Abstract
Objective
To assess whether differences in readmission rates between safety-net hospitals (SNH) and non-SNHs are due to differences in hospital quality, and to compare the results of hospital profiling with and without SES adjustment.
Importance
In response to concerns that quality measures unfairly penalizes safety-net hospitals (SNH), NQF recently recommended that performance measures adjust for socioeconomic status (SES) when SES is a risk factor for poor patient outcomes.
Methods
Multivariate regression was used to examine the association between SNH status and 30-day readmission after major surgery. The results of hospital profiling with and without SES adjustment were compared using the CMS Hospital Compare and the Hospital Readmissions Reduction Program (HRRP) methodologies.
Results
Adjusting for patient risk and SES, patients admitted to SNHs were not more likely to be readmitted compared to patients in in non-SNHs (AOR 1.08;95% CI:0.95-1.23;P = 0.23). The results of hospital profiling based on Hospital Compare were nearly identical with and without SES adjustment (ICC 0.99, kappa 0.96). Using the HRRP threshold approach, 61% of SNHs were assigned to the penalty group versus 50% of non-SNHs. After adjusting for SES, 51% of SNHs were assigned to the penalty group.
Conclusion
Differences in surgery readmissions between SNHs and non-SNHs are due to differences in the patient case mix of low-SES patients, and not to differences in quality. Adjusting readmission measures for SES leads to changes in hospital ranking using the HRRP threshold approach, but not using the CMS Hospital Compare methodology. CMS should consider either adjusting for the effects of SES when calculating readmission thresholds for HRRP, or replace it with the approach used in Hospital Compare.
Introduction
Nearly one fifth of Medicare inpatients are rehospitalized within 30 days at a cost of over $17 billion per year.1 Readmission rates vary nearly three-fold across hospital referral regions.2 Under the CMS Hospital Readmissions Reduction Program, hospitals with excessive numbers of readmissions will be subject to up to 3% reductions in Medicare reimbursements in 2015.3 CMS initiatives linking hospital payments to performance have led to 1.3 million fewer hospital-acquired conditions and 50,000 fewer deaths between 2010 and 2013, generating savings of $12 billion.4 Early reports show that the readmission rate for Medicare patients between 2012 and 2013 dropped by about 0.5 to 1% resulting in an estimated 150,000 fewer readmissions.5
There is, however, widespread public concern that current readmission measures unfairly penalize safety-net hospitals that care for large numbers of vulnerable patients. Although socially disadvantaged patients may be more likely to require hospital readmission due to factors beyond a hospital's control, CMS does not risk adjust for socioeconomic status (SES). Critics of this decision note that factors such as poverty, low levels of formal education, lack of social or community support, lack of access to ambulatory care, and poor living conditions may predispose patients to readmission in ways that are unrelated to the quality of care received during a patient's initial hospitalization.6 These concerns led the National Quality Forum to recommend, in its August 2014 report, that quality measures adjust for SES when there is empiric evidence that SES influences outcomes.7 Responding to the NQF recommendations, CMS stated that adjusting for SES “would establish a different standard of care for providers based on the SES of the patients they care for and mask disparities in the quality of care provided.” CMS also asserted that [NQF's recommendation] “is premature, given the lack of evidence that has been generated to warrant such a recommendation.”8
In this study, we examined the impact of SES adjustment on hospital surgical readmission rates using all-payer data from New York State. We chose readmissions after surgery - as opposed to readmissions following acute myocardial infarctions, heart failure or pneumonia – because surgery readmissions may be more closely associated with quality of care than medical readmissions.9-11 We sought to answer three questions. First, does adjusting for SES lead to significant changes in hospital rankings? Second, are hospitals that treat predominantly low-SES patient populations more likely to be ranked as low-performing hospitals compared to hospitals that treat few low-SES patients when performance is not risk adjusted for SES? And third, are there systematic differences in performance between hospitals with high concentrations of low-SES patients compared to other hospitals? Answering these questions should help policy makers reduce hospital readmissions without inadvertently worsening health care disparities.
Methods
Data Source
This analysis used data from the Health Cost and Utilization Project Inpatient Database (HCUP SID) for New York State (NYS) between 2009 and 2011. The SID contains all-payer population-based data for all inpatient discharge records from non-Federal short term acute care hospitals.12 The NYS SID includes information on patient demographic characteristics, admission source, type of admission (urgent, emergency, elective), ICD-9-CM diagnostic and procedure codes, Agency for Healthcare Research and Quality comorbidity measures,13 payer source, in-hospital mortality, and hospital identifiers. The NYS SID also contains a unique encrypted patient identifier and a date indicator to identify readmissions.14 Because the SID does not provide data on patient-level socioeconomic factors such as education, occupation or income, we used Medicaid, dual eligibility status (Medicare and Medicaid), and homelessness to identify low-SES patients.15 The Institutional Review Board of the University of Rochester School of Medicine exempted this study from review.
Patient Population
We limited our study sample to patients undergoing one of six major surgeries: isolated coronary artery bypass grafting (CABG), pulmonary lobectomy, endovascular repair of abdominal aortic aneurysm (AAA), open repair of AAA, colectomy, and hip replacement using the coding algorithm by Tsai and colleagues.9 These procedures were chosen because patients undergoing major surgery are at high risk for readmission, and readmission rates for these surgeries vary significantly across US hospitals.9 Furthermore, CMS is planning to add readmission measures for CABG and hip arthroplasty to the Hospital Readmission Reduction Program (HRRP).16 For our primary study sample, we identified 138,621 adult patients (age ≥ 18 years) who underwent one of the six major surgeries, were discharged from the hospital alive, and were not transferred to another acute care hospital. We excluded 3,582 patients who were discharged in December of 2011 because 30-day readmission information was not available for these patients. We also excluded patients with missing information on race (5,553) or emergency status (239). The final analytic sample consisted of 129,247 records from 185 hospitals.
Hospital performance assessment
We constructed two risk adjustment models for all-cause 30-day readmissions: (1) baseline model without SES adjustment; and (2) SES-enhanced model (Appendix 1). The baseline model included demographics (age, sex), urgency of surgery, comorbidities, transfer status, and surgery procedure. We used the AHRQ Elixhauser algorithm instead of the CMS risk adjustment model because we did not have access to outpatient claims data. The Elixhauser algorithm is widely used in risk adjustment models based on administrative data.13, 17-19
Using an approach similar to that employed by CMS, hospital performance was estimated using hierarchical logistic regression specifying hospitals as a random effect. The empirical-Bayes estimate of the hospital effect from the above risk adjustment model was exponentiated to yield an adjusted odds ratio.20 The hospital adjusted odds ratio (AOR) is the likelihood that patients undergoing surgery at a specific hospital will be readmitted compared to patients in the average hospital. Hospitals with AOR significantly less than or greater than 1 (P<0.05) were categorized as high-performance or low-performance outliers, respectively. We also used the CMS HRRP threshold approach, which assigns hospitals to a financial penalty group if they have any readmissions in excess of their predicted readmission rates (point estimate for AOR > 1), without regard for statistical significance.
Analysis of impact of SES adjustment on performance ranking
We then quantified the level of agreement between hospital performance ranking with or without SES adjustment. First, we examined the level of agreement for the hospital AOR using the intraclass correlation coefficient. Second, we performed a kappa analysis to examine the amount of agreement for the categorical measures of hospital quality (high, low, and average performance hospitals) with and without SES adjustment. Third, we compared the proportion of safety-net hospitals (SNHs) and non-SHNs assigned to the penalty group, based on the CMS HRRP threshold approach, with and without SES adjustment. Hospitals were classified into quartiles based on the proportion of low-SES patients admitted (all medical and surgical admissions): low (<21%), medium (≥21 – 30%), medium-high (≥30-44), and high (≥ 44%). Using an approach similar to prior studies, we defined safety-net hospitals (SNH) as hospitals serving the highest quartile of low-SES patients.15, 21, 22
Next, we examined whether SNHs were more likely to readmit surgical patients compared to non-SHNs. We estimated the association between hospital SES quartiles and the likelihood of readmission by including hospital SES quartile in our baseline model (without patient SES), using non-hierarchical logistic regression, to quantify the “between-hospital” difference in readmissions. We then re-estimated this model, including both the hospital SES quartile and a patient-level SES variable, to determine whether potential differences in performance across hospital SES quartiles was due to differences in hospital SES case mix (proportion of low-SES patients) or differences in hospital performance unrelated to differences in case mix. If we find that hospital SES is associated with readmissions, but that this effect became negligible after adjusting for patient SES, then the primary driver for hospital-level differences in readmissions is patient SES casemix, as opposed to systematic differences in quality between SNHs and non-SNHs.7
To further clarify whether differences in readmission rates between SNHs and non-SNHs were attributable to differences in hospital performance versus differences in hospital case mix, we modified the baseline model by including patient SES and hospital indicator variables as fixed effects. This model estimates the association between patient SES and readmission after controlling for other patient risk factors and hospital performance. We then compared the estimated coefficient for patient SES in this model with the baseline model without hospital fixed effects. If controlling for hospital fixed effects (performance) has minimal impact on the estimated patient SES effect, this would provide further evidence that performance differences between SNHs and non-SNHs are due to differences in patient casemix as opposed to systematic differences in quality between SNHs and non-SNHs. We included patients with missing race in sensitivity analyses. The results were similar and are not reported.
Finally, we performed a descriptive analysis to examine how likely patients are to be readmitted if they undergo surgery at high versus low-performance outlier hospitals. We identified outlier hospitals using the baseline hierarchical readmission model (without SES adjustment), and then examined the association between hospital performance and the risk of readmission using non-hierarchical logistic regression in which we specified hospital performance using indicator variables. All statistical analyses were performed using STATA SE/MP Version 13.2 (Stata Corp, College Station, Texas). The performance of non-hierarchical logistic regression models was assessed using measures of discrimination (C statistic) and calibration (Brier statistic).
Results
Patient Characteristics
The overall incidence of 30-day readmissions for patients undergoing major surgery was 6.9%, and was higher in SNHs compared to hospitals with the fewest low-SES patients, which we refer to as high-SES hospitals (hospitals with <21% of low-SES patients) (8.9% vs. 6.3%; P<0.001) (Table 1). As expected, patients admitted to SNHs were more likely to be Black (28.5% vs. 5.6%; P <0.001)) or Hispanic (14.5% vs.4.2%; P <0.001). Patients in high-SES and SNHs both had, on average, 2 comorbidities. However, patients in SNHs were more likely to have comorbid conditions that often lead to readmission, such as congestive heart failure (3.9% vs. 2.6%; P <0.001), diabetes (22.8% vs. 15.6%; P <0.001), or renal failure (6.8% vs. 4.9%; P<0.001).
Table 1. Patient characteristics.
| All Patients | Safety-net Hospitals (≥44% low-SES patients) | High-SES Hospitals (<21% low-SES patients) | |
|---|---|---|---|
|
|
|
|
|
| N = 129,247 | N = 13,540 | N = 48,721 | |
| Age (years) | 66 | 63 | 65 |
|
|
|
|
|
| Female | 48.3 | 46.5 | 48.9 |
|
|
|
|
|
| Race | |||
|
|
|
|
|
| White | 78.7 | 47.1 | 87.5 |
| Black | 10.6 | 28.5 | 5.6 |
| Other | 10.7 | 24.4 | 6.9 |
|
|
|
|
|
| Hispanic | 6.5 | 14.5 | 4.2 |
|
|
|
|
|
| Urgency | |||
|
|
|
|
|
| Elective | 72.9 | 51,4 | 78.8 |
| Urgent | 5.4 | 7.8 | 4.7 |
| emergency | 21.8 | 40.8 | 16.5 |
|
|
|
|
|
| Transfer status | |||
|
|
|
|
|
| Transfer from acute care hospital | 4.3 | 4.0 | 4.4 |
| Transfer in from other type of health facility | 0.5 | 1.1 | 0.3 |
|
|
|
|
|
| Admitted on weekend | 6.1 | 9.4 | 4.7 |
|
|
|
|
|
| Low-SES (Medicaid, Dual Eligible, or homeless) | 12.6 | 37.5 | 5.6 |
|
|
|
|
|
| Surgical Procedure | |||
|
|
|
|
|
| Hip replacement | 44.3 | 27.1 | 49.1 |
| Lobectomy | 6.7 | 5.6 | 7.0 |
| Endovascular AAA | 3.2 | 3.7 | 3.1 |
| Open AAA¥ | 0.8 | 0.9 | 0.8 |
| Colectomy | 29.3 | 42.8 | 25.6 |
| CABG | 15.7 | 20.0 | 14.4 |
|
|
|
|
|
| AHRQ Comorbidity Measures | |||
|
|
|
|
|
| Alcohol abuse | 1.5 | 2.5 | 1.2 |
| Deficiency anemia¥ | 11.9 | 11.4 | 12.0 |
| Rheumatoid arthritis/collagen vascular disease | 2.5 | 1.7 | 2.8 |
| Chronic blood loss anemia | 0.9 | 1.3 | 0.8 |
| Congestive heart failure | 2.9 | 3.9 | 2.6 |
| Chronic pulmonary disease¥ | 16.1 | 15.7 | 16.3 |
| Coagulopathy | 4.5 | 4.4 | 4.6 |
| Depression | 8.0 | 4.9 | 8.9 |
| Diabetes, uncomplicated | 17.2 | 22.8 | 15.6 |
| Diabetes with chronic complications¥ | 1.8 | 2.0 | 1.8 |
| Drug abuse | 0.9 | 1.9 | 0.6 |
| Hypertension | 58.2 | 60.1 | 57.6 |
| Hypothyroidism | 10.5 | 6.7 | 11.5 |
| Liver disease | 1.3 | 1.5 | 1.2 |
| Lymphoma | 0.5 | 0.4 | 0.6 |
| Fluid and electrolyte disorders | 16.6 | 15.2 | 17.0 |
| Metastatic cancer | 6.4 | 7.1 | 6.2 |
| Other neurological disorders | 3.3 | 3.6 | 3.2 |
| Obesity | 10.3 | 7.8 | 11.0 |
| Paralysis | 0.8 | 1.6 | 0.6 |
| Peripheral vascular disorder | 5.7 | 5.2 | 5.8 |
| Psychoses | 1.5 | 2.1 | 1.3 |
| Pulmonary circulation disorder¥ | 1.3 | 1.3 | 1.2 |
| Renal failure | 5.3 | 6.8 | 4.9 |
| Solid tumor without metastasis | 1.6 | 2.1 | 1.4 |
| Peptic ulcer disease | 0.04 | 0.1 | 0.003 |
| Valvular disease | 4.4 | 1.8 | 5.1 |
| Weight loss | 2.6 | 4.3 | 2.2 |
|
|
|
|
|
| Number of comorbidities¥ | 2 | 2 | 2 |
|
|
|
|
|
| 30-day readmission | 6.9 | 8.9 | 6.3 |
All numbers are percentages unless otherwise stated.
All differences between low-SES and high-SES hospitals are significant (P <0.05) unless indicated (¥).
Hospital SES percentage used to define low-SES hospitals and high-SES hospitals is based on all inpatient admissions.
Hospital Ranking With versus Without SES Adjustment
Patients undergoing surgery at low-performance hospitals were nearly twice as likely to be readmitted within 30-days (adjusted 30-day readmission rate 9.29%: 95% CI, 8.62-9.96) compared to patients admitted to high-performance hospitals (5.26%; 95% CI: 4.36- 6.16%). Figure 1 demonstrates the level of agreement between hospital AOR with and without SES adjustment. The intraclass correlation coefficient of 0.994 (95% CI, 0.991-0.997) indicates near-perfect agreement between the two metrics with and without SES adjustment. Kappa analysis revealed that these two models displayed excellent agreement on which hospitals were categorized as low-, intermediate, and high-performance hospitals: kappa of 0.96. We did determine, however, that in the absence of SES risk adjustment, SNHs are more likely to be penalized using the CMS HRRP threshold approach (Appendix 2). Without SES adjustment, 61% of the SNH hospitals were found to have greater-than-predicted admissions. With SES adjustment, roughly half (51%) of the SNHs were assigned to the penalty group, a similar proportion to that observed among non-SNHs.
Figure 1.
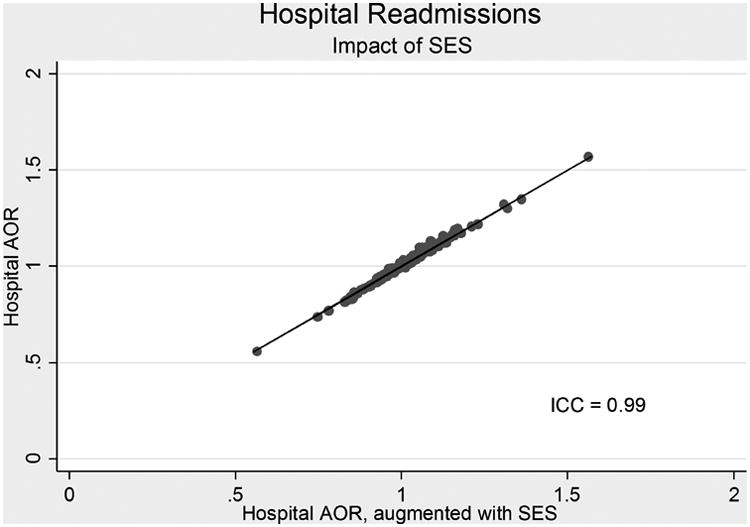
Impact of including SES in risk adjustment model for 30-day readmission. The hospital AOR represents the likelihood that patients undergoing major surgery at a specific hospital are likely to be readmitted within 30-days compared to patients undergoing major surgery at the “average” hospital, after adjusting for patient casemix. The identity line represents perfect agreement.
SNHs versus non-SNHs
Without risk adjustment, patients undergoing one of the six surgical procedures in SNHs were 44% more likely to be readmitted compared to patients in high-SES hospitals (odds ratio [OR] 1.44; 95% confidence interval [CI]: 1.05-1.97; P= 0.023) (Table 2). With risk adjustment, patients in SNHs were 14% more likely to be readmitted compared to patients in high-SES hospitals (adjusted odds ratio [AOR] 1.14; 95% CI: 1.00-1.31; P= 0.044). After adjusting for patient risk factors and patient SES, patients admitted to SNHs were not significantly more likely to be readmitted compared to patients in high-SES hospitals (AOR 1.08; 95% CI: 0.95-1.23; P = 0.23). (Table 2) These findings suggest that differences in patient case mix, including patient SES, may account for the higher readmission rates in SNHs, as opposed to systematic differences in hospital performance.
Table 2.
Influence of Hospital Concentration of Low-SES patients on 30-day Readmission Rates.
| Unadjusted | Patient Characteristics | Patient Characteristics + SES | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| crude OR (95%CI) | P | AOR (95%CI) | P | AOR (95% CI) | P | |
|
|
|
|
||||
| Hospital proportion of Low-SES patients | ||||||
|
|
|
|
||||
| Lowest | Reference | Reference | Reference | |||
| Low | 1.20 (0.88-1.63) | 0.26 | 1.02 (0.89-1.16) | 0.81 | 1.01 (0.88-1.15) | 0.87 |
| Middle | 1.35 (1.00-1.84) | 0.05 | 1.10 (0.97-1.24) | 0.13 | 1.08 (0.96-1.22) | 0.20 |
| High | 1.44 (1.05-1.97) | 0.023 | 1.14 (1.00-1.31) | 0.044 | 1.08 (0.95-1.23) | 0.23 |
Results are based on regression analysis (see text).
AOR – adjusted odds ratio; OR – odds ratio; CI – confidence interval
Before adjusting for patient risk, low-SES patients were 44% more likely to be readmitted within 30-days (unadjusted OR 1.44; 95% CI: 1.27-1.64; P<0.001) (Table 3). After adjusting for patient risk, low-SES patients were still more likely to be readmitted (AOR 1.24; 95% CI: 1.16-1.33; P <0.001), but the magnitude of the difference was less. After adjusting for patient risk and hospital fixed effects, the likelihood of readmission was nearly the same (AOR1.20; 95% CI: 1.12-1.28; P<0.001). Figure 2 displays the adjusted 30-day readmission rates as a function of the hospital strata based on the proportion of low-SES patients. This figure visually confirms the finding that SNHs performance is not different than the performance of non-SNHs. Collectively, these findings suggest that the higher risk of readmission in SNHs is due to differences in the proportion of low-SES patients between SNHs and non-SNHs, as opposed to quality differences between SNHs and non-SNHs.
Table 3.
Influence of Patient SES on 30-day Readmission Rates.
| Unadjusted | Patient Characteristics | Patient Characteristics + Hospital Effect | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Crude OR (95%CI) | P | AOR (95%CI) | P | AOR (95% CI) | P | |
|
|
|
|
||||
| Low-SES | 1.44 (1.27-1/64) | <0.001 | 1.24 (1.16-1.33) | <0.001 | 1.20 (1.12-1.28) | <0.001 |
|
|
|
|
||||
Results are based on regression analysis (see text for description).
AOR – adjusted odds ratio; CI – confidence interval
Figure 2.
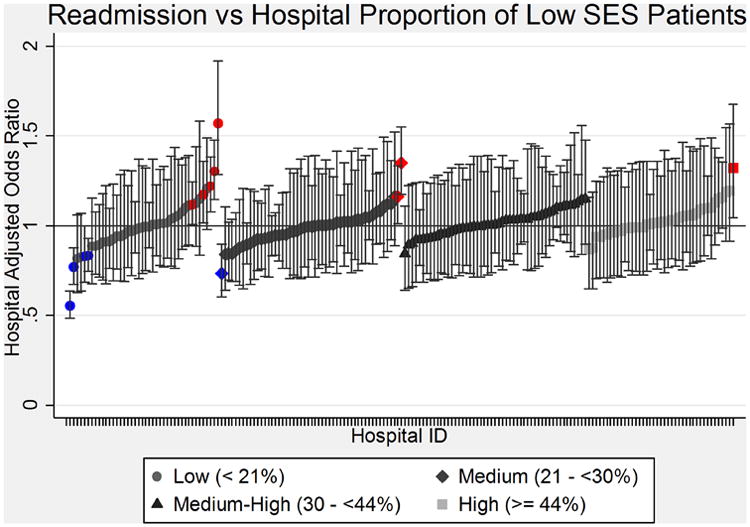
Hospital 30-day readmission rates as a function of the hospital proportion of low- SES patients. Each hospital is represented by a separate point. Error bars represent 95% confidence intervals.
Model performance is described in the Appendix. Both models displayed acceptable discrimination, as measured by the C statistic: 0.66. The C statistics for our models are consistent with the published literature for readmission risk adjustment models.23 Model calibration, quantified using the Brier score, was excellent for both models.
Discussion
Compared to hospitals caring for fewer low-SES patients, safety-net hospitals are slightly more likely to readmit patients after major surgery. However, after adjusting for patient SES, readmission rates at SNHs are not significantly higher than those of non-SNHs. This suggests that the performance of SNHs with surgical readmissions is no worse than that of hospitals that care for few low-SES patients. Interestingly, including SES in risk adjustment had almost no influence on a hospital's ranking. However, because the CMS HRRP penalizes any hospital that has readmissions in excess of the predicted number of readmissions, SNHs are more likely to be penalized under the HRRP approach than non-SNHs. If CMS were to implement SES adjustment, it would level the playing field, and penalize SNHs and non-SNHs at roughly equal rates.
Previous studies have reported that low-SES patients are more likely to be readmitted.17, 18, 24, 25 Other studies found that, under the HRRP, safety-net hospitals are more likely to be penalized for excessive readmissions than non-SNHs.18, 26 However, when the effects of SES adjustment on hospital ranking were examined, the impact on ranking was negligible.25, 27 The reason for the apparent discrepancy between the effects of SES adjustment on a hospital's performance in the HRRP versus its impact on conventional hospital profiling is because the HRRP does not use typical statistical criteria to determine whether a hospital's observed readmission rate is significantly greater than its predicted readmission rates. Instead, HRRP applies a threshold that is extremely sensitive to small changes in the rate of readmission. In comparison, Hospital Compare uses a Bayesian approach for quality reporting, which is very conservative way to identify quality outliers. Unlike prior studies, ours is the first to report the impact of SES adjustment on surgical patients. We are also the first group to identify differences in the effects of SES adjustment on hospital ranking depending on which approach is used by CMS: Hospital Compare versus the HRRP.
It is not surprising that risk-adjusting for SES had little impact on risk-adjusted hospital readmission rates. Since the seminal work by Iezonni titled the “Risk of Risk Adjustment,”28 it has been recognized that the choice of risk adjustment model can strongly influence a hospital's quality ranking 29 if the risk factors included in competing risk-adjustment models are quite different. But, SES-enhanced models add only a small number of SES predictors, while leaving the rest of the model unchanged. And, as we and others have shown, low-SES is only modestly associated with an increased risk of readmission.17, 18, 24, 25 There are other examples in the literature where model enhancements did not have a substantial impact on hospital ranking.30 For example, enhancing a claims-based model using a small number of clinical data elements did not have a significant impact of on hospital ranking for readmission after heart failure.31
Our study has several potential limitations. First, our use of administrative data may have limited our ability to appropriately adjust for patient casemix. However, if one assumes that low-SES patients tend to be sicker, then low-SES will be a proxy for severity-of-disease, and the lack of comprehensive clinical data will amplify the impact of not adjusting for SES on hospital profiling. Since we found that SES adjustment has no effect on hospital quality ranking, use of administrative data is not a significant limitation in our analysis. Furthermore, from a practical standpoint, CMS uses administrative and not clinical data in Hospital Compare and the HRRP. Second, because our analysis is limited to New York State, it may not be generalizable to the rest of the U.S. However, our findings are similar to those reported for medical patients using national data, making generalizability less of a concern. Third, our definition of low-SES may not capture the full spectrum of factors, such as limited education and lack of social support, that increase a patient's risk of readmission. If additional SES information becomes routinely available in national data sets, it will enable more precise SES specification for risk adjustment.
The decision to adjust readmission measures for SES has potentially important policy implications. On the one hand, not adjusting SES may unfairly disadvantage SNHs – and deprive them of the financial resources necessary to care for vulnerable patient populations.18, 26 On the other hand, adjusting for SES may disincentives hospitals from targeting low-SES patients with programs specifically designed for low-SES patients to reduce the likelihood of hospital readmissions. We are not aware of any data showing that penalties imposed on SNHs have resulted in worse outcomes. However, since the Hospital Readmission Reduction Program was initiated in October 2012, and because of the lag in the availability of large databases for research, it may take some time before such results become available. We also expect that there are examples of SNHs that have succeeded in successfully lowering readmission rates. But we also believe, that on average, penalizing SNHs will lead to worse outcomes for patients in healthcare systems that are already financially stressed to care for low-income and vulnerable patients.
Conclusion
Differences in surgery readmission rates between SNHs and non-SNHs are due to differences in patient case mix of low-SES patients, and not to differences in hospital quality. This finding does not support the CMS position that adjusting for SES would mask poor quality care. Adjusting readmission measures for SES leads to changes in hospital ranking using the HRRP threshold approach, but not using the CMS Hospital Compare methodology. The HRRP threshold approach, which is used by CMS in value-based purchasing, does not account for differences in SES, and is more likely to penalize SNHs than non-SNHs. Because the HRRP unduly penalizes hospitals that serve the greatest numbers of vulnerable patients, it may unintentionally hurt the poorest patients by taking resources away from SNHs, and encourage hospitals with more resources to avoid poor patients. However, if the HRRP approach were to adjust for SES, SNHs and non-SNHs would be equally likely to be penalized. CMS should consider either adjusting for the effects of SES when calculating readmission thresholds for HRRP, or replace it with the approach used in Hospital Compare.
Acknowledgments
This project was supported with funding from the Department of Anesthesiology at the University of Rochester School of Medicine and by the National Institute On Minority Health And Health Disparities of the National Institutes of Health under Award Number R01MD006231. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the Uniformed Services University of the Health Sciences, or those of the Department of Defense.
Appendix 1
30-day Readmission models.
| Risk Factors | Baseline Model | Baseline Model + SES | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| AOR | 95% CI | P | AOR | 95% CI | P | |
| Age (years) | 1.009 | 1.007-1.011 | <0.001 | 1.01 | 1.008-1.013 | <0.001 |
|
|
|
|
||||
| Female | 0.98 | 0.93-1.03 | 0.47 | 0.97 | 0.93-1.02 | 0.30 |
|
|
|
|
||||
| Urgency | ||||||
|
|
|
|
||||
| Elective | ref | ref | ||||
| Urgent | 1.20 | 1.09-1.32 | <0.001 | 1.19 | 1.09-1.32 | <0.001 |
| emergency | 1.39 | 1.28-1.50 | <0.001 | 1.36 | 1.26-1.47 | <0.001 |
|
|
|
|
||||
| Transfer status | ||||||
|
|
|
|
||||
| Transfer from acute care hospital | 1.07 | 0.99-1.15 | 0.093 | 1.06 | 0.98-1.14 | 0.13 |
| Transfer in from other type of health facility | 1.17 | 0.96-1.44 | 0.12 | 1.14 | 0.93-1.39 | 0.22 |
|
|
|
|
||||
| Admitted on weekend | 1.06 | 0.99-1.13 | 0.10 | 1.06 | 0.99-1.13 | 0.11 |
|
|
|
|
||||
| Low-SES (Medicaid, Dual Eligible, or homeless) | NA | 1.24 | 1.16-1.33 | <0.001 | ||
|
|
|
|
||||
| Surgical Procedure | ||||||
|
|
|
|
||||
| Hip replacement | ref | ref | ||||
| Lobectomy | 1.95 | 1.63-2.33 | <0.001 | 1.93 | 1.62-2.30 | <0.001 |
| Endovascular AAA | 2.11 | 1.72-2.58 | <0.001 | 2.09 | 1.72-2.55 | <0.001 |
| Open AAA | 2.24 | 1.74-2.88 | <0.001 | 2.24 | 1.74-2.87 | <0.001 |
| Colectomy | 2.27 | 1.91-2.70 | <0.001 | 2.26 | 1.91-2.67 | <0.001 |
| CABG | 2.20 | 1.83-2.64 | <0.001 | 2.18 | 1.82-2.61 | <0.001 |
|
|
|
|
||||
| AHRQ Comorbidity Measures | ||||||
|
|
|
|
||||
| Alcohol abuse | 1.00 | 0.85-1.17 | 0.99 | 0.99 | 0.84-1.16 | 0.88 |
| Deficiency anemia | 1.07 | 1.01-1.13 | 0.012 | 1.06 | 1.01-1.12 | 0.021 |
| Rheumatoid arthritis/collagen vascular disease | 1.10 | 0.97-1.26 | 0.15 | 1.11 | 0.97-1.26 | 0.13 |
| Chronic blood loss anemia | 0.91 | 0.77-1.09 | 0.30 | 0.91 | 0.76-1.09 | 0.30 |
| Congestive heart failure | 1.47 | 1.33-1.62 | <0.001 | 1.46 | 1.32-1.61 | <0.001 |
| Chronic pulmonary disease | 1.20 | 1.14-1.26 | <0.001 | 1.19 | 1.14-1.25 | <0.001 |
| Coagulopathy | 1.13 | 1.02-1.25 | 0.023 | 1.13 | 1.02-1.25 | 0.020 |
| Depression | 1.12 | 1.03-1.22 | 0.006 | 1.12 | 1.03-1.22 | 0.006 |
| Diabetes, uncomplicated | 1.13 | 1.07-1.19 | <0.001 | 1.12 | 1.06-1.18 | <0.001 |
| Diabetes with chronic complications | 1.18 | 1.05-1.33 | 0.006 | 1.17 | 1.04-1.31 | 0.011 |
| Drug abuse | 1.04 | 0.84-1.29 | 0.71 | 0.99 | 0.80-1.23 | 0.94 |
| Hypertension | 0.97 | 0.92-1.03 | 0.33 | 0.97 | 0.92-1.02 | 0.24 |
| Hypothyroidism | 1.01 | 0.94-1.08 | 0.83 | 1.01 | 0.95-1.09 | 0.69 |
| Liver disease | 1.06 | 0.87-1.20 | 0.56 | 1.05 | 0.86-1.27 | 0.66 |
| Lymphoma | 1.25 | 0.99-1.57 | 0.06 | 1.26 | 1.00-1.58 | 0.05 |
| Fluid and electrolyte disorders | 1.18 | 1.11-1.26 | <0.001 | 1.18 | 1.11-1.25 | <0.001 |
| Metastatic cancer | 1.14 | 1.03-1.26 | 0.009 | 1.14 | 1.03-1.26 | 0.012 |
| Other neurological disorders | 1.09 | 0.97-1.23 | 0.13 | 1.07 | 0.96-1.22 | 0.19 |
| Obesity | 1.16 | 1.09-1.25 | <0.001 | 1.17 | 1.09-1.26 | <0.001 |
| Paralysis | 1.19 | 0.97-1.45 | 0.09 | 1.16 | 0.95-1.41 | 0.15 |
| Peripheral vascular disorder | 1.20 | 1.12-1.30 | <0.001 | 1.20 | 1.12-1.30 | <0.001 |
| Psychoses | 1.23 | 1.06-1.43 | 0.007 | 1.18 | 1.02-1.38 | 0.03 |
| Pulmonary circulation disorder | 1.39 | 1.19-1.62 | <0.001 | 1.39 | 1.19-1.62 | <0.001 |
| Renal failure | 1.27 | 1.18-1.36 | <0.001 | 1.26 | 1.17-1.35 | <0.001 |
| Solid tumor without metastasis | 1.28 | 1.12-1.46 | <0.001 | 1.28 | 1.11-1.46 | <0.001 |
| Peptic ulcer disease | 0.61 | 0.17-2.14 | 0.44 | 0.61 | 0.18-2.14 | 0.44 |
| Valvular disease | 0.99 | 0.87-1.12 | 0.87 | 1.00 | 0.88-1.13 | 0.96 |
| Weight loss | 1.30 | 1.19-1.43 | <0.001 | 1.29 | 1.18-1.42 | <0.001 |
|
|
|
|
||||
| C statistic | 0.66 | 0.66 | ||||
|
|
|
|
||||
| Brier score | 0.067 | 0.067 | ||||
|
|
|
|
||||
Abbreviations: ref – reference; NA – not applicable
Appendix 2
Hospitals with higher-than-predicted readmission rates as a function of SES adjustment.
| SNH No. (%) | Non-SNH No. (%) | |
|---|---|---|
| Base Model | ||
|
| ||
| Penalty group | 25 (61) | 72 (50) |
| No penalty | 16 (39) | 72 (50) |
|
| ||
| Base Model + SES | ||
|
| ||
| Penalty group | 21 (51) | 71 (49) |
| No penalty | 20 (49) | 73 (51) |
No. – number of hospitals; SES – socioeconomic status; SNH - safety-net hospital
References
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2.Epstein AM, Jha AK, Orav EJ. The relationship between hospital admission rates and rehospitalizations. N Engl J Med. 2011;365(24):2287–95. doi: 10.1056/NEJMsa1101942. [DOI] [PubMed] [Google Scholar]
- 3.CfMM, editor. Services. 2014. Readmissions Reduction Program. [Google Scholar]
- 4.Burwell S. Interim update on 2013 annual hospital-acquired condition rate and estimates of cost savings and deaths averted from 2010 to 2013. In: HaH, editor. Services. 2014. [Google Scholar]
- 5.UDoHaH, editor. Services. 2014. New HHS Data Shows Major STrides Made in Patient Safety, leading to Improved Care and Savings. [Google Scholar]
- 6.Calvillo-King L, Arnold D, Eubank KJ, et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J Gen Intern Med. 2013;28(2):269–82. doi: 10.1007/s11606-012-2235-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Risk Adjustment for Socioeconomic Status or Other Sociodemographic Factors. National Quality Forum. 2014 [Google Scholar]
- 8.Lipstein SH, Dunagan WC. The risks of not adjusting performance measures for sociodemographic factors. Annals of Internal Medicine. 2014;161(8):594–6. doi: 10.7326/M14-1601. [DOI] [PubMed] [Google Scholar]
- 9.Tsai TC, Joynt KE, Orav EJ, et al. Variation in surgical-readmission rates and quality of hospital care. N Engl J Med. 2013;369(12):1134–42. doi: 10.1056/NEJMsa1303118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glance LG, Kellermann AL, Osler TM, et al. Hospital readmission after noncardiac surgery: the role of major complications. JAMA Surg. 2014;149(5):439–45. doi: 10.1001/jamasurg.2014.4. [DOI] [PubMed] [Google Scholar]
- 11.Krumholz HM, Lin Z, Keenan PS, et al. Relationship between hospital readmission and mortality rates for patients hospitalized with acute myocardial infarction, heart failure, or pneumonia. JAMA. 2013;309(6):587–93. doi: 10.1001/jama.2013.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Introduction to the HCUP State Inpatient Databases (SID) [Accessed 9/17/2014];Journal. 2013 serial online. Available from: Agency for Healthcare Research and Quality Rockville, Maryland. [Google Scholar]
- 13.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 14.HCUP Supplemental Variables for Revisit Analysis. Agency for Healthcare Research and Quality; 2014. [Google Scholar]
- 15.Werner RM, Goldman LE, Dudley RA. Comparison of change in quality of care between safety-net and non-safety-net hospitals. JAMA. 2008;299(18):2180–7. doi: 10.1001/jama.299.18.2180. [DOI] [PubMed] [Google Scholar]
- 16.CMS, editor. Fact sheets - CMS to Improve Quality of Care durding Hospital Inpatient Stays. Baltimore, MD: 2014. [Google Scholar]
- 17.Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305(7):675–81. doi: 10.1001/jama.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gu Q, Koenig L, Faerberg J, et al. The Medicare Hospital Readmissions Reduction Program: potential unintended consequences for hospitals serving vulnerable populations. Health Serv Res. 2014;49(3):818–37. doi: 10.1111/1475-6773.12150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharabiani MT, Aylin P, Bottle A. Systematic review of comorbidity indices for administrative data. Med Care. 2012;50(12):1109–18. doi: 10.1097/MLR.0b013e31825f64d0. [DOI] [PubMed] [Google Scholar]
- 20.DeLong ER, Peterson ED, DeLong DM, et al. Comparing risk-adjustment methods for provider profiling. Stat Med. 1997;16(23):2645–2664. doi: 10.1002/(sici)1097-0258(19971215)16:23<2645::aid-sim696>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 21.Wakeam E, Hevelone ND, Maine R, et al. Failure to rescue in safety-net hospitals: availability of hospital resources and differences in performance. JAMA Surg. 2014;149(3):229–35. doi: 10.1001/jamasurg.2013.3566. [DOI] [PubMed] [Google Scholar]
- 22.Ross JS, Bernheim SM, Lin Z, et al. Based on key measures, care quality for Medicare enrollees at safety-net and non-safety-net hospitals was almost equal. Health Aff (Millwood) 2012;31(8):1739–48. doi: 10.1377/hlthaff.2011.1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306(15):1688–98. doi: 10.1001/jama.2011.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hu J, Gonsahn MD, Nerenz DR. Socioeconomic status and readmissions: evidence from an urban teaching hospital. Health Aff (Millwood) 2014;33(5):778–85. doi: 10.1377/hlthaff.2013.0816. [DOI] [PubMed] [Google Scholar]
- 25.Blum AB, Egorova NN, Sosunov EA, et al. Impact of socioeconomic status measures on hospital profiling in New York City. Circ Cardiovasc Qual Outcomes. 2014;7(3):391–7. doi: 10.1161/CIRCOUTCOMES.113.000520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA. 2013;309(4):342–3. doi: 10.1001/jama.2012.94856. [DOI] [PubMed] [Google Scholar]
- 27.Keyhani S, Myers LJ, Cheng E, et al. Effect of clinical and social risk factors on hospital profiling for stroke readmission: a cohort study. Annals of Internal Medicine. 2014;161(11):775–84. doi: 10.7326/M14-0361. [DOI] [PubMed] [Google Scholar]
- 28.Iezzoni LI. The risks of risk adjustment. JAMA. 1997;278(19):1600–7. doi: 10.1001/jama.278.19.1600. [DOI] [PubMed] [Google Scholar]
- 29.Shahian DM, Wolf RE, Iezzoni LI, et al. Variability in the measurement of hospital-wide mortality rates. N Engl J Med. 2010;363(26):2530–9. doi: 10.1056/NEJMsa1006396. [DOI] [PubMed] [Google Scholar]
- 30.Glance LG, Dick AW, Mukamel DB, et al. The effect of preexisting conditions on hospital quality measurement for injured patients. Ann Surg. 2010;251(4):728–734. doi: 10.1097/SLA.0b013e3181d56770. [DOI] [PubMed] [Google Scholar]
- 31.Hammill BG, Curtis LH, Fonarow GC, et al. Incremental value of clinical data beyond claims data in predicting 30-day outcomes after heart failure hospitalization. Circ Cardiovasc Qual Outcomes. 2011;4(1):60–7. doi: 10.1161/CIRCOUTCOMES.110.954693. [DOI] [PubMed] [Google Scholar]


