Abstract
Patient: Male, 43
Final Diagnosis: ST-elevation myocardial infarction
Symptoms: Dyspnea • ear pain
Medication: —
Clinical Procedure: Percutaneous coronary intervention
Specialty: Cardiology
Objective:
Unknown ethiology
Background:
Myocardial infarction (MI) is one of the most serious conditions presenting to the Emergency Department. Typical/classical symptoms of MI include chest pain and tightness that is referred to the left arm.
Case Report:
We present a case of ST-elevation myocardial infarction (STEMI) with a primary atypical presentation of right ear pain. The patient was diagnosed with STEMI based on electrocardiogram (ECG) and cardiac markers. As a result, the patient underwent percutaneous intervention (PCI), which showed an occluded left anterior descending artery (LAD) compared to the previous reported studies with similar presentation in which the right coronary artery (RCA) was affected.
Conclusions:
While MI is known for its typical presentation, being vigilant to patients who present atypically especially when they possess risk factors is extremely important and doing so can be critical to the outcome because MI treatment is dependent on fast and prompt management.
MeSH Keywords: Earache, Myocardial Infarction, Percutaneous Coronary Intervention
Background
A patient experiencing an MI characteristically reports having chest pain that radiates to the arms and neck, pressure to the chest, shortness of breath, and sweating [1,2]. While atypical presentation of MI is known to occur, especially in females, elderly, and patients with other comorbidities like diabetes, otalgia is still considered extremely rare as a presenting symptom, even in these cases [1–3].
To the best of our knowledge, and after searching PubMed, Cochrane Library, and Google scholar with the keywords (Myocardial infarction, STEMI, Otalgia, Earache, PCI), we found that only 5 cases of an MI with otalgia as a main presenting symptom were reported in the English literature, and we found no cases with this presentation that had an anterior infarction with a LAD occlusion, like in our case. Also, in 4 out of the 5 patients, risk factors (old age, smoking, diabetes mellitus) were reported that could explain the atypical presentation [1–4].
In this paper, we report an interesting case of a patient who presented to our Emergency Department with a STEMI, mainly complaining of right ear pain. We aim to show the importance of properly identifying these patients and promptly treating them.
Case Report
A 43-year-old Saudi man presented to the Emergency Department with a chief complaint of sharp right ear pain associated with mild dyspnea and fatigability, which began on the previous day. The patient did not complain of chest pain, chest tightness, nausea, vomiting, or dizziness. He had diabetes mellitus for 6 years that was controlled by medications, along with dyslipidemia for 2 years. He was a heavy smoker and has a family history of hypertension and ischemic heart disease. His pulse rate was 79 bpm and his blood pressure was 132/89 mmHg. The right ear appeared normal, with no tenderness. Results of his otoscopic examination were unremarkable.
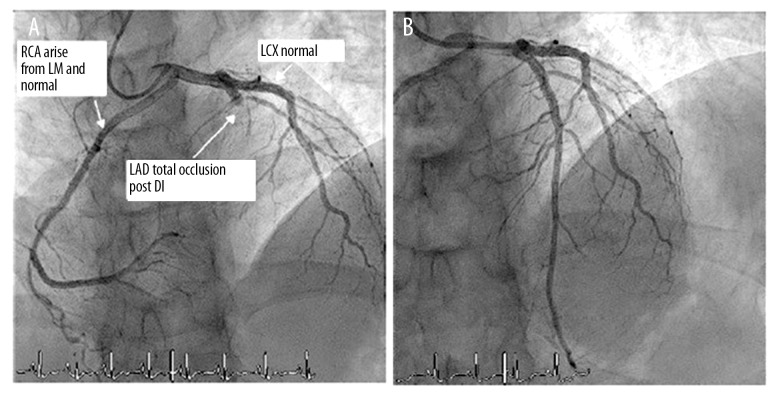
Due to the patient’s risk factors for coronary artery disease – diabetes mellitus, dyslipidemia, cigarette smoking, lack of physical activity, and family history of ischemic heart disease – an ECG was done, which showed normal sinus rhythm and ST elevations in the anterior leads, consistent with MI. His troponin T value was 165 ng/L. His routine CBC and biochemical values were unremarkable. Based on the elevated troponin T combined with the ECG changes, the patient was managed as a case of STEMI. After the acute coronary syndrome (ACS) protocol was initiated, it was decided for the patient to undergo primary PCI with door-to-balloon time of 139 minutes. A coronary angiogram showed selective opacification of the LAD coronary artery. The LAD coronary artery originates from the left anterior sinus. This artery was large and regular, without calcification. Mid-LAD had an acute occlusion, with reference diameter of 3.5 mm. However, the distal bed of LAD was not visualized. The 1st diagonal coronary artery had severe stenosis of 70–90%, which was mildly calcified, with reference diameter of 2.5 mm, and the distal bed was not diseased. The circumflex coronary artery originated from the left anterior sinus and was not diseased. The RCA originated from the left main coronary artery, which is considered a rare anomaly, with its course being between the aorta and pulmonary artery; however, the right coronary artery was large, regular, and without calcification or stenosis in this patient. Angioplasty was performed on the Mid-LAD and the 1st diagonal coronary artery with placement of 1 drug-eluting stent on Mid-LAD (Figure 1). The patient came to a follow-up appointment 2 weeks after PCI was done, in which he had no complaints or complications. He did not come to subsequent follow-up appointments.
Figure 1.
Coronary angiogram. (A) Before intervention showing total occlusion of LAD. (B) Restoration of normal flow post-stenting of LAD. RCA – right coronary artery, LM – left main artery, LCX – left Circumflex artery, LAD – left anterior descending artery, D1 – 1st diagonal coronary artery.
Discussion
Patients with an MI usually present with central retro-sternal chest pain and tightness that radiates to multiple regions, classically to the left arm but also possibly to the head and neck, but for an MI to manifest primarily as craniofacial pain without a chest pain is rare and even more so as an otalgia [2]. To demonstrate this, a study on 296 patients hospitalized with ischemic heart disease showed that only 53 patients experienced craniofacial pain, none of which was ear-specific, and was accompanied with chest pain in all of them [5]. Another study that included 186 patients with a confirmed acute coronary syndrome reported that 32% of them had craniofacial pain concurrent with other types of pain, while only 6% had craniofacial pain alone [6]. A literature review of 9 studies on the referred pain location for patients treated with a vagus nerve stimulator (VNS) demonstrated that the most common referred pain site was the throat and jaw, reported by 8 and 4 studies respectively, and only 1 study reported referred ear pain [7].
It has been theorized that referred pain from the heart to the craniofacial region is carried by the vagus nerve, especially seen in cases where RCA is occluded, as it supplies the right sinoatrial node that is innervated by the parasympathetic branches from the vagus nerve, which also carries visceral afferent fibers from the heart [1,3]. This mechanism can cause referred pain to the ear because the vagus nerve directly supplies the external auditory canal, which is known as the Arnold nerve [2,8]. Since our patient had an LAD and not an RCA occlusion, we theorize that referred pain to the vagus nerve can still occur because the sympathetic visceral afferent branches from the heart, which usually carry the pain signals, pass through the cardiac plexus, which the vagus nerve is part of [9]. The lack of pain manifestation in the chest or other common somatic regions can be explained by the patient’s medical history of diabetes and smoking, which are both known to be causes of such atypical presentation of MI [2].
The patient was coincidentally found to have an RCA anomaly as it passes between the aorta and pulmonary artery, which might subject it to an extra-luminal compression resulting in an MI [10]. However, we found that it was unrelated to his MI, as the RCA was normal and unaffected.
While it is important to know that MI can present atypically, as in our case, it is also crucial to keep in mind that even a typical MI presentation can be caused by other disorders that prompt treatment to prevent mortality and morbidity [11].
Conclusions
MI mortality and morbidity are time-dependent; thus, it is crucial to promptly identify and treat MI patients. Patients with risk factors for atypical presentation of MI should be investigated for it upon presenting to the healthcare provider, especially with unexplained pain in the ear, face, jaw, and arms, even with the lack of the characteristic chest pain. In our case, the patient’s atypical presentation was most likely due to his comorbidities and medical history, highlighting the importance of recognizing these patients.
Acknowledgments
We thank Lina Kibbi, MD, for the helpful discussions and input and the Specialized Medical Center Hospital management and staff in facilitating and helping our efforts to produce this case report.
References:
- 1.Dundar R, Kulduk E, Kemal Soy F, et al. Myocardial infarction as a rare cause of otalgia. Case Rep Otolaryngol. 2014;2014:106938. doi: 10.1155/2014/106938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sheikh M, Adlakha S, Chahal M, et al. “Cardiac otalgia”: Acute coronary syndrome masquerading as bilateral ear pain. Cardiol J. 2010;17(6):623–24. [PubMed] [Google Scholar]
- 3.Amirhaeri S, Spencer D. Myocardial infarction with unusual presentation of otalgia: A case report. Int J Emerg Med. 2010;3(4):459–60. doi: 10.1007/s12245-010-0222-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rothwell PM. Angina and myocardial infarction presenting with pain confined to the ear. Postgrad Med J. 1993;69(810):300–1. doi: 10.1136/pgmj.69.810.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bakhshi M, Rezaei R, Baharvand M, Bakhtiari S. Frequency of craniofacial pain in patients with ischemic heart disease. J Clin Exp Dent. 2017;9(1):e91. doi: 10.4317/jced.53078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kreiner M, Okeson JP, Michelis V, et al. Craniofacial pain as the sole symptom of cardiac ischemia: A prospective multicenter study. J Am Dent Assoc. 2007;138(1):74–79. doi: 10.14219/jada.archive.2007.0024. [DOI] [PubMed] [Google Scholar]
- 7.Myers DE. Vagus nerve pain referred to the craniofacial region. A case report and literature review with implications for referred cardiac pain. Br Dent J. 2008;204(4):187–89. doi: 10.1038/bdj.2008.101. [DOI] [PubMed] [Google Scholar]
- 8.Chen RC, Khorsandi AS, Shatzkes DR, Holliday RA. The radiology of referred otalgia. Am J Neuroradiol. 2009;30(10):1817–23. doi: 10.3174/ajnr.A1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Standring S, editor. Gray’s anatomy: The anatomical basis of clinical practice. Elsevier Health Sciences; 2015. pp. 202–3. [Google Scholar]
- 10.Ho JS, Strickman NE. Anomalous origin of the right coronary artery from the left coronary sinus: Case report and literature review. Texas Heart Inst J. 2002;29(1):37–39. [PMC free article] [PubMed] [Google Scholar]
- 11.Zou Y, Lin L, Xiao H, Xiang D. A rare case of toxic myocarditis caused by bacterial liver abscess mimicking acute myocardial infarction. Am J Case Rep. 2016;17:1–5. doi: 10.12659/AJCR.895350. [DOI] [PMC free article] [PubMed] [Google Scholar]