Abstract
Objective:
Although mechanical ventilation is frequently a life-saving therapy, its use can result in unwanted side effects. It has been well documented that the choice of sedating agent may influence the duration of mechanical ventilation. Melatonin is a sedative and analgesic agent without any respiratory depressant effect which makes it an attractive adjuvant for sedation in the intubated patients. The aim of this study is to evaluate the effect of melatonin on the duration of mechanical ventilation in patients with hemorrhagic stroke.
Methods:
Forty adult intubated patients with hemorrhagic stroke, who were admitted to the Intensive Care Unit (ICU) within 24 h of onset, were enrolled in this randomized double-blind study. Subjects in the melatonin group received 30 mg of melatonin every night throughout the nasogastric tube. Length of ICU stay, mortality, and duration of mechanical ventilation were recorded for all patients.
Findings:
The duration of mechanical ventilation and length of ICU stay were shorter in patients who received melatonin in comparison with the control group, and this difference was statistically significant for the length of ICU stay and marginally significant for the duration of mechanical ventilation. Although not statistically significant, the mortality rate of the control group was 30%, almost double that of the study group (15%).
Conclusion:
Melatonin possesses hypnotic, analgesic, anti-inflammatory, and anti-oxidative properties that distinguish it as an attractive adjuvant in patients under mechanical ventilation. In conclusion, the administration of melatonin may facilitate the weaning process through decreasing the consumption of sedatives with respiratory depressant properties as well as preventing ventilator-associated lung injury.
KEYWORDS: Hemorrhagic stroke, mechanical ventilation, Melatonin
INTRODUCTION
Spontaneous, nontraumatic intracerebral hemorrhage (ICH) is the second most common cause of stroke following ischemic stroke, which can cause 35%–50% 30-day mortality. Evidence has shown that most patients present with small ICHs, can survive with a good medical care.[1,2] This suggests that an appropriate medical interventions may improve the outcome of these patients.[3] The current data have shown that early initiation of neuroprotective treatment might protect threatened neurons and improve outcome in hemorrhagic stroke.[4] Melatonin is a neurohormone which has generated a great deal of interest as a therapeutic modality for various neurological diseases because of its low toxicity, antioxidative, antiapoptotic, and anti-inflammatory properties. In addition, it has some exclusive properties that are highly desirable in the Intensive Care Unit (ICU).[5,6]
The aim of this study is to evaluate the effect of exogenous melatonin as an adjuvant on the duration of mechanical ventilation, length of ICU stay, and mortality in intubated patients with hemorrhagic stroke.
METHODS
This study was registered as a clinical trial in IRCT (www.irct.ir) with an allocated number of IRCT2016100530164N1. Forty adult patients with acute, spontaneous ICH, confirmed by cranial computed tomography (CT), who were admitted to the ICU within 24 h of onset, were enrolled in this randomized double-blind study.
Exclusion criteria included evidence of traumatic ICH, contraindications to receiving oral medication, brain tumor, Glasgow coma scale (GCS) score of 8 or more, underlying respiratory disease, renal impairment (estimated glomerular filtration rate <60 ml/min), and pregnancy or breastfeeding.
A full written informed consent was obtained from a legal surrogate, this was because the patients lacked capacity due to being dysphasic or confused. The study protocol was approved by the Ethics Committee for Human Research at Tehran University of Medical Sciences. Patients were allocated to each group using permuted-block randomization method. Subjects in the melatonin group received 30 mg of melatonin (Melatonin, Webber naturals, Canada) every night throughout the nasogastric tube. A sedation and analgesic strategy, using opioid plus benzodiazepine, was chosen as a protocol for all intubated patients. Sedative and analgesic medications were titrated to maintain a light level of sedation according to the Richmond Agitation–Sedation Scale. Risk factors and demographic and clinical characteristics were recorded at the time of enrollment. Length of ICU stay, mortality, and duration of mechanical ventilation were assessed for all patients.
Continuous variables were presented as mean with standard deviation and median with interquartile range boundaries when the data were not normally distributed. Continuous variables were compared between groups using Student's t-test or Mann–Whitney U-test. Categorical variables were expressed through frequency in percentage and were compared between two groups using Chi-square test. P ≤ 0.05 was considered statistically significant. IBM SPSS Statistics for Windows, Version 20.0 (IBM Corp., Armonk, NY, USA) was applied to conduct the analyses [Figure 1].
Figure 1.
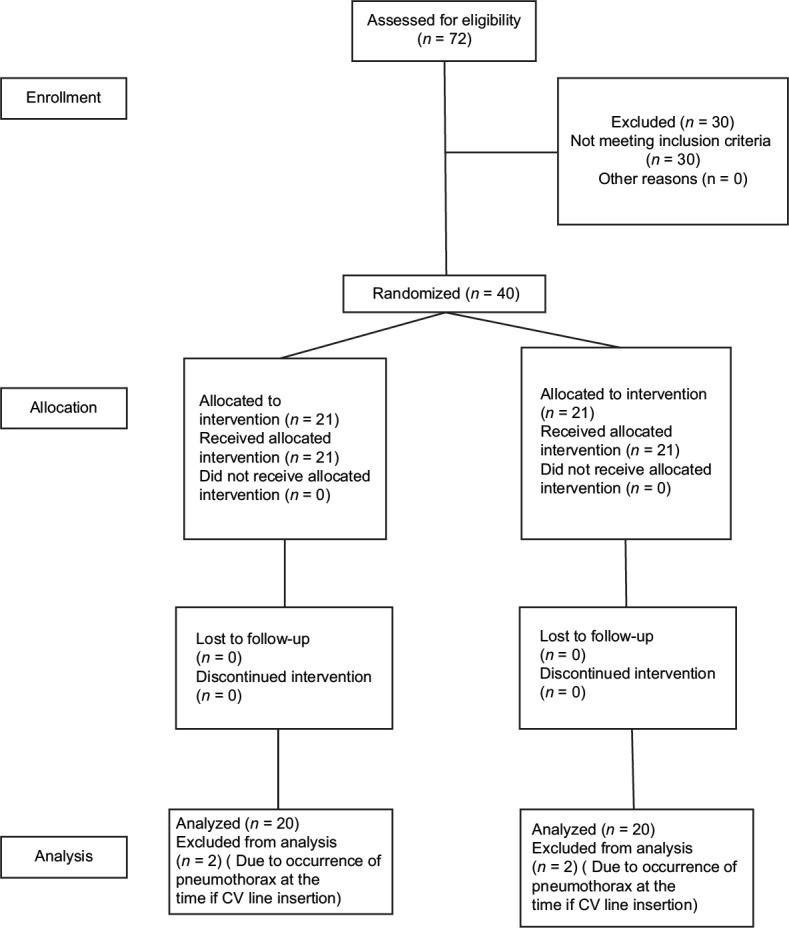
CONSORT flow chart
RESULTS
From 72 ICH patients, 42 patients who met the inclusion criteria were enrolled in our study. Of this total, 2 patients were excluded from the trial due to the occurrence of pneumothorax after central venus (CV) line insertion. Therefore, the statistical analysis was performed on 40 patients: 20 (50%) subjects in the melatonin group and 20 (50%) as a control group [Figure 1].
There was no significant difference in the baseline characteristics of the included patients except for body mass index [Table 1].
Table 1.
Demographic data and clinical characteristics of the study groups
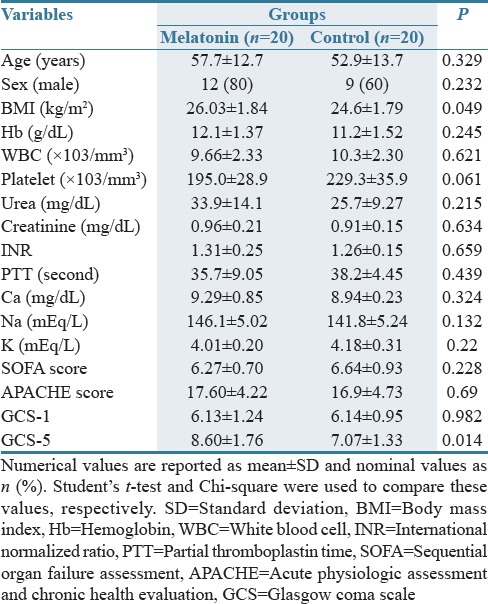
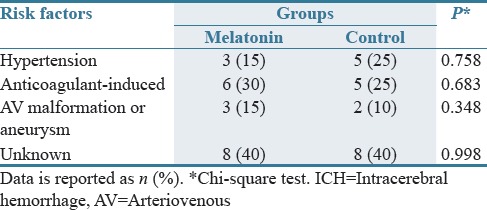
At day 5, GCS score was improved in both groups, but this improvement was more significant for the melatonin group compare with control one [Table 1]. There were no differences between groups regarding the risk factor of ICH [Table 2].
Table 2.
Comparison of the risk factors for intracerebral hemorrhage in two study groups (N=20 in each group)
The duration of mechanical ventilation and length of ICU stay were shorter in patients who received melatonin in comparison with the control group, and this difference was statistically significant for the length of ICU stay and marginally significant for the duration of mechanical ventilation (P = 0.065) [Table 3].
Table 3.
Comparison of duration of mechanical ventilation, length of Intensive Care Unit stay, and in.Intensive Care Unit mortality rate, in two study groups (N=20 in each group)
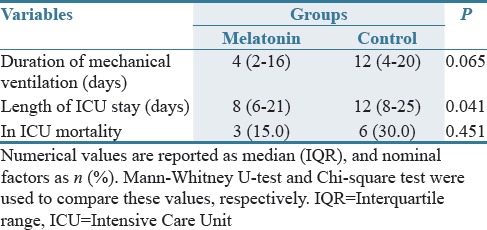
Although not statistically significant, the mortality rate of the control group was 30%, almost double that of the study group (15%) [Table 3].
DISCUSSION
Melatonin is a neurohormone originated from the amino acid, tryptophan, and is mainly secreted by the pineal gland into the blood stream.[7] The efficacy and safety of exogenous melatonin for the treatment of insomnia have been confirmed in a meta-analysis.[8] This hormone has generated a great deal of interest as a therapeutic modality for various targets in the ICU.[9] Thanks to its antioxidant activity, melatonin has shown protective effects against oxidative injury in different in vitro and in vivo models of neurodegenerative diseases, not only by neutralizing free radicals but also by upregulating antioxidant and downregulating pro-oxidative and proinflammatory enzymes.[10,11,12] Efficacy of melatonin on animal models of stroke has been demonstrated in a meta-analysis.[13] Available clinical data have shown that melatonin is as effective as benzodiazepines in reducing anxiety without inducing any cognitive impairment or adverse effect on psychomotor performance. Moreover, unlike the conventional sedative agents, this hormone does not worsen nocturnal hypoxemia or ventilator responses.[7,14,15] In addition, it has been shown that melatonin is able to treat and prevent the ICU delirium.[16,17]
All of the patients with hemorrhagic stroke and low degrees of consciousness need to be mechanically ventilated. Although mechanical ventilation is frequently a life-saving therapy, its use can result in unwanted side effects, including ventilator associated lung injury, ventilator associated pneumonia, sinusitis, gastrointestinal bleeding, and venous thromboembolism.[18,19,20] Moreover, investigations have shown that the duration of mechanical ventilation is associated with short and long term mortality.[21]
It has been well documented that the choice of sedating agent may influence the duration of mechanical ventilation. Benzodiazepines and opiates are the most commonly used agents for sedation and analgesia in the ICU. Both of these agents possess some respiratory depressant effect, which can cause the duration of mechanical ventilation to be prolonged.[22,23,24]
Melatonin is a neuroprotective agent with sedative, hypnotic, and analgesic properties without any respiratory depressant effect which makes it an attractive adjuvant for sedation in the ICU.[7,9]
As shown in Table 2, the duration of mechanical ventilation was shorter in patients who received melatonin in comparison with the control group. According to the literature, it can be hypothesized that the administration of melatonin as an adjuvant with hypnotic properties may have reduced the amount of sedative agents and related adverse effects, including respiratory depression and delirium, which are both risk factors of prolonged weaning. On the other hand, as shown in Table 1, the level of consciousness was raised in melatonin group in comparison with the control one, which can be attributed to the neuroprotective effect of melatonin on stroke.
In a study which was conducted by Frisk et al., a decreased melatonin secretion was observed during mechanical ventilation.[25] Dessap et al. investigate the relationship between plasma melatonin levels and successful weaning from mechanical ventilation. They concluded that the lower plasma melatonin levels were associated with unsuccessful and prolonged weaning.[26] In an investigation which was operated by Mistraletti et al., administration of melatonin as a supplement in critically ill patients was associated with a decrease in the consumption of sedative agents, shortening the duration of mechanical ventilation, improved neurological indicators, and cost reduction.[27]
In addition to the studies mentioned above, it has long been known that one of the complications of mechanical ventilation is ventilator-associated lung injury, which is believed to be caused by free radicals.[28,29] With regard to the extraordinary high antioxidant effect of melatonin, it has been hypothesized that administration of melatonin may be protective against this kind of injury.[30,31,32] Gitto et al. showed that the administration of melatonin in mechanically ventilated newborns reduced the proinflammatory cytokines and improved the clinical outcome.[29]
Melatonin possesses hypnotic, analgesic, anticonvulsive, anti-inflammatory, and anti-oxidative properties that distinguish it as a novel and an attractive adjuvant in patients under mechanical ventilation.[8,9,33] Its sedative and analgesic properties may help patients better tolerate the mechanical ventilation.[8]
Our study encountered some limitations. In this study, the cumulative dose of sedative and analgesic agents were not measured to see to what extent the administration of melatonin could decrease the dose of these agents. In addition, there was no placebo group in this study, which may adversely affect the results and can be mentioned as a limitation of the study. Although it was not statistically meaningful, our study showed that the administration of melatonin may decrease the duration of mechanical ventilation. This observation is too weak to be considered reliable. However, they deserve to be considered as hypotheses-generating observations.
The administration of melatonin may facilitate the weaning process through decreasing the consumption of sedatives with respiratory depressant properties as well as preventing ventilator-associated lung injury.
AUTHORS' CONTRIBUTION
Mehrnoush Dianatkhah contributed in concept, study design, definition of intellectual content, literature search, clinical studies, experimental studies, data acquisition, data analysis, statistical analysis, manuscript preparation, manuscript editing and manuscript review. Atabak Najafi and Arezoo Ahmadi contributed in concept and study design. Mohammad Sharifzadeh participated in clinical and experimental studies. Hamidreza Sharifnia and Mojtaba Mojtahedzadeh have done the manuscript editing and manuscript review. Farhad Najmeddin contributed in data analysis. Azadeh Moghaddas has prepared and edited the manuscript.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Sacco S, Marini C, Toni D, Olivieri L, Carolei A. Incidence and 10-year survival of intracerebral hemorrhage in a population-based registry. Stroke. 2009;40:394–9. doi: 10.1161/STROKEAHA.108.523209. [DOI] [PubMed] [Google Scholar]
- 2.Silva Y, Leira R, Tejada J, Lainez JM, Castillo J, Dávalos A, et al. Molecular signatures of vascular injury are associated with early growth of intracerebral hemorrhage. Stroke. 2005;36:86–91. doi: 10.1161/01.STR.0000149615.51204.0b. [DOI] [PubMed] [Google Scholar]
- 3.Hemphill JC, 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46:2032–60. doi: 10.1161/STR.0000000000000069. [DOI] [PubMed] [Google Scholar]
- 4.Dorman PJ, Sandercock PA. Considerations in the design of clinical trials of neuroprotective therapy in acute stroke. Stroke. 1996;27:1507–15. doi: 10.1161/01.str.27.9.1507. [DOI] [PubMed] [Google Scholar]
- 5.Andrabi SS, Parvez S, Tabassum H. Melatonin and ischemic stroke: Mechanistic roles and action. Adv Pharmacol Sci. 2015;2015:384750. doi: 10.1155/2015/384750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lekic T, Hartman R, Rojas H, Manaenko A, Chen W, Ayer R, et al. Protective effect of melatonin upon neuropathology, striatal function, and memory ability after intracerebral hemorrhage in rats. J Neurotrauma. 2010;27:627–37. doi: 10.1089/neu.2009.1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dianatkhah M, Ghaeli P, Hajhossein Talasaz A, Karimi A, Salehiomran A, Bina P, et al. Evaluating the potential effect of melatonin on the post-cardiac surgery sleep disorder. J Tehran Heart Cent. 2015;10:122–8. [PMC free article] [PubMed] [Google Scholar]
- 8.Buscemi N, Vandermeer B, Hooton N, Pandya R, Tjosvold L, Hartling L, et al. The efficacy and safety of exogenous melatonin for primary sleep disorders. A meta-analysis. J Gen Intern Med. 2005;20:1151–8. doi: 10.1111/j.1525-1497.2005.0243.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kurdi MS, Patel T. The role of melatonin in anaesthesia and critical care. Indian J Anaesth. 2013;57:137–44. doi: 10.4103/0019-5049.111837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Watson N, Diamandis T, Gonzales-Portillo C, Reyes S, Borlongan CV. Melatonin as an antioxidant for stroke neuroprotection. Cell Transplant. 2016;25:883–91. doi: 10.3727/096368915X689749. [DOI] [PubMed] [Google Scholar]
- 11.Altun A, Ugur-Altun B. Melatonin: Therapeutic and clinical utilization. Int J Clin Pract. 2007;61:835–45. doi: 10.1111/j.1742-1241.2006.01191.x. [DOI] [PubMed] [Google Scholar]
- 12.Hardeland R, Cardinali DP, Brown GM, Pandi-Perumal SR. Melatonin and brain inflammaging. Prog Neurobiol. 2015;127-128:46–63. doi: 10.1016/j.pneurobio.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 13.Macleod MR, O'Collins T, Horky LL, Howells DW, Donnan GA. Systematic review and meta-analysis of the efficacy of melatonin in experimental stroke. J Pineal Res. 2005;38:35–41. doi: 10.1111/j.1600-079X.2004.00172.x. [DOI] [PubMed] [Google Scholar]
- 14.Maitra S, Baidya DK, Khanna P. Melatonin in perioperative medicine: Current perspective. Saudi J Anaesth. 2013;7:315–21. doi: 10.4103/1658-354X.115316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Halvani AM, Abadi EE. Effect of melatonin on sleep quality of chronic obstructive pulmonary disease (COPD) patients. Eur Respir J. 2012;40:3477. [Google Scholar]
- 16.Chakraborti D, Tampi DJ, Tampi RR. Melatonin and melatonin agonist for delirium in the elderly patients. Am J Alzheimers Dis Other Demen. 2015;30:119–29. doi: 10.1177/1533317514539379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Jonghe A, Korevaar JC, van Munster BC, de Rooij SE. Effectiveness of melatonin treatment on circadian rhythm disturbances in dementia. are there implications for delirium? A systematic review. Int J Geriatr Psychiatry. 2010;25:1201–8. doi: 10.1002/gps.2454. [DOI] [PubMed] [Google Scholar]
- 18.Ward D, Fulbrook P. Nursing strategies for effective weaning of the critically ill mechanically ventilated patient. Crit Care Nurs Clin North Am. 2016;28:499–512. doi: 10.1016/j.cnc.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 19.Mutlu GM, Mutlu EA, Factor P. Prevention and treatment of gastrointestinal complications in patients on mechanical ventilation. Am J Respir Med. 2003;2:395–411. doi: 10.1007/BF03256667. [DOI] [PubMed] [Google Scholar]
- 20.Baid H. Patient safety: Identifying and managing complications of mechanical ventilation. Crit Care Nurs Clin North Am. 2016;28:451–62. doi: 10.1016/j.cnc.2016.07.005. [DOI] [PubMed] [Google Scholar]
- 21.Esteban A, Anzueto A, Frutos F, Alía I, Brochard L, Stewart TE, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: A 28-day international study. JAMA. 2002;287:345–55. doi: 10.1001/jama.287.3.345. [DOI] [PubMed] [Google Scholar]
- 22.Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the Intensive Care Unit. Crit Care Med. 2013;41:263–306. doi: 10.1097/CCM.0b013e3182783b72. [DOI] [PubMed] [Google Scholar]
- 23.Riker RR, Fraser GL. Adverse events associated with sedatives, analgesics, and other drugs that provide patient comfort in the Intensive Care Unit. Pharmacotherapy. 2005;25:8S–18S. doi: 10.1592/phco.2005.25.5_part_2.8s. [DOI] [PubMed] [Google Scholar]
- 24.Jarman A, Duke G, Reade M, Casamento A. The association between sedation practices and duration of mechanical ventilation in Intensive Care. Anaesth Intensive Care. 2013;41:311–5. doi: 10.1177/0310057X1304100306. [DOI] [PubMed] [Google Scholar]
- 25.Frisk U, Olsson J, Nylén P, Hahn RG. Low melatonin excretion during mechanical ventilation in the Intensive Care Unit. Clin Sci (Lond) 2004;107:47–53. doi: 10.1042/CS20030374. [DOI] [PubMed] [Google Scholar]
- 26.Dessap AM, Roche-Campo F, Launay JM, Charles-Nelson A, Katsahian S, Brun-Buisson C, et al. Delirium and circadian rhythm of melatonin during weaning from mechanical ventilation: An ancillary study of a weaning trial. Chest. 2015;148:1231–241. doi: 10.1378/chest.15-0525. [DOI] [PubMed] [Google Scholar]
- 27.Mistraletti G, Umbrello M, Sabbatini G, Miori S, Taverna M, Cerri B, et al. Melatonin reduces the need for sedation in ICU patients: A randomized controlled trial. Minerva Anestesiol. 2015;81:1298–310. [PubMed] [Google Scholar]
- 28.Parker JC, Hernandez LA, Peevy KJ. Mechanisms of ventilator-induced lung injury. Crit Care Med. 1993;21:131–43. doi: 10.1097/00003246-199301000-00024. [DOI] [PubMed] [Google Scholar]
- 29.Gitto E, Reiter RJ, Sabatino G, Buonocore G, Romeo C, Gitto P, et al. Correlation among cytokines, bronchopulmonary dysplasia and modality of ventilation in preterm newborns: Improvement with melatonin treatment. J Pineal Res. 2005;39:287–93. doi: 10.1111/j.1600-079X.2005.00251.x. [DOI] [PubMed] [Google Scholar]
- 30.Mistraletti G, Paroni R, Umbrello M, D'Amato L, Sabbatini G, Taverna M, et al. Melatonin pharmacological blood levels increase total antioxidant capacity in critically ill patients. Int J Mol Sci. 2017;18:pii: E759. doi: 10.3390/ijms18040759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tordjman S, Chokron S, Delorme R, Charrier A, Bellissant E, Jaafari N, et al. Melatonin: Pharmacology, functions and therapeutic benefits. Curr Neuropharmacol. 2017;15:434–43. doi: 10.2174/1570159X14666161228122115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ozdinc S, Oz G, Ozdemir C, Kilic I, Karakaya Z, Bal A, et al. Melatonin: Is it an effective antioxidant for pulmonary contusion? J Surg Res. 2016;204:445–51. doi: 10.1016/j.jss.2016.05.020. [DOI] [PubMed] [Google Scholar]
- 33.Arushanian EB. Experimental and clinical evidence for anticonvulsant activity of melatonin. Zh Nevrol Psikhiatr Im S S Korsakova. 2013;113:111–5. [PubMed] [Google Scholar]


