in Europe and the USA [7, 8] and receive cardiopulmonary resuscitation (CPR). Patients who achieve return of spontaneous circulation (ROSC) following CA have high morbidity and mortality mainly due to cerebral and cardiac dysfunction that accompany whole-body ischaemia and reperfusion [9]. These disabilities can lead to the post-CA syndrome, which is defined as multiple organ failure after CA. Despite advances in critical and emergency care, survival rates after in-hospital cardiac arrest (IHCA) and out-of-hospital cardiac arrest (OHCA) are generally poor and varying greatly for OHCA between 8–16% [10, 11] and for IHCA 14–23% [12–14].
Data on occurrence and outcome of CA in patients with liver cirrhosis are not available. Therefore, the aim of the study was to investigate cause and outcome in patients with liver cirrhosis after CA and ROSC compared to a large cohort of patients with CA and ROSC without liver cirrhosis.
Methods
This study was based on a prospectively maintained registry at the Emergency Department of the Medical University of Vienna. This registry was approved by the ethics committee of the Medical University of Vienna. Due to the observational character of the study, informed consent was waived. The study was performed between January 2005 and January 2012. All consecutive patients admitted to the Emergency Department of the Medical University Vienna after CA and ROSC were included in the analysis. CPR and post-CA care were performed in accordance with the European Resuscitation Council guidelines [15, 16]. The data were collected prospectively according to Utstein-style guidelines [17, 18]. Patients suffering from OHCA were treated by the Viennese two-tier EMS system, featured by an EMS physician and paramedics; the EMS system was described previously in detail [19, 20]. No-flow time was defined as the time period from onset of CA to the start of resuscitation efforts. Low-flow time was defined as the time period from the start of resuscitation efforts until ROSC. Time to ROSC was defined as time from onset of CA until ROSC. CA survivors were followed prospectively for at least 1 year after admission to the emergency department for assessment of survival and neurological outcome. Rates of 28-day mortality, 6-month mortality and 1-year mortality were assessed on site or by contacting the patients or their attending physicians. Cerebral function and overall performance were assessed on admission and after 28 days, 6 months and 1 year, by clinical visits, by physicians on site or contacting the attending physician, the patients or the family of the patient directly by telephone. Cerebral performance categories (CPC) [21] and overall performance categories (OPC) scales were used to assess neurological and overall outcome. A CPC/OPC score of 1–2 was defined as favourable neurological/overall outcome, such as 3–5 as unfavourable. The primary outcome was good neurological survival (CPC 1/2) after 6 months; our secondary outcome was overall mortality after 1 year.
Routine laboratory assessment including coagulation and liver function parameters was performed on daily basis. Furthermore, aetiology of CA (cardiac and non-cardiac origin like pulmonary, traumatic, cerebral, septic, intoxication, drowning, hypothermia, unclear and others) and underlying diseases were assessed and documented.
Severity of illness was evaluated in all patients using Sequential Organ Failure Assessment (SOFA) score [22] and Simplified Acute Physiology Score (SAPS II) [23]. Charlson comorbidity index (CCI) [24] was calculated in all patients. For patients with liver cirrhosis, model of end-stage liver disease score (MELD) [25], Child–Turcotte–Pugh (CTP) score [26] and CLIF-SOFA score [3] were calculated on admission, and CLIF-SOFA was additionally calculated 24 and 48 h after ROSC.
All patients were screened for signs of liver cirrhosis. Presence of liver cirrhosis was defined via histology, if available, otherwise by a combination of clinical characteristics (ascites, spider angiomata, caput medusa), laboratory and radiological findings (typical morphological changes of the liver, sings of portal hypertension, etc. in ultrasonography or computed tomography scanning).
Statistical analysis
Data are presented as count and relative frequency or median and 25–75% interquartile range (IQR). We tabulated clinical variables according to liver cirrhosis status and used Chi-squared, Fisher exact or Mann–Whitney U test for hypothesis testing as appropriate. The prognostic factor of interest was liver cirrhosis, and we used logistic regression to estimate the effect on neurological intact survival. The dependent variable was favourable neurological survival (best CPC 1 or 2; yes vs. no). In a multivariable logistic regression model, we entered liver cirrhosis as main covariable and age, sex, OHCA, witnessed CA, time to ROSC, presence of shockable rhythm, cardiac cause of CA, mechanical ventilation, SOFA on admission, initiation of MTH, CCI and cumulative adrenaline dose as other covariates to the model. To allow for potentially non-random missing data for time to ROSC caused by unwitnessed cardiac arrest, we categorised this variable for 0–4, 5–12, 13–24, 25–44, 45 + minutes as well as ‘missing’ as the sixth category. We used a similar model to estimate the associations with mortality at one year as the outcome. In all models, we tested for linear effects, first-order interactions and model fit using the likelihood ratio test. Survival function estimates were calculated using Kaplan–Meier method and were compared by the log-rank test. Statistical analysis was conducted using Stata 14 (StataCorp, College Station, TX) and IBM SPSS Statistics version 23.0 (IBM Corp., Armonk, NY). Generally, a p value < 0.05 was considered statistically significant.
Results
Study population
In total, 1068 patients (72% male, median age 61 years) after CA and ROSC were included in this study. Forty-seven (4%) of these patients had liver cirrhosis. Main cause of CA was cardiac in 678 (63%) patients of the total cohort. A total of 798 (75%) patients suffered CA out of hospital. Patients with liver cirrhosis had a significantly higher underlying non-cardiac cause compared to patients without cirrhosis. Median SOFA, SAPS II and CCI on admission were significantly higher in patients with liver cirrhosis. Sex, age, height and weight were distributed equally between both groups. Detailed characteristics of the study population are given in Table 1. Liver function and coagulation parameters were significantly different between patients with and without cirrhosis on hospital admission as illustrated in Additional file 1: Table S1.
Table 1.
Patients’ characteristics of the study population at admission stratified according to the presence of cirrhosis
| Parameters | All patients (n = 1068) | Cirrhosis (n = 47) | No cirrhosis (n = 1021) | p value |
|---|---|---|---|---|
| Age, years median; IQR | 61 (50–72) | 62 (51–67) | 61 (50–72) | 0.92 |
| Male, n % | 765 (72) | 35 (74) | 730 (72) | 0.66 |
| Weight, kg median; IQR | 80 (70–90) | 80 (69.5–93) | 80 (70–90) | 0.72 |
| Height, cm median; IQR | 175 (168–180) | 175 (165–180) | 175 (168–180) | 0.59 |
| SOFA admission, pts median; IQR | 9 (6–12) | 11 (7.5–13) | 9 (6–12) | < 0.05 |
| SAPS II admission, pts median; IQR | 80 (74–88) | 87 (77.5–100) | 80 (73–87) | < 0.001 |
| Charlson comorbidity index, pts. median; IQR | 1 (0–3) | 4 (2.5–6) | 1 (0–2) | < 0.001 |
| Cause of arrest, n % | ||||
| Cardiac | 678 (63) | 21 (45) | 657 (64) | < 0.05 |
| Out of hospital, n % | 798 (75) | 31 (66) | 767 (75) | 0.16 |
| Invasive mechanical ventilation, n % | 850 (80) | 35 (74) | 815 (80) | 0.37 |
| Before cardiac arrest—normal CPC, n % | 1043 (98) | 45 (96) | 998 (98) | 0.45 |
| Before cardiac arrest—normal OPC, n % | 973 (91) | 39 (83) | 934 (91) | 0.09 |
| Ischaemic time, min median; IQR* | ||||
| No flow | 0 (0–3) | 0 (0–3.5) | 0 (0–3) | 0.49 |
| Low flow | 13 (4–25) | 11 (3–23) | 13 (4–25) | 0.51 |
| Time to ROSC | 16 (5–30) | 15 (3–27) | 16 (5–30) | 0.42 |
| Epinephrine cumulative (mg) median; IQR | 3 (1–4) | 3 (1–5.5) | 3 (1–4) | < 0.001 |
| Witnessed cardiac arrest, n % | 921 (86) | 42 (89) | 879 (86) | 0.56 |
| Initial rhythm, n % | ||||
| VT/VF | 550 (51) | 10 (21) | 540 (53) | < 0.001 |
| PEA/asystole | 465 (44) | 35 (75) | 430 (42) | |
| Other/unknown | 53 (5) | 2 (4) | 51 (5) | 0.82 |
| Defibrillation, n % | 646 (60) | 14 (30) | 632 (62) | < 0.001 |
| Therapeutic hypothermia, n % | 666 (62) | 18 (38) | 648 (63) | < 0.001 |
SOFA Sequential Organ Failure Assessment, SAPS Simplified Acute Physiology Score, CPC cerebral performance categories, OPC overall performance categories, ROSC return of spontaneous circulation, VT ventricular tachycardia, VF ventricular fibrillation, PEA pulseless electrical activity
* Overall (n = 926), cirrhosis (n = 41), no cirrhosis (n = 1021)
Characteristics of patients with liver cirrhosis
Main underlying aetiology of liver cirrhosis was alcoholic liver disease (n = 35, 74%) followed by viral hepatitis (n = 6, 13%) and others (n = 6, 13%). Child–Turcotte–Pugh (CTP) class prior to admission was A in 17 (36%), B in 17 (36%) and C in 13 (28%) patients. Hepatocellular carcinoma (HCC) was present in three patients. Three patients had transjugular intrahepatic portosystemic shunt (TIPS), and one patient was listed for liver transplantation prior to occurrence of CA. No patient had liver transplantation during follow-up. Aetiology of CA was cardiac (n = 21, 45%), variceal bleeding (n = 6, 13%), sepsis (n = 5, 11%), respiratory insufficiency (n = 5, 11%), electrolyte disturbances (n = 4, 9%) and other causes (n = 6, 13%). Detailed data are illustrated in Table 2.
Table 2.
Characteristics of patients with cirrhosis stratified according to good 28-day outcome and bad 28-day outcome
| Parameters | Overall (n = 47) | Good 28-day outcome (n = 9) | Bad 28-day outcome (n = 38) | p value* |
|---|---|---|---|---|
| Aetiology of cirrhosis, n % | 0.33 | |||
| Alcoholic | 35 (74) | 7 (78) | 28 (74) | |
| Viral | 6 (13) | 2 (22) | 4 (10) | |
| Other (cryptogenic, cardiac, etc.) | 6 (13) | 0 (0) | 6 (16) | |
| Hepatocellular carcinoma, n % | 3 (6) | 0 (0) | 3 (8) | 0.38 |
| Liver TX during follow-up, n % | 0 (0) | 0 (0) | 0 (0) | |
| TIPS, n % | 3 (6) | 0 (0) | 3 (8) | 0.38 |
| CLIF-SOFA—admission median; IQR | 10 (6–12.5) | 4 (3–4) | 11 (9–13) | < 0.001 |
| CLIF-SOFA—24 h median; IQR | 10 (4.5–14) | 4 (2–7) | 12 (8.25–15.5) | 0.01 |
| CLIF-SOFA—48 h median; IQR | 7 (2–12.5) | 1 (1–7) | 11 (6–13.75) | 0.01 |
| CTP—before admission, n % | 0.05 | |||
| A | 17 (36) | 6 (67) | 11 (29) | |
| B | 17 (36) | 3 (33) | 14 (37) | |
| C | 13 (28) | 0 (0) | 13 (34) | |
| CTP points—before admission median; IQR | 7 (5.5–10) | 6 (5–7) | 8 (6–11) | 0.03 |
| MELD—admission median; IQR | 19 (10.5–24) | 10 (9–10) | 21 (14–24) | < 0.001 |
| SOFA—admission median; IQR | 11 (7.5–13) | 4 (3–7) | 12 (10–13.75) | < 0.001 |
| SAPS II—admission median; IQR | 87 (77.5–100) | 66 (66–75) | 92 (85–102.75) | < 0.001 |
| Ascites—before admission, n % | 0.33 | |||
| None | 15 (32) | 4 (44) | 11 (29) | |
| Mild | 25 (53) | 5 (56) | 20 (53) | |
| Severe | 7 (15) | 0 (0) | 7 (18) | |
| HE—before admission, n % | 0.22 | |||
| None | 25 (53) | 7 (78) | 18 (47) | |
| I–II | 17 (36) | 2 (22) | 15 (40) | |
| III–IV | 5 (11) | 0 (0) | 5 (13) | |
| ACLF—on admission, n % | < 0.001 | |||
| Grade 1 | 11 (23) | 1 (11) | 10 (26) | |
| Grade 2 | 11 (23) | 0 (0) | 11 (30) | |
| Grade 3 | 11 (23) | 0 (0) | 11 (30) | |
| No ACLF | 14 (30) | 8 (89) | 6 (16) | |
| ACLF—during follow-up, n % | < 0.001 | |||
| Grade 1 | 1 (2) | 1 (11) | 0 (0) | |
| Grade 2 | 3 (6) | 1 (11) | 2 (5) | |
| Grade 3 | 0 (0) | 0 (0) | 0 (0) | |
| No ACLF | 10 (21) | 6 (67) | 4 (11) | |
| Ischaemic time, min median; IQR | ||||
| No flow | 0 (0–3.5) | 0 (0–0) | 0 (0–5) | < 0.01 |
| Low flow | 11 (3–23) | 1 (1–3) | 16 (8–23.5) | 0.06 |
| Time to ROSC | 15 (3–27) | 1 (1–3) | 19.5 (11–28) | < 0.05 |
| Initial rhythm, n % | ||||
| VT/VF | 10 (21) | 3 (33) | 7 (18) | 0.569 |
| PEA/Asystole | 35 (75) | 4 (45) | 31 (82) | < 0.05 |
| Other/unknown | 2 (4) | 2 (22) | 0 (0) | 0.305 |
| Witnessed cardiac arrest, n % | 42 (89) | 9 (100) | 33 (87) | 0.118 |
| Defibrillation, n % | 14 (30) | 3 (33) | 11 (29) | 0.569 |
| Therapeutic hypothermia, n % | 18 (38) | 1 (11) | 17 (45) | < 0.01 |
CPC cerebral performance categories, TX transplantation, TIPS transjugular intrahepatic portosystemic shunt, CLIF-SOFA chronic liver failure-Sequential Organ Failure Assessment, CTP Child–Turcotte–Pugh, MELD model for end-stage liver disease, SOFA Sequential Organ Failure Assessment, SAPS Simplified Acute Physiology Score, HE hepatic encephalopathy, ACLF acute-on-chronic liver failure
* CPC 1/2 versus CPC 3/4 or mortality
CLIF-SOFA on admission, 24 and 48 h following hospital admission, and MELD, SOFA and SAPS II on admission and CTP score prior to CA were significantly higher in patients with unfavourable neurological outcome or mortality within 28 days.
Thirty-three patients (70%) had ACLF on admission. Four (29%) out of 14 patients without ACLF on admission developed ACLF within 48 h after ROSC. Two (4%) of the patients had ACLF prior to admission. ACLF grades 1, 2 and 3 were present in 12 (32%), 14 (38%) and 11 (30%) patients, respectively.
CPR-specific data
The majority of patients of the total cohort (75%) suffered OHCA. This rate did not differ significantly in patients with and without cirrhosis. Cardiac arrest was witnessed in 921 (86%) patients. No-flow time was median 0 (IQR 0–3) minutes, low-flow 13 (IQR 4–25) minutes and time to ROSC 16 (IQR 5–30) minutes, which did not differ significantly between patients with and without cirrhosis. Initial shockable rhythm (VT/VF) was significantly more frequent present in patients without cirrhosis. Accordingly, frequency of defibrillation during CPR was significantly lower in patients with liver cirrhosis. Furthermore, cumulative epinephrine dosage during CPR was significantly higher in patients with cirrhosis. First measured lactate levels were significantly higher in patients with liver cirrhosis. Table 1 and Additional file 1: Table S3 illustrate the detailed CPR data.
Functional outcome and survival after CA
Almost all patients both with and without cirrhosis showed a normal CPC and OPC score prior to occurrence of CA as given in Table 1. Rate of favourable neurological outcome was 19% after 28 days, 6 months and 1 year in patients with cirrhosis, compared to 47% after 28 days and 6 months and 43% after 1 year in patients without cirrhosis, respectively. Rate of favourable neurological outcome in CA survivors after 6 months was significantly lower in patients with liver cirrhosis (19 vs. 47%, crude OR 0.26; 95% CI 0.13–0.53). This association continued to be statistically significant after adjustment for covariables (multivariable-adjusted OR 0.13; 95% CI 0.04–0.36, see Table 3). Mortality in patients with cirrhosis was significantly higher compared to patients without cirrhosis (74, 77 and 79% versus 41, 48 and 50% after 28 days, 6 months and 1 year, respectively; OR for 1-year mortality 3.69; 95% CI 1.82–7.51). Figure 1 demonstrates the survival of patients with and without cirrhosis. Cirrhosis was an independent risk factor for 1-year mortality in multivariate regression analysis (multivariable-adjusted OR 3.25; 95% CI 1.33–7.96, see Table 4).
Table 3.
Logistic regression model for factors associated with good neurological outcome (CPC 1/2 vs. > 2 or deceased)
| Parameter | OR (95% CI) | p value |
|---|---|---|
| Cirrhosis (yes vs. no) | 0.13 (0.04–0.36) | < 0.001 |
| Age (years) | 0.96 (0.96–0.98) | < 0.001 |
| Time to ROSC (per category)* | 0.56 (0.47–0.67) | < 0.001 |
| Shockable rhythm (yes vs. no) | 2.16 (1.45–3.23) | < 0.001 |
| Intubated on admission (yes vs. no) | 0.17 (0.09–0.34) | < 0.001 |
| SOFA admission (per category)* | 0.73 (0.64–0.82) | < 0.001 |
| Cardiac cause (yes vs. no) | 1.73 (1.17–2.58) | 0.01 |
| Epinephrine cumulative dose (per mg) | 0.91 (0.85–0.98) | 0.01 |
| Witnessed cardiac arrest (yes vs. no) | 0.62 (0.32–1.23) | 0.17 |
| Mild therapeutic hypothermia (yes vs. no) | 1.23 (0.80–1.90) | 0.36 |
| Out-of-hospital cardiac arrest (yes vs. no) | 0.89 (0.58–1.38) | 0.61 |
| Male (vs. female) | 0.92 (0.65–1.31) | 0.65 |
| Charlson comorbidity index (per category)* | 0.97 (0.84–1.12) | 0.67 |
OR multivariable-adjusted odds ratio, CI confidence interval, ROSC return of spontaneous circulation, SOFA Sequential Organ Failure Assessment, mg milligram
* Time to ROSC categories: 0–4, 5–12, 13–24, 25–44, 45 + min, or missing; SOFA categories (score): 5, 6–8, 9–10, 11–12, 12 +, or missing; Carlson comorbidity categories: 0, 1, 2 + 3, 4 +, or missing
Fig. 1.
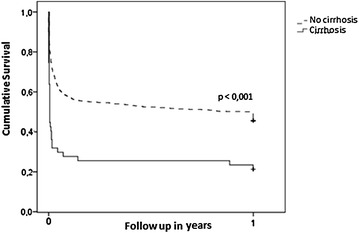
Survival after ICU admission for cardiac arrest according to the presence and absence of cirrhosis estimated by Kaplan–Meier method
Table 4.
Logistic regression model for factors associated with 1-year mortality
| 1-year mortality | OR | (95% CI) | p value |
|---|---|---|---|
| Age | 1.05 | (1.03–1.06) | < 0.001 |
| Time to ROSC* | 1.57 | (1.32–1.87) | < 0.001 |
| Shockable rhythm | 0.45 | (0.31–0.67) | < 0.001 |
| Tube admission | 2.33 | (1.35–4.03) | < 0.001 |
| SOFA admission* | 1.36 | (1.20–1.54) | < 0.001 |
| Cirrhosis | 3.25 | (1.33–7.96) | 0.01 |
| Charlson comorbidity index* | 1.19 | (1.03–1.37) | 0.02 |
| Epinephrine cumulative | 1.07 | (1.01–1.15) | 0.03 |
| Male | 1.41 | (1.00–1.98) | 0.05 |
| Cardiac cause of CA | 0.68 | (0.46–1.00) | 0.05 |
| Mild therapeutic hypothermia | 0.68 | (0.45–1.05) | 0.09 |
| OHCA | 0.99 | (0.66–1.50) | 0.98 |
| Witnessed CA | 1.00 | (0.51–1.94) | 0.99 |
OR multivariable-adjusted odds ratio, CI confidence interval, OHCA out-of-hospital cardiac arrest, CA cardiac arrest, ROSC return of spontaneous circulation, SOFA Sequential Organ Failure Assessment
* Time to ROSC categories: 0–4, 5–12, 13–24, 25–44, 45 + min, or missing; SOFA categories (score): 5, 6–8, 9–10, 11–12, 12 +, or missing; Charlson comorbidity categories: 0, 1, 2 + 3, 4 +, or missing
No patient with liver cirrhosis CTP C as well as no patient with HCC or pre-existing TIPS survived longer than 28 days following ROSC with good neurological outcome. Figure 2 demonstrates the survival of patients with favourable neurological outcome in cirrhosis CTP A + B versus CTP C.
Fig. 2.
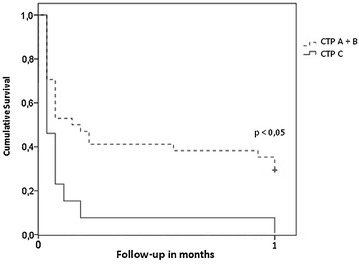
Probability of having a good neurological outcome after a cardiac arrest among cirrhotic patients according to Child–Turcotte–Pugh score estimated by Kaplan–Meier method
Forty per cent (n = 4) of patients with cirrhosis without ACLF died within 28 days following ROSC or had unfavourable neurological outcome compared to 92% (n = 34) of patients with ACLF (p < 0.001). In detail, 83% (n = 10) of patients with ACLF grade 1, 93% (n = 13) with ACLF grade 2 and 100% (n = 11) with ACLF grade 3 had unfavourable neurological outcome or died within 28 days. Multiple organ failure as cause of death was observed in 30 patients with cirrhosis, one patient had cerebral herniation following hypoxic brain injury, and four patients died with palliative care following irreversible hypoxic brain damage.
Mild therapeutic hypothermia (MTH) was applied in 666 (62%) patients of the total cohort [18 (38%) patients with cirrhosis and 648 (63%) without cirrhosis (p < 0.001)]. Furthermore, MTH was significantly less frequent applied in patients with liver cirrhosis. In the cirrhosis population, patients with MTH were older, had lower SOFA, SAPS II, CLIF-SOFA and MELD score on admission and had significantly longer time to ROSC compared to patients without MTH. We could not observe bleeding or any other complication related to MTH. Twenty-eight-day mortality did not differ significantly between patients with cirrhosis and MTH versus no MTH (78 vs. 72%). Additional file 1: Table S2 illustrates the detailed data on MTH in patients with cirrhosis.
Discussion
In our study, we analysed 1068 critically ill patients following CA and ROSC. Forty-seven of these patients suffered from liver cirrhosis. Presence of cirrhosis was associated with low rates of favourable neurological outcome and increased mortality. Highest rates of unfavourable functional outcome were found in advanced stages of cirrhosis and ACLF.
Cardiac arrest was witnessed in 921 (86%) patients of our cohort, and this is comparable to a previous publication [27]. Seventy-five per cent of the total cohort had OHCA. The first recorded rhythm was shockable in 52% of these patients which is comparable to the reported prevalence of 20–60% in the literature [10, 11, 28]. In contrast, shockable rhythms (35%) were found less frequent in IHCA in accordance with the literature (21–39%) [13, 14, 29]. In the total cohort, 1-year mortality was 50% and favourable functional outcome was observed in 43% of patients following CA. This high rate of favourable outcome may be the consequence of several circumstances. First, we included only patients following ROSC after CA. Accordingly, the rate of good functional outcome was comparable to other studies including only patients with ROSC [27, 30]. Second, we observed in average a short no-flow period in our cohort, which may contribute to the high rate of favourable functional outcome. Third, the vast majority (86%) of CAs was witnessed and we observed a shockable rhythm in about half of the patients.
We identified 47 (4%) patients with cirrhosis in our cohort. This finding is comparable to publications of critical illness, where prevalence of cirrhosis was about 4–7% in the general intensive care setting [31, 32]. These patients had significantly higher SOFA, SAPS II and CCI on hospital admission. Time to ROSC was comparable between patients with and without cirrhosis. However, we observed several significant differences in CA in patients with and without cirrhosis. First, a cardiac aetiology was less frequent and patients with cirrhosis were more likely to have a non-shockable initial ECG rhythm. Second, cumulative epinephrine dosage was higher during CPR and third defibrillations were less frequently performed in patients with cirrhosis. These differences seem to be mainly a consequence of the fact that patients with cirrhosis frequently developed CA following complications of cirrhosis like variceal haemorrhage, severe infection or severe electrolyte disturbances.
Rates of unfavourable functional outcome and mortality were significantly higher in patients with cirrhosis despite no-flow times that were comparable to patients without cirrhosis. This can be explained by the higher comorbidity rate, higher rate of non-cardiac cause and higher rate of non-shockable rhythm in patients with cirrhosis. Furthermore, multivariate regression analysis identified presence of cirrhosis per se as an independent predictor of unfavourable outcome.
Overall 38 (81%) patients with cirrhosis had unfavourable neurological outcome or died within 28 days following CA. These patients had a significant higher severity of liver disease and organ failure represented by CTP class, CLIF-SOFA, MELD and ACLF grade as illustrated in Table 2. ACLF was present in 33 (70%) cirrhotic patients at ICU admission following ROSC, and four patients developed ACLF within 48 h after admission. These patients had dramatically worse functional outcome: out of 37 patients with ACLF, 34 (92%) had unfavourable neurology or died within 28 days. Moreover, we observed significant differences in CA characteristics. Patients with cirrhosis and favourable 28-day outcome had a significantly lower no-flow time and time to ROSC and a significantly lower rate of non-shockable rhythm compared to patients with unfavourable neurological outcome or mortality. Furthermore, CA was witnessed in all cases in patients with favourable 28-day outcome. Ischaemic times, especially no flow, seem to be crucial for development of organ failure and unfavourable outcome in patients with cirrhosis. The higher rate of unfavourable 28-day outcome in patients with cirrhosis following CA and ROSC compared to critically ill patients with liver cirrhosis [3, 4, 33] may be explained mainly by the higher severity of illness at baseline in our cohort [4].
The post-CA phase is frequently complicated by the post-CA syndrome, a unique pathophysiological process involving multiple organs [9]. For instance, post-CA brain injury frequently complicates the post-CA phase and accounts for high morbidity and mortality [9, 33]. Factors like hyperglycaemia, impaired cerebral autoregulation as well as pre-existing cerebral impairment in the sense of hepatic encephalopathy could lead to further cerebral injury in patients with cirrhosis. Additionally, post-CA myocardial dysfunction and systemic ischaemia and reperfusion response are frequent findings and account for high morbidity and mortality after CA [15]. The severity of the post-CA syndrome varies according to duration and cause of CA [15]. In our cohort of patients with cirrhosis, death was mainly related to multiple organ failure (86%). Post-anoxic encephalopathy as solitaire cause of death was observed in a minority of patients with cirrhosis, only. Patients with cirrhosis seem to be more prone to organ impairment following CA. This seems to be a consequence of a higher vulnerability for new onset of organ failure and higher severity of illness during CA as discussed previously.
Mild therapeutic hypothermia, i.e. targeted temperature 32–36 °C for 24 h [15], is frequently used despite recent controversial findings as standardised post-CA care [27, 30, 34]. MTH was performed in 666 (62%) patients of our total cohort and in 18 (38%) patients with cirrhosis. Main reason for withholding MTH in cirrhosis was severely abnormal coagulation. A recent study of patients with cirrhosis demonstrated that abnormal coagulation parameters, especially fibrinogen and platelet counts, predict new onset of major bleeding in patients with cirrhosis at the ICU [33]. Data on bleeding complications due to MTH in patients with liver diseases are scarce. Two small case series [35, 36], a randomised controlled trial [37] and a retrospective study [38] of MTH in patients with acute liver failure did not observe an association of MTH and increased rate of bleeding complications. We could not observe new onset of bleeding or any other complication related to MTH in our cohort of critically ill patients with cirrhosis. Twenty-eight-day mortality did not differ significantly in patients with cirrhosis and MTH compared to patients with cirrhosis without MTH. This may be a consequence of the rather small number of patients with cirrhosis, the higher rate of OHCA and a significantly longer time to ROSC in the MTH group. In addition, this study was not powered to analyse the effect of MTH on prognosis in cirrhotic patients. Additional file 1: Table S2 illustrates the detailed data.
Multiple organ failure is associated with high mortality in patients with liver cirrhosis. ACLF is a dynamic condition, which can improve or worsen in a short period of time [39]. Early and repeated risk stratification may help and guide clinical decision making in this extremely sick population [40, 41]. Although our study is able to identify the population that is at highest risk of worst outcome (patients with advanced stages of ACLF and patients with cirrhosis CTP C), we do not believe that current knowledge is already sufficient to provide (i.e. score-based) cut-offs in regard to the decision whether to continue or to stop treatment due to futility. Rather, we are convinced that further therapeutic decisions, especially for withdrawal of care, must take individual patient based factors (i.e. severity of acute and chronic illness, patient’s wishes, etc.) into account. Furthermore, remaining treatment options (e.g. liver transplantation), course of the disease and severity of acute illness should be taken into account for further decisions by the attending physician. Future studies are warranted for end-of-life decisions in critically ill patients with cirrhosis [41, 42].
Our study has some limitations. The number of patients with cirrhosis is rather small. However, this is the first study investigating CA in patients with cirrhosis. Furthermore, this study was conducted in a medical intensive care setting. Thus, our data may not be transferable to surgical ICUs. Residual confounding arising from unmeasured covariates cannot be entirely excluded.
In conclusion, CA survivors with cirrhosis have worse outcome than those without pre-existent chronic liver disease. Although one quarter of patients with liver cirrhosis survived longer than 28 days after successful CPR, patients with CTP C as well as advanced ACLF did not survive 28 days with good neurological outcome.
Authors’ contributions
KRo, CWa, FS and VF participated in study conception and design. AD, TH, KRu, AS, JO, PH, CWe, JKM, DJ, CWa, VF and KRo were involved in acquisition of data. KRo, VF, FS, CWa and HH contributed to analysis and interpretation of data. KRo and CWa drafted the manuscript. VF, FS and HH were involved in critical revision of the manuscript for important intellectual content. VF and FS participated in supervision. All authors read and approved the final manuscript.
Acknowledgements
The authors would like to thank the staff of the Emergency Department and ICUs of the Medical University of Vienna and appreciate their work.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study was based on a prospectively maintained registry at the Emergency Department of the Medical University of Vienna. This registry was approved by the ethics committee of the Medical University of Vienna. Due to the observational character of the study, informed consent was waived.
Funding
No financial support has been received conducting this study.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- CA
cardiac arrest
- ROSC
return of spontaneous circulation
- ICU
intensive care unit
- OHCA
out-of-hospital cardiac arrest
- IHCA
in-hospital cardiac arrest
- MTH
mild therapeutic hypothermia
- CPC
cerebral performance categories
- OPC
overall performance categories
- SOFA
Sequential Organ Failure Assessment
- SAPS
Simplified Acute Physiology Score
- CCI
Charlson comorbidity index
- MELD
model of end-stage liver disease
- CTP
Child–Turcotte–Pugh
- TIPS
transjugular intrahepatic portosystemic shunt
- HCC
hepatocellular carcinoma
- PCI
percutaneous coronary intervention
Additional file
Additional file 1: Table S1. Routine laboratory on admission. Table S2. Characteristics of cirrhotic patients with and without mild therapeutic hypothermia. Table S3. CPR-specific data according to in- and out-hospital cardiac arrest.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1186/s13613-017-0322-1) contains supplementary material, which is available to authorized users.
Kevin Roedl and Christian Wallmüller have contributed equally to this work
Contributor Information
Kevin Roedl, Email: k.roedl@uke.de.
Christian Wallmüller, Email: christian.wallmueller@meduniwien.ac.at.
Andreas Drolz, Email: a.drolz@uke.de.
Thomas Horvatits, Email: t.horvatits@uke.de.
Karoline Rutter, Email: k.rutter@uke.de.
Alexander Spiel, Email: alexander.spiel@meduniwien.ac.at.
Julia Ortbauer, Email: j.ortbauer@gmx.at.
Peter Stratil, Email: peter.stratil@meduniwien.ac.at.
Pia Hubner, Email: pia.hubner@meduniwien.ac.at.
Christoph Weiser, Email: christoph.weiser@meduniwien.ac.at.
Jasmin Katrin Motaabbed, Email: jasminmot@gmx.at.
Dominik Jarczak, Email: d.jarczak@uke.de.
Harald Herkner, Email: herald.herkner@meduniwien.ac.at.
Fritz Sterz, Email: fritz.sterz@meduniwien.ac.at.
Valentin Fuhrmann, Phone: 0049 40 7410 57020, Email: v.fuhrmann@uke.de.
References
- 1.Shellman RG, Fulkerson WJ, DeLong E, Piantadosi CA. Prognosis of patients with cirrhosis and chronic liver disease admitted to the medical intensive care unit. Crit Care Med. 1988;16:671–678. doi: 10.1097/00003246-198807000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Jalan R, Gines P, Olson JC, Mookerjee RP, Moreau R, Garcia-Tsao G, et al. Acute-on chronic liver failure. J Hepatol. 2012;57:1336–1348. doi: 10.1016/j.jhep.2012.06.026. [DOI] [PubMed] [Google Scholar]
- 3.Moreau R, Jalan R, Gines P, Pavesi M, Angeli P, Cordoba J, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology. 2013;144:1426–1437. doi: 10.1053/j.gastro.2013.02.042. [DOI] [PubMed] [Google Scholar]
- 4.McPhail MJW, Shawcross DL, Abeles RD, Chang A, Patel V, Lee G-H, et al. Increased survival for patients with cirrhosis and organ failure in liver intensive care and validation of the chronic liver failure-sequential organ failure scoring system. Clin Gastroenterol Hepatol. 2015;13(1353–1360):e1358. doi: 10.1016/j.cgh.2014.08.041. [DOI] [PubMed] [Google Scholar]
- 5.Arabi Y, Ahmed QA, Haddad S, Aljumah A, Al-Shimemeri A. Outcome predictors of cirrhosis patients admitted to the intensive care unit. Eur J Gastroenterol Hepatol. 2004;16:333–339. doi: 10.1097/00042737-200403000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Cholongitas E, Senzolo M, Patch D, Kwong K, Nikolopoulou V, Leandro G, et al. Risk factors, sequential organ failure assessment and model for end-stage liver disease scores for predicting short term mortality in cirrhotic patients admitted to intensive care unit. Aliment Pharmacol Ther. 2006;23:883–893. doi: 10.1111/j.1365-2036.2006.02842.x. [DOI] [PubMed] [Google Scholar]
- 7.Berdowski J, Berg RA, Tijssen JGP, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81:1479–1487. doi: 10.1016/j.resuscitation.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 8.Mozaffarian D, Benjamin EJ, Go ES, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circ. 2016;33(4):e38–360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 9.Neumar RW, Nolan JP, Adrie C, Aibiki M, Berg RA, Böttiger BW, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation. 2008;118:2452–2483. doi: 10.1161/CIRCULATIONAHA.108.190652. [DOI] [PubMed] [Google Scholar]
- 10.Atwood C, Eisenberg MS, Herlitz J, Rea TD. Incidence of EMS-treated out-of-hospital cardiac arrest in Europe. Resuscitation. 2005;67:75–80. doi: 10.1016/j.resuscitation.2005.03.021. [DOI] [PubMed] [Google Scholar]
- 11.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/S0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 13.Meaney PA, Nadkarni VM, Kern KB, Indik JH, Halperin HR, Berg RA. Rhythms and outcomes of adult in-hospital cardiac arrest. Crit Care Med. 2010;38:101–108. doi: 10.1097/CCM.0b013e3181b43282. [DOI] [PubMed] [Google Scholar]
- 14.Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS. Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2012;367:1912–1920. doi: 10.1056/NEJMoa1109148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nolan JP, Soar J, Cariou A, Cronberg T, Moulaert VRM, Deakin CD, et al. European Resuscitation Council and European Society of Intensive Care Medicine Guidelines for Post-resuscitation Care 2015: Section 5 of the European Resuscitation Council Guidelines for Resuscitation 2015. Resuscitation. 2015;95:202–222. doi: 10.1016/j.resuscitation.2015.07.018. [DOI] [PubMed] [Google Scholar]
- 16.Soar J, Nolan JP, Böttiger BW, Perkins GD, Lott C, Carli P. Section 3. Adult advanced life support: European Resuscitation Council guidelines for resuscitation 2015. Resuscitation. 2015;95:100–147. doi: 10.1016/j.resuscitation.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 17.Cummins RO, Chamberlain D, Hazinski MF, Nadkarni V, Kloeck W, Kramer E, et al. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital ‘Utstein style’. A statement for healthcare professionals from the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, the Australian Resuscitation Council, and the Resuscitation Councils of Southern Africa. Resuscitation. 1997;34:151–183. doi: 10.1016/S0300-9572(97)01112-X. [DOI] [PubMed] [Google Scholar]
- 18.Cummins RO, Chamberlain DA, Abramson NS, Allen M, Baskett PJ, Becker L, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein Style. A statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation. 1991;84:960–975. doi: 10.1161/01.CIR.84.2.960. [DOI] [PubMed] [Google Scholar]
- 19.Schober A, Sterz F, Laggner AN, Poppe M, Sulzgruber P, Lobmeyr E, et al. Admission of out-of-hospital cardiac arrest victims to a high volume cardiac arrest center is linked to improved outcome. Resuscitation. 2016;106:42–48. doi: 10.1016/j.resuscitation.2016.06.021. [DOI] [PubMed] [Google Scholar]
- 20.Nurnberger A, Sterz F, Malzer R, Warenits A, Girsa M, Stockl M, et al. Out of hospital cardiac arrest in Vienna: incidence and outcome. Resuscitation. 2013;84:42–47. doi: 10.1016/j.resuscitation.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 21.Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–484. doi: 10.1016/S0140-6736(75)92830-5. [DOI] [PubMed] [Google Scholar]
- 22.Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–710. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 23.Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957–2963. doi: 10.1001/jama.1993.03510240069035. [DOI] [PubMed] [Google Scholar]
- 24.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 25.Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464–470. doi: 10.1053/jhep.2001.22172. [DOI] [PubMed] [Google Scholar]
- 26.Cholongitas E, Papatheodoridis GV, Vangeli M, Terreni N, Patch D, Burroughs AK. Systematic review: the model for end-stage liver disease—should it replace Child-Pugh’s classification for assessing prognosis in cirrhosis? Aliment Pharmacol Ther. 2005;22:1079–1089. doi: 10.1111/j.1365-2036.2005.02691.x. [DOI] [PubMed] [Google Scholar]
- 27.Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, et al. Targeted temperature management at 33 °C versus 36 °C after cardiac arrest. N Engl J Med. 2013;369:2197–2206. doi: 10.1056/NEJMoa1310519. [DOI] [PubMed] [Google Scholar]
- 28.Schober A, Sterz F, Herkner H, Locker GJ, Heinz G, Fuhrmann V, et al. Post-resuscitation care at the emergency department with critical care facilities—a length-of-stay analysis. Resuscitation. 2011;82:853–858. doi: 10.1016/j.resuscitation.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 29.Wallmuller C, Meron G, Kurkciyan I, Schober A, Stratil P, Sterz F. Causes of in-hospital cardiac arrest and influence on outcome. Resuscitation. 2012;83:1206–1211. doi: 10.1016/j.resuscitation.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 30.Group HaCAS Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346:549–556. doi: 10.1056/NEJMoa012689. [DOI] [PubMed] [Google Scholar]
- 31.Piton G, Chaignat C, Giabicani M, Cervoni JP, Tamion F, Weiss E, et al. Prognosis of cirrhotic patients admitted to the general ICU. Ann Intensive Care. 2016;6:94. doi: 10.1186/s13613-016-0194-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fuhrmann V, Kneidinger N, Herkner H, Heinz G, Nikfardjam M, Bojic A, et al. Impact of hypoxic hepatitis on mortality in the intensive care unit. Intensive Care Med. 2011;37:1302–1310. doi: 10.1007/s00134-011-2248-7. [DOI] [PubMed] [Google Scholar]
- 33.Drolz A, Horvatits T, Roedl K, Rutter K, Staufer K, Kneidinger N, et al. Coagulation parameters and major bleeding in critically ill patients with cirrhosis. Hepatology. 2016;64:556–568. doi: 10.1002/hep.28628. [DOI] [PubMed] [Google Scholar]
- 34.Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557–563. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- 35.Jalan R, Olde Damink SWM, Deutz NEP, Hayes PC, Lee A. Moderate hypothermia in patients with acute liver failure and uncontrolled intracranial hypertension. Gastroenterology. 2004;127:1338–1346. doi: 10.1053/j.gastro.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 36.Jalan R, ODamink SW, Deutz NE, Lee A, Hayes PC. Moderate hypothermia for uncontrolled intracranial hypertension in acute liver failure. Lancet. 1999;354:1164–1168. doi: 10.1016/S0140-6736(98)12440-6. [DOI] [PubMed] [Google Scholar]
- 37.Bernal W, Murphy N, Brown S, Whitehouse T, Bjerring PN, Hauerberg J, et al. A multicentre randomized controlled trial of moderate hypothermia to prevent intracranial hypertension in acute liver failure. J Hepatol. 2016;65(2):273–279. doi: 10.1016/j.jhep.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 38.Karvellas CJ, Todd Stravitz R, Battenhouse H, Lee WM, Schilsky ML, Group UALFS Therapeutic hypothermia in acute liver failure: a multicenter retrospective cohort analysis. Liver Transpl. 2015;21:4–12. doi: 10.1002/lt.24021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Arroyo V, Moreau R, Jalan R, Gines P. Acute-on-chronic liver failure: a new syndrome that will re-classify cirrhosis. J Hepatol. 2015;62:S131–S143. doi: 10.1016/j.jhep.2014.11.045. [DOI] [PubMed] [Google Scholar]
- 40.Saliba F, Ichai P, Levesque E, Samuel D. Cirrhotic patients in the ICU: prognostic markers and outcome. Curr Opin Crit Care. 2013;19:154–160. doi: 10.1097/MCC.0b013e32835f0c17. [DOI] [PubMed] [Google Scholar]
- 41.Gustot T, Fernandez J, Garcia E, Morando F, Caraceni P, Alessandria C, et al. Clinical course of acute-on-chronic liver failure syndrome and effects on prognosis. Hepatology. 2015;62:243–252. doi: 10.1002/hep.27849. [DOI] [PubMed] [Google Scholar]
- 42.McPhail MJ, Auzinger G, Bernal W, Wendon JA. Decisions on futility in patients with cirrhosis and organ failure. Hepatology. 2016;64:986. doi: 10.1002/hep.28539. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets supporting the conclusions of this article are included within the article.


