Abstract
Objective
The current study examined the adherence of psychiatrists to the Schedule of Recommended First and Second Line Antipsychotic Medications (“Antipsychotic Schedule”), which was implemented in two Recovery After an Initial Schizophrenia Episode (RAISE) Connection Program Implementation and Evaluation Study clinics.
Methods
Sixty-five individuals with a first episode of psychosis were enrolled in the RAISE Connection Program clinics. Two psychiatrists received training and ongoing consultation on using a shared decision-making approach to prescribing antipsychotic medications according to the Antipsychotic Schedule. Information on participants, prescribed antipsychotic medications, and completion of side effects assessments were obtained from standardized research assessments and chart extractions. Descriptive statistics were used to characterize the extent to which patterns of antipsychotic prescribing and side effect monitoring were consistent with the Antipsychotic Schedule.
Results
Over 90% (n=60) of participants were prescribed an antipsychotic medication, and received the medication on 76% (± 35%) of the days they were in treatment. Seventy-seven percent of participants were prescribed at least one Antipsychotic Schedule first-line antipsychotic, 20% were prescribed olanzapine, and 10% received a trial of clozapine. Regarding monitoring for metabolic side effects, 92% of participants (n=55) had at least one weight recorded, 72% (n=43) had at least one blood glucose measure recorded, and 62% (n=37) had at least one lipid profile recorded.
Conclusions
In the context of a controlled study, in which training and ongoing clinical supervision by experts was provided to psychiatrists and shared decision-making was encouraged, antipsychotic prescribing patterns closely adhered to recommendations established by the RAISE Connection Program.
Introduction
Multiple studies have examined the use of antipsychotic medications in people experiencing a first episode of schizophrenia or related disorder. These studies suggest that up to 80 percent of these individuals will respond to antipsychotic treatment; they are more likely to respond to lower doses; there are minimal efficacy differences among the various antipsychotics, but substantial differences in their side effect profiles; and adolescents are more sensitive than adults to adverse effects (1–8).
However, many people experiencing a first episode of schizophrenia will opt not to adhere to their prescribed antipsychotic regimen (9–14). Adverse effects are a major obstacle to ongoing treatment with these agents (9), with metabolic and neurological side effects, prolactin elevation, and sedation the most common and distressing. Non-adherence may also be related to not believing one is ill, substance abuse, and actual or perceived lack of medication efficacy (9–16). Antipsychotic treatment non-adherence can lead to inadequate symptom control, which can compromise the ability of the person to fully engage in treatment.
There is emerging evidence to suggest that the use of a shared decision-making approach may increase the likelihood of treatment participation. Shared decision-making is a collaborative process in which both consumers and providers are viewed as experts and equal partners in sharing knowledge and information with each other and actively participating in treatment decisions (17,18). The role of the treatment provider is to educate the consumer/family concerning available, evidence-based treatments; to share their clinical experience in using these treatments; to acknowledge and help clarify consumer preferences and values around treatment; and to empower consumers to take an active role in the treatment decision-making process. Consumers are the experts on their own values, lived experience with the disorder and treatments, and treatment preferences and goals (19). A shared decision-making approach reflects current efforts to increase consumer involvement in their own care, which is in line with a recovery-oriented, client-centered approach designed to foster treatment engagement (20–22).
We developed the Recovery After an Initial Schizophrenia Episode Connection Program (RAISE CP) Schedule of Recommended First and Second Line Antipsychotic Medications (“Antipsychotic Schedule”) to guide the selection of antipsychotic treatment within a shared decision-making framework. We conducted a longitudinal, observational study to evaluate the adherence of psychiatrists to the Antipsychotic Schedule in individuals with first episode schizophrenia participating in the RAISE CP Implementation and Evaluation Study (23).
Methods
An overview of the RAISE CP Implementation and Evaluation Study and primary and secondary study outcomes are provided elsewhere (23–26). In brief, RAISE CP was a multi-disciplinary and multi-element program designed to reduce morbidity and disability in individuals experiencing a first episode of psychosis suggestive of schizophrenia. Treatment was offered for up to two years and was based on a critical time intervention framework (27) that included community-based outreach. RAISE CP treatment teams were comprised of a Team Leader, an Individual Placement and Support worker, a Recovery Coach, and a psychiatrist, who was responsible for psychiatric assessment and medication management. The study was conducted at two sites: Baltimore, MD and Manhattan, NY, between July 2011 and March 2013. All participants (and, for minors, the participant’s parent or guardian) provided written informed consent; minors provided assent. The New York State Psychiatric Institute and University of Maryland Institutional Review Boards approved study procedures.
The Antipsychotic Schedule was used to guide antipsychotic medication management (see Table 1). The included medications had been previously shown to be effective for first-episode schizophrenia and, when prescribed appropriately, had relatively tolerable side effect profiles, thereby increasing the likelihood that the treatment experience would facilitate treatment engagement (1). Both oral and long-acting injectable (LAI) antipsychotics were included as first-line treatment options to increase the probability that there would be an available agent to meet the particular needs and preferences of a participant (28). We included most long-acting injectable antipsychotics, because these agents are relatively underutilized in the U.S., especially in individuals with first-episode psychosis. We did not include extended release olanzapine, because of the requirement that individuals who receive this agent most be observed for three hours after the injection. Oral olanzapine was recommended as a second-line treatment option, because of its increased liability for weight gain and other metabolic adverse effects (8). The recommended dosage range for all first- and second-line treatment options was the lower half of the Schizophrenia Patient Outcomes Research Team (PORT) recommended range for each agent for individuals with multi-episode schizophrenia (1). If distressing psychopathology persisted after two adequate antipsychotic trials, it was recommended that participants be offered a clozapine trial.
Table 1.
The RAISE Connection Program Schedule of Recommended First and Second Line Antipsychotic Medications
| Antipsychotic medication | Dosage range and frequency of administration |
|---|---|
| First-line treatment options | |
| Oral formulations | |
| Aripiprazole | 5–15 mg/day |
| Loxapine | 10–25 mg/day |
| Lurasidone | 40–80mg/day |
| Perphenazine | 4–12 mg/day |
| Risperidone | 1–4 mg/day |
| Long-acting injectable formulations | |
| Fluphenazine decanoate | 6.25–12.5 mg every 2 weeks |
| Haloperidol decanoate | 25–100 mg every 4 weeks |
| Paliperidone palmitate | 39–117 mg every 4 weeks |
| Risperidone microspheres | 12.5–50 mg every 2 weeks |
| Second-line treatment option | |
| Olanzapine | 5–15 mg/day |
Other agents (e.g., oral haloperidol) were not included in the Antipsychotic Schedule, because of concerns about longer-term efficacy and neurological side effects relative to other medications included in the Antipsychotic Schedule (1), or due to potentially burdensome administration in younger individuals (e.g., administering ziprasidone with food).
RAISE CP psychiatrists were expected to implement the Antipsychotic Schedule using a shared decision-making approach with participants and family members. The overarching expectation was that antipsychotic medications would be prescribed continuously to all individuals willing to accept such treatment. Measurement-based care principles were also employed to guide antipsychotic treatment management. Psychiatrists were asked to regularly evaluate treatment response and the occurrence of specific side effects. Psychiatrists used abbreviated (4 item) objective assessments, adapted from validated scales of positive (29), negative (30), and depressive (31) symptoms, to assess efficacy; a checklist to evaluate participant-reported antipsychotic side effects; and abbreviated assessments of extra-pyramidal side effects (3 items) (32) and tardive dyskinesia (1 item) (33) to assess neurological side effects. Symptom and side effect assessments were scheduled for the first visit, monthly for the first 3 months, and every 90 days thereafter. In order to evaluate possible weight gain and the development of metabolic abnormalities, it was recommended that psychiatrists measure weight at baseline and then monthly, and to obtain blood glucose and a lipid profile measures at baseline, 2 months later, and annually thereafter (25).
A two-day training followed by ongoing consultation with experts in the psychopharmacological management of psychosis, treatment of adolescents with psychotic disorders, and shared decision-making was provided to RAISE CP psychiatrists throughout the study. The consultation consisted of bimonthly hour-long conference calls and, as needed, telephone and e-mail consultations between the scheduled calls.
Data collection and data analyses
Information on previous antipsychotic prescriptions was collected through research interviews (23). Information on prescribed antipsychotic medications, including start and stop dates and dosages, and dates on which side effect assessments were completed were obtained from chart extractions (25).
We used descriptive statistics to describe the sample, and to characterize antipsychotic prescriptions to participants immediately prior to entry and while receiving treatment in the RAISE CP, including whether first- or second-line Antipsychotic Schedule antipsychotics were prescribed. We also computed the dosage mean, standard deviation, and median for each antipsychotic prescribed, and determined whether participants were prescribed dosages in the lower half of the ranges recommended by the Schizophrenia PORT (1). These dose analyses were only conducted for those medications for which there was more than one 30-day prescription.
To examine overall antipsychotic ‘coverage’, we computed the percentage of days that each participant was prescribed at least one antipsychotic medication, excluding days the participant was hospitalized. We excluded the first month of treatment from these calculations, because the majority of participants entered the study post-hospitalization with an active antipsychotic prescription and did not need a prescription from the team psychiatrist. We also excluded months 21–24 due to low sample size.
A number of participants were prescribed more than one antipsychotic during their study participation. Therefore, we calculated the median number of days until a participant was prescribed a 2nd and 3rd different antipsychotic medication, regardless of whether the antipsychotic was included in the Antipsychotic Schedule or not. These analyses only included participants who were prescribed an antipsychotic by the team psychiatrist. We also calculated the frequency of antipsychotic polypharmacy, which was examined using two different thresholds, i.e., the concurrent prescription of two or more different antipsychotic medications for at least 30 or 60 days. In these analyses, the same medication but different formulations were considered the same drug.
Finally, we evaluated adherence to the recommended frequency of side effect assessments by examining whether at least one side effect checklist, weight measurement, fasting blood glucose or glycosylated hemoglobin level, or lipid profile was recorded in the medical record at any time during the study.
Results
Sixty-five participants were enrolled in the study; their demographic and clinical characteristics can be found in the primary report (23). In brief, their mean age was 22.2 ± 4.2 years, 63% were male, and the Positive and Negative Syndrome Scale (34) mean total score was 64.0 ± 14.3. Over the course of their treatment, they experienced significant reductions in positive and negative symptoms, improvements in social and occupational functioning, and reported high rates of shared decision-making, with over 90% of participants reporting that their psychiatrist involved them in decisions about their medications (23,25).
Fifty-six of the 65 (86%) participants entered the study already prescribed an antipsychotic medication. Thirty-seven (66%) were prescribed an Antipsychotic Schedule first-line antipsychotic, 17 (30%) were prescribed a non-first-line antipsychotic medication, 2 (4%) were prescribed both first and non-first line antipsychotic medications, and 9 (14%) were not prescribed any psychotropic medications at study entry. Among these 9 individuals, 2 were never prescribed an antipsychotic during the study, 2 were prescribed a first-line antipsychotic medication, 2 received the second-line antipsychotic medication: olanzapine, and 3 were prescribed a non-first-line/non-second-line antipsychotic medication.
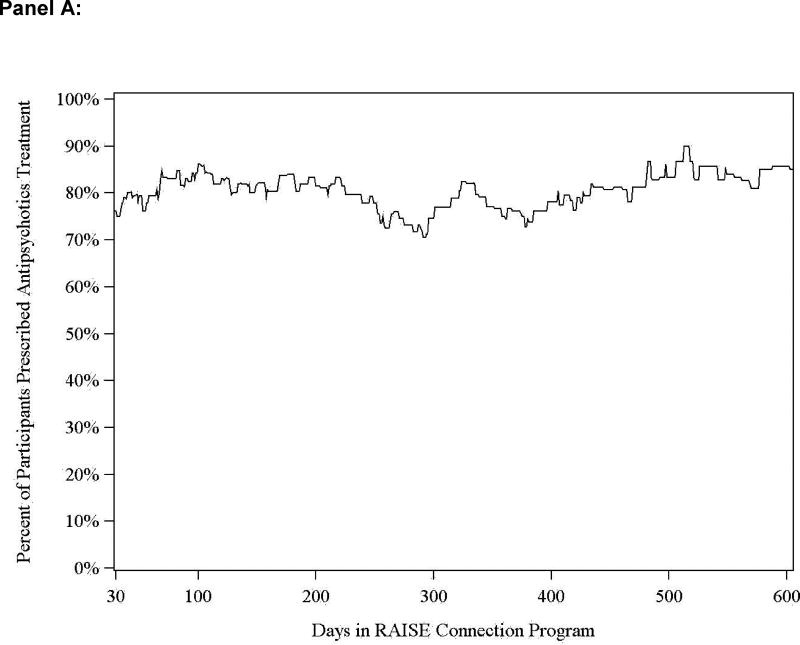
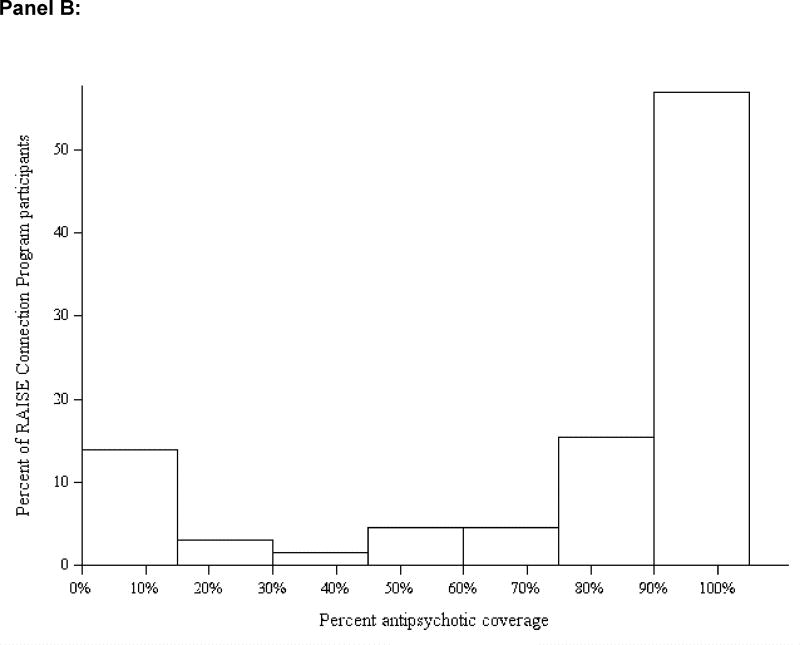
During the study period, 60 (92%) participants were ever and 5 (8%) were never prescribed an antipsychotic medication. The mean percentage of days all participants were prescribed at least one antipsychotic medication was 76% ± 35% (see Figure 1). The figure suggests that the percentage of participants who received an antipsychotic remained consistent over the course of the study (see Figure 1.A.). Among the 60 individuals who were ever prescribed an antipsychotic, the most commonly prescribed antipsychotics were: aripiprazole (n=26), oral risperidone (n=24), quetiapine (n=14), oral haloperidol (n=13), olanzapine (n=12), perphenazine (n=11), haloperidol long-acting injection (n=8), clozapine (n=6), and others (4 or less).
Figure 1.
Percentage of RAISE CP participants prescribed antipsychotic treatment
Mean and median prescribed doses, the prescribed dosage range, and the recommended dosage range for each antipsychotic with more than one 30-day prescription are displayed in Table 2. In general, mean prescribed dosages were within the recommended ranges, except for perphenazine (16.9 ± 8.6mg), which was prescribed above the recommended range, and for two antipsychotics not included in the Antipsychotic Schedule, oral haloperidol (12.0 ± 5.6mg) and quetiapine (269.9 ± 179.2mg), in which prescribed doses were above and below the recommended ranges, respectively.
Table 2.
Prescribed dosages of antipsychotic medications in the RAISE Connection Program
| Antipsychotic medication |
Recommended dosage range (mg) |
No. of drug days |
Mean dose (mg) |
Standard deviation |
Median dose (mg) |
Dosage range (mg) |
|---|---|---|---|---|---|---|
| Aripiprazole | 5–15 | 7167 | 12.95 | 8.73 | 10 | 2–40 |
| Clozapine | 200–600 | 1901 | 407.21 | 121.06 | 400 | 12.5–700 |
| Haloperidol (oral) | 2–6 | 3145 | 12.02 | 5.55 | 10 | 2–20 |
| Haloperidol decanoate | 25–100 | 1957 | 93.71 | 17.26 | 100 | 50–125 |
| Loxapine | 10–25 | 57 | 18.60 | 13.69 | 10 | 10–50 |
| Lurasidone | 40–80 | 414 | 44.15 | 12.22 | 40 | 40–80 |
| Olanzapine | 5–15 | 2707 | 9.40 | 7.17 | 5 | 2.5–30 |
| Perphenazine | 4–12 | 2392 | 16.88 | 8.61 | 16 | 2–40 |
| Quetiapine | 300–600 | 3421 | 269.88 | 176.25 | 200 | 25–800 |
| Risperidone (oral) | 1–4 | 4056 | 3.09 | 1.34 | 3 | 0.5–6 |
| Risperidone microspheres | 12.5–50 | 1291 | 31.56 | 12.95 | 25 | 12.5–50 |
Among the 60 individuals prescribed antipsychotics, 77% (n=46) were prescribed at least one Antipsychotic Schedule first-line antipsychotic. This included 7 of 16 individuals who entered RAISE CP prescribed a non-first-line antipsychotic, and 3 of 7 who entered the treatment program not receiving any antipsychotic treatment. Twelve individuals (20%) were prescribed a LAI antipsychotic, all of which were Antipsychotic Schedule first-line treatments.
During their time in the study, almost half of the participants were treated with a second antipsychotic (29/60; 48%). The median time to the prescription of the second antipsychotic was 58 days. The majority of these antipsychotics were first-line agents (23/29; 79%). Ten out of 60 (17%) participants were treated with a third antipsychotic. The median time to the prescription of the third antipsychotic was 161 days.
During the study, n=12 (20%) participants were prescribed olanzapine, including 5 individuals who entered RAISE CP on olanzapine and 7 participants newly prescribed olanzapine during the study. In two of these 7 cases, one or more first-line antipsychotics were prescribed prior to the olanzapine trial. If a participant did not respond to a second antipsychotic trial, RAISE CP psychiatrists were encouraged to consider prescribing clozapine. Six (10%) participants had at least one clozapine trial during the course of the study.
Less than a quarter of participants were prescribed non-recommended antipsychotics during the study, with 13/60 (22%) prescribed oral haloperidol and 14/60 (23%) prescribed quetiapine. Of note, 69% prescribed oral haloperidol and 57% prescribed quetiapine were prescribed one of the first-line antipsychotics at some other time during the study. At some point during the study, 14 (22%) participants were prescribed two concurrent antipsychotics for greater than 30 consecutive days; the most commonly prescribed antipsychotic combination was oral or injectable haloperidol with quetiapine. Olanzapine was prescribed to 2 of the 14 individuals, but no one received clozapine, prior to the initiation of antipsychotic polypharmacy. The use of a 60-day criterion for defining polypharmacy produced similar results.
All 60 participants prescribed an antipsychotic had one or more medication side effect checklists completed. While 55 (92%) participants had at least one weight recorded, only 43 (72%) participants had at least one blood glucose measure and only 37 (62%) had at least one lipid profile recorded during their RAISE CP participation.
Discussion
In line with RAISE CP recommendations, the majority of participants (92%) were prescribed an antipsychotic medication. The 74% average rate of antipsychotic coverage achieved likely reflects the use of a shared decision-making approach, in which participants were able to continue to receive RAISE CP services and meet with the psychiatrist, even if they did not receive antipsychotic treatment. These ongoing psychiatrist visits provided the opportunity for close monitoring of symptoms; the opportunity to restart antipsychotic medication if symptoms worsened; and facilitated the use of non-pharmacological approaches to symptom management, all of which were jointly agreed upon by the treatment team and the participant.
Over half of study participants entered the study already prescribed an Antipsychotic Schedule first-line antipsychotic, and almost 80% of those prescribed antipsychotics during the study received one of these agents, including 12 participants who were treated with a LAI antipsychotic. While approximately 20% of participants did receive a non-recommended antipsychotic, it is possible some patients requested to continue on their previously prescribed medication. However, it should be noted that 60–75% of those who received non-recommended antipsychotics were prescribed a first-line antipsychotic agent at some point during the study. Further, only three antipsychotics were prescribed at mean dosages that fell outside of RAISE CP recommended ranges, and two of these agents were non-first line medications. The large number of participants who were treated with a first-line antipsychotic, within the prescribed dosage range, supports the ability of psychiatrists to adhere to the use of the Antipsychotic Schedule. Since the medications included in the Antipsychotic Schedule were selected for tolerability, as well as efficacy (2–8), the extensive use of these first-line agents, within a shared decision-making framework, may have contributed to the high rate of engagement and retention of study participants, who remained in RAISE CP treatment for 91% (±21%) of the total possible time they could have received services (24).
While the literature is clear that individuals experiencing a first episode of psychosis are likely to respond to antipsychotic treatment, almost half of study participants received a second antipsychotic. A smaller percentage (17%) was treated with a third agent. In this study, only 20% of participants were prescribed the second-line antipsychotic olanzapine, a rate that was considerably lower than that reported in the RAISE Early Treatment Program (ETP) Study (32%). Also consistent with the RAISE CP Antipsychotic Schedule, six participants received at least one clozapine trial. These data suggest that prescribers should be prepared to engage in ongoing shared-decision making with patients in order to identify alternative medication choices consistent with their preferences.
Although not recommended, the use of antipsychotic polypharmacy was relatively common, with over 20% of participants treated, at some point during their study participation, with two antipsychotics. The 30- and 60-day criteria produced similar polypharmacy rates, which suggests that the observed cases were not examples of antipsychotic medication cross-titration. The antipsychotic polypharmacy rates were similar to those observed in the RAISE ETP Study (23%) (35). These data suggest that even early in the course of treatment, a subgroup of people with first-episode psychosis may experience inadequate symptom response prompting the use of treatment regimens typically reserved for individuals who are later in the course of their illness, including treatment regimens for which evidence for efficacy is lacking and concerns about safety have been raised (i.e., antipsychotic polypharmacy) (1).
Because antipsychotic medication side effects are major contributors to treatment non-adherence and can adversely effect physical health and well-being, the RAISE CP emphasized the role of the psychiatrist in monitoring the occurrence of side effects. Our ability to at least partially implement such monitoring was evidenced through the demonstration that all participants, who were prescribed an antipsychotic, were systematically asked about side effects at least once during their time in the program. While most participants had their weights recorded at least one time, these measurements occurred less frequently than the benchmark of at least once per month for individuals prescribed an antipsychotic. Consistent with previous research (36), glucose and lipid level evaluations also fell short of the recommended frequency. This demonstrates that even specialized services may have difficulty attaining recommended antipsychotic side effect monitoring goals. In this study, psychiatrists cited both logistical and patient barriers to adhering to the recommended monitoring schedule, including not having on-site phlebotomy or laboratory services. The addition of a nurse who can draw blood on site and develop a trusting relationship with individuals may address these barriers and has been implemented in current RAISE-based treatment teams.
This study had several limitations, including a relatively small sample size, the observational design, and prescribing patterns reflecting that of only two sites. Because the study lacked a comparison group, we cannot know if the extent of adherence to the Antipsychotic Schedule was a result of the training and ongoing consultation received by the psychiatrists or some other aspect of the controlled study. Also, while we were able to evaluate whether common antipsychotic side effects were assessed, we were unable to examine whether the recommended symptom assessments were completed, although participants reported high rates of having their psychiatrist ask them about symptoms and side effects (25). Finally, we recognize that there may be disagreements regarding the inclusion and exclusion of specific agents in the Antipsychotic Schedule. For example, despite recommending long-acting injectable haloperidol as a first-line treatment, we elected not to include low dose oral haloperidol, because of controlled studies suggesting that long-term efficacy was not comparable to other agents included in the Antipsychotic Schedule and that haloperidol may be associated with more neurological side effects (1). However, a reasonable approach would have been to include oral haloperidol as a second-line treatment.
Conclusions
In a controlled study, RAISE CP psychiatrists largely adhered to a schedule that recommended specific antipsychotic agents and dosage ranges to individuals experiencing a first episode of psychosis. The ability to adhere to the schedule was facilitated through the use of a shared-decision making framework to maintain participant engagement in treatment. The implementation of shared decision-making was enhanced by training and clinical supervision sessions for psychiatrists led by experts in these treatments, including an individual with lived experience with the disorder. The extent to which these components of the approach to the pharmacological treatment of this population can be feasibly disseminated and implemented in regular clinical practice requires additional investigation.
Acknowledgments
Dr. C has served on advisory boards for the following: Alkermes, Ameritox, Forum, Otsuka/Lundbeck, Merck. Dr. C has served as an expert witness for Forest. Dr. C has received research grants from the following companies: Alkermes, Ameritox, Auspex, Avanir, Otsuka, Merck, Roche/Genentech, Sunovion. Dr. G provides training in a derivative of the RAISE Connection program, but does not accrue any personal income from this activity. Dr. I has served on advisory boards for the following: AbbVie, Amgen, Boehringer Ingelheim-RCV, EnVivo (now Forum), Lundbeck, Roche, and Takeda; has served as a consultant for AbbVie, BMS, EnVivo (now Forum), and Omeros; and has served on a Data and Safety Monitoring Board for Pfizer.
This project was funded in part with federal funds from the American Recovery and Reinvestment Act of 2009, from the National Institute of Mental Health under contract HHSN271200900020C (Dr. G, principal investigator), and from the New York State Office of Mental Health and the Maryland Mental Hygiene Administration.
Footnotes
Disclosures
Dr. A, Dr. B, Dr. D, Dr. E, Dr. F, and Dr. H, report no potential conflicts of interest.
Contributor Information
Julie Kreyenbuhl, University of Maryland School of Medicine - Psychiatry, Baltimore, Maryland; VA Capitol Healthcare Network (VISN 5) Mental Illness Research, Education, and Clinical Center (MIRECC) - Baltimore, Maryland.
Deborah Medoff, University of Maryland School of Medicine - Psychiatry, Baltimore, Maryland; VA Capitol Healthcare Network (VISN 5) Mental Illness Research, Education, and Clinical Center (MIRECC), Baltimore, Maryland.
Joseph P. McEvoy, Georgia Regents University, Medical College of Georgia - Psychiatry, Augusta, Georgia
Thomas E. Smith, Columbia University College of Physicians and Surgeons - Psychiatry, New York City, New York New York State Psychiatric Institute – Psychiatry, New York.
Ann Hackman, University of Maryland School of Medicine - Psychiatry, Baltimore, Maryland.
Ilana R. Nossel, Columbia University College of Physicians and Surgeons - Psychiatry, New York New York State Psychiatric Institute, New York.
Lisa B. Dixon, Columbia University College of Physicians and Surgeons - Psychiatry, New York New York State Psychiatric Institute - Psychiatry, New York.
Susan M. Essock, College of Physicians & Surgeons, Columbia University - Psychiatry, New York New York State Psychiatric Institute - Mental Health Services and Policy Research, New York.
Robert W. Buchanan, Maryland Psych Res Center – Department of Psych, Baltimore, Maryland
References
- 1.Buchanan RW, Kreyenbuhl J, Kelly DL, et al. The 2009 Schizophrenia PORT Psychopharmacological Treatment Recommendations and Summary Statements. Schizophrenia Bulletin. 2010;36:71–93. doi: 10.1093/schbul/sbp116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lieberman JA, Phillips M, Gu H, et al. Atypical and conventional antipsychotic drugs in treatment naïve first episode schizophrenia: a 52-week randomized trial of clozapine vs. chlorpromazine. Neuropsychopharmacology. 2003;28:995–1003. doi: 10.1038/sj.npp.1300157. [DOI] [PubMed] [Google Scholar]
- 3.Schooler N, Rabinowitz J, Davidson M, et al. Risperidone and haloperidol in first-episode psychosis: A long-term randomized trial. American Journal of Psychiatry. 2005;162:947–953. doi: 10.1176/appi.ajp.162.5.947. [DOI] [PubMed] [Google Scholar]
- 4.Robinson DG, Woerner MG, Napolitano B, et al. Randomized comparison of olanzapine versus risperidone for the treatment of first-episode schizophrenia: 4-month outcomes. American Journal of Psychiatry. 2006;163:2096–2102. doi: 10.1176/ajp.2006.163.12.2096. [DOI] [PubMed] [Google Scholar]
- 5.Gaebel W, Riesbeck M, Wolwer W, et al. Maintenance treatment with risperidone or low-dose haloperidol in first-episode schizophrenia: 1 year results of a randomized controlled trial within the German Research Network on Schizophrenia. Journal of Clinical Psychiatry. 2007;68:1763–1774. doi: 10.4088/jcp.v68n1116. [DOI] [PubMed] [Google Scholar]
- 6.McEvoy JP, Lieberman JA, Perkins DO, et al. Efficacy and tolerability of olanzapine, quetiapine, and risperidone in the treatment of early psychosis: a randomized, double-blind 52-week comparison (CAFE) American Journal of Psychiatry. 2007;164:1050–1060. doi: 10.1176/ajp.2007.164.7.1050. [DOI] [PubMed] [Google Scholar]
- 7.Kahn RS, Fleischhacker WW, Boter H, et al. Effectiveness of antipsychotic drugs in first-episode schizophrenia and schizophreniform disorder: an open randomised clinical trial. Lancet. 2008;371:1085–1097. doi: 10.1016/S0140-6736(08)60486-9. [DOI] [PubMed] [Google Scholar]
- 8.Sikich L, Frazier JA, McClellan J, et al. Double-blind comparison of first- and second- generation antipsychotics in early-onset schiozphrenia and schizo-affective disorder: findings from the treatment of early-onset schizophrenia spectrum disorders (TEOSS) study. American Journal of Psychiatry. 2008;165:1420–1431. doi: 10.1176/appi.ajp.2008.08050756. [DOI] [PubMed] [Google Scholar]
- 9.Velligan DI, Weiden PJ, Sajatovic M, et al. The expert consensus guideline series: adherence problems in patients with serious and persistent mental illness. Journal of Clinical Psychiatry. 2009;70(Suppl 4):1–46. [PubMed] [Google Scholar]
- 10.Robinson DG, Woerner MG, Alvir JMJ, et al. Predictors of medication discontinuation by patients with first-episode schizophrenia and schizoaffective disorder. Schizophrenia Research. 2002;57:209–219. doi: 10.1016/s0920-9964(01)00312-7. [DOI] [PubMed] [Google Scholar]
- 11.Kamali M, Kelly BD, Clarke M, et al. A prospective evaluation of adherence to medication in first episode schizophrenia. European psychiatry: the journal of the Association of European Psychiatrists. 2006;21:29–33. doi: 10.1016/j.eurpsy.2005.05.015. [DOI] [PubMed] [Google Scholar]
- 12.Perkins DO, Gu H, Weiden PJ, et al. Predictors of treatment discontinuation and medication nonadherence in patients recovering from a first episode of schizophrenia, schizophreniform disorder, or schizoaffective disorder: a randomized, double-blind, flexible-dose, multicenter study. Journal of Clinical Psychiatry. 2008;69:106–113. doi: 10.4088/jcp.v69n0114. [DOI] [PubMed] [Google Scholar]
- 13.Coldham El, Addington J, Addington D. Medication adherence of individuals with a first-episode of psychosis. Acta psychiatrica Scandinavica. 2002;106:286–290. doi: 10.1034/j.1600-0447.2002.02437.x. [DOI] [PubMed] [Google Scholar]
- 14.Subotnik KL, Nuechterlein KH, Ventura J, et al. Risperidone nonadherence and return of positive symptoms in the early course of schizophrenia. American Journal of Psychiatry. 2011;168:286–92. doi: 10.1176/appi.ajp.2010.09010087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mutsatsa SH, Joyce EM, Hutton SB, et al. Clinical correlates of early medication adherence: West London first episode schizophrenia study. Acta psychiatrica Scandinavica. 2003;108:439–446. doi: 10.1046/j.0001-690x.2003.00193.x. [DOI] [PubMed] [Google Scholar]
- 16.Perkins DO, Johnson JL, Hamer RA, et al. Predictors of antipsychotic medications adherence in patients recovering from a first psychotic episode. Schizophrenia Research. 2006;83:53–63. doi: 10.1016/j.schres.2005.10.016. [DOI] [PubMed] [Google Scholar]
- 17.Adams J, Drake R. Shared decision-making and evidence-based practice. Community Mental Health Journal. 2006;42:87–105. doi: 10.1007/s10597-005-9005-8. [DOI] [PubMed] [Google Scholar]
- 18.Deegan PE, Drake RE. Shared decision making and medication management in the recovery process. Psychiatric Services. 2006;57:1636–1639. doi: 10.1176/ps.2006.57.11.1636. [DOI] [PubMed] [Google Scholar]
- 19.Mistler LA, Drake RE. Shared decision making in antipsychotic management. Journal of Psychiatric Practice. 2008;14:333–44. doi: 10.1097/01.pra.0000341889.97759.54. [DOI] [PubMed] [Google Scholar]
- 20.Achieving the Promise: Transforming Mental Health Care in America. Rockville, Md: Department of Health and Human Services, President’s New Freedom Commission on Mental Health; 2003. Pub no SMA-03-3832. [Google Scholar]
- 21.Drake RE, Deegan PE, Rapp C. The promise of shared decision making in mental health. Psychiatric Rehabilitation Journal. 2010;34:7–13. doi: 10.2975/34.1.2010.7.13. [DOI] [PubMed] [Google Scholar]
- 22.Kreyenbuhl J, Nossel IR, Dixon LB. Disengagement from mental health treatment among individuals with schizophrenia and strategies for facilitating connections to care: A review of the literature. Schizophrenia Bulletin. 2009;35:696–703. doi: 10.1093/schbul/sbp046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dixon LB, Goldman HH, Bennett ME, et al. Implementing coordinated specialty care for early psychosis: The RAISE Connection Program. Psychiatric Services. 2015;66:691–8. doi: 10.1176/appi.ps.201400281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marino L, Nossel I, Choi JC, et al. The RAISE Connection Program for early psychosis: Secondary outcomes and mediators and moderators of improvement. Journal of Nervous and Mental Disease. 2015;203:365–71. doi: 10.1097/NMD.0000000000000293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Essock SM, Nossel IR, McNamara K, et al. Practical monitoring of treatment fidelity: Examples from a team-based intervention for people with early psychosis. Psychiatric Services. 2015;66:674–6. doi: 10.1176/appi.ps.201400531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Essock SM, Goldman HH, Hogan MF, et al. State partnerships for first-episode psychosis services. Psychiatric Services. 2015;66:671–3. doi: 10.1176/appi.ps.201400117. [DOI] [PubMed] [Google Scholar]
- 27.Herman D, Conover S, Felix A, et al. Critical Time Intervention: an empirically supported model for preventing homelessness in high risk groups. Journal of Primary Prevention. 2007;28:295–312. doi: 10.1007/s10935-007-0099-3. [DOI] [PubMed] [Google Scholar]
- 28.Subotnik KL, Casaus LR, Ventura J, et al. Long-acting injectable risperidone for relapse prevention and control of breakthrough symptoms after a recent first episode of schizophrenia: A randomized clinical trial. JAMA Psychiatry. 2015;72:822–829. doi: 10.1001/jamapsychiatry.2015.0270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychological Reports. 1962;10:799–812. [Google Scholar]
- 30.Andreasen NC. Negative symptoms in schizophrenia: definition and reliability. Archives of General Psychiatry. 1982;39:784–788. doi: 10.1001/archpsyc.1982.04290070020005. [DOI] [PubMed] [Google Scholar]
- 31.Addington D, Addington J, Schissel B. A depression rating scale for schizophrenics. Schizophrenia Research. 1990;3:247–251. doi: 10.1016/0920-9964(90)90005-r. [DOI] [PubMed] [Google Scholar]
- 32.Simpson GM, Angus JWS. A rating scale for extrapyramidal side effects. Acta psychiatrica Scandinavica. 1970;212:11–19. doi: 10.1111/j.1600-0447.1970.tb02066.x. [DOI] [PubMed] [Google Scholar]
- 33.Guy W. ECDEU Assessment Manual for Psychopharmacology: Revised (DHEW publication number ADM 76-338) Rockville, MD: US Department of Health, Education and Welfare, Public Health Service, Alcohol, Drug Abuse and Mental Health Administration, NIMH Psychopharmacology Research Branch, Division of Extramural Research Programs; 1976. pp. 534–537. [Google Scholar]
- 34.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophrenia Bulletin. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 35.Robinson DG, Schooler NR, John M, et al. Prescription practices in the treatment of first-episode schizophrenia spectrum disorders: data from the national RAISE-ETP study. American Journal of Psychiatry. 2015;172:237–248. doi: 10.1176/appi.ajp.2014.13101355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mitchell AJ, Delaffon V, Vancampfort D, et al. Guideline concordant monitoring of metabolic risk in people treated with antipsychotic medication: systematic review and meta-analysis of screening practices. Psychological Medicine. 2012;42:125–47. doi: 10.1017/S003329171100105X. [DOI] [PubMed] [Google Scholar]