Abstract
In this study, we analysed 180 eyes with myopia in order to determine the “criticai” length of bulbar axis for the occurrence of retinal ruptures as the main cause for retinal detachment.
After the focused ophthalmological assessment, ultrasonic measurement of the bulbar axis length, indirect binocular ophtalmoscopy, we analysed diag-nosed retinal ruptures according to the shape and axis length.
Mean age of our patients was between 48,43 and to 51,60 years with SD ranging from 13,88 to 18,45. The study included 102 (56,6%) male and 78 (43,3%) female patients; there was no statistically significant difference regarding the occurrence of retinal ruptures between male and female patients compared to the axis length. Most dominant was round (28,2%), then oval (25%) category - multiple small ruptures (19,2%), and horseshoe-shaped (15,3%), and finally the ruptures with operculum.
We consider the length of bulbar axis ranging from 24,52 mm to 26,51 mm to be a predictive factor in the occurrence of retinal rupture, and later in retinal detachment.
Keywords: myopia, “critical”, length of bulbar axis, retinal rupture
INTRODUCTION
Every day ophthalmologists witness the occurrence of retinal detachment in people with myopia. The retinal detachment involves separation of the neurosensory retina from the pigmented retinal epithelium and it is one of the emergency states in ophthalmology. Many researches showed that in the pathogenesis of retinal detachment, an important role is played by peripheral retinal degenerations, retinal ruptures, viteroretinal tractions and detachment of vitreous cavity (1,2). Also associated with myopia are 42% of retinal detachments (3). Prevalence of myopia-related refraction among adults is 20 % in the USA, in Western European countries 26,6%, UK 53,6%, and in Australia 77% (4,5,6). Early detection of the predisposing lesions and retinal ruptures and application of the adequate prophylactic measures have important role in prevention of retinal detachment (7). Retinal ruptures represent a break into retina continuity, which affects all layers except pigmented epithe- lia. Rupture existence was first noticed by Helmholtz, while Gonin pointed out the importance of its surgical closure in order to treat retinal detachment (8). In morphological sense, we distinguish horseshoe-shaped ruptures with operculum, round or oval, U-shaped rup- tures, incomplete or layered erosions. Desinsertio s. dialysis retinae represent special shape of retinal ruptures when the retina is separated in the area of ora serata (9). The main goal of this research is to find the “critical length” of the bulbus in case of which we will find the largest number of retinal ruptures as a direct cause for the occurrence of retinal detachment.
PATIENTS AND METHODS
The study is conducted as clinical, prospective, and controlled. We analysed 180 eyes of the patients with myopia. Study involved all the patients who have veri-fied myopia of 0,25 dsph or more by the ophthalmol-ogy methods of examination, regardless of gender, profession and stage o diseases, and children over 7 years. From the study excluded were the patients with the acute ophthalmology diseases, and other diseases which cause less transparency in the optical mediums. After ophthalmology anamnesis which is analysed as personal with special review of clarity of sight and symptoms: “flying fly”, “sparks” and occurrence of “curtain” within field of vision, we analysed family history in terms of positive anamnesis in clos-est relatives. Afterward we measure the length of the bulbar axis by the ultrasonic A scan method.
We conducted examination of the chorioretinae in the indirect binocular biomicroscopy using Volk lens of 90 dsph and Goldmann contact prism. All noticed changes were noted on the Amsler-Dubois scheme, modified according to Schepens, which involves the area of ora serata, using Meyer-Schwickerath symbols. In the elements of vital statistics, we analysed samples according to gender and age. In case of parametric values, we used Student t test, and for the nonparametric data Chi-square test. All eyes were divided into three groups according to the length of bulbar axis:
from 22,01 to 24,51 mm
from 24,52 to 26,51 mm
from 26,52 to 32,99 mm
FIGURE 1.
A scan echogram in different length axis bulbi
RESULTS
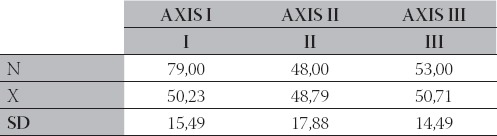
Patient’s age is placed in ration to the length of bulbar axis. Mean patients age ranging from 48,79 to 50,71 with SD mean ranging from 14,49 to 17,88 (Table 1).
TABLE 1.
Patients’ age compared to the bulbar axis length
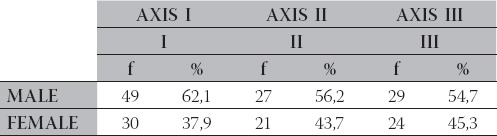
In case of all axis length, male patients were more present than female. There was no statistically significant differ-ence regarding gender and bulbar axis length (Table 2).
TABLE 2.
Distribution of patients according to gender compared to axis
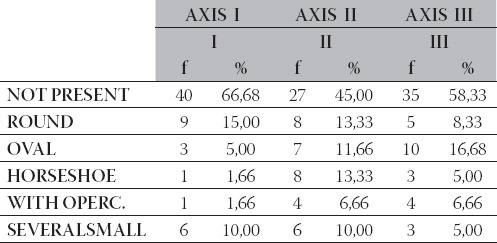
We analysed the retinal ruptures according to shape at location equator -ora serata compared to the length of bulbar axis. According to shape, we divide them into: round, oval, horseshoe-shaped, ruptures with opercu-lum and category of several small ruptures (Table 3).
TABLE 3.
Distribution of peripheral ruptures according to axis
Within the baseline of 180 tested eyes, we found 78 (43,3%) retinal ruptures, and without them among 102 (56,6%) tested eyes (Table 4).
TABLE 4.
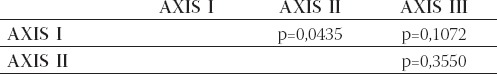
Chi-square test α=0.05 (*fields in orange represent significance) related to Table 3.
DISCUSSION
Retinal ruptures within eye of myopia patients are a huge threat of the occurrence of retinal detachment, which results in a decrease of sight and damage to other functions of sight. Ruptures can vary in shape and location. In case of diagnosed ruptures in one eye, it is rec-ommended to test also the other “healthy eye”. Bilateral ruptures are often combined with their symmetric localization. Ruptures can be located in various sectors and meridians of the fundus, including macula (10,11). But the upper temporal quadrant is considered to be the most frequent location of ruptures in general, 67% ac-cording to Evertt and 55% according to Tulloh (12,13). In this study, we analysed the occurrence of reti-nal rupture in case of various lengths of bulbar axis. Mean age of our patients varied from 48,43 to 51,60 with SD ranging from 13,88 to 18,45. After in-group analyses of retinal rupture numbers, we did not find any statistical-ly significant difference related to patient’s age (Table 1). This study covered 102 (56,6%) males and 78 (43,3%) females. Analysis between groups with Chi-square test did not find any statistically significant difference regarding the occurrence of retinal ruptures among male and female patients compared to the axis length (Table 2). In our patients, we found 78 (43,3%) retinal ruptures, located in the area of equator-ora serata in different quadrants, usually in the upper temporal. We analysed those retinal ruptures according to shape. The most frequent were round (28,2%), then oval (25%), category of multiple smaller ruptures (19,2%) and horseshoe-shaped (15,3%), and finally ruptures with operculum. From a total of 78 detected retinal ruptures, 33 (42,3%) were in the second group with the length of axis varying from 24,52 mm to 26,51 mm (Table 3). After the statistical analysis of groups with Chi-square test, we found statistical significance between the first and sec-ond groups with p=0,0435 for alpha = 0,05 (Table 4). Based on the data obtained, we can conclude that in the group with myopia and above the mentioned axis length, the frequency of ruptures is the highest, or we can consider this axis length as predictive for the occur-rence of retinal detachment. Also, with this we proved the existence of positive correlation between the fre-quency of retinal ruptures and the bulbar axis length. Occurrence of retinal ruptures in myopia eye must be taken seriously. Patients’ complaints are usually meta- morphopsy, micropsy, glittering in front of the eye and opacities. In some cases ruptures are “silent”; they pass undetected, and are discovered during routine examinations. Retinal ruptures with edges without vitreo-retinal tractions do not need to be preventively treated (16,17). But, in cases of myopia, aphakia, pseudoaphykia, in persons actively participating in sport, in patients with a positive family history or similar changes in the other eye, it is recommended to close the ruptures in order to prevent retinal detachment (18,19). The fol-lowing methods can be applied: laser photocoagulation, retinopexis, scleral bucking, and injections of expanding gas into the vitreous cavity (20, 21, 22). After these interventions, complications can oc-cur such as macular pucker from 0 to 2,2 %, degeneration of vitreous cavity from 2,1 to 6,7% and retina detachment from 1,8 to 6,2% of cases (18,19).
CONCLUSION
We consider the ength of bulbar axis ranging from 24,52 mm to 26,51 mm to be a predictive factor in the occurrence of retinal rupture, and later in retinal detachment.
In order to prevent retinal detachment in the eye with myopia, we suggest a detailed examination of the eye fundus in case of patients with the above mentioned length of bulbar axis. Diagnosed retinal ruptures can be adequately surgically treated as prophylaxis.
REFERENCES
- 1.Akyol N, Kukner A.S, Ozdemir T, Esmerligil S. Choroidal and retinal blood flow changes in degenerative myopia. Can. J. Oph-thalmol. 1996;31(3):113–119. [PubMed] [Google Scholar]
- 2.Ghazi N.G, Green W.R. Pathology and pathogenesis of retinal detachment. Eye. 2002;16(4):411–421. doi: 10.1038/sj.eye.6700197. [DOI] [PubMed] [Google Scholar]
- 3.Burton T.C. The influence of refractive error and lattice degeneration on the incidence of retinal detachment, From the Eye institute, Wisconsin. Tr. Am. Ophth. 1989:143–157. [PMC free article] [PubMed] [Google Scholar]
- 4.Logan N.S, Davies L.N, Mallen E.A, Gilmartin B. Ametropia and ocular biometry in a UK university student population. Optom. Vis. Sci. 2005;82(4):261–266. doi: 10.1097/01.opx.0000159358.71125.95. [DOI] [PubMed] [Google Scholar]
- 5.Wensor M, McCarty C.A, Taylor H.R. Prevalence and risk fac-tors of myopia in Victoria, Australia. Arch. Ophthalmol. 1999;117(5):658–663. doi: 10.1001/archopht.117.5.658. [DOI] [PubMed] [Google Scholar]
- 6.Kempen J.H, Mitchell P, Lee K.E, Tielsch J.M, Broman A.T, Taylor H.R, Ikram M.K, Congdon N.G, O’Colmam B.J. Eye Dis-eases Prevalence Research Group. “The prevalence of refractive errors among adults in the United States, Western Europe, and Australia.”. Arch. Ophthalmol. 2004;122(4):495–505. doi: 10.1001/archopht.122.4.495. [DOI] [PubMed] [Google Scholar]
- 7.Mastropasqua L, Carpineto P, Ciancaglini M, Falconio G, Gallenga P.E. Treatment of retinal tears and lattice degenerations in fellow eyes in high risk patients suffering retinal detachment: a prospective study. Br. J. Ophthalmol. 1999;83(9):1046–1049. doi: 10.1136/bjo.83.9.1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gonin J, Helmholtz I. In: Clinical characteristics of retinal detachment, Retinal detachement, surgical therapy, pre-vention. Blagojević M, editor. Beograd: Eye Clinic “Đorđe Nešić PhD MD”; 1976. p. 7992. [Google Scholar]
- 9.Kanski J. Patogenesis of retinal detach-ment. Oxford: Butterworta, Heinemann LTD; 1994. Clinical Ophthalmology; p. 317.p. 328. [Google Scholar]
- 10.Katušić D, Klinger M, Šikić J, Kordić R, editors. The find of the other eye in case of retinal detachement regmatogenes. JOA. 1986;24(3-4):193–195. [Google Scholar]
- 11.Peyman A.G, Schulman A.J. Vitreus changes in myopia. Intravitreal surgery Principles and Practice. Prentice-Hall International Inc: Appleton & Lange USA. 1994:29–31. [Google Scholar]
- 12.Everett W.G, Katzin D. Merdional distribution of retinal breaks in aphakic retinal detachment. Am. J. Ophthalmol. 1968;66:928–932. doi: 10.1016/0002-9394(68)92815-8. [DOI] [PubMed] [Google Scholar]
- 13.Tulloh N. Revue Chibret, No-Spec. Prevention du decollement delaretina. Clermont: Ferrand: 1974. [Google Scholar]
- 14.Michels R.G, Wilkinson C.P, Rice T.A. Retinal detachment. Prevention of retinal detachment. 1990:1093–1107. [Google Scholar]
- 15.Blagojević M. Clinical characteristics of retinal detachment, Reti-nal detachement, surgical therapy, prevention. Beograd: Eye Clinic “Đorđe Nešić PhD MD”; 1976. pp. 79–92. [Google Scholar]
- 16.American Academy of Ophthalmology. Preferred practice pattern: retinal detachment. San Francisco: AAO; 1990. [Google Scholar]
- 17.Pierro I, Camesasca F.J, Mischi M, Brancato R. Peripheral retinal changes and axial myopia. Retina. 1992;12:12–17. doi: 10.1097/00006982-199212010-00003. [DOI] [PubMed] [Google Scholar]
- 18.Jones W.L, Cavallerano A.A, Margan K.M, Semes L.P, Sherman J.F, Vandervort R.S, Wooldridge R.P. Optometric clinical practice guideline care of the patient with retinal detachment and related peripheral vitreoretinal disease. U.S.A, St. Louis: AOA; 1995. reviewed 2004. [Google Scholar]
- 19.Meyer-Schwickerath G, Frider M. Prophylaxis of retinal detach-ment. Trans. Ophthalmol. Sc.UK. 1980;100:56–65. [PubMed] [Google Scholar]
- 20.Alimanović Halilović E. Laser in ophthalmology. Laser photoco-agulation in retinal breaks and partial rhegmatogenous retinal detachment. Sarajevo: The Institute for Scientific and Development Clinical Center University of Sarajevo; 2006. pp. 69–72. [Google Scholar]
- 21.Alimanović Halilović E. Correlation Between Refraction Level and Retinal Breaks in Myopic Eye. Bosn. J. Basic Med. Sci. 2008;8(4):346, 349. doi: 10.17305/bjbms.2008.2895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ehlers J.P, Shah C.P. Retinal break. Retinal detachment. Philadelphia USA: Wolters Kluwer, Lippincott Williams & Wilkins; 2008. The Wills eye manual office and emergency room diagnosis and treatment of eye disease; pp. 275–279. [Google Scholar]


