Abstract
Our study aimed to assess the associations of plasma magnesium with prediabetes and type 2 diabetes (T2D) among Chinese adults. We conducted a case-control analysis of 4447 participants: 867 newly diagnosed prediabetes patients, 1475 newly diagnosed T2D patients and 2105 normal glucose tolerance (NGT) individuals. In a subsample of 599 apparently healthy individuals, we measured plasma hs-CRP levels to examine their relation to plasma magnesium. Plasma magnesium and hs-CRP were measured by inductively coupled plasma mass spectrometry and an enzyme-linked immunosorbent assay, respectively. Plasma magnesium decreased from NGT to prediabetes to T2D, and was inversely associated with prediabetes and T2D. After adjustment for potential confounding factors, the ORs from the lowest to highest quartiles of plasma magnesium were 1, 0.57 (95%CI, 0.44–0.74), 0.49 (0.37–0.65) and 0.51 (0.37–0.70) for prediabetes, and 1, 0.26 (0.20–0.33), 0.15 (0.12–0.20) and 0.15 (0.11–0.20) for T2D. Consistently, plasma magnesium was inversely correlated with plasma hs-CRP in our subsample analysis; the geometric mean hs-CRP concentration for ascending quartiles of plasma magnesium were 1.29 (1.06–1.57), 1.16 (0.95–1.41), 1.00 (0.81–1.22), and 0.71 (0.58–0.88) mg/l. Plasma magnesium was independently and inversely associated with prediabetes and T2D in Chinese adults.
Introduction
Magnesium is an essential mineral found in many foods, including whole grains, green leafy vegetables, coffee, legumes and nuts1. Meanwhile, magnesium is an essential cofactor for multiple enzymes involved in glucose metabolism and is hypothesized to play a role in glucose homeostasis, insulin action and in the development of type 2 diabetes (T2D)2. Prediabetes, characterized by impaired fasting glucose (IFG) and/or impaired glucose tolerance (IGT), is considered an important risk factor for the development of overt diabetes and cardiovascular disease3,4. Epidemiological studies have investigated the association of serum magnesium with prediabetes and T2D, but the findings were inconsistent5–9. On the other hand, recent studies indicated that increasing dietary magnesium intake may be associated with a reduced risk of T2D and have a dose-response relationship10,11. In addition, calcium has been suggested having a role in the development of T2D for its potential in improving pancreatic β-cell function and insulin sensitivity12–16, and dietary calcium and magnesium intakes are moderately/highly correlated in diverse populations5,15–17. However, few studies were conducted to regard the associations of serum or plasma magnesium with prediabetes and T2D, considering the confounding of plasma calcium within the same population.
Therefore, the objective of this study was to investigate the relationship between plasma magnesium concentrations and newly diagnosed prediabetes and T2D in a large case-control study conducted among a Chinese population. To explore possible mechanisms, we also examined whether plasma magnesium was associated with plasma high sensitivity C-reactive protein (hs-CRP) concentrations in a subsample of apparently healthy individuals.
Results
Patient characteristics
Anthropometric and metabolic characteristics of the 4447 participants (867 prediabetes, 1475 T2D, 2105 NGT) are shown in Table 1. Plasma magnesium concentrations were significantly decreased in the individuals with prediabetes and T2D compared with the controls (median: 22.12 mg/l in NGT, 21.42 mg/l in prediabetes, and 19.84 mg/l in T2D, P < 0.001). Compared to controls, the patients with prediabetes and T2D had higher BMI, prevalence of family history of diabetes and hypertension, higher levels of total cholesterol, triglyceride, fasting plasma glucose (FPG), fasting plasma insulin (FPI), 2-h post-glucose load, HbA1C, lower plasma calcium and magnesium concentration. When looking at the insulin sensitivity indexes, we observed higher HOMA-IR in prediabetes and T2D.
Table 1.
Anthropometric and metabolic characteristics of NGT, prediabetes and T2D groups.
| Variable | NGT | Prediabetes | T2D | P value |
|---|---|---|---|---|
| n = 2105 | n = 867 | n = 1475 | ||
| Age (years) | 52.21 ± 12.89 | 52.96 ± 12.22 | 51.20 ± 11.23 | <0.001 |
| Male (%) | 59.71 | 61.15 | 59.78 | 0.754 |
| BMI (kg/m2) | 23.30 ± 3.53 | 25.09 ± 5.19 | 25.14 ± 3.93 | <0.001 |
| Smoker (%) | 35.11 | 27.16 | 33.60 | <0.001 |
| Drinker (%) | 34.39 | 32.54 | 35.08 | 0.480 |
| Family history of diabetes (%) | 8.32 | 17.30 | 22.62 | <0.001 |
| Hypertension (%) | 22.89 | 33.50 | 35.78 | <0.001 |
| FPG (mmol/l) | 5.09 ± 0.66 | 6.16 ± 0.53 | 9.72 ± 3.21 | <0.001 |
| OGTT2h (mmol/l) | 6.43 ± 0.95 | 8.74 ± 1.46 | 17.61 ± 5.56 | <0.001 |
| HbA1C (%) | 5.57 ± 0.40 | 5.94 ± 0.60 | 8.79 ± 2.37 | <0.001 |
| FPI (mmol/l) | 7.88 (5.38–11.45) | 9.54 (6.58–13.98) | 9.46 (6.14–14.35) | <0.001 |
| HOMA-β | 85.87 (59.54–122.59) | 73.94 (49.63–113.47) | 36.15 (19.07–62.75) | 0.067 |
| HOMA-IR | 1.90 (1.26–2.76) | 2.58 (1.76–3.84) | 3.84 (2.53–6.01) | <0.001 |
| Total cholesterol (mmol/l) | 4.39 (3.57–5.14) | 4.69 (3.87–5.42) | 4.61 (3.98–5.32) | <0.001 |
| Triglyceride (mmol/l) | 1.12 (0.8–1.57) | 1.30 (0.89–1.86) | 1.38 (0.95–2.11) | <0.001 |
| HDL-c (mmol/l) | 1.25 (0.98–1.54) | 1.21 (0.98–1.5) | 1.11 (0.89–1.4) | <0.001 |
| LDL-c (mmol/l) | 2.58 (2.04–3.19) | 2.74 (2.1–3.34) | 3.02 (2.36–3.67) | 0.550 |
| Mg (mg/l) | 22.12 ± 2.78 | 21.42 ± 2.97 | 19.84 ± 3.47 | <0.001 |
| Ca (mg/l) | 73.14 ± 9.56 | 71.10 ± 9.83 | 68.60 ± 11.28 | <0.001 |
Abbreviations: BMI, body mass index; FPG, fasting plasma glucose; FPI, fasting plasma insulin; HDL-c, high-density lipoprotein cholesterol; HOMA-β, homeostasis model assessment of β cell function; HOMA-IR, homeostasis model assessment of insulin resistance; LDL-c, low-density lipoprotein cholesterol; NGT, normal glucose tolerance; OGTT2h, 2-h post-glucose load; T2D, type 2 diabetes. Data were presented as percentage for categorical data, mean (standard deviation) for parametrically distributed data or median (interquartile range) for nonparametrically distributed data.
Association of serum magnesium levels with prediabetes and T2D
Table 2 presents odds ratios (ORs) for prediabetes and T2D associated with the levels of plasma magnesium concentrations as continuous variables and categorized into quartiles according to the distribution in the controls. Lower ORs for prediabetes and T2D were associated with higher plasma magnesium concentrations. After adjustment for age, sex, BMI, current smoking status, current alcohol drinking status, hypertension, family history of diabetes, and plasma calcium, the ORs (95% confidence interval (CI)) for prediabetes and T2D in the highest quartile compared with the lowest quartile of plasma magnesium were 0.51 (0.37–0.70) and 0.15 (0.11–0.20), P for trend < 0.001. Meanwhile, the adjusted ORs for prediabetes and T2D across 1 mg/l higher plasma magnesium were 0.90 (95% CI, 0.86–0.94) and 0.76 (0.73–0.79). In spline regression models, the odds of prediabetes and T2D decreased significantly with increasing magnesium concentrations at less than 22 mg/l, and no significant decline thereafter (Fig. 1). The nonlinear spline terms were not statistically significant (P > 0.05), indicating that the relationship between plasma magnesium concentration and T2D was nonlinear.
Table 2.
Associations of plasma magnesium concentration with prediabetes and T2D.
| Variables | Quartiles of plasma magnesium concentration (mg/l) | Per 1 mg/l of plasma magnesium | P value for trend | |||
|---|---|---|---|---|---|---|
| 1 (Lowest) | 2 | 3 | 4 (Highest) | |||
| ≤20.47 | 20.48–22.01 | 22.02–23.65 | ≥23.65 | |||
| Prediabetes vs . NGT | ||||||
| Model 1 | 1 | 0.56 (0.44–0.70) | 0.44 (0.34–0.56) | 0.44 (0.35–0.57) | 0.88 (0.86–0.91) | <0.001 |
| Model 2 | 1 | 0.55 (0.43–0.71) | 0.46 (0.36–0.60) | 0.47 (0.37–0.61) | 0.89 (0.86–0.93) | <0.001 |
| Model 3 | 1 | 0.57 (0.44–0.74) | 0.49 (0.37–0.65) | 0.51 (0.37–0.70) | 0.90 (0.86–0.94) | <0.001 |
| T2D vs . NGT | ||||||
| Model 1 | 1 | 0.30 (0.25–0.36) | 0.17 (0.14–0.22) | 0.19 (0.16–0.24) | 0.79 (0.77–0.82) | <0.001 |
| Model 2 | 1 | 0.29 (0.23–0.36) | 0.18 (0.14–0.22) | 0.19 (0.15–0.24) | 0.80 (0.77–0.82) | <0.001 |
| Model 3 | 1 | 0.26 (0.20–0.33) | 0.15 (0.12–0.20) | 0.15 (0.11–0.20) | 0.76 (0.73–0.79) | <0.001 |
Model 1, adjusted for age, sex and BMI. Model 2, adjusted for Model 1, current smoking status, current alcohol drinking status, family history of diabetes, and hypertension. Model 3, adjusted for Model 2 and plasma calcium.
Figure 1.
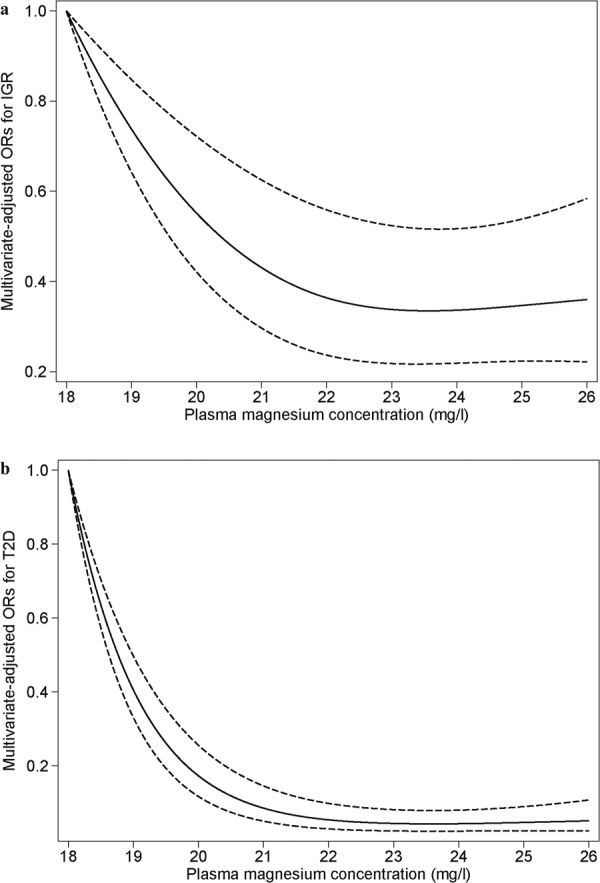
Adjusted ORs for prediabetes and T2D by plasma magnesium concentrations. Lines represent ORs (solid line) and 95% CIs (dashed line) based on restricted cubic splines for plasma magnesium concentrations. The analysis was adjusted for age, sex, BMI, current smoking status, current alcohol drinking status, family history of diabetes, hypertension and plasma calcium. (a) Adjusted ORs for prediabetes; (b) Adjusted ORs for T2D.
By stratifying data according to age, sex, BMI, family history of diabetes and hypertension, the inverse associations were consistently observed in all subgroups except the <50 years group for prediabetes (Table 3). Interaction effects were found between plasma magnesium concentration and sex (P < 0.001), age (P < 0.001), as well as between plasma magnesium concentration and hypertension (P = 0.031) for T2D; however, the reason for such interactions remains to be elucidated.
Table 3.
Adjusted ORs for each 1 mg/l increment of plasma magnesium associated with prediabetes and T2D in subgroups.
| Groups | % | Prediabetes | P for interaction | % | T2D | P for interaction |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Male | 59.7 | 0.91 (0.86–0.97) | 0.710 | 60.1 | 0.75 (0.71–0.79) | <0.001 |
| Female | 40.3 | 0.86 (0.80–0.93) | 39.9 | 0.75 (0.70–0.80) | ||
| Age | ||||||
| <50 | 40.3 | 0.99 (0.91–1.06) | 0.060 | 37.4 | 0.83 (0.78–0.88) | <0.001 |
| ≥50 | 59.7 | 0.87 (0.82–0.92) | 62.6 | 0.72 (0.68–0.76) | ||
| BMI | ||||||
| <24 | 51.7 | 0.89 (0.83–0.95) | 0.650 | 54.5 | 0.73 (0.68–0.77) | 0.075 |
| ≥24 | 48.3 | 0.91 (0.85–0.96) | 45.5 | 0.77 (0.73–0.82) | ||
| Family history of diabetes | ||||||
| Yes | 14.4 | 0.87 (0.77–0.98) | 0.233 | 11.1 | 0.73 (0.65–0.83) | 0.534 |
| No | 85.6 | 0.88 (0.84–0.93) | 88.9 | 0.76 (0.73–0.79) | ||
| Hypertension | ||||||
| Yes | 27.9 | 0.91 (0.84–0.99) | 0.792 | 25.9 | 0.80 (0.74–0.86) | 0.031 |
| No | 72.1 | 0.89 (0.84–0.94) | 74.1 | 0.73 (0.70–0.77) | ||
Models adjusted for age, sex, BMI, current smoking status, current alcohol drinking status, family history of diabetes, hypertension, and plasma calcium. The % in 2nd column represents the percent of each subgroup in the populations of prediabetes and NGT. The % in 5th column represents the percent of each subgroup in the populations of T2D and NGT.
Association of serum magnesium levels with hs-CRP
There was a consistent relation between hs-CRP levels and plasma magnesium in a subsample of 599 apparently healthy individuals study (Table 4). After adjustment for sex, age, BMI, hypertension and family history of diabetes, the geometric mean hs-CRP concentration for ascending quartiles of plasma magnesium were 1.31 (1.08–1.59), 1.17 (0.96–1.42), 0.99 (0.81–1.22), and 0.70 (0.57–0.86) mg/l. Although plasma calcium is highly correlated with plasma magnesium (correlation coefficient = 0.68, P < 0.001), further adjustment for plasma calcium did not attenuate the association between plasma magnesium and hs-CRP concentrations and the geometric mean hs-CRP concentration for ascending quartiles of plasma magnesium were 1.29 (1.06–1.57), 1.16 (0.95–1.41), 1.00 (0.81–1.22), and 0.71 (0.58–0.88) mg/l. All the tests for liner trend in every model were significant (P < 0.001).
Table 4.
Associations of inflammatory marker (CRP) with plasma magnesium levels in 599 apparently healthy individuals.
| Plasma CRP (mg/l) | Quartiles of plasma magnesium concentration (mg/l) | P value for trend | |||
|---|---|---|---|---|---|
| 1 (Lowest) | 2 | 3 | 4 (Highest) | ||
| Median of plasma magnesium | 18.85 | 20.86 | 22.43 | 25.07 | |
| Crude* | 1.21 (0.81–2.38) | 0.99 (0.59–1.74) | 0.95 (0.50–1.55) | 0.66 (0.32–1.33) | <0.001 |
| Model 1 | 1.38 (1.19–1.59) | 1.11 (0.96–1.29) | 0.94 (0.81–1.09) | 0.67 (0.58–0.78) | <0.001 |
| Model 2 | 1.31 (1.08–1.59) | 1.17 (0.96–1.42) | 0.99 (0.81–1.22) | 0.70 (0.57–0.86) | <0.001 |
| Model 3 | 1.29 (1.06–1.57) | 1.16 (0.95–1.41) | 1.00 (0.81–1.22) | 0.71 (0.58–0.88) | <0.001 |
CRP, C-reactive protein. *Data were presented as median (interquartilerange). Data were presented as adjusted geometric means (95% CI, unless noted otherwise). Model 1, adjusted for age, sex and BMI. Model 2, adjusted for Model 1, current smoking status, current alcohol drinking status, family history of diabetes, and hypertension. Model 3, adjusted for Model 2 and plasma calcium.
Discussion
In this study, after adjustment for potential confounding factors, the odds of prediabetes and T2D decreased significantly with increasing magnesium concentrations at less than 22 mg/l, and then no significant decline was observed. The inverse association remained consistent across different subgroups. Also, our subsample study in healthy subjects showed a consistent inverse association between plasma magnesium and plasma levels of hs-CRP.
In our study, the inverse association of plasma magnesium with prediabetes and T2D were both significant after multivariable adjustment. Our findings are generally consistent with results from some of the previous studies5–8, which showed lower serum magnesium in diabetic subjects than controls. However, none of the study contained more than 140 diabetic participants or reported a detailed dose-response analysis. Besides, the Atherosclerosis Risk in Communities (ARIC) study found an inverse association between serum magnesium levels and risk of T2D among white participants, but not among black participants9. Moreover, even among the white participants, the liner trend between serum magnesium levels and T2D could disappear after all multivariable adjustments. The inconsistent findings for the correlation of serum magnesium with diabetes may attribute to the difference in population, measurements of magnesium and diagnosis of diabetes. These studies were mainly conducted in Western populations that have been shown to have higher insulin resistance than Asians, and diagnosis of diabetes in these studies was different. In this study, as concerns of ORs for T2D, we found a significant interaction between plasma magnesium and sex and age. The interactions have not been assessed in previous studies and may warrant confirmation in further studies.
Our finding of an inverse association between plasma magnesium and hs-CRP levels was consistent with some previous studies. So far, findings on the association of magnesium and CRP levels are not consistent. Several cross-sectional studies reported an inverse association between dietary magnesium intake and CRP levels18–21. However, a cross-sectional study found no association between dietary magnesium intake and CRP levels22. Nevertheless, a recent meta-analysis based on cross-sectional studies and intervention studies indicated that dietary magnesium intake was inversely associated with serum CRP levels23. CRP, as a more sensitive and robust marker of systemic inflammation than other inflammatory markers24, has been proved as an independent predictor of risk for the development of T2D25,26. The inverse association between magnesium and C-reactive protein suggested that magnesium deficiency might be involved in the development of low chronic inflammatory syndrome, which can modulate diabetes27. These findings support the possible pathway for altering systemic inflammation and may explain, at least in part, the potential beneficial effect of high magnesium status on diabetes risk.
Several mechanisms, including facilitating insulin secretion and alleviating inflammation, have been proposed to explain the effect of plasma magnesium on diabetes pathogenesis28,29. Over 300 enzymes require the presence of magnesium ions for their catalytic action, including all enzymes utilizing or synthesizing adenosine triphosphate (ATP), and several enzymes that play an important role in glucose metabolism1,30. For example, intracellular magnesium deficiency may lead to decreasing tyrosine kinase activity of insulin receptors and to a post-receptorial impairment in insulin action, which may result in the development of insulin resistance2. Consistent with the effect of magnesium on insulin resistance, studies have found an inverse association of magnesium intake with fasting insulin level31, and HOMA-IR20,32, and Hruby et al. observed that magnesium intake was particularly beneficial in offsetting risk of developing diabetes among those at high risk33. Moreover, experimental findings showed that magnesium modulates cellular events involved in inflammation, because the molecular basis for inflammatory response is probably the result of modulation of intracellular calcium concentration, and magnesium could act as a natural calcium antagonist34,35. Consistently, an inverse association of CRP levels with magnesium intake or serum magnesium was reported in several epidemiological studies18–21, which suggested that magnesium deficiency might be involved in the development of low chronic inflammatory syndrome, which can modulate T2D25. Clinical trials have also suggested that magnesium supplementation downgraded inflammations in healthy or diabetic participants36–38, and could be effective in reducing plasma fasting glucose levels in people with diabetes and improving insulin-sensitivity parameters in people at high risk of diabetes39.
Our subjects with T2D were confined to the newly diagnosed and drug naive in order to exclude the effects of artificial interventions, because diabetes patients customarily take many measures to control blood glucose levels, and drugs can change the status of metabolism including magnesium1. Moreover, we defined diabetes based mainly on fasting and postprandial glucose levels from an oral glucose tolerance test (OGTT), and in our study, we tried to adjust for confounding factors influencing the association between plasma magnesium and diabetes, including plasma calcium.
Our study has several limitations. First, the cross-sectional nature of our study does not allow us to infer any causality between plasma magnesium and T2D, and plasma magnesium level may be reduced by the development of T2D40. Therefore, these findings should be confirmed in further prospective cohort studies. Second, our measurement of magnesium was confined to plasma compartment, accounting for roughly 1% of whole body magnesium level. Nonetheless, it has been suggested that if one with suspected magnesium deficiency, a low serum magnesium concentration is sufficient to confirm the diagnosis29. We used plasma magnesium concentration as a biomarker to measure magnesium status to avoid possible bias through dietary assessment, such as systematic measurement error in diet exposure and the influence of other nutrients on the bioavailability of magnesium41,42. In addition, all participants in this study were of Chinese Han ethnicity, which minimizes the confounding effects by ethnic background but doesn’t allow us to explore whether the association between plasma magnesium and diabetes is different between ethnicities.
In conclusion, this study demonstrates that plasma magnesium is independently and inversely associated with plasma hs-CRP and odds of newly diagnosed prediabetes and T2D. Further studies are warranted to confirm our findings and elucidate the mechanisms behind this association.
Methods
Study population
The study population consisted of 4447 participants: 867 newly diagnosed prediabetes, 1475 newly diagnosed T2D patients and 2105 normal glucose tolerance (NGT) individuals. The patients of newly diagnosed prediabetes and T2D were consecutively recruited from those for the first time attending the outpatient clinics of Department of Endocrinology, Tongji Medical College Hospital, Wuhan, China. Age- and sex-matched healthy NGT individuals were recruited from an unselected population undergoing a routine health check-up in the same hospital from 2007 to 2009. The inclusion criteria of NGT, newly diagnosed prediabetes and T2D were: age ≥30 years, body mass index (BMI) < 40 kg/m2, no history of a diagnosis of diabetes, not receiving pharmacological treatment for hyperlipidaemia or hypertension, and not taking medication known to affect glucose tolerance or insulin secretion. Patients with clinically significant neurological, endocrinological or other systemic diseases, as well as acute illness and chronic inflammatory or infective diseases, were excluded from the study. All the participants enrolled were of Chinese Han ethnicity.
This study was conducted in accordance with the Declaration of Helsinki and was approved by the ethics committee of the Tongji Medical College. Written informed consent was obtained from each participant.
Assessment of prediabetes and T2D
The definitions of prediabetes and T2D met the respective diagnostic criteria recommended by the World Health Organization in 199943. Prediabetes was defined as impaired fasting glucose (FPG ≥ 6.1 mmol/l and <7.0 mmol/l and 2-h post-glucose load <7.8 mmol/l) and/or impaired glucose tolerance (FPG < 7.0 mmol/l and 2-h post-glucose load ≥7.8 mmol/l and <11.1 mmol/l). T2D was diagnosed when FPG ≥ 7.0 mmol/l and/or 2-h post-glucose load ≥11.1 mmol/l.
Body composition and blood parameters
Personal information on demography was collected by using questionnaires, including sex, age, history of diseases (hypertension and hyperlipemia), family history of diabetes, current smoking status, and alcohol drinking status. Anthropometric data including height (m) and weight (kg) were measured with standardized techniques. BMI was calculated as weight divided by the square of height (kg/m2). Blood samples were collected in all participants after an overnight fast of at least 10 hours. All participants were given a standard 75 g glucose solution, and plasma glucose was measured at 0 and 2 hours after administration during the OGTT. FPI, total cholesterol, triglyceride, high-density lipoprotein cholesterol, and low-density lipoprotein cholesterol was measured within 2 hours, as described in our previous study44. Homoeostasis model assessment insulin resistance (HOMA-IR) score was computed using the following formula: FPI [m-units (milliunits)/l] × FPG (mmol/L)/22.5. The index of HOMA of β-cell function (HOMA-β) was calculated as (20 × FPI)/(FPG − 3.5)45.
Measurement of plasma magnesium concentrations and hs-CRP
Plasma magnesium concentrations were measured in the Ministry of Education Key Laboratory of Environment and Health at School of Public Health at Tongji Medical College of Huazhong University of Science and Technology using inductively coupled plasma mass spectrometry (ICP-MS) (Agilent 7700 Series, Japan). Plasma samples were stored at −80 °C, and thawed on ice. Working standard solutions were prepared by dilution of 1,000 mg/l calibration verification standard (Agilent P/N 5183–4682). For quality assurance, the CRM (certified reference material) ClinChek No. 8883 and No. 8884 human plasma controls were used. For No. 8883, we determined a concentration of: 17.0 ± 1.1 mg/l (certified: 16.9 ± 1.7 mg/l) and for No. 8884 we measured: 31.1 ± 1.7 mg/l (certified: 29.7 ± 3.0 mg/l). Quality control was performed (1 out of 20 samples), and the inter-assay and intra-assay coefficients of variation were <5% and <5%, respectively. Hs-CRP concentration was measured via high-sensitivity enzyme-linked immunosorbent assay.
Statistical analysis
Descriptive statistics were calculated for all demographic and clinical characteristics of the study subjects. To test for differences of characteristics among different glucose regulation status, continuous variables were compared using one-way ANOVA, and a Chi-square test was used for categorical variables. For calculation of the ORs for prediabetes and T2D, plasma magnesium concentrations were as continuous variables and categorized in quartiles according to the NGT group: category 1, ≤20.47 mg/l; category 2, 20.48–22.01 mg/l, category 3, 22.02–23.65 mg/l and category 4, ≥23.65 mg/l. Multinomial logistic regression analysis was used to assess the associations of prediabetes and T2D with plasma magnesium concentrations. ORs were adjusted for known risk factors for prediabetes and T2D, including age, sex, BMI, current smoking status (yes or no), and alcohol drinking (yes or no), hypertension, family history of diabetes and plasma calcium concentrations. Tests of linear trend across increasing quartiles of plasma magnesium were conducted by assigning the means of plasma magnesium in quartiles as continuous variables. Nonlinear relationships were examined using restricted cubic splines, excluding values outside the 5th and 95th percentiles via Stata version 12 (Stata Corp).
Then stratified analyses were conducted determining the ORs of prediabetes and diabetes with each 1 mg/l increment of plasma magnesium by age, sex, BMI, current smoking status, and alcohol drinking status, hypertension, and family history of diabetes. Likelihood ratio test was used to determine the interactions between the above variables and plasma magnesium. We examined the association between plasma magnesium concentration and plasma hs-CRP levels. A logarithmic transformation was used to improve the normality of hs-CRP distributions. Multiple linear regression models were used to control for the same potential confounding factors included in the logistic regression model. All data analyses were performed with SAS 9.1 (SAS Institute Inc. Cary, NC, USA). P values presented are two-tailed with a significant level at 0.05.
Acknowledgements
This study was funded by the National Science and Technology Support Program of China (2012BAI02B02), and Integrated Innovative Team for Major Human Disease Program of Tongji Medical College, HUST, Technique Innovation Program (Major Program) of Hubei Province of China (2016ACA136).
Author Contributions
S.C., X.J., J.L., T.S., M.X., W.B., X.Y., X.Y., Y.Z., H.Z., Z.S., and L.L. designed and conducted research. S.C. and Z.S. drafted the original manuscript; Z.S. analyzed the data; S.C., X.J., and T.S. contributed to the data collection; M.X., W.B., X.Y., X.Y., Y.Z., and H.Z. supervised the data analysis and commented on drafts; and L.L. had primary responsibility for final content. L.L. is the guarantor of this work and has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors read and approved the final manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Zhilei Shan, Email: shanzhilei3118@126.com.
Liegang Liu, Email: lgliu@mails.tjmu.edu.cn.
References
- 1.Saris NE, Mervaala E, Karppanen H, Khawaja JA, Lewenstam A. Magnesium. An update on physiological, clinical and analytical aspects. Clin Chim Acta. 2000;294:1–26. doi: 10.1016/S0009-8981(99)00258-2. [DOI] [PubMed] [Google Scholar]
- 2.Barbagallo M, Dominguez LJ. Magnesium metabolism in type 2 diabetes mellitus, metabolic syndrome and insulin resistance. Arch Biochem Biophys. 2007;458:40–47. doi: 10.1016/j.abb.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 3.Nichols GA, Hillier TA, Brown JB. Progression from newly acquired impaired fasting glusose to type 2 diabetes. Diabetes Care. 2007;30:228–233. doi: 10.2337/dc06-1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barr EL, et al. Risk of cardiovascular and all-cause mortality in individuals with diabetes mellitus, impaired fasting glucose, and impaired glucose tolerance: the Australian Diabetes, Obesity, and Lifestyle Study (AusDiab) Circulation. 2007;116:151–157. doi: 10.1161/CIRCULATIONAHA.106.685628. [DOI] [PubMed] [Google Scholar]
- 5.Xu J, et al. Associations of serum and urinary magnesium with the pre-diabetes, diabetes and diabetic complications in the Chinese Northeast population. PLoS One. 2013;8:e56750. doi: 10.1371/journal.pone.0056750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simmons D, Joshi S, Shaw J. Hypomagnesaemia is associated with diabetes: Not pre-diabetes, obesity or the metabolic syndrome. Diabetes Res Clin Pract. 2010;87:261–266. doi: 10.1016/j.diabres.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 7.Guerrero-Romero F, Rascon-Pacheco RA, Rodriguez-Moran M, de la Pena JE, Wacher N. Hypomagnesaemia and risk for metabolic glucose disorders: a 10-year follow-up study. Eur J Clin Invest. 2008;38:389–396. doi: 10.1111/j.1365-2362.2008.01957.x. [DOI] [PubMed] [Google Scholar]
- 8.Fang C, et al. Association of Serum Magnesium Level with Odds of Prediabetes and Diabetes in a Southern Chinese Population: a Prospective Nested Case-Control Study. Biol Trace Elem Res. 2016;172:307–314. doi: 10.1007/s12011-015-0594-y. [DOI] [PubMed] [Google Scholar]
- 9.Kao WH, et al. Serum and dietary magnesium and the risk for type 2 diabetes mellitus: the Atherosclerosis Risk in Communities Study. Arch Intern Med. 1999;159:2151–2159. doi: 10.1001/archinte.159.18.2151. [DOI] [PubMed] [Google Scholar]
- 10.Fang X, et al. Dietary magnesium intake and the risk of cardiovascular disease, type 2 diabetes, and all-cause mortality: a dose-response meta-analysis of prospective cohort studies. BMC Med. 2016;14:210. doi: 10.1186/s12916-016-0742-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fang, X. et al. Dose-Response Relationship between Dietary Magnesium Intake and Risk of Type 2 Diabetes Mellitus: A Systematic Review and Meta-Regression Analysis of Prospective CohortStudies. Nutrients 8, 10.3390/nu8110739 (2016). [DOI] [PMC free article] [PubMed]
- 12.Dong JY, Qin LQ. Dietary calcium intake and risk of type 2 diabetes: possible confounding by magnesium. Eur J Clin Nutr. 2012;66:408–410. doi: 10.1038/ejcn.2012.5. [DOI] [PubMed] [Google Scholar]
- 13.Pittas AG, Lau J, Hu FB, Dawson-Hughes B. The role of vitamin D and calcium in type 2 diabetes. A systematic review and meta-analysis. J Clin Endocrinol Metab. 2007;92:2017–2029. doi: 10.1210/jc.2007-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gagnon C, et al. Serum 25-hydroxyvitamin D, calcium intake, and risk of type 2 diabetes after 5 years: results from a national, population-based prospective study (the Australian Diabetes, Obesity and Lifestyle study) Diabetes Care. 2011;34:1133–1138. doi: 10.2337/dc10-2167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pittas AG, et al. Vitamin D and calcium intake in relation to type 2 diabetes in women. Diabetes Care. 2006;29:650–656. doi: 10.2337/diacare.29.03.06.dc05-1961. [DOI] [PubMed] [Google Scholar]
- 16.van Dam RM, Hu FB, Rosenberg L, Krishnan S, Palmer JR. Dietary calcium and magnesium, major food sources, and risk of type 2 diabetes in U.S. black women. Diabetes Care. 2006;29:2238–2243. doi: 10.2337/dc06-1014. [DOI] [PubMed] [Google Scholar]
- 17.Kirii K, et al. Calcium, vitamin D and dairy intake in relation to type 2 diabetes risk in a Japanese cohort. Diabetologia. 2009;52:2542–2550. doi: 10.1007/s00125-009-1554-x. [DOI] [PubMed] [Google Scholar]
- 18.Song Y, et al. Magnesium intake, C-reactive protein, and the prevalence of metabolic syndrome in middle-aged and older U.S. women. Diabetes Care. 2005;28:1438–1444. doi: 10.2337/diacare.28.6.1438. [DOI] [PubMed] [Google Scholar]
- 19.Chacko SA, et al. Relations of dietary magnesium intake to biomarkers of inflammation and endothelial dysfunction in an ethnically diverse cohort of postmenopausal women. Diabetes Care. 2010;33:304–310. doi: 10.2337/dc09-1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim DJ, et al. Magnesium intake in relation to systemic inflammation, insulin resistance, and the incidence of diabetes. Diabetes Care. 2010;33:2604–2610. doi: 10.2337/dc10-0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Song Y, Li TY, van Dam RM, Manson JE, Hu FB. Magnesium intake and plasma concentrations of markers of systemic inflammation and endothelial dysfunction in women. Am J Clin Nutr. 2007;85:1068–1074. doi: 10.1093/ajcn/85.4.1068. [DOI] [PubMed] [Google Scholar]
- 22.de Oliveira Otto MC, et al. Dietary micronutrient intakes are associated with markers of inflammation but not with markers of subclinical atherosclerosis. J Nutr. 2011;141:1508–1515. doi: 10.3945/jn.111.138115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dibaba DT, Xun P, He K. Dietary magnesium intake is inversely associated with serum C-reactive protein levels: meta-analysis and systematic review. Eur J Clin Nutr. 2014;68:510–516. doi: 10.1038/ejcn.2014.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rifai N, Ridker PM. High-sensitivity C-reactive protein: a novel and promising marker of coronary heart disease. Clin Chem. 2001;47:403–411. [PubMed] [Google Scholar]
- 25.Pradhan AD, Manson JE, Rifai N, Buring JE, Ridker PM. C-reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. JAMA. 2001;286:327–334. doi: 10.1001/jama.286.3.327. [DOI] [PubMed] [Google Scholar]
- 26.Wang X, et al. Inflammatory markers and risk of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2013;36:166–175. doi: 10.2337/dc12-0702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Donath MY, Shoelson SE. Type 2 diabetes as an inflammatory disease. Nat Rev Immunol. 2011;11:98–107. doi: 10.1038/nri2925. [DOI] [PubMed] [Google Scholar]
- 28.Weglicki WB. Hypomagnesemia and inflammation: clinical and basic aspects. Annu Rev Nutr. 2012;32:55–71. doi: 10.1146/annurev-nutr-071811-150656. [DOI] [PubMed] [Google Scholar]
- 29.Tosiello L. Hypomagnesemia and diabetes mellitus. A review of clinical implications. Arch Intern Med. 1996;156:1143–1148. doi: 10.1001/archinte.1996.00440100029005. [DOI] [PubMed] [Google Scholar]
- 30.Paolisso G, Scheen A, D’Onofrio F, Lefebvre P. Magnesium and glucose homeostasis. Diabetologia. 1990;33:511–514. doi: 10.1007/BF00404136. [DOI] [PubMed] [Google Scholar]
- 31.Song Y, Manson JE, Buring JE, Liu S. Dietary magnesium intake in relation to plasma insulin levels and risk of type 2 diabetes in women. Diabetes Care. 2004;27:59–65. doi: 10.2337/diacare.27.1.59. [DOI] [PubMed] [Google Scholar]
- 32.Cahill F, et al. High dietary magnesium intake is associated with low insulin resistance in the Newfoundland population. PLoS One. 2013;8:e58278. doi: 10.1371/journal.pone.0058278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hruby A, Meigs JB, O’Donnell CJ, Jacques PF, McKeown NM. Higher magnesium intake reduces risk of impaired glucose and insulin metabolism and progression from prediabetes to diabetes in middle-aged americans. Diabetes Care. 2014;37:419–427. doi: 10.2337/dc13-1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mazur A, et al. Magnesium and the inflammatory response: potential physiopathological implications. Arch Biochem Biophys. 2007;458:48–56. doi: 10.1016/j.abb.2006.03.031. [DOI] [PubMed] [Google Scholar]
- 35.Bussiere FI, et al. Increased phagocytosis and production of reactive oxygen species by neutrophils during magnesium deficiency in rats and inhibition by high magnesium concentration. Br J Nutr. 2002;87:107–113. doi: 10.1079/BJN2001498. [DOI] [PubMed] [Google Scholar]
- 36.Chacko SA, et al. Magnesium supplementation, metabolic and inflammatory markers, and global genomic and proteomic profiling: a randomized, double-blind, controlled, crossover trial in overweight individuals. Am J Clin Nutr. 2011;93:463–473. doi: 10.3945/ajcn.110.002949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nielsen FH, Johnson LK, Zeng H. Magnesium supplementation improves indicators of low magnesium status and inflammatory stress in adults older than 51 years with poor quality sleep. Magnes Res. 2010;23:158–168. doi: 10.1684/mrh.2010.0220. [DOI] [PubMed] [Google Scholar]
- 38.Moslehi N, Vafa M, Rahimi-Foroushani A, Golestan B. Effects of oral magnesium supplementation on inflammatory markers in middle-aged overweight women. J Res Med Sci. 2012;17:607–614. [PMC free article] [PubMed] [Google Scholar]
- 39.Veronese N, et al. Effect of magnesium supplementation on glucose metabolism in people with or at risk of diabetes: a systematic review and meta-analysis of double-blind randomized controlled trials. Eur J Clin Nutr. 2016;70:1354–1359. doi: 10.1038/ejcn.2016.154. [DOI] [PubMed] [Google Scholar]
- 40.Pham PC, Pham PM, Pham SV, Miller JM, Pham PT. Hypomagnesemia in patients with type 2 diabetes. Clin J Am Soc Nephrol. 2007;2:366–373. doi: 10.2215/CJN.02960906. [DOI] [PubMed] [Google Scholar]
- 41.Coudray C, et al. Dietary inulin intake and age can significantly affect intestinal absorption of calcium and magnesium in rats: a stable isotope approach. Nutr J. 2005;4:29. doi: 10.1186/1475-2891-4-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Coudray C, Demigne C, Rayssiguier Y. Effects of dietary fibers on magnesium absorption in animals and humans. J Nutr. 2003;133:1–4. doi: 10.1093/jn/133.1.1. [DOI] [PubMed] [Google Scholar]
- 43.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 44.Shan Z, et al. Interactions between Zinc Transporter-8 Gene (SLC30A8) and Plasma Zinc Concentrations for Impaired Glucose Regulation and Type 2 Diabetes. Diabetes. 2013;63:1796–1803. doi: 10.2337/db13-0606. [DOI] [PubMed] [Google Scholar]
- 45.Matthews DR, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]


