Abstract
Background:
After the establishment of Primary Health Care (PHC) program in Iran, health indicators have improved every year. This progress was so rapid that a number of shortcomings and weaknesses of the PHC program remained silent behind its successes. This study aimed to assess the status of Iran’s PHC system (strengths, weaknesses, opportunities and threats) in terms of health system’s control knobs.
Methods:
The search was conducted through two English ‘databases of Web of Knowledge and PubMed, two English publications of Science Direct and Springer and two Persian databases of Magiran and SID. Keywords were selected from MeSH and included primary health care, PHC and Iran in both Persian and English. No time limit was considered.
Results:
Iran’s PHC system has numerous successes in dealing with health system’s control knobs; which largely part of that related to the health network implementation, the role of Behvarz, improvement of health indicators in rural areas and the elimination of urban-rural inequality, but there are some weaknesses, opportunities and threats in the Iranian PHC system as well.
Conclusion:
By considering socio-economic changes the current structure of PHC system needs to be reformed to coordinate with phenomenon of chronic diseases, accidents and aging. The current information system in PHC does not provide the required information for decision makers and policy makers so it needs to be transformed to the electronic system with unique electronic health file for individuals.
Keywords: Primary health care, Health system, Control knob, Iran
Introduction
The most important historical event in the development and delivery of health services is the international community’s decision on the adoption of Primary Health Care (PHC) in order to achieve community justice in access to basic health services (1,2). The general goal was health for all by the year 2000 and the key to achieve such goal is defined PHC services (1, 3–5). Around 1974, Iran began studying on health system. The first signs of the establishment of PHC appeared in 1979, but the full deployment of health care networks occurred in 1985 (6–8).
According to the structure of PHC system in Iran, each village (sometimes a collection of villages) has a health-house, staffed by trained health care provider named Behvarz (Multi-purpose health care worker), who covers health care of 1200 inhabitants. These health-houses are the first level of contact between families and the health system. In the big villages in addition to health-houses, there are rural health centers. Their staff is a qualified physician and a team of up to 10 health workers that provide care for more complex health problems. Each rural health center covers almost 7000 inhabitants. In urban areas health posts and health centers provide similar services as health-houses and rural health centers. This network is managed by district health centers, under the supervision of medical sciences universities. In each province, there is at least one Medical Sciences University (8, 9).
After the establishment of PHC program, health indicators continued to improve every year. This progress was so rapid, therefore, number of shortcomings and weaknesses of the PHC program was not apparent, or remained silent behind the successes of it. Despite the rapid development of the system and obtaining magnificent achievements, this system needs to be modified because of the gradually changing the pattern of the disease, community’s needs and also changing the epidemiological structures (8).
The most important factors that determine the outcomes of each health system are control knobs (10). Control knobs are types of ‘tools’ available for all managers and policy makers to determine health system status. Five control knobs are financing, payment, organizing, regulation and behavior (11). Health system policy makers usually focus on the final goals, which are providing healthcare, responsiveness and fairness in financing. Their important instruments to reach these goals are control knobs. Control knobs’ framework first expressed (12) and further refined (11).
Control knobs are used for understanding the health system and its performance (13) and by considering these facts that most previous studies were about success or weaknesses of Iran’s PHC system and is not done yet any comprehensive study on determining system status in terms of strengths, weaknesses, opportunities and threats from the perspective of health system control knobs, the objective of this study was to determine the status of Iran’s PHC system in terms of health systems five control knobs.
Materials and Methods
The search was carried out for published literature in two English databases of Web of Knowledge and PubMed, two English publications of Science Direct and Springer and two Persian information resources of Magiran and SID, as well as other sources such as books, reports, websites of the Ministry of Health and Medical Education and some international organizations such as WHO and World Bank.
All published evidence about PHC in Iran aimed to review, using the “primary health care” and “PHC” MeSH terms and “Iran” as keywords in both Persian and English databases. No time limit was considered and the search was conducted from 29th of Aug 2014 until 20th of Nov 2014. A repeated search was performed in Aug 2016 to update the data.
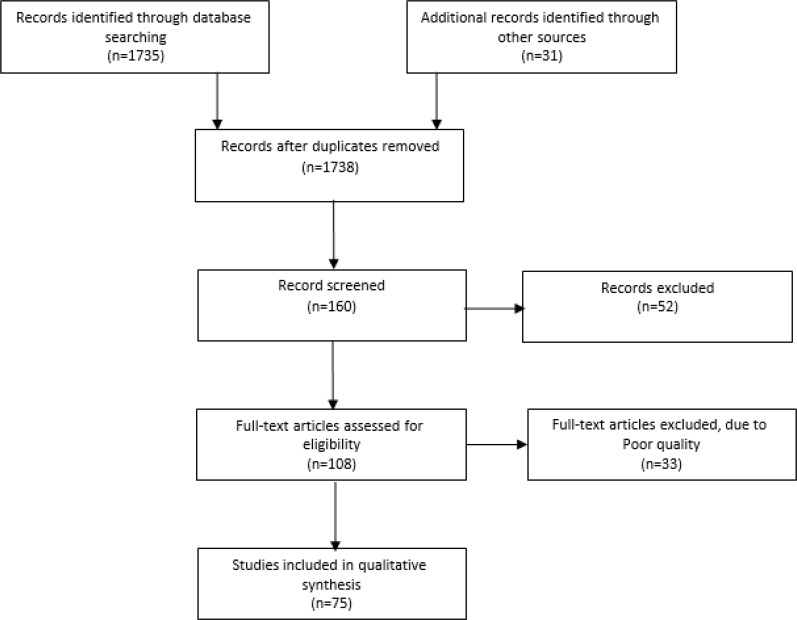
Cross-sectional studies, qualitative studies, reviews and meta-analyses that reported evidence about Iran’s health system status were assessed. All papers that described strengths, weaknesses, opportunities and threats of Iran’s PHC system were included in the study. Studies that only had described Iran’s PHC structure were excluded. A large number of documents were obtained from the search (Fig. 1).
Fig. 1:
Process of study selection
Two authors independently assessed retrieved relevant evidence for further assessment. We used Critical Appraisal Skills Program (CASP) tools to review qualitative studies and systematic reviews (14), for cross-sectional studies, the “National Heart, Lung and Blood Institute, quality Assessment tool for observational cohort and cross-sectional studies” were used (15).
Any disagreement between reviewers was resolved by consensus (11, 16, 17). After reading the selected evidence, the strengths, weaknesses, opportunities and threats of the Iranian PHC system were identified by two authors using Robert and Partner’s control knobs classification in 2004 (10).
Results
Overall, 75 studies were fully studied. The strengths, weaknesses, opportunities and threats of the Iranian PHC system based on health system’s control knobs are shown in Table 1.
Table 1:
Iran’s PHC system’s status based on health system’s control knobs
| Health system status | Internal Status | External Status | ||
|---|---|---|---|---|
| Control Knobs Organizing | Strengths | Weaknesses | Opportunities | Threats |
|
|
|||
| Regulation | Strengths | Weaknesses | opportunities | Threats |
|
|
|||
| Behavior | Strengths | Weaknesses | opportunities | Threats |
| Financing | Strengths | Weaknesses | Threats | |
|
||||
| Payment | Strengths | Weaknesses | Threats | |
| - |
|
|||
The number in parentheses indicates the content references listed at the end of the article.
Discussion
Financing means the way of mobilizing money and method of using it. This control knob affects some health system’s outcomes such as; health status and risk protection (12). The greatest strength of the Iranian PHC system in the financing is related to free of charge services that lead to economic access of communities (18–21). In PHC statement, was emphasized that “the cost of PHC should be payable by the community and government” (21). This prerequisite can be seen in the PHC system of Iran. Nevertheless, inadequate financial resources, discontinuity and unfair distribution of financial resources are the main weaknesses of the Iranian PHC system (22–24). However, the PHC, especially during the implementation phase (particularly in developing countries) requires great financial resources (21).
Financial problems in the health systems are the most common problem in the developing countries. Sabri (2008) in his article by the title of “Thirty years of PHC in the eastern Mediterranean region” reported that most of the countries in eastern Mediterranean region are facing limited funding (17).
Falling Gross Domestic Product (GDP) and health budget have also impacted negatively on PHC performance in many countries in Africa as well (25). Threats observed in the financing control knob are economic problems such as inflation, unemployment, the negative impact of the Iraq war (from Sep 1980 to Aug 1988), a large refugee population mainly from Afghanistan and oil dependent state budget. All of these threats could be influenced financial status of PHC system (8, 11, 22, 26, 27).
PHC system of Iran is facing the problem of shortage of funds for its programs, some issues such as; inefficient health systems and high administrative costs had been highlighted this problem (28). A variety of health service financing systems was expressed as important challenge for PHC system of Iran (29).
Payment implies the methods of paying out of money raised by financing to provider or consumer individuals and organizations (12). Lack of motivations in payment systems used in the Iranian PHC system and the dominance of salary and fee for services payments are weaknesses of payment in the Iranian PHC system (29–31). The Alma-Ata declaration statement noted that “Individual payment on a fee-for-service basis is certainly not a solution widely applied” because in the long-term will increase health costs (21). There is insufficient evidence to support the role of financial incentives to improve the quality of PHC, so financial motivations should be used with caution (32).The main threat in this area related to negative effect of inflation rate at real value of a health staff salaries and wages that make job dissatisfaction among health workers (22).
In general, various studies show that provider’s payment system was not desirable in Iran’s PHC; therefore the salary system could not be an incentive to improve performance, quality and efficiency (29).
In terms of “organizing”, the Iranian PHC system has many strong points including wide network of health centers and the formation of urban and rural branches in this network, which improves health indicators in rural areas and eliminate urban and rural discrimination (11, 21, 25, 33–38). The introduction of a new form of multi-purpose health workers called Behvarz is another achievement of the country’s health system, they are selected from the rural environment and educated in Behvarzi training center for two years and they get hired in the health-house of same village (39, 40). In PHC statement, stated that; “For many developing countries, the most reasonable solution for coverage community with essential health care is to employ community health workers who can be trained in a short time to operate specific tasks” (21) and Iran has particularly been successful in this case. Development of family physician program in rural and in the cities fewer than twenty thousand inhabitants is strength of Iranian PHC system in this area (23, 29, 31, 41–43).
Malekafzali (2014) in his sudy indicated that, one of the dramatic successes of Iran’s PHC system was comprehensive network of health care throughout the country. He emphasized that political commitment of Iranian has been led to the formation of the health network, despite the war conditions in the country (44).
On the other hand, Iran’s PHC system is also facing fundamental weaknesses in “organizing” such as mechanical organizational structure at local level that makes health system gradually weak to respond to the emerging needs of population. However, because of the multiplicity of programs and integrated instructions, PHC system is very formalized and centralized, which have reduced creativity and motivation of human resources (8, 17, 18, 30, 32, 36, 45–50). The PHC faces difficulties in urban areas such as fragmented and scattered PHC system and the lack of referral and goalkeeper system which increase parallel activities and causes ambiguity in patients (12, 17, 25, 29, 32, 33, 43, 47, 51, 52).
Another weakness of organizing is related to PHC traditional information system (paper-based) in collecting and sending data needed for policy-makers. In addition, there is a lack of adequate data management and analysis skills in health care employees (13, 16, 29–31, 53). According to PHC statement,” in order to plan and manage PHC, the right information is essential, but the collection of information has to be kept to the minimum required” (21). Besides, there is no coherent strategy about electronic health record system in Iran’s PHC system (22). The same weakness can also be seen in neighbor courtiers where primary health care system is challenged by under-utilization of the potential of electronic health strategies (16).
Moghadam (2012) in his study pointed out that centralization in decision making, poor analyzability and stratification of information system; are Iran’s PHC system challenges in organizing area (29).
Another fundamental weakness of organizing related to inappropriate human resources management and imbalance between demand and supply of health workers. For example, in some fields such as midwifery, can be seen surplus and unemployment of human resources; and in other fields such as family physician, there is a shortage of man power (8, 22, 43).
The presence of the private sector in the health care system is a big opportunity for Iranian PHC system in the area of organizing (54). In addition, the main threats in this control knob include separated components of the Iranian health governance and providing health services by some organizations that their main mission is not health service delivery such as; municipalities, banks, oil ministry, judicial system, which leads inefficiency in whole system (22). Another threat in this area is related to rapid epidemiological transition, changes in lifestyle and increasing chronic diseases prevalence, which are very important threats and requires appropriate modification in PHC structure (41, 55, 56).
“Regulation” is the use of the government power to change the behavior of individuals and organizations in the health system (10). Regulation is essential for proper implementation of PHC. In this regard, in some countries, new laws are needed or the old laws should be amended to facilitate the development of health services (21).
The main strengths of the Iranian PHC system in regulation and supervision control knobs are appropriate regulation and programs in health and disease prevention such as; the cesarean section rate reduction law in state and referral hospitals and existence of evidence-based clinical practice guidelines in family physician program (57, 58).
However, some weaknesses in this domain can be seen such as; inconsistency among some current health laws with each other and with the general policies at the country level, lack of effective control over providing health services (22), input-based assessments, lack of appropriate data (8) and lack of proper legislation about private sector behavior (29, 30, 43, 47, 59). The main opportunity of this control knob refers to existence of some articles in the Iranian constitution and the country’s twenty-year vision about the health of population and social determinants of health (60). However, the conflict of interest between policy-makers and managers (22) and low awareness of national authorities on health projects such as the family physician program (61) are important threats in this area.
Selecting Behvarz from local community, who is familiar with norms and culture of society and have friendly relations with the local people is the most important strength of Iran’s PHC system in behavior’s control knob (19, 20, 28, 35, 44, 62).
The Iranian health system has some weaknesses in this control knob, such as; lack of health system ownership sense in society members (19) and declined community involvement in solving health problems (31, 63). According to PHC statement; “community participation is the process by which individuals and families adopt responsibility for their own health and develop the capacity to participate for themselves and the community’s development” (21). Efforts have also been made to promote community participation and empowerment of society (17).
Raising adult literacy and its effect on understanding of health messages and self-care of individuals, strong support by the religious authorities based on the importance given to health in the Islamic religion are opportunities of this control knob (21, 64). There are many threats in this area, including changing lifestyles and rising obesity and chronic diseases (11, 18, 26, 65), long-term drug abuse habit among people (about one and a half million of population are addicted) (11, 66, 67), lack of comprehensive sex education for adults and learning sexual information from unreliable sources (68–70) which will have a devastating impact on community health.
Conclusion
The Iranian PHC system has numerous successes in dealing with health system’s control knobs; which largely part of that relates to health network deployment, the role of Behvarz, health indicator improvement in rural areas and the elimination of urban-rural inequality. However, there are some weaknesses in this system, such as; insufficient financial resources and lack of the continuity of financing. PHC system in urban areas is not coordinated and the steady decline in urban health center’s users can be seen. Moreover, by considering socio-economic changes the current structure of PHC system needs to be reformed to coordinate with phenomenon of chronic diseases, accidents and aging. The current information system in PHC does not provide the required information for decision makers and policy makers, so it needs to be transformed to the electronic system with unique electronic health file for people.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
We would like to acknowledge the financial support received from Health Services Management Research Center of Tabriz University of Medical Sciences, Tabriz, Iran.
Footnotes
Conflict of Interests
The authors declare that there is no conflict of interest.
References
- 1.Park JE, Park AK. (2004). Park’s textbook of preventive and social medicine. ed. Samat, Tehran. [Google Scholar]
- 2.Bagyani-Mogadam H, Ehraampoosh MH. (2003). Principles of Health Services. ed. Danesh Cherag-E, Tehran. [Google Scholar]
- 3.Shodjai-Tehrani H, Ebaadi-Fard-Azar F. (2003). Principles of Health Services. ed. Samat, Tehran. [Google Scholar]
- 4.Davoodi S. (2007). Health and Its Determinants. ed. Moaser Asar-E, Tehran. [Google Scholar]
- 5.Neale F. (2005). Western Australian Clinical Governance Guidelines. Health Reform Implementation Taskforce; Australia. [Google Scholar]
- 6.Mehrdad R. (2009). Health system in Iran. JMAJ, 52:69–73. [Google Scholar]
- 7.World Bank (2015). Annual population growth rate for year. The World Bank Group, Based on data from the Central Bank of Iran.
- 8.Naeli J, Mogimi D. (2007). Primary care health promotion policy document. Ministry of Health, Tehran, Iran. [Google Scholar]
- 9.Asadi-Lari M, Sayyari AA, Akbari ME, Gray D. (2004). Public health improvement in Iran--lessons from the last 20 years. Public Health, 118:395–402. [DOI] [PubMed] [Google Scholar]
- 10.Roberts MJ, Hsiao W, Berman P, Reich MR. (2003). Getting health reform right: A guide to improving perfrmance and eqity. ed. Oxford University Press. [Google Scholar]
- 11.Lea P. (2016). Iran: promises and prospects for health. Lancet, 387:918. [DOI] [PubMed] [Google Scholar]
- 12.Heshmati B, Joulaei H. (2016). Iran’s health-care system in transition. Lancet, 387:29–30. [DOI] [PubMed] [Google Scholar]
- 13.Sadoughi F, Shahi M, Ahmadi M, Davaridolatabadi N. (2016). Health information management system for elderly health sector: a qualitative study in Iran. Iran Red Crescent Med J, 18: e21520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anonymous (2013). Critical Appraisal Skills Programme (CASP). Oxford, UK. [Google Scholar]
- 15.Anonymous (2014). Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. National Heart, Lung and Blood Institute, USA: https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort [Google Scholar]
- 16.Maghsoudloo M, Abolhassani F, Lotfibakhshaiesh N. (2016). Connecting Primary Health Care: A Comprehensive Pilot Study. Acta Med Iran, 54:441–7. [PubMed] [Google Scholar]
- 17.Zanganeh Baygi M, Seyadin SH, Rajabi Fard Mazrae No F, Kouhsari Khameneh A. (2016). Adaptation Of Goals And Organizational Structure In Iran’s Primary Healthcare System, A Systematic Review. Payavard, 9:446–458. [Google Scholar]
- 18.Mohammad-Alizadeh CS, Wahlstrom R, Vahidi R, et al. (2009). Barriers to high-quality primary reproductive health services in an urban area of Iran: views of public health providers. Midwifery, 25:721–30. [DOI] [PubMed] [Google Scholar]
- 19.Sheikhattari P, Kamangar F. (2010). How can primary health care system and community-based participatory research be complementary? Int J Prev Med, 1:1–10. [PMC free article] [PubMed] [Google Scholar]
- 20.Tavassoli M. (2008). Iranian health houses open the door to primary care. Bull World Health Organ, 86:585–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eslami M, d’Arcangues C. (2016). Aiming for quality in Iran’s national family planning program—two decades of sustained efforts. Contraception, 93:209–215. [DOI] [PubMed] [Google Scholar]
- 22.Vosoogh Moghaddam A, Damari B, Alikhani S, et al. (2013). Health in the 5th 5-years Development Plan of Iran: Main Challenges, General Policies and Strategies. Iran J Public Health, 42(Supple1): 42–49. [PMC free article] [PubMed] [Google Scholar]
- 23.Khayati F, Saberi M. (2009). Primary Health Care (PHC) an Ever Strategy for Health Equity Extension. J Health Adm, 12:33–40. [Google Scholar]
- 24.Mostafavi Darani F, Ali Abedi H, Riji HM. (2009). Conditions Affecting the Elderly Primary Health Care in Urban Health Care Centers of Iran. Res J Med Sci, 3:202–213. [Google Scholar]
- 25.Moshiri E, Rashidian A, Arab M, Khosravi A. (2016). Using an Analytical Framework to Explain the Formation of Primary Health Care in Rural Iran in the 1980s. Arch Iran Med, 19:16–22. [PubMed] [Google Scholar]
- 26.Lebaron SW, Schultz SH. (2005). Family medicine in Iran: the birth of a new specialty. Fam Med, 37:502–5. [PubMed] [Google Scholar]
- 27.Parkash J, Younis M, Ward W. (2015). Healthcare for the Ageing Populations of Countries of Middle East and North Africa. Ageing Int, 40:3–12. [Google Scholar]
- 28.Bagheri Lankarani K, Alavian SM, Peymani P. (2013). Health in the Islamic Republic of Iran, challenges and progresses. Med J Islam Repub Iran, 27:42–49. [PMC free article] [PubMed] [Google Scholar]
- 29.Moghadam MN, Sadeghi V, Parva S. (2012). Weaknesses and challenges of primary healthcare system in Iran: a review. Int J Health Plann Manage, 27:e121–31. [DOI] [PubMed] [Google Scholar]
- 30.Baygi MZ, Seyedin H. (2013). Imbalance between Goals and Organizational Structure in Primary Health Care in Iran-a Systematic Review. Iran J Public Health, 42:665–672. [PMC free article] [PubMed] [Google Scholar]
- 31.Mehrolhassani M, Jafari Sirizi M, Poorhoseini S, Yazdi Feyzabadi V. (2012). The Challenges of Implementing Family Physician and Rural Insurance Policies in Kerman Province, Iran: A Qualitative Study. J Health Develop, 1:193–206. [Google Scholar]
- 32.Khayatzadeh-Mahani A, Takian A. (2014). Family physician program in Iran: considerations for adapting the policy in urban settings. Arch Iran Med, 17:776–8. [PubMed] [Google Scholar]
- 33.Nasseri K, Sadrizadeh B, Malek-Afzali H, et al. (1991). Primary health care and immunisation in Iran. Public Health, 105:229–238. [DOI] [PubMed] [Google Scholar]
- 34.Mohammad-Alizadeh S, Wahlström R, Vahidi R, Johansson A. (2009). Women’s perceptions of quality of family planning services in Tabriz, Iran. Reprod Health Matters, 17:171–80. [DOI] [PubMed] [Google Scholar]
- 35.Aghajanian A, Mehryar AH, Ahmadnia S, Kazemipour S. (2007). Impact of rural health development programme in the Islamic Republic of Iran on rural-urban disparities in health indicators. East Mediterr Health J, 13:1466–75. [DOI] [PubMed] [Google Scholar]
- 36.Rafiei M, Ezzatian R, Farshad A, et al. (2015). Occupational Health Services Integrated in Primary Health Care in Iran. Ann Glob Health, 81:561–7. [DOI] [PubMed] [Google Scholar]
- 37.Singh D, Negin J, Otim M, Orach CG, Cumming R. (2015). The effect of payment and incentives on motivation and focus of community health workers: five case studies from low-and middle-income countries. Hum Resour Health, 13:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Simbar M. (2012). Achievements of the Iranian family planning programmes 1956–2006. East Mediterr Health J, 18:279–86. [PubMed] [Google Scholar]
- 39.Mansouri N, Gharaee B, Shariat SV, et al. (2009). The change in attitude and knowledge of health care personnel and general population following trainings provided during integration of mental health in Primary Health Care in Iran: a systematic review. Int J Ment Health Syst, 3:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shadpour K. (2000). Primary health care networks in the Islamic Republic of Iran. East Mediterr Health J, 6:822–5. [PubMed] [Google Scholar]
- 41.Sohrabi MR, Albalushi RM. (2011). Clients’ satisfaction with primary health care in Tehran: A cross-sectional study on Iranian Health Centers. J Res Med Sci, 16:756–62. [PMC free article] [PubMed] [Google Scholar]
- 42.Benyoussef A, Christian B. (1977). Health care in developing countries. Soc Sci Med, 11:399–408. [DOI] [PubMed] [Google Scholar]
- 43.Mehryar A. (2004). Primary Health Care and the Rural Poor in the Islamic Republic of Iran. http://web.worldbank.org/archive/website00819C/WEB/PDF/IRAN_PRI.PDF
- 44.Malekafzali H. (2014). Primary Health case in Islamic Republic of Iran. http://journals.tums.ac.ir/sjsph/article-1-5150-en.pdf (In Persian).
- 45.Malekafzali H. (2009). Primary Health Care in the Rural Area of the Islamic Republic of Iran. Iran J Public Health, 38(Suppl.1):69–70. [Google Scholar]
- 46.Abou Basha LM, Fadali GA, Nour BM, Abdalla MS. (1989). Uncommon complications of human fascioliasis in Alexandria. J Egypt Soc Parasitol, 19(2):743–9. [PubMed] [Google Scholar]
- 47.Farzadfar F, Murray CJL, Gakidou E, et al. (2012). Effectiveness of diabetes and hypertension management by rural primary health-care workers (Behvarz workers) in Iran: a nationally representative observational study. Lancet, 379:47–54. [DOI] [PubMed] [Google Scholar]
- 48.Tehrani FR, Simbar M, Abedini M. (2011). Reproductive morbidity among Iranian women; issues often inappropriately addressed in health seeking behaviors. BMC Public Health, 11:863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Javanparast S, Coveney J, Saikia U. (2009). Exploring health stakeholders’ perceptions on moving towards comprehensive primary health care to address childhood malnutrition in Iran: a qualitative study. BMC Health Serv Res, 9:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Baygi MZ, Seyedin H, Salehi M, Sirizi MJ. (2015). Structural and contextual dimensions of Iranian primary health care system at local level. Iran Red Crescent Med J, 17: e17222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jafari F, Eftekhar H, Pourreza A, Mousavi J. (2010). Socio-economic and medical determinants of low birth weight in Iran: 20 years after establishment of a primary healthcare network. Public Health, 124:153–158. [DOI] [PubMed] [Google Scholar]
- 52.Forouzan AS, Ghazinour M, Dejman M, Rafeiey H, San Sebastian M. (2011). Testing the WHO responsiveness concept in the Iranian mental healthcare system: a qualitative study of service users. BMC Health Serv Res, 11:325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Farahbakhsh M, Nikniyaz AR, Zakeri A. (2006). Survey of data management in health care delivery system in the East Azarbaijan province. Health System, 2:51–58. [Google Scholar]
- 54.Schieber G, Klingen N. (1999). Islamic Republic of Iran Health Financing Reform in Iran: Principles and Possible Next Steps. Health Economic Congress, World Bank, Washington, DC. [Google Scholar]
- 55.Habibzadeh F. (2012). The control of non-communicable diseases in rural Iran. Lancet, 379:6–7. [DOI] [PubMed] [Google Scholar]
- 56.Rahmanian K, Shojaie M. (2012). The prevalence of pre-hypertension and its association to established cardiovascular risk factors in south of Iran. BMC Res Notes, 5:386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sadeghi Poor Roodsari HR, Heidari AB, Ghazy Sherbaf P. (2005). Study of The Ratea nd Causes of Islamshahr Urban Residents’ voiding to refer to The Health Centers For Receiving Health Services (2003). Tehran Univ Med J, 63:141–150. [Google Scholar]
- 58.Yazdizadeh B, Nedjat S, Mohammad K, et al. (2011). Cesarean section rate in Iran, multidimensional approaches for behavioral change of providers: a qualitative study. BMC Health Serv Res, 11:159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ekman B, Pathmanathan I, Liljestrand J. (2008). Integrating health interventions for women, newborn babies, and children: a framework for action. Lancet, 372:990–1000. [DOI] [PubMed] [Google Scholar]
- 60.Jafari Sirizi M, Yazdi Fiezabadi V, Aleksanyan AS. (2010). Major Policies in Health Area in Islamic Republic of Iran During Past 30 Years: Results, Challenges and Strategies. Res J Biol Sci, 5:683–691. [Google Scholar]
- 61.Asadi F, Hosseini A, Moghaddasi H, Nasr Haydarabadi N. (2012). Primary Health Care Information Systems in Health Centers of Tehran, Iran. Health Inform Manage, 9:1–10. [Google Scholar]
- 62.Javanparast S, Baum F, Labonte R, et al. (2012). The experience of community health workers training in Iran: a qualitative study. BMC Health Serv Res, 12:291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zohour A, Paryani A. (2001). Client satisfaction with the performance of home health and rural health centers in 1378 Qorveh city. ZUMS Journal, 9:74–77. [Google Scholar]
- 64.Vahidnia F. (2007). Case study: fertility decline in Iran. Popul Environ, 28:259–266. [Google Scholar]
- 65.Ziaoddini H, Kelishadi R, Kamsari F, et al. (2010). First nationwide survey of prevalence of weight disorders in Iranian children at school entry. World J Pediatr, 6:223–7. [DOI] [PubMed] [Google Scholar]
- 66.Yasamy MT, Shahmohammadi D, Bagheri Yazdi SA, et al. (2001). Mental health in the Islamic Republic of Iran: achievements and areas of need. East Mediterr Health J, 7:381–91. [PubMed] [Google Scholar]
- 67.Mojtahedzadeh V, Razani N, Malekinejad M, et al. (2008). Injection drug use in Rural Iran: integrating HIV prevention into iran’s rural primary health care system. AIDS Behav, 12:S7–12. [DOI] [PubMed] [Google Scholar]
- 68.Shirpak K, Chinichian M, Maticka-Tyndale E, et al. (2008). A Qualitative Assessment of the Sex Education Needs of Married Iranian Women. Sex Cult, 12:133–150. [Google Scholar]
- 69.Joulaei H, Motazedian N. (2013). Primary Health Care Strategic Key to Control HIV/AIDS in Iran. Iran J Public Health, 42:540–541. [PMC free article] [PubMed] [Google Scholar]
- 70.Mandel JS, Brickley DB. (2008). AIDS prevention research in low and middle-income countries: generating the evidence upon which local decisions are made. AIDS Behav, 12:S1–6. [DOI] [PubMed] [Google Scholar]
- 71.Rezayie A. (2004). The necessity of activating healthcare centers and proposes several operational approaches. Teb va Tazkiyeh, 13:9–0. (In Persian) [Google Scholar]
- 72.Esteghamati A, Khalilzadeh O, Anvari M, et al. (2009). The economic costs of diabetes: a population-based study in Tehran, Iran. Diabetologia, 52:1520–7. [DOI] [PubMed] [Google Scholar]
- 73.Adib-Hajbaghery M, Aghahoseini S. (2007). The evaluation of disability and its related factors among the elderly population in Kashan, Iran. BMC Public Health, 7:261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Delbari A, Roghani RS, Tabatabaei SS, Lökk J. (2010). A Stroke Study of an Urban Area of Iran: Risk Factors, Length of Stay, Case Fatality, and Discharge Destination. J Stroke Cerebrovasc Dis, 19:104–9. [DOI] [PubMed] [Google Scholar]
- 75.Barzegar MA, Djazayery A. (1981). Evaluation of rural primary health care services in Iran: report on vital statistics in West Azarbaijan. Am J Public Health, 71:739–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ahmad Kiadaliri A, Najafi B, Haghparast-Bidgoli H. (2011). Geographic distribution of need and access to health care in rural population: an ecological study in Iran. Int J Equity Health, 10:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Akbari N, Ramezankhani A, Pazargadi M. (2013). Accelerators/decelerators of achieving universal access to sexual and reproductive health services: a case study of Iranian health system. BMC Health Serv Res, 13:241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bristol N. (2010). US region to model health service on Iranian system. Lancet, 375:625. [DOI] [PubMed] [Google Scholar]
- 79.Javanparast S, Baum F, Labonte R, Sanders D. (2011). Community health workers’ perspectives on their contribution to rural health and well-being in Iran. Am J Public Health, 101:2287–2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Farzadfar F, Danaei G, Namdaritabar H, et al. (2011). National and subnational mortality effects of metabolic risk factors and smoking in Iran: a comparative risk assessment. Popul Health Metr, 9:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rezapur-Shahkolai F, Naghavi M, Shokouhi M, Laflamme L. (2008). Unintentional injuries in the rural population of Twiserkan, Iran: a cross-sectional study on their incidence, characteristics and preventability. BMC Public Health, 8:269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nabilou B, Rasouli J. (2013). Quality of family health services in selected cities of west azerbaijan province health posts from reality to expectations of service consumers. J Urmia Univ Med Sci, 24:277–285. [Google Scholar]
- 83.Joulaei H, Motazedian N. (2013). On the Effectiveness of Primary Health Care System in Controlling HIV/AIDS in Iran. Iran J Public Health, 42:783–784. [PMC free article] [PubMed] [Google Scholar]
- 84.Nabilou B, Farokh Eslamlou H. (2013). Assessing quality of family health services in view points of service users in urmia health posts. J Urmia Nurs Midwifery Fac, 11:343–349. [Google Scholar]
- 85.Shahidzadeh-Mahani A, Omidvari S, Baradaran HR, Azin SA. (2008). Factors affecting quality of care in family planning clinics: a study from Iran. Int J Qual Health Care, 20:284–90. [DOI] [PubMed] [Google Scholar]
- 86.Bhatti JA, Salmi L-R. (2008). Injury in the Developing World—From Prevention to Care. Int J Emerg Med, 1:235–250. [Google Scholar]