Abstract
Chronic pain has been linked to depression among individuals and their partners. Yet, little is known about long-term mutual influences between pain intensity and depressive symptoms within couples as they age. Using a nationally representative U.S. sample of wives and husbands aged 50 and older (mean = 64.53, SD = 7.86), this study explored the links between own and partner pain intensity and depressive symptoms across an 8-year period. A total of 963 heterosexual married couples drawn from the Health and Retirement Study completed interviews biennially from 2006 to 2014. Dyadic growth curve models examined mutual associations within couples and controlled for sociodemographic characteristics, length of marriage, and marital quality, along with self-rated health, number of chronic health conditions, and functional disability. For wives and husbands, their own greater baseline pain intensity was significantly linked to their own higher levels of depressive symptoms. Unexpectedly, wives with greater baseline pain intensity reported decreases in their depressive symptoms over time. There were also partner effects such that husbands’ greater pain intensity at baseline was associated with increases in wives’ depressive symptoms over time. Findings highlight the importance of considering both individual and spousal associations between pain intensity and depressive symptoms in later life. Understanding how individual and couple processes unfold may yield critical insights for the development of intervention and prevention efforts to maintain mental health among older chronic pain patients and their spouses.
Introduction
Chronic pain conditions are highly prevalent in older ages, with bothersome pain reported by more than half of community-dwelling adults ages 65 and older from large, nationally representative samples [53]. Persistent pain has widespread negative repercussions in later life such as reduced engagement in meaningful activities, social isolation, sleep deprivation, and obesity [46]. Consequently, it is critical to consider the long-term effects of chronic pain for older people’s health and well-being.
Pain is consistently associated with elevated depressive symptoms in older adults [25,26]. Although several studies indicate a reciprocal relationship between pain and depression in this population [14,58], pain has been found to predict increases in depressive symptoms over time as well as the onset of major depression [38,40]. Depression in later life is linked to a host of detrimental health effects including greater functional impairment [52,82] and a heightened risk of mortality [10,64]. Strikingly, the co-occurrence of chronic pain and depressive symptoms leads to a worse prognosis than either problem alone [16], resulting in more intense pain [5], higher health care utilization [18,78], and increased physical disability [41].
Beyond the individual-level links between pain intensity and depressive symptoms, there may be spousal associations in later life (i.e., partners’ pain may increase individuals’ depressive symptoms). Interdependence theory proposes that marital partners affect one another’s thoughts, feelings, and behaviors [62]. Spouses in turn shape both their own and their partner’s health trajectories, and these influences may become even stronger as couples age [24,43]. Supporting these perspectives, prior work demonstrates within-couple interrelations in depressed mood along with a range of other health indicators including physical activity, functional limitations, and sleep duration [3,11,24,47,54,59,67]. Likewise, spouses’ greater pain intensity has been linked to their partner’s poorer psychological well-being in cross-sectional [15,36,63,66] and longitudinal [4,56,71] research. Yet existing studies on the links between spousal pain and depressive symptoms largely focus on specific illness populations (e.g., cancer patients), examine individuals rather than marital dyads as the unit of analysis, and do not consider gender differences. Moreover, previous longitudinal studies are limited to a relatively short time frame (e.g., 6 months). Hence, little is known about the long-term mutual influences between pain and depressive symptoms that may occur within older couples in the general population.
Drawing from a nationally representative US sample of heterosexual married couples aged 50 and older, we evaluated how own and partner pain intensity are linked to depressive symptoms across an 8-year period. For wives and husbands, we predicted that greater own and partner reports of pain intensity at baseline would be associated with higher levels of depressive symptoms as well as increases in depressive symptoms over time. In line with research suggesting that women engage more often in pain catastrophizing (i.e., ruminating about or magnifying pain-related experiences) [6] and may have greater awareness and empathy for their partner’s pain than men [8,12,19,49], we predicted that these associations would be significantly stronger for wives than for husbands.
Methods
Participants and Sample
The US sample included 963 heterosexual married couples drawn from the nationally representative Health and Retirement Study (HRS), one of the largest studies of people aged 50 and older that includes data from both members of the spousal dyad. The HRS has collected data biennially since 1992 with a response rate of over 80% at each wave. In accordance with ongoing HRS procedures, all participants are read a confidentiality statement when first contacted, and give oral or implied consent by agreeing to be interviewed. Participants are also given a written informed consent document for each interview. Consistent with the University of Michigan’s policies, ethical approval for the current study was not required because publicly available secondary data with no individual identifiers were utilized.
Since 2006, data have been collected concerning social relationships, life circumstances, well-being, and biological measures. This portion of the HRS interview is referred to as the enhanced face-to-face interview, which is conducted biennially from 50% of the panel participants. The enhanced face-to-face interview includes a self-administered psychosocial questionnaire (SAQ) with questions about the marital relationship [69]. Participants were asked to complete and mail the SAQ back to the main field office at the University of Michigan.
In the present study, we used data from five waves of the HRS between 2006 and 2014. In 2006, HRS participants were contacted by telephone and asked to complete an interview. After gaining consent, telephone interviews were conducted with 18,469 participants, of whom 11,273 (61%) were married. Of the 11,273 married participants in 2006, 11,027 (98%) had spouses who also completed an interview. In total, 5,686 individual respondents (2,843 heterosexual couples) from unique households were consistently married to the same spouse from 2006 to 2014 and participated in each of the five waves. We were interested in examining the effects of own and partner pain intensity on depressive symptoms in later life, and so we selected 2,610 couples in which both spouses were aged 50 or older at baseline (2006).
Of the 2,610 couples who were aged 50 or older in 2006, we removed 1,495 couples in which one or both spouses did not complete the self-administered psychosocial questionnaire in 2006. Of the remaining 1,115 couples, we removed 152 who had missing data on one or more study variables. Hence, our analytic sample included a total of 963 wives (mean = 63.04 years, SD = 7.67, range = 50–85) and their husbands (mean = 66.02 years, SD = 57.78, range = 50–89) who were consistently married to one another and had complete data across the five waves. Compared with the 152 couples who were removed, the 963 couples in this study were younger (t(2228) = −3.62, p < .001), had more years of education (t(2225) = 7.08, p < .001), reported better self-rated health (t(2227) = 4.16, p < .001), and were less likely to be racial or ethnic minorities (χ2(1, N = 2230) = 12.14, p < .001). There were no significant differences in their baseline pain intensity or depressive symptoms. On average, couples had been married for 36.42 years (SD = 13.45, range = 0.50–65.20) at baseline. The majority of wives (73.3%) and husbands (71.9%) were in their first marriage. Table 1 shows background characteristics for the 963 couples, along with baseline scores for key variables.
Table 1.
Baseline Characteristics and Key Variables for Wives and Husbands
| Characteristic | Wives
|
Husbands
|
||
|---|---|---|---|---|
| M | SD | M | SD | |
| Age | 63.04 | 7.67 | 66.02 | 7.78 |
| Education in years | 13.30 | 2.53 | 13.48 | 2.87 |
| Pain intensity | 0.61 | 0.92 | 0.48 | 0.83 |
| Self-rated health | 3.57 | 0.96 | 3.51 | 0.97 |
| Total health conditions | 1.62 | 1.15 | 1.70 | 1.23 |
| Depressive symptoms | 1.02 | 1.63 | 0.78 | 1.36 |
| Negative marital quality | 1.96 | 0.63 | 1.88 | 0.59 |
| Number of living children | 3.16 | 1.90 | 3.16 | 1.90 |
| Proportions | ||||
|
|
||||
| Minority statusa | .09 | .09 | ||
| Works for pay | .45 | .50 | ||
| Disability statusb | .07 | .07 | ||
| Pain-related activity interferencec | .19 | .14 | ||
| Clinically significant paind | .23 | .17 | ||
| Clinically significant depressive symptomse | .09 | .05 | ||
Note.
1 = racial/ethnic minority, −1 = non-Hispanic White.
1 = has difficulty with one or more activities of daily living (ADLs), −1 = does not have difficulty with ADLs.
1 = has pain-related activity interference, −1 = does not have pain-related activity interference.
1 = moderate or severe pain, −1 = no or mild pain.
1 = reported clinically significant depressive symptoms, −1 = did not report clinically significant depressive symptoms.
N = 963 married couples.
Measures
Depressive symptoms
Depressive symptoms were measured at each wave with the 8-item version of the Center for Epidemiologic Studies Depression Scale (CES-D) [57], which has demonstrated high reliability and validity in older adult populations [29]. Participants reported whether they experienced the following symptoms much of the time over the past week (1 = yes, 0 = no): felt depressed, felt lonely, felt sad, felt everything was an effort, had restless sleep, could not get going, was happy, and enjoyed life. Ratings for the two positive mood items were reverse coded. Items were summed to create a total score, with higher scores indicating greater symptoms (wives: mean α = 0.77, husbands: mean α = 0.73). We also considered the presence of clinically significant depressive symptoms, which were indicated by total scores of 4 or higher [70].
Pain intensity
Pain intensity was assessed from two items. Participants were first asked whether they were often troubled with pain (yes or no). Participants who reported having trouble with pain were then asked to rate how bad their pain was most of the time: mild, moderate, or severe. We combined these items such that participants who were not troubled with pain received a score of 0 (little or no pain) and those who were troubled with pain received a score reflecting their pain intensity (1 = mild pain, 2 = moderate pain, 3 = severe pain). On the basis of research showing that moderate to higher levels of pain intensity are linked to functional impairment or pain-related activity interference [81], we also considered the presence of clinically significant pain (1 = moderate or severe pain, −1 = no or mild pain) at baseline. To evaluate whether pain was an ongoing problem, we examined whether participants had trouble with pain across the five study waves (1 = reported pain at all five waves, −1 = did not report pain at all five waves).
Covariates
We controlled for baseline sociodemographic characteristics: age, education in years, and minority status (1 = racial/ethnic minority, −1 = non-Hispanic White). We also controlled for two marital characteristics related to health: marital duration in years and negative marital quality [32,76]. Four brief but commonly used and validated items were used to assess negative marital quality [65,80]. Participants reported how often their spouse (a) makes too many demands on them; (b) criticizes them; (c) lets them down when counted upon; and (d) gets on their nerves. Responses ranged from 1 (a lot) to 4 (not at all). Items were reverse coded and averaged so that higher scores represented higher negative marital quality (wives: α = .78, husbands: α = .76).
To account for other physical health indicators, we controlled for self-rated health, total number of chronic health conditions, and disability status. Self-rated health was measured with a single item rating perceptions of overall physical health from 1 (excellent) to 5 (poor). Scores were reverse coded such that higher scores reflected better health. This measure is often used in survey research and is strongly associated with objective physical health status [28]. Participants reported whether they had been diagnosed with seven chronic health conditions (arthritis, cancer, diabetes, heart disease, hypertension, lung disease, and stroke; 1 = has condition, 0 = does not have condition). Total summed scores were created, with higher scores indicating a greater number of health conditions. We measured disability status from self-reported difficulty with one or more activities of daily living (ADLs): bathing, dressing, eating, getting in/out of bed, using the toilet, and walking (1 = has difficulty with one or more ADLs, −1 = does not have difficulty with ADLs). Finally, we considered own and partner pain-related activity interference. Wives and husbands who reported pain at baseline were asked whether their pain makes it difficult for them to do their usual activities including household chores or work (1 = yes, 0 = no). Participants in the current analysis who did not report baseline pain received a score of 0. We then created a dichotomous variable from this item (1 = has pain-related activity interference, −1 = does not have pain-related activity interference).
Statistical Analysis
We estimated dyadic growth curve models using the MIXED procedure in SPSS Version 22. This dyadic multilevel approach is a version of the actor-partner interdependence model (APIM) that enables the simultaneous modeling of own and partner influence within couples over time [31]. Models included the recommended two levels for longitudinal dyadic data, in which the lower level represents variability due to within person repeated measures for wives and husbands and the upper level represents between couple variability across wives and husbands [31]. The intercept and slope of time were permitted to vary between and within couples. The model also allowed for correlated errors between wives and husbands within a given wave using a heterogeneous compound symmetry error structure (CSH). In this study, actor effects represent the influence of wives’ and husbands’ own pain intensity on their own depressive symptoms (e.g., wives’ pain intensity predicting their own depressive symptoms). Partner effects represent the influence of each spouse’s pain intensity on his or her partner’s depressive symptoms (e.g., wives’ pain intensity predicting husbands’ depressive symptoms). We determined the links between baseline pain intensity and levels of depressive symptoms, as well as the effects of baseline pain intensity on change in depressive symptoms across time. Waves represented time, which was centered at baseline. There were two years in between each wave. Predictors included pain intensity (of the actor and partner), time, and two interaction terms (Actor Pain Intensity X Time; Partner Intensity X Time) which were included to test whether own and partner baseline pain intensity were linked to increases in depressive symptoms across waves. Covariates included age, education, minority status, marital duration, negative marital quality, self-rated health, total number of chronic health conditions, and disability status.
To evaluate actor and partner effects for each spouse in the couple, we estimated separate intercepts and slopes for wives and husbands using spouse gender (1 = wife, −1 = husband) as a distinguishing variable [31]. Continuous predictors and covariates were grand mean centered and binary variables were effect coded (i.e., 1, −1) so that parameter estimates represent the deviation of each level of the variable from the grand mean of depressive symptom scores [31]. We assessed whether there was a significant difference between the fit of the full model (with predictors and covariates) relative to a covariate-only model by subtracting the −2 log likelihood estimations of these models and examining differences on a chi-square distribution with degrees of freedom equaling the change in number of model parameters [68].
Results
We performed paired t tests in preliminary analyses to examine differences between wives and husbands in major variables at baseline. Wives reported higher pain intensity (t(962) = 3.42, p < .001) and greater depressive symptoms (t(962) = 3.78, p < .001) relative to their husbands. Spouses’ reports were positively correlated for pain intensity (r = .11, p = .001) and depressive symptoms (r = .13, p < .001). A total of 132 wives (13.7%) and 112 husbands (11.6%) reported being bothered by pain at all five waves.
Clinically significant pain was common in the sample. A total of 218 wives (22.6%) and 166 (17.2%) husbands reported clinically significant pain at baseline, and a total of 486 wives (50.5%) and 390 husbands (40.5%) reported clinically significant pain at least once across the waves. Clinically significant depressive symptoms were also relatively prevalent, with such symptoms reported by 83 wives (8.6%) and 52 husbands (5.4%) at baseline and by 218 wives (22.6%) and 149 husbands (15.5%) in at least one study wave.
Effects of Own and Partner Pain Intensity on Wives’ and Husbands’ Depressive Symptoms
Table 2 shows that the fit of the full model was significantly better than the covariate-only model (χ2 (4) = 62.47, p < .001), demonstrating that own and partner reports of pain intensity accounted for a significantly greater amount of variance in depressive symptoms relative to the covariates. Unstandardized coefficients and standardized betas are presented from the full model.
Table 2.
Dyadic Growth Curve Models Estimating the Effects of Pain Intensity on Depressive Symptoms for Wives and Husbands
| Parameter | Wives’ Depressive Symptoms |
Husbands’ Depressive Symptoms |
||||
|---|---|---|---|---|---|---|
| B | SE | β | B | SE | β | |
| Intercept | 1.18*** | .10 | 1.10*** | .07 | ||
| Time | .01 | .01 | .01 | .01 | .01 | .01 |
| Actor Pain intensity | .26*** | .05 | .19 | .23*** | .05 | .17 |
| Partner Pain intensity | −.05 | .05 | −.04 | .07 | .04 | .05 |
| Actor Pain intensity X Time | −.02* | .01 | −.01 | −.01 | .01 | −.01 |
| Partner Pain intensity X Time | .02** | .01 | .01 | −.001 | .01 | −.001 |
| Δ −2 Log Likelihood | 62.47*** | |||||
| Covariates | ||||||
| Age | −.01* | .01 | −.01 | −.01 | .01 | −.01 |
| Minority status | −.03 | .06 | −.02 | .01 | .05 | .01 |
| Education in years | −.06*** | .02 | −.04 | −.05*** | .01 | −.04 |
| Self-rated health | −.38*** | .05 | −.27 | −.24*** | .04 | −.17 |
| Total health conditions | −.003 | .04 | −.002 | .09** | .03 | .07 |
| Disability status | .30*** | .08 | .22 | .34*** | .06 | .25 |
| Marital duration in years | −.01 | .003 | −.01 | −.01* | .003 | −.01 |
| Negative marital quality | .38*** | .06 | .27 | .31*** | .05 | .22 |
Note. Change in −2 log likelihood for the full model (31,106.83) is based on comparison with a covariate-only model (31,169.30). Estimates are presented from the full model.
N = 963 married couples.
p ≤ .05.
p ≤ .01.
p ≤ .001.
Wives’ depressive symptoms
As shown in Table 2, wives’ greater baseline pain intensity was significantly associated with their own higher levels of depressive symptoms (B = .26, β = .19, p < .001). Husbands’ pain intensity at baseline, however, was unrelated to the level of wives’ depressive symptoms.
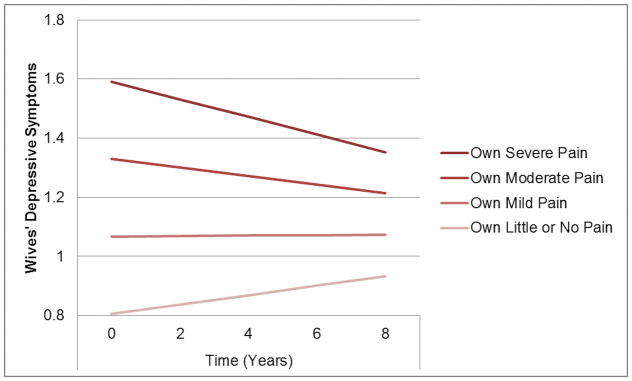
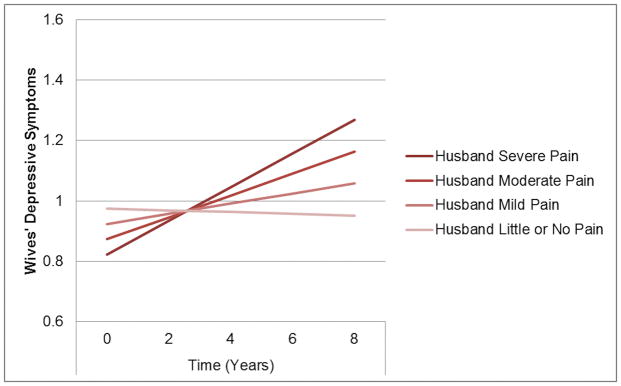
As presented in Figure 1, wives with greater baseline pain intensity showed decreases in depressive symptoms over time (B = −.02, β = −.01, p = .03). By contrast, Figure 2 shows that when husbands reported greater pain intensity at baseline, wives demonstrated increased depressive symptoms across waves (B = .02, β = .01, p = .01).
Fig. 1.
The significant effect of wives’ own pain intensity on their own depressive symptoms over time. Growth trajectories of depressive symptoms (possible range = 0 – 8) were plotted using estimated marginal means for wives with little or no pain, mild pain, moderate pain, and severe pain at baseline (controlling for partner pain intensity and all covariates).
Fig. 2.
The significant effect of husbands’ pain intensity on wives’ depressive symptoms over time. Growth trajectories of depressive symptoms (possible range = 0 – 8) were plotted using estimated marginal means for wives of husbands with little or no pain, mild pain, moderate pain, and severe pain at baseline (controlling for own pain intensity and all covariates).
Husbands’ depressive symptoms
Table 2 shows that husbands’ greater pain intensity at baseline was significantly linked to their own higher levels of depressive symptoms (B = .23, β = .17, p < .001). Wives’ greater baseline pain intensity, however, was not linked to husbands’ level of depressive symptoms. Likewise, neither wives’ nor husbands’ reports of greater baseline pain intensity were linked to husbands’ changes in depressive symptoms over time.
Post Hoc Tests
To further test the distinct effects of baseline pain intensity on depressive symptoms across waves, we estimated a separate model controlling for own and partner pain-related activity interference at baseline and whether or not each spouse consistently reported pain at each wave. The pattern of findings from the main analysis did not change, confirming their stability.
We then tested whether the associations between wives’ and husbands’ own pain intensity at baseline and depressive symptoms varied by their partner’s pain intensity at baseline. We estimated a model that included two actor-partner interaction terms (Actor Pain Intensity X Partner Pain Intensity; Actor Pain Intensity X Partner Pain Intensity X Time). Neither of these interaction effects was significant for wives or husbands, suggesting that individual associations between pain intensity and depressive symptoms did not vary by partner reports of pain intensity.
To consider bidirectional associations between pain intensity and depressive symptoms within couples, we estimated models with own and partner baseline depressive symptoms predicting pain intensity across waves. For wives and husbands, their own greater depressive symptoms (B = .10, β = .21, p < .001 and B = .06, β = .17, p < .001, respectively) at baseline were significantly associated with their own higher levels of pain intensity. Partners’ baseline depressive symptoms were not associated with levels of pain intensity for wives or husbands. Similarly, among wives and husbands, neither own nor partner reports of depressive symptoms at baseline were associated with changes in pain intensity over time.
Discussion
This study provides evidence that bothersome pain has significant implications for the psychological well-being of older married couples. We build upon prior research by examining dyadic associations between pain intensity and depressive symptoms over an 8-year period in a population-based sample of wives and husbands aged 50 and older. The present findings demonstrate that pain intensity has robust associations with depressive symptoms in aging couples, independent of the variance explained by marital quality and multiple health indictors. Remarkably, these links remained even after controlling for own and partner reports of pain-related activity interference and whether bothersome pain occurred across all five waves, suggesting that pain intensity has a unique and enduring impact on symptoms of depression in older couples. Moreover, whereas own and partner reports of pain intensity were linked to changes in wives’ depressive symptoms, depressive symptoms within the couple did not predict changes in pain intensity. This implies that pain intensity may have greater effects on depressive symptoms than vice versa. As a whole, the findings are in line with interdependence theory [62] and prior studies highlighting strong mutual health-related influences in later life marriages [3,11,24,47,54,59,67].
For both wives and husbands, their own greater baseline pain intensity was significantly associated with their own higher levels of depressive symptoms. These findings are consistent with research showing that pain and depression frequently co-occur in later life [25,26]. Post hoc tests revealed that these associations did not vary by partner reports of pain intensity. Thus, contrary to prior work suggesting that partners’ shared experience of pain may mitigate the negative impact of pain intensity on their psychological well-being [17,27], the current findings indicate that associations between one’s own greater pain intensity and elevated depressive symptoms persists despite the level of pain experienced by one’s partner.
Counter to previous research [4,61], wives and husbands with higher baseline pain intensity did not show increased depressive symptoms over time. Most work, however, has focused on specific illness populations or patients with severe chronic pain [61]. Furthermore, prior longitudinal studies have examined the links between pain intensity and depressive symptoms across a relatively short period (e.g., 3 or 6 months) [4]. One’s own greater pain intensity, therefore, may only be linked to increasing depressive symptoms in clinical samples and over a shorter time frame.
Unexpectedly, wives reporting higher pain intensity at baseline showed decreases in depressive symptoms across waves. One possible explanation is that more intense pain may predispose the development of greater resilience among older married women that restores their mental health over time [72]. Prior work has found that women are generally more resilient than men in later life [20,50], which may be partly attributed to their stronger ability to maintain social connections and community involvement [33,35]. This pattern of findings was not observed for husbands, raising the possibility that married men who report high pain intensity in later life may tend to experience sustained levels of elevated depressive symptoms as they age.
Over and above the effects of their own pain intensity, wives reported increases in depressive symptoms when their husband had more intense pain at baseline. By contrast, this cross-partner effect was not observed for husbands. There are at least three plausible reasons for these findings. First, partners’ pain may elicit greater psychological distress for wives than for husbands because wives express higher levels of empathy and emotional contagion in response to their partner’s suffering [19,49]. Second, compared with husbands, wives may be more aware of their spouse’s pain and related functional impairment. Supporting this possibility, research suggests that women may be more accurate than men regarding perceptions of their partner’s pain and physical disability [8,12]. Third, wives tend to be more involved with providing caregiving support to their ill or disabled partners [48,74]. Husbands who have greater pain intensity are likely to show worsening health over time. This may coincide with wives’ increased caregiving, which can ultimately erode their well-being. Indeed, relative to caregiving husbands, caregiving wives typically provide more hours of spousal care, engage in a greater number of direct care tasks (e.g., bathing, dressing), receive less care-related support from family members, and report higher levels of depressive symptoms [55]. Taken together, this study indicates that partners’ pain may have harmful consequences for wives’ long-term mental health.
It is important to acknowledge several limitations of this work as well as key directions for subsequent research. First, in line with other population-based studies [79], wives and husbands reported low levels of pain intensity on average. This limits generalizability to couples in which one or both partners has severe chronic pain or a specific pain condition (e.g., knee osteoarthritis). Second, although our available measure of pain intensity is commonly used in survey research [21,22], it is a single item scale with a limited response range. Third, we focused on a sample of consistently married heterosexual couples. Consequently, the findings may not generalize to other types of couples, such as same-sex spouses, cohabiting partners, or those who eventually divorce. Finally, most couples in this study were non-Hispanic White and middle class. Future studies should attempt to replicate and extend the present findings in samples of more sociodemographically diverse couples, which would further elucidate understanding of the long-term associations between pain intensity and depressive symptoms in the broader population.
Future work should also investigate more proximal mechanisms that may partly explain the present findings. Husbands’ deteriorating health and functioning due to severe pain, for example, may restrict the couple’s shared engagement in valued social events, physical activity and exercise, and other leisure activities [9]. This change in marital routines may reduce sources of positive reinforcement for wives and increase caregiver burden, thereby contributing to greater depressive symptoms [47,51]. Additionally, husbands’ pain could lead to marital problems that heighten wives’ psychological distress. Pain behaviors are reciprocally related to aversive spousal interactions, which can result in marital conflict, diminished emotional closeness and intimacy, and the eventual erosion of partner support [37,60]. People with severe pain also commonly withdraw from their marriage and other important social ties in ways that may strain these relationships and amplify the emotional consequences of pain [73]. This may be especially likely for older married men with chronic pain because husbands tend to engage in withdrawal behaviors (e.g., disengaging from discussions with one’s spouse) more often than their wives into the later years of marriage [23]. The consideration of such short-term marital processes would be valuable in the development of targeted interventions for older individuals and couples managing chronic pain.
Given that most older adults in the US are married and living with their spouses [77], this study has critical implications for policymakers and clinicians working with people who may vulnerable to poor mental health linked to their own or their partner’s pain. Primary care patients with comorbid pain and depression frequently report only somatic complaints [2]. As a consequence, depression may be underdiagnosed with the presence of pain in routine practice [42]. The current study indicates that regular screenings for depressive symptoms in the long-term care of older chronic pain patients may be warranted, with the awareness that pain is often more strongly linked to somatic symptoms than cognitive symptoms of depression [34,75]. Nearly one-quarter of wives reported clinically significant depressive symptoms at one or more waves, and so providing regular depression screenings to wives of aging men with chronic pain may be particularly beneficial. Along with preserving their own well-being, proactive attention to maintaining the mental health of these wives may support their ability to provide quality caregiving as their partner’s functioning declines.
Lastly, the present findings underscore the importance of spousal involvement in the ongoing treatment and management of chronic pain, which may benefit patients and their partners. Recent work suggests that brief motivational therapeutic assessment and tailored feedback of the couple’s relationship and coping may lower patients’ pain intensity and improve their own and their spouse’s mood and perceptions of marital quality [44,45]. Likewise, couple-based interventions have shown considerable promise in improving patients’ pain along with the psychological well-being and marital satisfaction of patients and spouses [7,13,39]. Spouse-assisted training in pain coping skills, for example, may reduce patients’ fear of movement and rumination about pain [1] as well as improve their physical fitness and strength [30]. Spouses report elevated depressive symptoms when patients are physically inactive because of pain or related symptoms [47], and so such improvements could contribute to lasting benefits for the couple. In addition to these advantages, including spouses in the treatment of chronic pain in later life could help in sustaining independence and quality of life for both older adults.
To summarize, this study demonstrates that higher pain intensity may place aging adults and their partners at risk of elevated depressive symptoms. The findings suggest that older women may be highly susceptible to the negative mental health consequences of their spouse’s chronic pain. Additional work is needed to determine comprehensive healthcare policies and treatment strategies that more fully address the complex long-term needs of couples coping with pain in middle and later life.
Acknowledgments
This work was supported by training grant T32 MH073553-11 from the National Institute of Mental Health (Stephen J. Bartels, Principal Investigator). The Health and Retirement Study is sponsored by the National Institute on Aging (U01AG009740) and is conducted by the University of Michigan. The authors have no conflicts of interest to report.
References
- 1.Abbasi M, Dehghani M, Keefe FJ, Jafari H, Behtash H, Shams J. Spouse-assisted training in pain coping skills and the outcome of multidisciplinary pain management for chronic low back pain treatment: A 1-year randomized controlled trial. Eur J Pain. 2012;16:1033–1043. doi: 10.1002/j.1532-2149.2011.00097.x. [DOI] [PubMed] [Google Scholar]
- 2.Agüera L, Failde I, Cervilla JA, Díaz-Fernández P, Mico JA. Medically unexplained pain complaints are associated with underlying unrecognized mood disorders in primary care. BMC Fam Pract. 2010;11:11–17. doi: 10.1186/1471-2296-11-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ayotte B, Yang FM, Jones RN. Physical health and depression: A dyadic study of chronic health conditions and depressive symptomatology in older adult couples. J Gerontol B Psychol Sci Soc Sci. 2010;65:438–448. doi: 10.1093/geronb/gbq033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Badr H, Sten MJ. Pain catastrophizing, pain intensity, and dyadic adjustment influence patient and partner depression in metastatic breast cancer. Clin J Pain. 2014;30:923–933. doi: 10.1097/AJP.0000000000000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: A literature review. Arch Intern Med. 2003;163:2433–2445. doi: 10.1001/archinte.163.20.2433. [DOI] [PubMed] [Google Scholar]
- 6.Bartley EJ, Fillingim RB. Sex differences in pain: A brief review of clinical and experimental findings. Br J Anaesth. 2013;111(1):52–58. doi: 10.1093/bja/aet127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baucom DH, Porter LS, Kirby JS, Hudepohl J. Couple-based interventions for medical problems. Behav Ther. 2012;43:61–76. doi: 10.1016/j.beth.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 8.Beaupre P, Keefe FJ, Lester N, Affleck G, Fredrickson B, Caldwell S. A computer-assisted observational method for assessing spouses’ ratings of osteoarthritis patients’ pain. Psychol Health Med. 1997;2:99–108. [Google Scholar]
- 9.Benyamini Y, Lomranz J. The relationship of activity restriction and replacement with depressive symptoms among older adults. Psychol Aging. 2004;19:362–366. doi: 10.1037/0882-7974.19.2.362. [DOI] [PubMed] [Google Scholar]
- 10.Bogner HR, Morales KH, Reynolds CF, Cary MS, Bruce ML. Course of depression and mortality among older primary care patients. Am J Geriatr Psychiatry. 2012;20:895–903. doi: 10.1097/JGP.0b013e3182331104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bookwala J, Schulz R. Spousal similarity in subjective well-being: The Cardiovascular Health Study. Psychol Aging. 1996;11:582–590. doi: 10.1037//0882-7974.11.4.582. [DOI] [PubMed] [Google Scholar]
- 12.Cano A, Johansen AB, Geisser M. Spousal congruence on disability, pain, and spouse responses to pain. Pain. 2004;109:258–65. doi: 10.1016/j.pain.2004.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cano A, Leonard M. Integrative behavioral couple therapy for chronic pain: Promoting behavior change and emotional acceptance. J Clin Psychol. 2006;62:1409–1418. doi: 10.1002/jclp.20320. [DOI] [PubMed] [Google Scholar]
- 14.Chou KL. Reciprocal relationship between pain and depression in older adults: Evidence from the English Longitudinal Study of Ageing. J Affect Disord. 2007;102:115–123. doi: 10.1016/j.jad.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 15.Flor H, Turk DC, Scholz OB. Impact of chronic pain on the spouse: Marital, emotional and physical consequences. J Psychosom Res. 1987;31:63–71. doi: 10.1016/0022-3999(87)90099-7. [DOI] [PubMed] [Google Scholar]
- 16.Geerlings SW, Twisk JW, Beekman AT, Deeg DJ, van Tilburg W. Longitudinal relationship between pain and depression in older adults: Sex, age and physical disability. Soc Psychiatry Psychiatr Epidemiol. 2002;37:23–30. doi: 10.1007/s127-002-8210-2. [DOI] [PubMed] [Google Scholar]
- 17.Goubert L, Craig K, Vervoort T, Morley S, Sullivan M, Williams A, Cano A, Crombez G. Facing others in pain: The effects of empathy. Pain. 2005;118:285–288. doi: 10.1016/j.pain.2005.10.025. [DOI] [PubMed] [Google Scholar]
- 18.Greenberg PE, Leong SA, Birnbaum HG, Robinson RL. The economic burden of depression with painful symptoms. J Clin Psychiatry. 2003;64:17–23. [PubMed] [Google Scholar]
- 19.Hagedoorn M, Sanderman R, Bolks HN, Tuinstra J, Coyne JC. Distress in couples coping with cancer: A meta-analysis and critical review of role and gender effects. Psychol Bull. 2008;134:1–30. doi: 10.1037/0033-2909.134.1.1. [DOI] [PubMed] [Google Scholar]
- 20.Hahn EA, Cichy KE, Almeida DM, Haley WE. Time use and well-being in older widows: Adaptation and resilience. J Women Aging. 2011;23:149–159. doi: 10.1080/08952841.2011.561139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Herr KA, Garand L. Assessment and measurement of pain in older adults. Clin Geriatr Med. 2001;17:457–476. doi: 10.1016/s0749-0690(05)70080-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Herr K, Mobily P. Comparison of selected pain assessment tools for use with the elderly. Appl Nurs Res. 1993;6:39–46. doi: 10.1016/s0897-1897(05)80041-2. [DOI] [PubMed] [Google Scholar]
- 23.Holley SR, Haase CM, Levenson RW. Age-related changes in demand–withdraw communication behaviors. J Marriage Fam. 2013;75:822–836. doi: 10.1111/jomf.12051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoppmann C, Gerstorf D, Hibbert A. Spousal associations between functional limitations and depressive symptom trajectories: Longitudinal findings from the Study of Asset and Health Dynamics among the Oldest Old (AHEAD) Health Psychol. 2011;30:153–162. doi: 10.1037/a0022094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Iliffe S, Kharicha K, Carmaciu C, Harari D, Swift C, Gillman G, Stuck AE. The relationship between pain intensity and severity and depression in older people: Exploratory study. BMC Fam Pract. 2009;10:1–7. doi: 10.1186/1471-2296-10-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jakobsson U, Klevsgard R, Westergren A, Hallberg IR. Old people in pain: A comparative study. J Pain Symptom Manage. 2003;26:625–636. doi: 10.1016/s0885-3924(03)00145-3. [DOI] [PubMed] [Google Scholar]
- 27.Johansen AB, Cano A. A preliminary investigation of affective interaction in chronic pain couples. Pain. 2007;132:86–95. doi: 10.1016/j.pain.2007.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jylha M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med. 2009;69:307–316. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 29.Karim J, Weisz R, Bibi Z, Rehman S. Validation of the eight-item Center for Epidemiologic Studies Depression Scale (CES-D) among older adults. Curr Psychol. 2015;34:681–692. [Google Scholar]
- 30.Keefe FJ, Blumenthal J, Baucom D, Affleck G, Waugh R, Caldwell SD, Beaupre P, Kashikar-Zuck S, Wright K, Egert J, Lefebvre J. Effects of spouse-assisted coping skills training and exercise training in patients with osteoarthritic knee pain: A randomized controlled trial. Pain. 2004;110:539–549. doi: 10.1016/j.pain.2004.03.022. [DOI] [PubMed] [Google Scholar]
- 31.Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. New York, NY: The Guilford Press; 2006. [Google Scholar]
- 32.Kiecolt-Glaser JK, Newton TL. Marriage and health: His and hers. Psychol Bull. 2001;127:472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- 33.Kinsel B. Resilience and adaptation in older women. J Women Aging. 2005;17:23–39. doi: 10.1300/J074v17n03_03. [DOI] [PubMed] [Google Scholar]
- 34.Korff MV, Simon G. The relationship between pain and depression. Brit J Psychiat. 1996;168:101–108. [PubMed] [Google Scholar]
- 35.Lamond AJ, Depp CA, Allison M, Langer R, Reichstadt J, Moore DJ, Golshan S, Ganiats TG, Jeste DV. Measurement and predictors of resilience among community-dwelling older women. J Psychiatr Res. 2008;43:148–154. doi: 10.1016/j.jpsychires.2008.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Leonard MT, Cano A. Pain affects spouses too: Personal experience with pain and catastrophizing as correlates of spouse distress. Pain. 2006;126:139–146. doi: 10.1016/j.pain.2006.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Leonard MT, Cano A, Johansen AB. Chronic pain in a couples context: A review and integration of theoretical models and empirical evidence. J Pain. 2006;7:377–390. doi: 10.1016/j.jpain.2006.01.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mäntyselkä P, Lupsakko T, Kautiainen H, Vanhala M. Neck–shoulder pain and depressive symptoms: A cohort study with a 7-year follow-up. Eur J Pain. 2010;14:189–193. doi: 10.1016/j.ejpain.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 39.Martire LM, Schulz R, Helgeson VS, Small BJ, Saghafi EM. Review and meta-analysis of couple-oriented interventions for chronic illness. Ann Beh Med. 2010;40(3):325–342. doi: 10.1007/s12160-010-9216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mavandadi S, Sorkin DH, Rook KS, Newsom JT. Pain, positive and negative social exchanges, and depressive symptomatology in later life. J Aging Health. 2007;62:361–370. doi: 10.1177/0898264307305179. [DOI] [PubMed] [Google Scholar]
- 41.Melzer D, Gardener E, Guralnik JM. Mobility disability in the middle-aged: Cross-sectional associations in the English Longitudinal Study of Ageing. Age Ageing. 2005;34:594–602. doi: 10.1093/ageing/afi188. [DOI] [PubMed] [Google Scholar]
- 42.Menchetti M, Murri MB, Bertakis K, Bortolotti B, Berardi D. Recognition and treatment of depression in primary care: Effect of patients’ presentation and frequency of consultation. J Psychosom Res. 2009;66:335–341. doi: 10.1016/j.jpsychores.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 43.Meyler D, Stimpson JP, Peek MK. Health concordance within couples: A systematic review. Soc Sci Med. 2007;64:2297–2310. doi: 10.1016/j.socscimed.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 44.Miller-Matero LR, Cano A. Encouraging couples to change: A motivational assessment to promote well-being in people with chronic pain and their partners. Pain Med. 2015;16:348–355. doi: 10.1111/pme.12600. [DOI] [PubMed] [Google Scholar]
- 45.Miller LR, Cano A, Wurm LH. A motivational therapeutic assessment improves pain, mood, and relationship satisfaction in couples with chronic pain. J Pain. 2013;14:525–537. doi: 10.1016/j.jpain.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 46.Molton IR, Terrill AL. Overview of persistent pain in older adults. Am Psychol. 2014;69(2):197–207. doi: 10.1037/a0035794. [DOI] [PubMed] [Google Scholar]
- 47.Monin JK, Chen B, Stahl ST. Dyadic associations between physical activity and depressive symptoms in older adults with musculoskeletal conditions and their spouses. Stress Health. 2016;32:244–252. doi: 10.1002/smi.2603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Monin JK, Clark MS. Why do men benefit more from marriage than do women? Thinking more broadly about interpersonal processes that occur within and outside of marriage. Sex Roles. 2011;65:320–326. [Google Scholar]
- 49.Monin JK, Levy BR, Kane HS. To love is to suffer: Older adults’ daily emotional contagion to perceived spousal suffering. J Gerontol B Psychol Sci Soc Sci. 2015 Sep 29; doi: 10.1093/geronb/gbv070. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Netuveli G, Wiggins RD, Montgomery SM, Hildon Z, Blane D. Mental health and resilience at older ages: Bouncing back after adversity in the British Household Panel Survey. J Epidemiol Community Health. 2008;62:987–991. doi: 10.1136/jech.2007.069138. [DOI] [PubMed] [Google Scholar]
- 51.Nieboer AP, Schulz R, Matthews KA, Scheier MF, Ormel J, Lindberg SM. Spousal caregivers’ activity restriction and depression: A model for changes over time. Soc Sci Med. 1998;47:1361–1371. doi: 10.1016/s0277-9536(98)00214-7. [DOI] [PubMed] [Google Scholar]
- 52.Nyunt MS, Lim ML, Yap KB, Ng TP. Changes in depressive symptoms and functional disability among community-dwelling depressive older adults. Int Psychogeriatr. 2012;24:1633–1641. doi: 10.1017/S1041610212000890. [DOI] [PubMed] [Google Scholar]
- 53.Patel KV, Guralnik JM, Dansie EJ, Turk DC. Prevalence and impact of pain among older adults in the United States: Findings from the 2011 National Health and Aging Trends Study. Pain. 2013;154:2649–2657. doi: 10.1016/j.pain.2013.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Peek KM, Markides KS. Blood pressure concordance in older married Mexican-American couples. J Am Geriatr Soc. 2003;51:1655–1659. doi: 10.1046/j.1532-5415.2003.51520.x. [DOI] [PubMed] [Google Scholar]
- 55.Pinquart M, Sörenson S. Gender differences in caregiver stressors, social resources, and health: An updated meta analysis. J Gerontol B Psychol Sci Soc Sci. 2006;61:33–45. doi: 10.1093/geronb/61.1.p33. [DOI] [PubMed] [Google Scholar]
- 56.Polenick CA, Martire LM, Hemphill RC, Stephens MAP. Effects of change in arthritis severity on spouse well-being: The moderating role of relationship closeness. J Fam Psychol. 2015;29:331–338. doi: 10.1037/fam0000093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psych Meas. 1977;3:385–401. [Google Scholar]
- 58.Reid MC, Williams CS, Concato J, Tinetti ME, Gill TM. Depressive symptoms as a risk factor for disabling back pain in community-dwelling older persons. J Am Geriatr Soc. 2003;51:1710–1717. doi: 10.1046/j.1532-5415.2003.51554.x. [DOI] [PubMed] [Google Scholar]
- 59.Revenson TA, Marín-Chollom AM, Rundle AG, Wisnivesky J, Neugut AI. Hey Mr. Sandman: Dyadic effects of anxiety, depressive symptoms and sleep among married couples. J Beh Med. 2016;39:225–232. doi: 10.1007/s10865-015-9693-7. [DOI] [PubMed] [Google Scholar]
- 60.Riffin C, Fried T, Pillemer K. Impact of pain on family members and caregivers of geriatric patients. Clin Geriatr Med. 2016;32:663–675. doi: 10.1016/j.cger.2016.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Romano JM, Schmaling KB. Assessment of couples and families with chronic pain. In: Turk D, Melzack R, editors. Handbook of pain assessment. 2. New York, NY: Guilford Press; 2001. pp. 346–262. [Google Scholar]
- 62.Rusbult CE, Van Lange PAM. Why we need interdependence theory. Soc Personal Psychol Compass. 2008;2:2049–2070. [Google Scholar]
- 63.Schlesinger L. Chronic pain, intimacy, and sexuality: A qualitative study of women who live with pain. J Sex Res. 1996;33:249–256. [Google Scholar]
- 64.Schulz R, Beach S, Ives D. Association between depression and mortality in older adults: The Cardiovascular Health Study. Arch Intern Med. 2000;160:1761–1768. doi: 10.1001/archinte.160.12.1761. [DOI] [PubMed] [Google Scholar]
- 65.Schuster TL, Kessler RC, Aseltine RH. Supportive interactions, negative interactions, and depressed mood. Am J Community Psychol. 1990;18:423–438. doi: 10.1007/BF00938116. [DOI] [PubMed] [Google Scholar]
- 66.Schwartz L, Slater MA, Birchler GR, Atkinson JH. Depression in spouses of chronic pain patients: The role of patient pain and anger, and marital satisfaction. Pain. 1991;44:61–67. doi: 10.1016/0304-3959(91)90148-Q. [DOI] [PubMed] [Google Scholar]
- 67.Siegel MJ, Bradley EH, Gallo WT, Kasl SV. The effect of spousal mental and physical health on husbands’ and wives’ depressive symptoms, among older adults: Longitudinal evidence from the Health and Retirement Survey. J Aging Health. 2004;16:398–425. doi: 10.1177/0898264304264208. [DOI] [PubMed] [Google Scholar]
- 68.Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. Oxford, UK: Oxford University Press; 2003. [Google Scholar]
- 69.Smith J, Fisher G, Ryan L, Clarke P, House J, Weir D. Documentation Report Core Section LB. Ann Arbor, MI: Survey Research Center, Institute for Social Research, University of Michigan; 2013. Psychosocial and lifestyle questionnaire, 2006–2010. [Google Scholar]
- 70.Steffick D. Documentation of affective functioning measures in the Health and Retirement Study. Ann Arbor, MI: Survey Research Center, Institute for Social Research, University of Michigan; 2000. [Google Scholar]
- 71.Stephens MAP, Martire LM, Cremeans-Smith JK, Druely JA, Wojno WC. Older women with osteoarthritis and their caregiving husbands: Effects of pain and pain expression on husbands’ well-being and support. Rehabil Psychol. 2006;51:3–12. [Google Scholar]
- 72.Sturgeon JA, Zautra AJ. Resilience: A new paradigm for adaptation to chronic pain. Curr Pain Headache Rep. 2010;14:105–112. doi: 10.1007/s11916-010-0095-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sturgeon JA, Zautra AJ, Arewasikporn A. A multilevel structural equation modeling analysis of vulnerabilities and resilience resources influencing affective adaptation to chronic pain. Pain. 2014;155:292–298. doi: 10.1016/j.pain.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Thomeer MB, Reczek C, Umberson D. Gendered emotion work around physical health problems in mid- and later-life marriages. J Aging Stud. 2015;32:12–22. doi: 10.1016/j.jaging.2014.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Turk DC, Okifuji A, Scharff L. Chronic pain and depression: Role of perceived impact and perceived control in different age cohorts. Pain. 1995;61:93–101. doi: 10.1016/0304-3959(94)00167-D. [DOI] [PubMed] [Google Scholar]
- 76.Umberson D, Williams K, Powers DA, Liu H, Needham B. You make me sick: Marital quality and health over the life course. J Health Soc Behav. 2006;47:1–16. doi: 10.1177/002214650604700101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.US Census Bureau. America’s families and living arrangements. 2013 Available at: http://www.census.gov/hhes/families/data/cps2013A.html.
- 78.Vali FM, Walkup J. Combined medical and psychological symptoms: Impact on disability and health care utilization of patients with arthritis. Med Care. 1998;36:1073–1084. doi: 10.1097/00005650-199807000-00013. [DOI] [PubMed] [Google Scholar]
- 79.Van Der Leeuw G, Eggermont LH, Shi L, Milberg WP, Gross AL, Hausdorff JM, Bean JF, Leveille SG. Pain and cognitive function among older adults living in the community. J Gerontol A Biol Sci Med Sci. 2016;71:398–405. doi: 10.1093/gerona/glv166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Walen HR, Lachman ME. Social support and strain from partner, family, and friends: Costs and benefits for men and women in adulthood. J Soc Pers Relat. 2000;17:5–30. [Google Scholar]
- 81.Woo A, Lechner B, Fu T, Wong CS, Chiu N, Lam H, Pulenzas N, Soliman H, DeAngelis C, Chow E. Cut points for mild, moderate, and severe pain among cancer and non-cancer patients: A literature review. Ann Palliat Med. 2015;4(4):176–183. doi: 10.3978/j.issn.2224-5820.2015.09.04. [DOI] [PubMed] [Google Scholar]
- 82.Zeiss A, Lewinsohn P, Rohde P. Relationship of physical disease and functional impairment to depression in older people. Psychol Aging. 1996;11:572–581. doi: 10.1037//0882-7974.11.4.572. [DOI] [PubMed] [Google Scholar]