Abstract
Objectives
Preservation of both anterior and posterior cruciate ligaments in total knee arthroplasty (TKA) can lead to near-normal post-operative joint mechanics and improved knee function. We hypothesised that a patient-specific bicruciate-retaining prosthesis preserves near-normal kinematics better than standard off-the-shelf posterior cruciate-retaining and bicruciate-retaining prostheses in TKA.
Methods
We developed the validated models to evaluate the post-operative kinematics in patient-specific bicruciate-retaining, standard off-the-shelf bicruciate-retaining and posterior cruciate-retaining TKA under gait and deep knee bend loading conditions using numerical simulation.
Results
Tibial posterior translation and internal rotation in patient-specific bicruciate-retaining prostheses preserved near-normal kinematics better than other standard off-the-shelf prostheses under gait loading conditions. Differences from normal kinematics were minimised for femoral rollback and internal-external rotation in patient-specific bicruciate-retaining, followed by standard off-the-shelf bicruciate-retaining and posterior cruciate-retaining TKA under deep knee bend loading conditions. Moreover, the standard off-the-shelf posterior cruciate-retaining TKA in this study showed the most abnormal performance in kinematics under gait and deep knee bend loading conditions, whereas patient-specific bicruciate-retaining TKA led to near-normal kinematics.
Conclusion
This study showed that restoration of the normal geometry of the knee joint in patient-specific bicruciate-retaining TKA and preservation of the anterior cruciate ligament can lead to improvement in kinematics compared with the standard off-the-shelf posterior cruciate-retaining and bicruciate-retaining TKA.
Cite this article: Y-G. Koh, J. Son, S-K. Kwon, H-J. Kim, O-R. Kwon, K-T. Kang. Preservation of kinematics with posterior cruciate-, bicruciate- and patient-specific bicruciate-retaining prostheses in total knee arthroplasty by using computational simulation with normal knee model. Bone Joint Res 2017;6:557–565. DOI: 10.1302/2046-3758.69.BJR-2016-0250.R1.
Keywords: Patient-specific implant, Bicruciate-retaining total knee arthroplasty, Finite element analysis
Article focus
To what extent is patient-specific bicruciate-retaining total knee arthroplasty (TKA) biomechanically superior to conventional bicruciate-retaining TKA and posterior cruciate-retaining TKA?
Computational simulation was performed and kinematics were compared between normal and TKA knee joints to evaluate the biomechanical effect under gait and deep knee bend conditions.
Key messages
Patient-specific bicruciate-retaining TKA showed closer to normal kinematics, particularly in tibial posterior translation and internal rotation, when compared with other conventional TKAs under gait loading conditions.
Patient-specific bicruciate-retaining TKA normal kinematics were minimised for femoral rollback and internal-external rotation under deep knee bend conditions.
Strengths and limitations
Strength: Kinematics of patient-specific arthroplasty provides closer to normal knee kinematics under both gait and deep knee bend loading conditions.
Limitation: This is a finite element analysis study using a normal adult knee model, rather than patients with osteoarthritic knees.
Introduction
A major purpose of total knee arthroplasty (TKA) is the restoration of normal kinematics. However, this is rarely achieved because one or both cruciate ligaments may be sacrificed during the operation.1-3 The anterior cruciate ligament (ACL) is usually removed in TKA, although other options are now available that are aimed at either preserving or substituting the posterior cruciate ligament (PCL).4 While there have been many biomechanical, kinematic and clinical studies, there is still no consensus whether the PCL should be retained or replaced in patients undergoing TKA.5 In addition, the most posterior-stabilised prosthesis still does not restore normal kinematics, because of the absence of the ACL, even though PCL function has been replicated.3 Abnormal post-operative kinematics contribute to restriction in knee flexion, reduction of quadriceps efficiency, inferior functional outcome and increased pain, particularly from the anterior part of the knee.2-6 These abnormal kinematics are normally prevented by both the ACL and PCL, which are resected or disabled in TKA.2
As a result, alternative implant designs and surgical techniques have been suggested to improve abnormal kinematics and post-operative outcomes.7,8 Previous studies have shown that retention of the ACL leads to near-normal kinematics in the knee joint.9-11 Developing of a new prosthesis could provide patients with a more natural knee, a higher level of activity and greater patient satisfaction.12 In addition, the bicruciate-retaining TKA has theoretically improved longevity of the implant, by reducing stress transmitted through the prosthesis when using a less constrained polyethylene tibial insert.12 One such device, developed by Zimmer Biomet (Warsaw, Indiana), is now used clinically.13,14 In order to restore near-normal post-operative kinematics in TKA, next-generation materials and new surgical methods such as navigation, robotics and patient-specific instrumentation have been developed.15 In particular, patient-specific TKA has offset the disadvantages of standard, off-the-shelf TKA prostheses as it is able to restore near-normal anatomy.16-18 Other advantages of patient-specific TKA include optimised contact area and stress distribution on the resected surface of the bone and near-normal joint kinematics.16-18
However, there has been no report evaluating the biomechanical effects of cruciate-retaining TKA, bicruciate-retaining TKA, and patient-specific bicruciate-retaining TKA on kinematics. In this study, we have compared the kinematics in these different types of prosthesis with a normal healthy knee under gait and deep knee bend loading conditions, using finite element analysis. We hypothesised that patient-specific bicruciate-retaining TKA restores kinematics close to that of normal healthy knees because the design is based on normal knee anatomy and retains both cruciate ligaments.
Materials and Methods
Normal knee model
A 3D non-linear finite element model (FEM) of a normal healthy knee joint was developed using CT and MRI from a 36-year-old male subject. These were performed with a 64-channel CT scanner (Somatom Sensation 64; Siemens Healthcare GmbH, Erlangen, Germany) and a 3T MRI system (Discovery MR750w; GE Healthcare, Milwaukee, Wisconsin). The subject had no history of musculoskeletal disorders, nor any problems related to alignment in the tibiofemoral knee joint. This computational knee joint model has been described previously.19-22
The knee joint model was validated with previous cadaveric data, including analysing the pressure on the medial and lateral compartments, as well as kinematic evaluation at 20°, 40° and 60° of knee flexion.22 In addition, the contact area on the articular cartilage under weight-bearing conditions20 and kinematics from a laxity test21 were validated with identical subject and loading conditions to experiments in our previous study.
3D reconstruction was initially performed to develop the FEM. The CT and MRI images were segmented with software (Mimics 17.0; Materialise, Leuven, Belgium) to generate 3D lower extremity structures, which were combined with the positional alignment of each FEM by using Rapidform (3D Systems Korea Inc., Seoul, South Korea), in which the bony structure was assumed to be composed of rigid bodies.23 The articular cartilage and menisci were modelled as isotropic and transversely isotropic, respectively, with linear elastic material properties.24 To simulate meniscal attachments, each meniscal horn was fixed to bone using linear spring elements.24 In addition, the major ligaments were modelled with non-linear and tension-only spring elements.25-27 The force-displacement relationship based on the functional bundles in the actual ligament anatomy refers to the following:
where f(ε) is the current force, k is the stiffness, ε is the strain, and ε1 is assumed to be constant at 0.03. The ligament bundle slack length l0 can be calculated by using the reference bundle length lr and the reference strain εr in the upright reference position.
The interfaces between the articular cartilage and the bones were assumed to be fully bonded. Six pairs of tibiofemoral contacts between the femoral cartilage and the meniscus, the meniscus and the tibial cartilage, and the femoral cartilage and the tibial cartilage, were modelled for both the medial and lateral sides of the knee.19 A finite sliding frictionless hard-contact algorithm with no penetration was applied to all contacts in all articulations.19 Convergence was defined as a relative change of > 5% between two adjacent meshes. The mean element size of the simulated articular cartilage and menisci was 0.8 mm.
Design of posterior stabilised TKA
The patient-specific anatomy of the bony structure and surface data subjected to 3D reconstruction were used to develop the anatomy of patient-specific bicruciate-retaining TKA. By using Mimics, the 3D images were transformed to standard tessellation language files and imported into the digital computer-aided-design (CAD) software 3-Matic (Materialise). 3-Matic version 9.0 makes it possible to combine geometries from mixed sources into one project. The initial graphics exchange specification files exported from 3-Matic were imported into Unigraphics NX (Version 7.0; Siemens PLM Software, Torrance, California) to develop the patient-specific bicruciate-retaining TKA. The sagittal anatomy of the patient’s bone was fundamentally used for the geometry of the patient-specific femoral component.
The three patient-specific J curves for the trochlear grooves and the medial and lateral condyles from the patients’ normal articular anatomy were generated by the CAD software in this study.28-32 Planes were introduced into the condyles in the sagittal view, in which the anatomy of the articulating surfaces was extracted from the curves (Fig. 1). In general, the femur of a patient in the coronal plane provides asymmetric lateral and medial condyles that are defined as the coronal offset. These patient-specific differences were considered in the patient-specific femoral component design (Fig. 1). The coronal offset is defined as the difference in height between the medial and lateral femoral condyles in the coronal extension plane. This offset typically supports an asymmetric extension gap between the tibial articular surface and the posterior femoral condyles, which needs to be taken into account.33 The lateral posterior condyle is shorter than the medial condyle and also leads to an asymmetric flexion gap.33 These femoral J curves were matched with patient-specific polyethylene inserts, the perimeters of which corresponded to an individual tibial plateau that preserved the distal medial-lateral offset of the patient’s femoral condyles. This was achieved by the height of the patient-specific polyethylene insert and reflected the condylar offset maintaining the normal mechanical axis alignment. Patient-specific sagittal radii were also applied to the polyethylene inserts, which were derived from the sagittal J curves of the patient’s femoral condyles. The bone coverage was greater than 95% in patient-specific bicruciate-retaining TKA.31,33
Fig. 1.
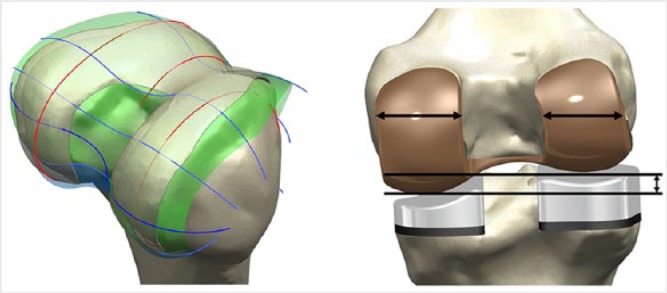
Procedure for patient-specific total knee arthroplasty (TKA) design in a) patient’s anatomical ‘J’ and spline curves, and b) restoration of the patient’s medial and lateral joint lines and condylar offsets in femoral component and corresponding polyethylene insert.
FEM for standard cruciate-retaining, bicruciate-retaining and patient-specific bicruciate-retaining TKA
The FEM for the three different TKAs were developed using a 3D laser scanner.34 A neutral position FEM was developed for both standard off-the-shelf TKA and bicruciate-retaining TKA by using the normal mechanical axes and ligaments from the normal knee model (Fig. 2). Genesis II (Smith & Nephew Inc., Memphis, Tennessee) and Vanguard XP (Zimmer Biomet) were the standard off-the-shelf and bicruciate-retaining implants used.
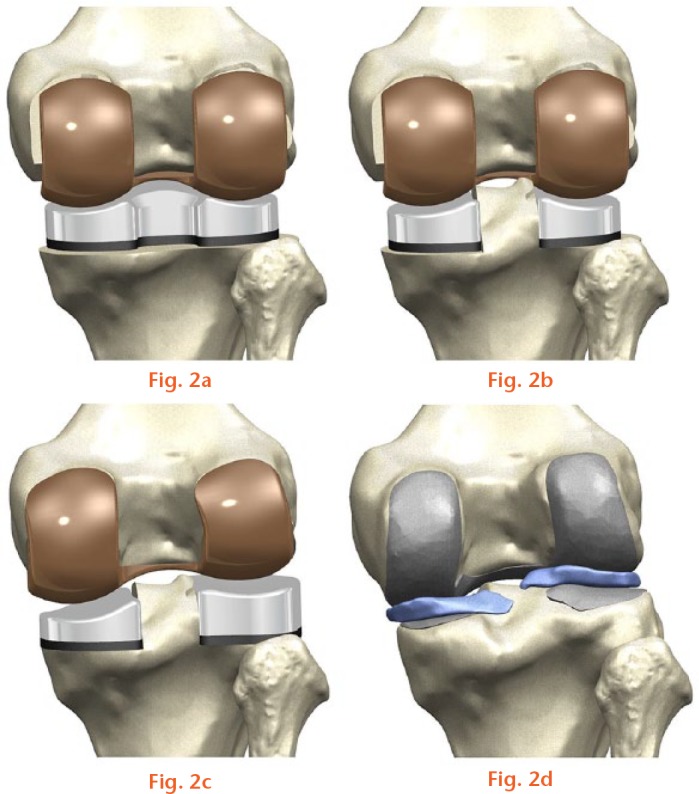
FEM used in analysis: a) standard off-the-shelf cruciate-retaining total knee arthroplasty (TKA); b) standard off-the-shelf bicruciate-retaining TKA; c) patient-specific bicruciate-retaining TKA; d) normal adult knee.
Contact conditions were applied between the femoral component, polyethylene insert and the patellar button in TKA. The coefficient of friction between the polyethylene and metal materials was assumed to be 0.04 for consistency with previous FEMs.35 The femoral component and tibial baseplate in the models were fully bonded to the femur and tibia to replicate the bone cement application.19 The materials for the femoral component, polyethylene insert and tibial baseplate have been previously described.35,36
The effect of the patient-specific design on the standard off-the-shelf TKA and on the bicruciate-retaining TKA, when anterior-posterior forces were applied to the femur during gait and deep knee bend loading conditions, was evaluated. The computational analysis was performed with an anterior-posterior force applied to the femur with respect to the compressive load applied to the hip.37-40 A proportional-integral-derivative (PID) controller was incorporated into the computational model to allow for the control of the quadriceps.41
The control system used to calculate the instantaneous quadriceps displacement required to match a target flexion profile was the same as in the experimental group.41 Internal-external and varus-valgus torques were applied to the tibia.37-40 FEMs were analysed by using Abaqus software (Version 6.11; Dassault Systèmes Simulia Corp., Providence, Rhode Island). In order to investigate the biomechanical similarity of patient-specific bicruciate-retaining TKA to the kinematics of the normal healthy knee, certain measurements were performed. These included anterior-posterior translations and internal-external rotations of the tibia in the standard off-the-shelf cruciate-retaining, bicruciate-retaining and patient-specific bicruciate-retaining TKA, and also in a normal healthy knee, notably under gait and deep knee bend loading conditions.
A three-cylindrical knee joint model was developed in six degrees of freedom (6DoF) for relative kinematics of the tibiofemoral and patellofemoral articulations.42 Embedded coordinate frames in the femur, tibia and patella were considered using nodes, and their positions were evaluated throughout the loading conditions.
Results
Kinematics in the four different knee models by FEM
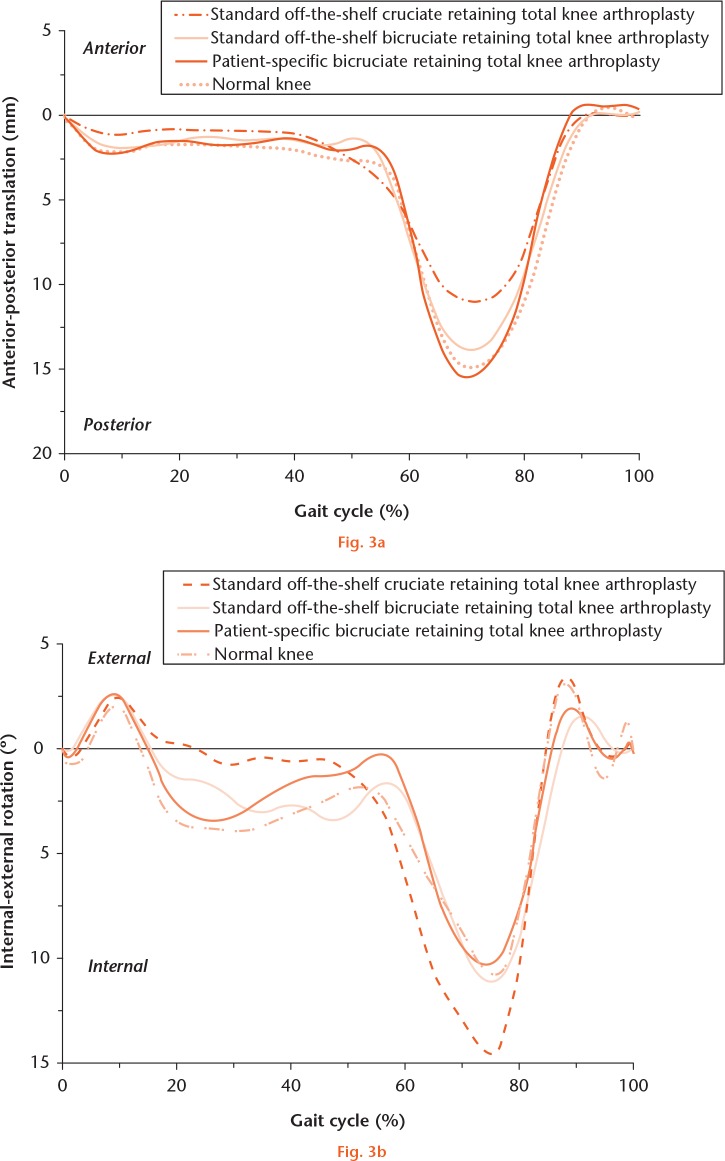
Figure 3 shows the anterior-posterior translations and internal-external rotations of the tibia in standard off-the-shelf cruciate-retaining and bicruciate-retaining TKA, in patient-specific bicruciate-retaining TKA, and in a normal healthy knee under gait loading conditions.
Evaluations of a) anterior-posterior tibial translation, and b) internal-external tibial rotation in standard off-the-shelf cruciate-retaining total knee arthroplasty (TKA), standard off-the-shelf bicruciate-retaining TKA, patient-specific bicruciate-retaining TKA and a normal adult knee, under gait loading conditions.
The post-operative patterns of tibial anterior-posterior kinematics in standard off-the-shelf cruciate-retaining TKA were not matched with a normal healthy knee under gait loading conditions (Fig. 3a). However, the tibial anterior-posterior translation in standard off-the-shelf bicruciate-retaining TKA and patient-specific bicruciate-retaining TKA resembled the patterns in a normal healthy knee under gait loading conditions (Fig. 3a). The tibial posterior translation in all three TKAs was less than in a normal healthy knee under gait loading conditions. Anterior-posterior tibial translation in the anterior direction was greater by 4.1 mm, 2.9 mm and 1.3 mm, respectively, compared with a normal healthy knee, in standard off-the-shelf cruciate-retaining TKA, standard off-the-shelf bicruciate-retaining TKA, and patient-specific bicruciate-retaining TKA during the swing phase (Fig. 3a).
The internal rotation in standard off-the-shelf cruciate-retaining TKA was less in the stance phase, but greater in the swing phase, compared with a normal healthy knee (Fig. 3b). However, in both standard off-the-shelf bicruciate-retaining TKA and patient-specific bicruciate-retaining TKA, the internal rotation was continuously less than that in a normal healthy knee during the gait cycle (Fig. 3b). The maximum differences in internal rotation from a normal healthy knee were 2.3° and 1.2°, respectively, in standard off-the-shelf bicruciate-retaining TKA and patient-specific bicruciate-retaining TKA during the gait cycle. Overall, the kinematics of anterior-posterior translation and internal-external rotation were well matched between patient-specific bicruciate-retaining TKA and a normal healthy knee under gait loading conditions (Fig. 3).
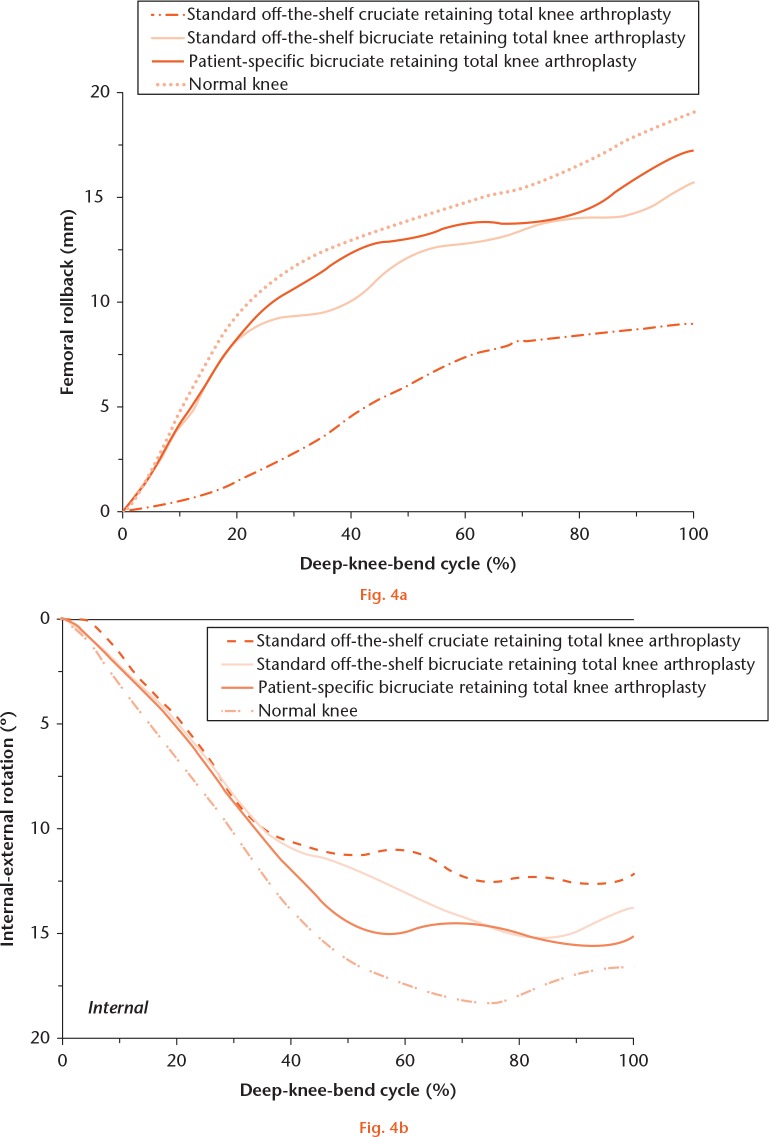
Figure 4 shows the rollback of the femur and internal-external rotation of the tibia in standard off-the-shelf cruciate-retaining and bicruciate-retaining TKA, in patient-specific bicruciate-retaining TKA and in a normal healthy knee under deep knee bend conditions. The kinematics of the knees implanted with patient-specific bicruciate-retaining TKA provided near-normal femoral rollback, with a difference of 1.4 mm, but the differences were 4.9 mm and 9.8 mm in standard off-the-shelf bicruciate-retaining and cruciate-retaining TKA, respectively, compared with a normal healthy knee under deep knee bend loading conditions (Fig. 4a).
Comparison of kinematics for a) femoral rollback rotation, and b) internal-external tibial rotation in standard off-the-shelf cruciate-retaining total knee arthroplasty (TKA), standard off-the-shelf bicruciate-retaining TKA, patient-specific bicruciate-retaining TKA and normal knee under deep knee bend loading conditions.
Tibial internal rotation was less in all standard off-the-shelf bicruciate-retaining and cruciate-retaining TKA, and patient-specific bicruciate-retaining TKA, compared with a normal healthy knee, under deep knee bend conditions. The differences in tibial rotation were smaller by 1.4°, 3.4° and 5.8°, compared with a normal healthy knee, in patient-specific bicruciate-retaining TKA, standard off-the-shelf bicruciate-retaining TKA, and standard off-the-shelf cruciate-retaining TKA, respectively, under deep knee bend conditions (Fig. 4b).
Discussion
Factors such as the surgical procedure, design of the prosthesis and daily activities can affect post-operative kinematics of the knee following TKA.43-45 Currently the bicruciate-retaining TKA is considered to be the optimal method, because of the weakness of cruciate-retaining and posterior-stabilising TKA.12 Johnson et al46 evaluated the integrity of the ACL in 200 patients undergoing TKA and found that 78% of patients had an intact ACL at operation, while 69% were intact on MRI. However, Cushner et al47 found that only 26% of ACL were still intact in osteoarthritic patients.
Bicruciate-retaining TKA was developed in the 1960s to prevent eccentric motion and degradation, and also to maintain the structural integrity in the replaced knee joint.37 In 1966, Gunston48,49 introduced a resurfacing technique for femoral condyles and tibial plateaus by using cemented prosthetic implants that preserved both collateral and cruciate ligaments and improved knee stability resulting in normal knee joint biomechanics. Unfortunately, the early designs of bicruciate-retaining TKA led to prosthetic loosening due in part to the more demanding surgical technique.50 However, the design of the bicruciate-retaining TKA has now improved.51
The aim of these advanced prosthetic designs is the restoration of normal knee function, by preserving the ligaments in the knee joint, particularly the ACL.45,52 Patients who have undergone bicruciate-retaining TKA have near-normal function and flexibility, thus providing better anterior stability to the knee joint.52 The main finding of our study was that bicruciate-retaining TKA showed near-normal kinematics compared with cruciate-retaining TKA; however, the nearest to normal kinematics were observed in the patient-specific bicruciate-retaining TKA.
During the gait cycle, the standard off-the-shelf bicruciate-retaining TKA and patient-specific bicruciate-retaining TKA showed less internal tibial rotation and greater posterior translation, compared with standard off-the-shelf cruciate-retaining TKA. The standard off-the-shelf bicruciate-retaining TKA and patient-specific bicruciate-retaining TKA both showed reduced external rotation in the swing phase, due to the presence of the ACL. Andriacchi et al53 reported a mean tibial external rotation of 2.9° less in the ACL deficient knee in kinematics evaluation when compared with a normal healthy knee, which is similar to our findings. On the other hand, standard off-the-shelf cruciate-retaining TKA resulted in abnormal kinematics, particularly during the swing phase, under gait loading conditions. Internal rotation in standard off-the-shelf cruciate-retaining TKA was less in the stance phase and greater in the swing phase compared with a normal healthy knee under gait loading conditions. This rotational tendency could be caused by three factors: 1) tibial baseplate alignment, 2) polyethylene insert geometry, or 3) integrity of the ACL.45 Internal rotation was dependent on the conformity of the anatomy during the stance phase, but an ACL that was removed in standard off-the-shelf cruciate-retaining TKA was an important factor during the swing phase, where there is no axial load, under gait loading conditions. In addition, the kinematic patterns in standard off-the-shelf cruciate-retaining and bicruciate-retaining TKA in our study were well matched with previous reports.9,54 In contrast, Moro-oka et al45 reported that bicruciate-retaining TKA resulted in greater posterior translation and internal rotation than cruciate-retaining TKA. However, they also acknowledged that the surgical technique for bicruciate-retaining TKA is more complicated than that for cruciate-retaining TKA.45
In a normal healthy knee, the tension exerted on the ACL maintains the lateral femoral condyle anteriorly in extension.55 In mid-flexion, both the ACL and PCL are active, whereas only the PCL is a factor in posterior rollback with greater flexion under deep knee bend loading conditions. This finding was also supported by our FEM of ACL function in anterior translation of the femur with less flexion, and PCL in femoral rollback with moderate to high flexion.56
Femoral rollback patterns were close to those of a normal healthy knee in the standard off-the-shelf bicruciate-retaining and patient-specific bicruciate-retaining TKA in mid-flexion range, particularly for patient-specific bicruciate-retaining TKA in which the anatomy of the patient was directly applied. In the patient-specific bicruciate-retaining TKA, the anatomical convexity of the lateral tibial articular anatomy is restored with ACL preservation, which generates a normal femoral rollback pattern. This contrasts with standard off-the-shelf bicruciate-retaining TKA, where the asymmetry of the tibial articular surface, especially for the lateral convexity, was not restored.
There was less internal rotation in all standard off-the-shelf cruciate-retaining and bicruciate-retaining TKAs and in patient-specific bicruciate-retaining TKA, compared with a normal healthy knee under deep knee bend loading conditions. Nevertheless, standard off-the-shelf bicruciate-retaining TKA and patient-specific bicruciate-retaining TKA showed kinematics that were relatively close to those of a normal healthy knee, although not identical. This could be due to stiffness influencing the kinematics and mechanics of the knee joint.
This study has limitations. First, the anatomy and TKA design were only virtually implanted in one knee. However, the advantage of a computational simulation using a single knee is that we were able to determine the effects of component alignment within the same subject without the effect of variables such as weight, height, bony geometry, ligament properties, and component size.57 Second, the TKA had been fully bonded and the effect of micromotion occurring between the tibial baseplate and the polyethylene insert was not considered in our study. Third, the intact FEM has not been validated for TKA, although this approach has been widely accepted in computational studies in orthopaedic biomechanics.19,23,24,34,36,58 Fourth, the bony structure was assumed to be a rigid body, but bone is not rigid, being composed of cortical and cancellous bone. However, the effect of rigidity had minimal influence on our study, as bone has greater stiffness than the related soft tissues.23 Fifth, our findings that restoration of the normal anatomy of the knee joint in patient-specific bicruciate-retaining TKA and preservation of the ACL lead to improvement in kinematics is only valid in the normal knee. Sixth, although the stiffness, length patterns and slack for each ligament were adjusted from the relevant anatomical literature, our model does not represent a true simulation of TKA, especially because of the variety of deformities that can occur in patients with osteoarthritis, for which there is no definitive data. Finally, the actual condition of the ACL or PCL were assumed to be identical to that found in the normal knee, but in patients who undergo TKA, these ligaments would not have been as good as in a normal healthy knee.
In conclusion, the kinematics of patient-specific bicruciate-retaining TKA, standard off-the-shelf cruciate-retaining and bicruciate-retaining TKA have been compared with that of a normal healthy knee, in order to evaluate the biomechanical effects of ACL preservation and patient-specific design on post-operative outcomes in TKA. The results showed that restoration of the normal geometry of the knee joint in patient-specific bicruciate-retaining TKA with preservation of the ACL may lead to remarkable improvements in kinematics compared with the standard off-the-shelf cruciate-retaining and bicruciate-retaining TKA. However, it needs to be stated that it is still unclear whether restoration of normal knee kinematics should be the ultimate goal in the osteoarthritic knee.15
Footnotes
Author Contribution: Y-G. Koh: Co-first author, Designing the study, Writing the paper, Data analysis, Surgical simulation
J. Son: Co-first author, Designing the study, Writing the paper, 3D model development
S-K. Kwon: Data analysis
H-J. Kim: Data analysis
O-R. Kwon: Co-corresponding author, Supervising the study, Data analysis, Surgical simulation
K-T. Kang: Co-corresponding author, Supervising the study, FEA result evaluation
Conflicts of Interest Statement: None declared
Funding Statement
None declared
References
- 1. de Jong RJ, Heesterbeek PJ, Wymenga AB. A new measurement technique for the tibiofemoral contact point in normal knees and knees with TKR. Knee Surg Sports Traumatol Arthrosc 2010;18:388-393. [DOI] [PubMed] [Google Scholar]
- 2. van Duren BH, Pandit H, Price M, et al. Bicruciate substituting total knee replacement: how effective are the added kinematic constraints in vivo? Knee Surg Sports Traumatol Arthrosc 2012;20:2002-2010. [DOI] [PubMed] [Google Scholar]
- 3. Ward TR, Burns AW, Gillespie MJ, Scarvell JM, Smith PN. Bicruciate-stabilised total knee replacements produce more normal sagittal plane kinematics than posterior-stabilised designs. J Bone Joint Surg [Br] 2011;93-B:907-913. [DOI] [PubMed] [Google Scholar]
- 4. Lo J, Müller O, Dilger T, Wülker N, Wünschel M. Translational and rotational knee joint stability in anterior and posterior cruciate-retaining knee arthroplasty. Knee 2011;18:491-495. [DOI] [PubMed] [Google Scholar]
- 5. Bellemans J, Corten K, Vanlauwe J, Vandenneucker H. Bicruciate retaining TKA: The future? In: Bonnin M, Amendola A, Bellemans J, MacDonald S, Ménétrey J, eds. The Knee Joint: Surgical Techniques and Strategies. Paris: Springer, 2012:735-739. [Google Scholar]
- 6. Conditt MA, Noble PC, Bertolusso R, Woody J, Parsley BS. The PCL significantly affects the functional outcome of total knee arthroplasty. J Arthroplasty 2004;19(Suppl 2):107-112. [DOI] [PubMed] [Google Scholar]
- 7. Andriacchi TP. Functional analysis of pre and post-knee surgery: total knee arthroplasty and ACL reconstruction. J Biomech Eng 1993;115:575-581. [DOI] [PubMed] [Google Scholar]
- 8. Christensen JC, Brothers J, Stoddard GJ, et al. Higher frequency of reoperation with a new bicruciate-retaining total knee arthroplasty. Clin Orthop Relat Res 2017;475:62-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Halewood C, Traynor A, Bellemans J, Victor J, Amis AA. Anteroposterior laxity after bicruciate-retaining total knee arthroplasty is closer to the native knee than ACL-resecting TKA: A biomechanical cadaver study. J Arthroplasty 2015;30:2315-2319. [DOI] [PubMed] [Google Scholar]
- 10. Komistek RD, Allain J, Anderson DT, Dennis DA, Goutallier D. In vivo kinematics for subjects with and without an anterior cruciate ligament. Clin Orthop Relat Res 2002;404:315-325. [DOI] [PubMed] [Google Scholar]
- 11. Stiehl JB, Komistek RD, Cloutier JM, Dennis DA. The cruciate ligaments in total knee arthroplasty: a kinematic analysis of 2 total knee arthroplasties. J Arthroplasty 2000;15:545-550. [DOI] [PubMed] [Google Scholar]
- 12. Cherian JJ, Kapadia BH, Banerjee S, et al. Bicruciate-retaining total knee arthroplasty: a review. J Knee Surg 2014;27:199-205. [DOI] [PubMed] [Google Scholar]
- 13. No authors listed. Hvidovre University Hospital. Comparison of Vanguard XP and Vanguard CR total knee arthroplasties. A trial evaluating early component migration by RSA and patient reported outcome. 2014. https://clinicaltrials.gov/ct2/show/NCT01966848 (date last accessed 12 September 2017).
- 14. DeClaire JH. Bicruciate TKA: science and development. 5th Annual Modern Trends in Joint Replacement, 2013. https://icjr.net/meeting/2013-5th-annual-modern-trends-in-joint-replacement-mtjr (date last accessed 12 September 2017).
- 15. Zumbrunn T, Varadarajan KM, Rubash HE, et al. Regaining native knee kinematics following joint arthroplasty: a novel biomimetic design with ACL and PCL preservation. J Arthroplasty 2015;30:2143-2148. [DOI] [PubMed] [Google Scholar]
- 16. Carpenter DP, Holmberg RR, Quartulli MJ, Barnes CL. Tibial plateau coverage in UKA: a comparison of patient specific and off-the-shelf implants. J Arthroplasty 2014;29:1694-1698. [DOI] [PubMed] [Google Scholar]
- 17. Schwechter EM, Fitz W. Design rationale for customized TKA: a new idea or revisiting the past? Curr Rev Musculoskelet Med 2012;5:303-308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zeller IM, Sharma A, Kurtz WB, Anderle MR, Komistek RD. Customized versus patient-sized cruciate-retaining total knee arthroplasty: an in vivo kinematics study using mobile fluoroscopy. J Arthroplasty 2017;32:1344-1350. [DOI] [PubMed] [Google Scholar]
- 19. Kwon OR, Kang KT, Son J, et al. Importance of joint line preservation in unicompartmental knee arthroplasty: finite element analysis. J Orthop Res 2017;35:347-352. [DOI] [PubMed] [Google Scholar]
- 20. Kang KT, Kim SH, Son J, et al. Probabilistic evaluation of the material properties of the in vivo subject-specific articular surface using a computational model. J Biomed Mater Res B Appl Biomater 2017;105:1390-1400. [DOI] [PubMed] [Google Scholar]
- 21. Kang KT, Kim SH, Son J, Lee YH, Chun HJ. Computational model-based probabilistic analysis of in vivo material properties for ligament stiffness using the laxity test and computed tomography. J Mater Sci Mater Med 2016;27:183. [DOI] [PubMed] [Google Scholar]
- 22. Kim YS, Kang KT, Son J, et al. Graft extrusion related to the position of allograft in lateral meniscal allograft transplantation: biomechanical comparison between parapatellar and transpatellar approaches using finite element analysis. Arthroscopy 2015;31:2380-2391.e2. [DOI] [PubMed] [Google Scholar]
- 23. Peña E, Calvo B, Martinez MA, Palanca D, Doblaré M. Why lateral meniscectomy is more dangerous than medial meniscectomy. A finite element study. J Orthop Res 2006;24:1001-1010. [DOI] [PubMed] [Google Scholar]
- 24. Haut Donahue TL, Hull ML, Rashid MM, Jacobs CR. How the stiffness of meniscal attachments and meniscal material properties affect tibio-femoral contact pressure computed using a validated finite element model of the human knee joint. J Biomech 2003;36:19-34. [DOI] [PubMed] [Google Scholar]
- 25. Mesfar W, Shirazi-Adl A. Biomechanics of the knee joint in flexion under various quadriceps forces. Knee 2005;12:424-434. [DOI] [PubMed] [Google Scholar]
- 26. Takeda Y, Xerogeanes JW, Livesay GA, Fu FH, Woo SL. Biomechanical function of the human anterior cruciate ligament. Arthroscopy 1994;10:140-147. [DOI] [PubMed] [Google Scholar]
- 27. Blankevoort L, Huiskes R. Validation of a three-dimensional model of the knee. J Biomech 1996;29:955-961. [DOI] [PubMed] [Google Scholar]
- 28. No authors listed. ConforMIS. Image-to-Implant Process. http://www.conformis.com/customized-knee-implants/image-to-implant-process (date last accessed 12 September 2017).
- 29. Kamal R, Kumar DA. Three-dimensional (3D) modeling of the knee and designing of custom made knee implant using mimics software. IJCET 2013;3:327-330. [Google Scholar]
- 30. Harrysson OL, Hosni YA, Nayfeh JF. Custom-designed orthopedic implants evaluated using finite element analysis of patient-specific computed tomography data: femoral-component case study. BMC Musculoskelet Disord 2007;8:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Steklov N, Slamin J, Srivastav S, D’Lima D. Unicompartmental knee resurfacing: enlarged tibio-femoral contact area and reduced contact stress using novel patient-derived geometries. Open Biomed Eng J 2010;4:85-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. van den Heever DJ, Scheffer C, Erasmus P, Dillon E. Contact stresses in a patient-specific unicompartmental knee replacement. Clin Biomech 2011;26:159-166. [DOI] [PubMed] [Google Scholar]
- 33. Kurtz WB, Slamin JE, Doody SW. Bone preservation in a novel patient specific total knee replacement. Reconstr Rev 2016;6:23-29. [Google Scholar]
- 34. Kwon OR, Kang KT, Son J, et al. Biomechanical comparison of fixed- and mobile-bearing for unicompartmental knee arthroplasty using finite element analysis. J Orthop Res 2014;32:338-345. [DOI] [PubMed] [Google Scholar]
- 35. Godest AC, Beaugonin M, Haug E, Taylor M, Gregson PJ. Simulation of a knee joint replacement during a gait cycle using explicit finite element analysis. J Biomech 2002;35:267-275. [DOI] [PubMed] [Google Scholar]
- 36. Innocenti B, Truyens E, Labey L, et al. Can medio-lateral baseplate position and load sharing induce asymptomatic local bone resorption of the proximal tibia? A finite element study. J Orthop Surg Res 2009;4:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Baldwin MA, Clary C, Maletsky LP, Rullkoetter PJ. Verification of predicted specimen-specific natural and implanted patellofemoral kinematics during simulated deep knee bend. J Biomech 2009;42:2341-2348. [DOI] [PubMed] [Google Scholar]
- 38. Kutzner I, Heinlein B, Graichen F, et al. Loading of the knee joint during activities of daily living measured in vivo in five subjects. J Biomech 2010;43:2164-2173. [DOI] [PubMed] [Google Scholar]
- 39. Halloran JP, Clary CW, Maletsky LP, et al. Verification of predicted knee replacement kinematics during simulated gait in the Kansas knee simulator. J Biomech Eng 2010;132:081010. [DOI] [PubMed] [Google Scholar]
- 40. Patil S, Bunn A, Bugbee WD, Colwell CW, Jr, D’Lima DD. Patient-specific implants with custom cutting blocks better approximate natural knee kinematics than standard TKA without custom cutting blocks. Knee 2015;22:624-629. [DOI] [PubMed] [Google Scholar]
- 41. Kang KT, Koh YG, Jung M, et al. The effects of posterior cruciate ligament deficiency on posterolateral corner structures under gait- and squat-loading conditions: A computational knee model. Bone Joint Res 2017;6:31-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 1983;105:136-144. [DOI] [PubMed] [Google Scholar]
- 43. Banks SA, Hodge WA. 2003 Hap Paul Award Paper of the International Society for Technology in Arthroplasty. Design and activity dependence of kinematics in fixed and mobile-bearing knee arthroplasties. J Arthroplasty 2004;19:809-816. [DOI] [PubMed] [Google Scholar]
- 44. Banks SA, Hodge WA. Implant design affects knee arthroplasty kinematics during stair-stepping. Clin Orthop Relat Res 2004;426:187-193. [DOI] [PubMed] [Google Scholar]
- 45. Moro-oka TA, Muenchinger M, Canciani JP, Banks SA. Comparing in vivo kinematics of anterior cruciate-retaining and posterior cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2007;15:93-99. [DOI] [PubMed] [Google Scholar]
- 46. Johnson AJ, Howell SM, Costa CR, Mont MA. The ACL in the arthritic knee: how often is it present and can preoperative tests predict its presence? Clin Orthop Relat Res 2013;471:181-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cushner FD, La Rosa DF, Vigorita VJ, et al. A quantitative histologic comparison: ACL degeneration in the osteoarthritic knee. J Arthroplasty 2003;18:687-692. [DOI] [PubMed] [Google Scholar]
- 48. Gunston FH. Polycentric knee arthroplasty. Prosthetic simulation of normal knee movement. J Bone Joint Surg [Br] 1971;53-B:272-277. [PubMed] [Google Scholar]
- 49. Bryan RS, Peterson LF, Combs JJ., Jr Polycentric knee arthroplasty. A review of 84 patients with more than one year follow-up. Clin Orthop Relat Res 1973;94:136-139. [PubMed] [Google Scholar]
- 50. Lombardi AV, Jr, McClanahan AJ, Berend KR. The bicruciate retaining TKA: two is better than one. Semin Arthroplasty 2015;26:51-58. [Google Scholar]
- 51. Mont MA, John M, Johnson A. Bicruciate retaining arthroplasty. Surg Technol Int 2012;22:236-242. [PubMed] [Google Scholar]
- 52. Dennis DA, Komistek RD, Mahfouz MR, Walker SA, Tucker A. A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res 2004;428:180-189. [DOI] [PubMed] [Google Scholar]
- 53. Andriacchi TP, Dyrby CO. Interactions between kinematics and loading during walking for the normal and ACL deficient knee. J Biomech 2005;38:293-298. [DOI] [PubMed] [Google Scholar]
- 54. Varadarajan KM, Harry RE, Johnson T, Li G. Can in vitro systems capture the characteristic differences between the flexion-extension kinematics of the healthy and TKA knee? Med Eng Phys 2009;31:899-906. [DOI] [PubMed] [Google Scholar]
- 55. Johal P, Williams A, Wragg P, Hunt D, Gedroyc W. Tibio-femoral movement in the living knee. A study of weight bearing and non-weight bearing knee kinematics using ‘interventional’ MRI. J Biomech 2005;38:269-276. [DOI] [PubMed] [Google Scholar]
- 56. Blankevoort L, Huiskes R, de Lange A. Recruitment of knee joint ligaments. J Biomech Eng 1991;113:94-103. [DOI] [PubMed] [Google Scholar]
- 57. Thompson JA, Hast MW, Granger JF, Piazza SJ, Siston RA. Biomechanical effects of total knee arthroplasty component malrotation: a computational simulation. J Orthop Res 2011;29:969-975. [DOI] [PubMed] [Google Scholar]
- 58. Kim HJ, Kang KT, Son J, et al. The influence of facet joint orientation and tropism on the stress at the adjacent segment after lumbar fusion surgery: a biomechanical analysis. Spine J 2015;15:1841-1847. [DOI] [PubMed] [Google Scholar]