Abstract
Background
Mandibular setback osteotomies potentially lead to narrowing of the pharyngeal airways, subsequently resulting in post-surgical obstructive sleep apnea (OSA).
Objective
To summarize current evidence from systematic reviews that has evaluated pharyngeal airway changes after mandibular setback with or without concomitant upper jaw osteotomies.
Methodology
PubMed, EMBASE, Web of Science, and Cochrane Library databases were searched with no restriction of language or date. Systematic reviews studying changes in pharyngeal airway dimensions and respiratory parameters after mandibular setback with or without concomitant upper jaw osteotomies have been identified, screened for eligibility, included and analyzed in this study.
Results
Six systematic reviews have been included. While isolated mandibular setback osteotomies result in reduced oropharyngeal airway dimensions, the reduction is lesser in cases with concomitant upper jaw osteotomies. Only scarce evidence exists currently to what happens to naso- and hypo-pharyngeal airways. There is no evidence for post-surgical OSA, even though some studies reported reduced respiratory parameters after single-jaw mandibular setback with or without concomitant upper jaw osteotomies.
Conclusion
Although mandibular setback osteotomies reduce pharyngeal airway dimensions, evidence confirming post-surgical OSA was not found. Nevertheless, potential post-surgical OSA should be taken into serious consideration during the treatment planning of particular orthognathic cases. As moderate evidence exists that double-jaw surgeries lead to less compromised post-surgical pharyngeal airways, they should be considered as the method of choice especially in cases with severe dentoskeletal Class III deformity.
Study registration
PROSPERO (registration number: CRD42016046484).
Introduction
Little attention has been paid to mandibular setback osteotomies and potentially compromised concomitant pharyngeal airways, though sporadic cases of post-surgical obstructive sleep apnea (OSA) have been reported since the 1980s[1, 2]. This potential post-surgical complication has been investigated more vigorously only since the last two decades. Numerous researchers[3–17] have investigated and evaluated the relationship between various orthognathic procedures, concomitant changes of pharyngeal airway dimensions and OSA. Movements of mandibular jaw segments during orthognathic surgery will affect the hyoid bone and tongue positions, which in turn might influence pharyngeal airway dimensions[18]. A narrow pharyngeal airway has always been considered as a predisposing factor for OSA, a disease that might affects both patient’s quality of life and physical health[19].
In principle, mandibular prognathism can be corrected by single-jaw mandibular setback osteotomies. However, a severe sagittal antero-posterior (AP) discrepancy of the jaws is usually tackled by a concomitant upper jaw osteotomy to reduce the magnitude of the mandibular setback. To date, some authors[10, 20] have claimed that single-jaw mandibular setback osteotomies will reduce pharyngeal airway dimensions significantly, while others[6, 7] suggested that two-jaw orthognathic surgeries might produce a less compromised post-surgical pharyngeal airways.
The actual anatomical and physiological changes in post-surgical pharyngeal airways, especially in correlations with different jaw movements are yet to be established. Therefore, an overview of systematic reviews is valuable to analyze and summarize the available data, and to identify any weaknesses, inconsistencies or unanswered questions in this research field. Hence, this article aimed to summarize and analyzed critically to date’s evidence from systematic reviews regarding to the question of how mandibular setback with or without concomitant maxillary osteotomies affects the post-surgical pharyngeal airway’s dimensions and respiratory outcomes in relation to iatrogenic post-surgical OSA.
Methodology
The reporting of these systematic reviews adheres to the Cochrane’s recommendation on overview of systematic reviews[21], and the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement[22, 23] where relevant. A review protocol was developed and registered with PROSPERO; registration number CRD42016046484 (http://www.crd.york.ac.uk/prospero/display_record.asp?ID=CRD42016046484).
Search method
The electronic databases PubMed, EMBASE, Web of Science, Scopus and Cochrane Library were searched using the search strategy outlined in Table 1. The Web of Science database search has included the search of both journals and proceedings. The last search was performed on 22nd April 2017 with no limitation on publication language or timeline. Subsequently, the search results were exported into Endnote X7 (Thomson Reuters, CA, USA) and duplicates were removed. The title and abstract of all articles were then screened for eligibility according to the pre-determined inclusion and exclusion criteria. The full texts of relevant articles were retrieved. Lastly, the reference lists of those articles were screen manually for further relevant articles. Two authors (TSK and RAZ) have performed both electronic and manual searches independently. Disagreement was resolved by discussion with the other two authors.
Table 1. Electronic databases search strategy (refer to S1 Text for the detailed search strategy).
| ELECTRONIC DATABASES | SEARCH STRATEGY |
|---|---|
| PubMed | (Systematic review OR review OR overview OR meta-analysis OR evidence based medicine OR evidence based dentistry OR review literature OR literature review) |
| EMBASE | AND |
| Web of Science | (orthognathic surgery OR orthognathic surgical procedure OR orthodontics surgery OR mandibular surgery OR maxillary surgery OR bimaxillary surgery OR jaw surgery OR surgical orthodontic treatment OR jaw setback OR jaw movement OR mandibular setback OR maxillary advancement) |
| Cochrane library | AND |
| Scopus | (upper airway OR pharynx OR pharyngeal OR oropharynx OR oropharyngeal OR nasopharynx OR nasopharyngeal OR hypopharynx OR hypopharyngeal) |
Selection of reviews
This overview has included systematic reviews that have assessed linear, cross sectional plane, or volumetric pharyngeal airway changes related to mandibular setback with or without concomitant maxillary osteotomies. Additionally, data on respiratory parameter changes in those reviews have also been assessed.
However, systematic reviews including cleft lip and palate and/or syndromic patients as well as reviews comprising cases of distraction osteogenesis were excluded from this overview.
Data extraction and management
Two authors (TSK, RAZ) extracted the following data from eligible systematic reviews independently: authors, publication year and title, method of analysis, number and study design of included studies, sample population (number, age and gender of patients), type of interventions, outcome measures and main findings, and follow up period.
Subsequently, all extracted data were inserted in pre-tabulated data sheets (Excel, Microsoft, New Mexico). Any disagreement was resolved by consensus of all authors to ensure consistency and reliability of extracted data.
Assessment of methodological quality of included reviews
The methodological quality of all included reviews was assessed independently by TSK and RAZ, using the Assessment of Multiple Systematic Reviews (AMSTAR) tool[24]. Furthermore, the quality of evidence of the primary studies included in this overview was evaluated based on assessments reported by each systematic review. Disagreements were resolved by in-depth discussion among all authors.
Data synthesis
Generally, the overview of the included systematic reviews was narrated. Additionally, meta-analysis was also performed when possible by pooling the data from primary studies across different included reviews using the “Review Manager” software (RevMan version 5.3; Copenhagen: Nordic Cochrane Center, Cochrane Collaboration; 2014). Only one primary study was included in the meta-analysis in case of an overlapping. Treatment effects across the studies were combined using the fixed effect model. The heterogeneity of trial results was assessed with the χ2 test for heterogeneity (p = 0.1) and the Ι2 measure for inconsistency. A significant heterogeneity was considered when p < 0.1 for χ2 test or Ι2 > 50%. Funnel plot was used to assess publication bias and Egger regression test was used to assess asymmetric funnel plot when more than ten primary studies were included in an analysis[25, 26].
Results
Quantity of current evidence
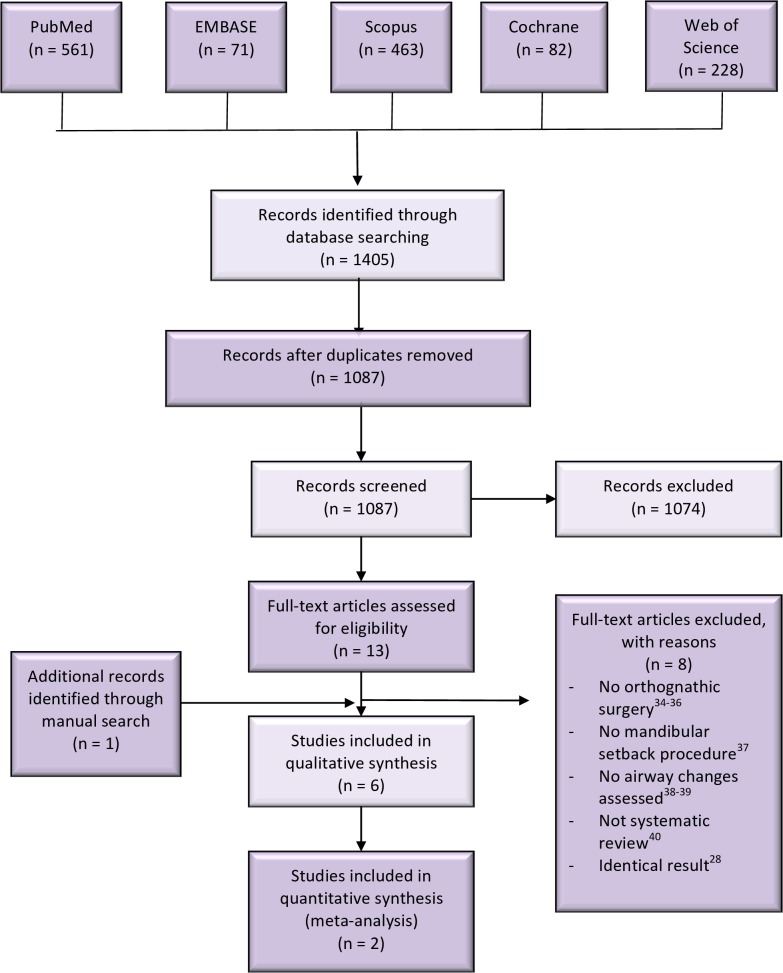
The search of electronic databases has generated an overall of 1405 articles. Titles and abstracts of 1087 articles were screened after removing duplicates. Full texts of 13 relevant articles were retrieved and assessed for their inclusion eligibility. The manual search of the reference lists of those 13 articles revealed one more relevant article. Seven articles[18, 27–32] have fulfilled both inclusion and exclusion criteria. A group of authors, with identical meta-analyses and results have published two systematic reviews[27, 28] in two different languages[33]. Although there was no language limitation on article selection, only one[27] of these studies has been included in this overview due to the reason stated above. Finally, eight articles were excluded[28, 34–40], while only six articles[18, 27, 29–32] were included for further analyses. The study selection process is summarized in Fig 1.
Fig 1. Study selection process.
Four[27, 29, 30, 32] of these systematic reviews have focused on mandibular setback with or without concomitant maxillary osteotomies, while two others[18, 31] investigated multiple orthognathic procedures. The characteristics of the included articles are shown in Table 2. Although five reviews[18, 27, 29–31] declared no conflict of interest, there was one review[32] did not mention about it. Besides, four included systematic reviews[18, 29, 31, 32] reported that they were not funded, one[30] did not declare on funding status, and only one review[27] was funded.
Table 2. Characteristics of included systematic reviews.
| Authors, year | Type of review | Database searched | Primary studies that have assessed dimensional changes of upper airway | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Airway assessed | Included studies | Participants | Interventions | Outcome | Measurement | Maximum follow-up period (Range) | ||||||
| With mandibular setback (Total) | Type | Total number (Range) | M/F | Age Range of mean (years) | ||||||||
| Al-Moraissi et al[29], 2015 | MA | Pubmed, Ovid, MEDLINE, Cochrane Central. | NP | 8 (8) | 1 RCT | 380 | 114/266 | 23.3- | 198 BM | Linear and cross-sectional area | 6 ceph | PO 6 months- |
| OP | 5 CCT | (21–78) | 28.2 | 183 MS | 1 CT | 2 years | ||||||
| HP | 2 R | (NR: 2 studies) | 1 CBCT | (NR: 3 studies) | ||||||||
| Canellas et al[30], 2015 | SR | PubMed interface of Medline, Science Direct platform, Cochrane library. | PAS | 9# (9) | 2 CCT | 232 | 84/148 | 20–25 | 134 BM | Cross-sectional area, volume and breathing parameters | 1 CBCT | PO 6–17 months |
| 6 CS | (6–78) | (NR: 1 study) | 98 MS | 7 Ceph | ||||||||
| 1 NR | ||||||||||||
| Christovam et al[31], 2016 | MA | Cochrane library, Medline (via PubMed), Scopus, VHL, Web of Science, Open-Grey. | UA | 15 (27) | 13 R | 391 |
185/181 |
20.3–30.04 | 106 MS | Cross-sectional area and volume | CT | PO 2 months- |
| 781 MxA+MS | ||||||||||||
| 2 P | (12–60) | (NR: 1 study) | 30 MxI+MS | >1 year | ||||||||
| 30 MxS+MxI+MS | ||||||||||||
| 20MxS+Ms | ||||||||||||
| Fernandez-Ferrer et al[32], 2015 | SR | Scopus, Pubmed, Cochrane, EMBASE. | NP | 14 (14) | 369 | 160/197 | 20.3–25.5 | MS | Linear, cross-sectional area, volume and respiratory parameters | 8 3-D imaging | 28 days-1.4 years | |
| OP | 12 R | |||||||||||
| 2 P | (9–78) | (NR: 2 studies) | (NR: 3 studies) | BM | 6 ventilation | (NR: 2 studies) | ||||||
| HP | ||||||||||||
| He et al[27], 2017 | MA | Scopus, Pubmed, Cochrane, EMBASE, Web of Science | NP | 18 (18) | 564 | 253/311 | 18.8–26.6 | 299 MxA+MdS | Cross-sectional area and volume | CT | NR | |
| OP | 12R | |||||||||||
| 6P | (11–72) | 264 Mds | ||||||||||
| HP | ||||||||||||
| Mattos et al[18], 2011 | MA | VHL, Scirus, Ovid, SIGLE. | OP | 19(22) | 12 R | 665 | 107/426 | 17.9–30 | 428 MS | Linear and cross-sectional area | 15: Ceph | PO 1 |
| 7 P | (10–66) | (NR: 3 studies) | (NR: 1 study) | 205 MxA+MS | 2: CT | month- | ||||||
| 2: Ceph + CT | 12 years | |||||||||||
# One of the included study did not assess the upper airway changes, but post-operative OSA was evaluated
Abbreviations:
SR = systematic review; MA = meta-analysis; NP = nasopharyngeal, OP = oropharyngeal, HP = hypopharyngeal, UA = upper airways, PAS = pharyngeal airway space; R = Retrospective study; P = Prospective study; RCT = randomized controlled trial; CCT = Case controlled trials; CS = Case series; MS = Mandibular setback, BM = bimaxillary surgery; MxA = Maxillary advancement, MMA = Maxillomandibular advancement; MxI = Maxillary impaction; MxS = maxillary; setback; Ceph = Cephalometric; CT = Computed tomography; CBCT = Cone-beam computed tomography; NR = not reported; PO = post-operative
Quality of systematic reviews (AMSTAR)
Analysis with the AMSTAR tool revealed that only three systematic reviews with high scores of 8[27, 31] and 10[18] “yes”, whereas the others[29, 30, 32] have scored 5 or less (Table 3). Although only three systematic reviews[18, 27, 31] reported on an ‘a priori’ design, all six articles have performed a comprehensive literature search with three or more electronic databases. The review of Mattos et al[18] accomplished the highest score of “yes”, and was the only review that has listed and referenced both included as well as excluded studies.
Table 3. Quality assessment of included systematic reviews with AMSTAR tool.
| AMSTAR criteria | *Al-Moraissi et al[29] | Canellas et al[30] | *Christovam et al[31] | Fernandez-Ferrer et al[32] | He et al[27] | *Mattos et al[18] |
|---|---|---|---|---|---|---|
| 1. Was an ‘a priori’ design provided? | CA | CA | Y | CA | Y | Y |
| 2. Was there duplicate study selection and data extraction? | CA | Y | Y | Y | Y | Y |
| 3. Was a comprehensive literature search performed? | Y | Y | Y | Y | Y | Y |
| 4. Was the status of publication (i.e. grey literature) used as an inclusion criterion? | Y | N | Y | N | N | Y |
| 5. Was a list of studies (included and excluded) provided? | N | N | N | N | N | Y |
| 6. Were the characteristics of the included studies provided? | Y | Y | Y | Y | Y | Y |
| 7. Was the scientific quality of the included studies assessed and documented? | Y | N | Y | Y | Y | Y |
| 8. Was the scientific quality of the included studies used appropriately in formulating conclusions? | N | NA | Y | N | Y | Y |
| 9. Were the methods used to combine the findings of studies appropriate? | Y | N | Y | Y | Y | Y |
| 10. Was the likelihood of publication bias assessed? | N | N | N | N | Y | Y |
| 11. Was the conflict of interest stated? | CA | CA | CA | CA | CA | CA |
| TOTAL “YES” | 5 | 3 | 8 | 5 | 8 | 10 |
Y = yes; N = no; CA = can’t answer; NA = not applicable
* Systematic reviews with meta-analysis
Quality of evidence from primary studies in included reviews
The majority of primary articles were retrospective studies with only one randomized controlled trial (Table 2). While Canellas et al[30] did not report on quality assessment of their included primary studies, no uniform quality assessment tool was used to assess the quality of primary studies across the other five systematic reviews. Christovam et al[31] have applied the assessment criteria compiled by Mattos et al[18] with a different scoring system that they have developed on their own (Table 4).
Table 4. Quality assessment for primary studies of included systematic reviews.
| QUALITY ASSESSMENT | SYSTEMATIC REVIEWS | |||||
|---|---|---|---|---|---|---|
| Al-Moraissi et al[29] | Canellas et al[30] | Fernandez-Ferrer et al[32] | He et al[27] | Christovam et al[31] | Mattos et al[18] | |
| Assessment method* | Self-developed criteria to assess risk of bias (based on MOOSE, STROBE and PRISMA) | Not reported |
CONSORT criteria | MINORS criteria | Risk of bias based on quality assessment method reported by Mattos et al[18] | Self-compiled criteria for quality of methodological soundness (mostly based on CONSORT statement) |
| Assessment criteria | 1. Random selection in population 2. Definition of inclusion and exclusion criteria 3. Report of losses to follow-up 4. Validated measurements 5. Statistical analysis |
- | Not reported | 12 items (details not reported) | 1. Eligible criteria for participants described 2. Presence of control group 3. Blinding assessment stated 4. Statistical treatment performed 5. Reliability of measures tested 6. Reporting drop-outs 7. Follow-up period reported 8. Potential bias and trial limitations addressed |
|
| Scoring method | Low risk (included all criteria), moderate risk (did not include one of the criteria), high risk (two /> criteria were missing) | - | Not reported | Low risk of bias (19–24); Moderate risk (13–18); High risk (0–12) | Low risk of bias (≥4.5); Moderate risk (>2 and <4.5); High risk (≤2) | High quality (>6 points); Moderate quality (4–6 points); Low quality (<4 points) |
| Results | 1 low risk; 7 moderate risk | - | 11 moderate quality; 3 high quality | 8 low risk; 10 moderate risk | 6 low risk; 7 moderate risk; | 11 moderate quality |
| Remark | - | - | Refer to text in discussion | - | High risk paper was excluded from the review | Low quality studies were excluded from the review. |
* MOOSE: Meta-Analysis of Observational Studies in Epidemiology Statement; STROBE: Strengthening the Reporting of Observational Studies in Epidemiology statement; PRISMA: Preferred Reporting items for Systematic Reviews and Meta-Analyses; CONSORT: Consolidated Standards of Reporting Trials; MINORS: Methodological Index for Non-Randomized Studies
Not all primary studies have been analyzed quantitatively in the four included meta-analyses[18, 27, 29, 31]. Hence, this section only evaluated primary studies that have been included and analyzed in those systematic reviews. Out of the 64 included primary studies being assessed, 18 were rated with a high quality or low risk of bias, while others were rated with moderate quality or risk of bias.
Airway changes in linear measurements
1. Nasopharyngeal (NP) airway
Al-Moraissi et al[29] did not find any significant differences (p = 0.72) in the antero-posterior (AP) dimension of post-surgical NP airways when comparing two-jaw versus single-jaw mandibular setback surgeries, using random-effects modeling in their meta-analysis (I2 = 78%); MD = 0.11mm [95% CI -0.49, 0.71]; 264 patients in five studies (172 double-jaw; 90 single jaw).
2. Oropharyngeal (OP) airway
Mattos et al[18] performed multiple meta-analyses to evaluate post-surgical OP airway changes based on different measurement locations after mandibular setback with or without concomitant maxillary osteotomies (Table 5). All results showed significantly reduced post-surgical AP dimension, except for the measurement from the posterior nasal spine to the pharyngeal wall that increased significantly (p<0.00001).
Table 5. Anteroposterior (AP) changes of OP airway at multiple measurement locations (based on meta-analyses results reported by Mattos et al[18]).
| Meta-analyses | Measurement location | Type of surgery | Number of primary studies | Number of patients | Result |
|---|---|---|---|---|---|
| (AP dimension of OP airway) | |||||
| 1 | PNS-pharyngeal wall | Maxillary advancement + mandibular setback | 3 | 62 | Significant increase (p<0.00001). MD = 3.81mm [95% CI 2.46, 5.16], I2: 0%, |
| 2 | Soft palate-pharyngeal wall | Mandibular setback | 5 | 142 | Significant decrease (p<0.00001). MD = -2.57mm [95% CI -3.3, -1.85], I2 = 50% |
| Maxillary advancement + mandibular setback | 6 | 159 | Significant decrease (p = 0.01). MD = -0.91mm [95%CI -1.62, -0.20], I2 = 69% | ||
| 3 | Base of tongue-pharyngeal wall | Mandibular setback | 7 | 190 | Significant decrease (p<0.00001). MD = -2.99mm [95% CI -3.67, -2.31], I2 = 35% |
| Maxillary advancement + mandibular setback | 2 | 43 | Significant decrease (p<0.00001). MD = -2.83mm [95%CI -3.98, -1.68], I2 = 0% | ||
| 4 | Vellacula-pharyngeal wall | Maxillary advancement + mandibular setback | 3 | 63 | Significant decrease (p<0.0001). MD = -2.20mm [95% CI -3.23, -1.18], I2 = 0% |
PNS = posterior nasal spine
Another meta-analysis[29] of five studies compared two-jaw (maxillary advancement and mandibular setback osteotomies) versus mandibular setback surgeries in 253 patients (152 two-jaw; 101 one-jaw). A highly significant difference in the post-surgical AP dimension was found favoring two-jaw over one-jaw surgeries (p<0.00001) in OP airways; MD = 3.04mm [95%CI2.76, 3.32], I2 = 48%.
3. AP measurement at minimal pharyngeal airway space
One meta-analysis[18] analyzing mandibular setback combined with maxillary advancement osteotomies discovered no significant changes related to the post-surgical minimal pharyngeal airway space (p = 0.72); MD = 0.27mm [96% CI -1.19, 1.72], I2 = 0%, 2 studies, 63 patients.
4. Lateral width of the oropharyngeal (OP) airways
A significantly decreased (p = 0.01) lateral width of OP airways at the level of the tongue base was detected after mandibular setback osteotomies; MD = -2.37mm [95% CI -4.23, -0.51], I2 = 0%, 2 studies, 54 patients.[18]
5. Bilateral sagittal split osteotomy (BSSO) versus vertical subsigmoid osteotomies (VSSO)
In a total of 69 patients (42 BSSO, 27 VSSO), two studies (1 randomized controlled trial, 1 retrospective study) investigated the effects of two different setback procedures on anteroposterior OP airway dimension by means of cephalometric analysis. The meta-analysis disclosed a highly significant (p = 0.006) narrower post-surgical OP airways after VSSO compared to BSSO; MD = 1.29mm [95% CI 0.37, 2.22], I2 = 0%.[29]
Cross-sectional airway changes
1. Nasopharyngeal (NP) airway
Al-Moraissi et al[29] pooled the results from three studies with an overall of 109 dentoskeletal class III patients (64 two-jaw, 45 single-jaw osteotomies) and compared the cross-sectional plane changes associated with each procedure. They concluded that maxillary advancement combined with mandibular setback osteotomies provide more favorable results than mandibular setback only (p = 0.0004); MD = 0.76mm2 [95% CI 0.34, 1.18].
This result was supported by another meta-analysis[27] of four studies (54 two-jaw, 63 single-jaw osteotomies) that also favored two-jaw over one-jaw surgeries (p = 0.002); MD = -0.59mm2 [95% CI -0.97, -0.22]; I2 = 0%.
2. Oropharyngeal (OP) airway
Al-Moraissi et al[29] further analyzed quantitatively cross-sectional plane changes of OP airways comparing two-jaw versus mandibular setback surgeries. Data evaluation from three studies comprising 109 patients (64 two-jaw, 45 single-jaw) revealed two-jaw surgeries result in more favorable post-surgical cross-sectional dimension (p = 0.01), MD = 1.37mm2 [95% CI 0.27, 2.46]; I2 = 82%. However, regional analysis at the level of soft palate have shown no significant difference between one- versus two-jaw surgery (p = 0.05) in six studies (107 two-jaw; 98 one-jaw); MD = -0.28mm2 [95% CI -0.57, 0.00]; I2 = 0%.[27].
Other regional meta-analyses of two-jaw surgeries have discovered no significant difference upon comparison of pre- and post-surgical OP airways at the level of soft palate (p = 0.59), MD = -10.73mm2 [95% CI -49.53, 28.07]; I2 = 0%, and tongue base (p = 0.36), MD = -16.88mm2 [95% CI -53.21, 19.44]; I2 = 0%.[18] The same authors[18], however, disclosed a highly significant (p = 0.004) reduction of post-surgical cross-sectional plane at the level of the tongue base after isolated mandibular setback osteotomies, MD = -46.23mm2 [95%CI -77.51, -14.96]; I2 = 0%.
3. Hypopharyngeal (HP) airway
One meta-analysis[29] investigated differences in HP airway changes after one- versus two-jaw surgeries in dentoskeletal class III patients. Based on one cephalometric and one CBCT studies, MD = 3.04mm2 [95% CI -2.15, 8.23], I2 = 97%, no significant difference (p = 0.25) between both procedures related to post-surgical cross-sectional HP airway changes was disclosed.
On the contrary, He et al[27] reported a highly significant result at the level of the epiglottis plane in post-surgical cross-sectional area favoring two-jaw over one-jaw surgeries (p = 0.002) in 6 studies (107 two-jaw, 98 one-jaw); MD = -0.46mm2 [95% CI -0.75, -0.17], I2 = 0%.
4. Regional minimum cross sectional area (CSAmin)
At the retro-palatal level, a significant increase of CSAmin was found after both two-jaw (118.63mm2) and one-jaw (23.03mm2) surgeries[31]. Meanwhile, two-jaw surgeries were also found to significantly increase the CSAmin (94.84mm2) at the retrolingual level.[31]
Volumetric airway changes
Total volumetric changes have been assessed in two meta-analyses[27, 31]. Christovam et al[31] reported a significant decrease of the total airway volume after mandibular setback osteotomies (*p = 0.00, mean = -1894.67mm3, six studies, 106 patients), as well as after combined maxillary advancement and mandibular setback osteotomies (*p = 0.00, mean = -1552.91mm3, 11 studies, 187 patients). However, no significant difference could be found when comparing one- versus two-jaw surgeries (p = 0.067, 3 studies, 97 patients, 54 single-jaw surgery, 43 double-jaw surgery).[31]
In contrast, He et al[27] have indicated that two-jaw surgeries are more favorable than one-jaw surgeries (p = 0.002) after assessing the post-surgical changes of total pharyngeal airway volume in four studies (75 two-jaw, 62 one-jaw); MD = -3.41ml, 95% CI -5.59, -1.29; I2 = 0%. However, their detailed analyses of regional volumetric changes indicated that the significant result favoring two-jaw surgeries only occurred at the level of NP (p<0.0001), but not at the level of OP (p = 0.08) or HP (p = 0.64)[27].
* An exact p-value was not revealed in the article.
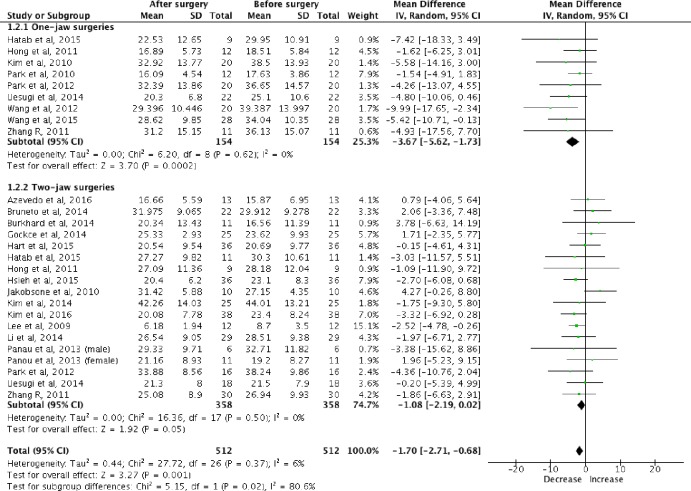
A meta-analysis was performed combining the primary studies of these two systematic reviews[27, 31] assessing the post-surgical total volumetric changes for pharyngeal airways, in one-jaw and two-jaw surgeries (Fig 2). Mandibular setback surgeries were found to significantly reduce (p = 0.0002) the post-surgical total pharyngeal airway volume (mean = -3.67ml, nine studies, 154 patients). On the contrary, no significant difference (p = 0.05) was detected in total pharyngeal airway volume after mandibular setback with maxillary advancement surgeries.
Fig 2. Total volumetric changes of pharyngeal airway after mandibular setback (one-jaw) and mandibular setback with maxillary advancement (two-jaw) surgeries.
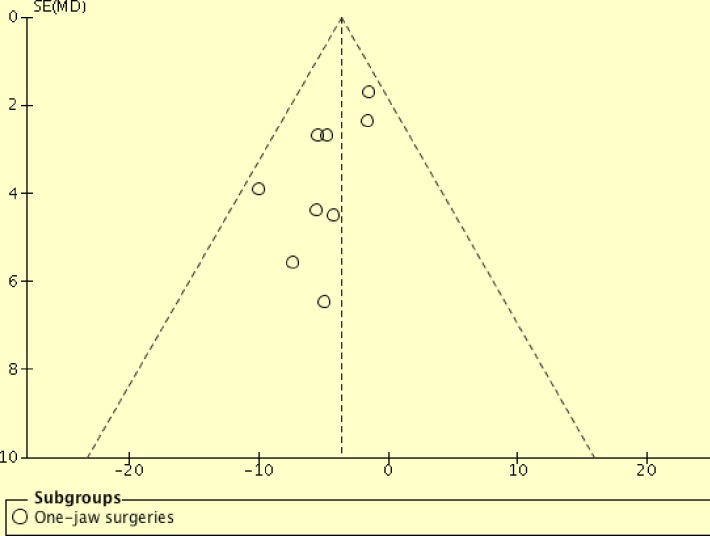
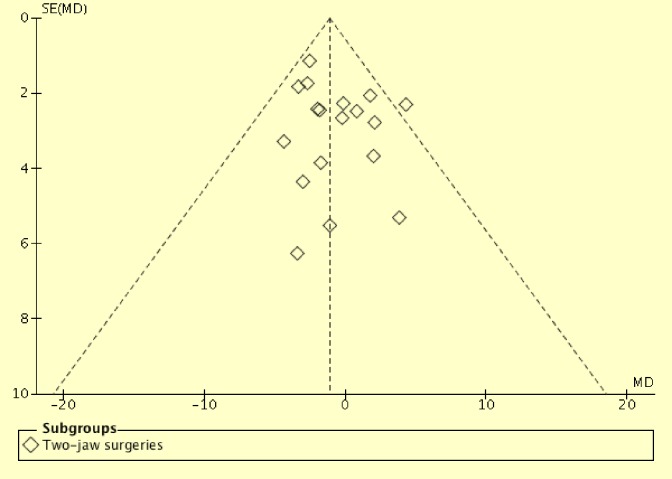
Additionally, one-jaw surgeries were found to reduce post-surgical total pharyngeal airway volume significantly (p = 0.02) compared to two-jaw surgeries (154 one-jaw; 358 two-jaw). This one-jaw versus two-jaw comparison has involved a much larger sample size (512 patients) compared with Christovam et al[31] (97 patients) and He et al[27] (137 patients). Assessments with funnel plots were performed (Figs 3 and 4). Asymmetric funnel plot was found for mandibular setback surgeries (Fig 3). However, Egger regression test was not performed, as tests for funnel plot asymmetry were not recommended when there are fewer than 10 studies in the analysis[26]. This asymmetry might be resulted from reporting bias, poor methodology quality in smaller studies, true heterogeneity, artifactual or by chance[26]. Future meta-analyses should investigate the cause for the funnel plot asymmetry when more primary studies are available.
Fig 3. Funnel plot for primary studies of mandibular setback surgeries.
Fig 4. Funnel plot for primary studies of mandibular setback with maxillary advancement surgeries.
Respiratory outcome measures
Both Canellas et al[30] and Fernandez-Ferrer et al[32] did not perform statistical meta-analyses in their systematic reviews. The former[30] included nine studies (232 patients) investigating the respiratory parameters in relation to one- or two-jaw surgeries.[30] Only seven patients showed an increased Apnea-Hypopnea Index (AHI) and Oxygen Desaturation Index (ODI) post-surgically, while no respiratory parameter deterioration was found among the others.[30] Both significant AHI and ODI findings after two-jaw surgeries were reported in the same primary study[41].
Canellas et al[30] have also detected significant but contradicting results of arterial oxygen saturation (SpO2) in two single-jaw surgery studies: one[8] with significantly reduced, the other[17] with significantly increased values. Meanwhile, Fernandez-Ferrer et al[32] detected that no post-surgical SpO2 reduction or AHI changes persisted in the long term.
Obstructive sleep apnea (OSA)
Canellas et al[30] reported that two out of 232 patients have developed post-surgical mild OSA. Both cases occurred after large mandibular setback movements of 13.7mm (single-jaw surgery) and 12.6mm (double-jaw surgery), respectively measured from the pogonion[30]. There were two systematic reviews[30, 32] screened the literature for respiratory parameters. Both concluded that 1) no evidence to confirm OSA development after mandibular setback[30, 32] or two-jaw[32] osteotomies within the first six months after surgery[30] and 2) respiratory changes do not persist in the long term[32].
Discussion
Impact of mandibular setback osteotomies on pharyngeal airways
Most primary studies of the included systematic reviews assessed pharyngeal airway changes by means of 2-D cephalometric analyses. As this technique allows only linear measurements, it cannot accurately assess 3-dimensional pharyngeal airway changes. Another significant limitation inherent to most studies was a lack of information about the head and neck posture and the tongue position during imaging[18]. Though RCTs stand for the highest level of evidence among clinical studies, under many circumstances it is neither ethical nor practical to perform RCTs to study various elective orthognathic techniques and their effect on airway changes. Therefore, prospective clinical studies with 3-D imaging and a defined long-term follow-up might probably represent the most appropriate future study design for this research topic.
Reports about nasopharyngeal (NP) airway changes after mandibular setback osteotomies are rare. While no significant difference was noted upon comparison of 1-jaw versus 2-jaw surgeries in AP dimension[29], interestingly 2-jaw surgery was found to generate more favorable outcomes in both cross-sectional[27, 29] and volumetric[27] analyses. It might be hypothesized that the maxillary advancement in 2-jaw surgeries possibly compensates the effect of the mandibular setback at nasopharynx.
More reports were found related to oropharyngeal (OP) airway changes associated with mandibular setback osteotomies. Generally, it was accepted that mandibular setback with or without concomitant maxillary osteotomies can lead to significantly reduced OP airway in AP dimension. An unusual AP increase of the OP airway at the level between posterior nasal spine and pharyngeal wall after two-jaw surgeries[18] probably represents the effect of concomitant maxillary advancement movement. Regional analyses[18, 27, 29] have shown more complex results indicating that post-surgical OP changes were not uniform, but differed depending on the level of measurements. Taking into account the various anatomical measurement points and methods of different authors, current results are subject to critical review.
Results of 3-D volumetric pharyngeal airway analyses seem to underlie interpretations that are more complicated. The overall pharyngeal airway volume was decreased both after 1- and 2-jaw surgeries.[31] While 1-D and 2-D analyses[29] have shown that two-jaw surgeries produced more favorable post-surgical effects on OP airways than 1-jaw surgeries, 3-D analyses of previous meta-analyses[27, 31] have reported contradictory results. However, the meta-analysis of this overview with larger sample size has supported the result of He et al[27] that 1-jaw surgeries resulted in a significantly reduced total pharyngeal volume in compared to 2-jaw surgeries. Again, regional analyses[27] have shown that both surgeries have different effects on the pharyngeal airways depending on the particular measurement location. Surprisingly one systematic review[31] has reported a reduction of the retro-palatal volume with an increased retro-lingual volume after 2-jaw surgeries. Even though those findings might be explained due to the novel anatomical positioning of hard and soft tissues, they are somewhat unexpected warranting further investigations, probably best in combination with dynamic airway flow measurements. 2-D and/or 3-D imaging techniques only provide static analyses of post-surgical hard and soft tissue positions and relations. The true physiological impact of new anatomical hard and soft tissue positions and their impact on dynamic airflow aspects still require in depth investigations and evaluations.
VSSO setback osteotomies resulted in significantly reduced OP airways in AP dimension compared to BSSO[29]. Posterior rotation of the mandible after releasing the mandibulo-maxillary fixation (MMF) after VSSO and post-surgical relapse in BSSO might explain this finding.[29]
Although mandibular setback osteotomies reduce OP airways to certain degree, the included reviews[30, 32] did not provide evidence that OSA develops post-surgically. Although reports of mild OSA after mandibular setback osteotomies are rare[30], nevertheless, these reports suggested that it might occur. Therefore it must not be disregarded completely as a potential adverse event after orthognathic setback osteotomies. Two-jaw surgeries should be taken into serious consideration during the treatment planning, especially in cases with severe mandibular prognathism or patients with predisposing factors for OSA[6, 7, 29, 30].
Although various articles have studied the effect of mandibular setback osteotomies on pharyngeal airways, it is difficult to find a common denominator to compare those results across the studies due to different measurement locations, methods and definitions[18, 31, 32]. For example, Al-Moraissi et al[29] have categorized the cross-sectional measurement of a primary study [7] in their meta-analysis at the level of soft palate (level at the most superior anterior point of the second cervical spine parallel to the Sella-Nasion line) under nasopaharyngeal (NP) group. Besides, this meta-analysis[29] has also categorized measurement at the level of posterior nasal spine (PNS) of another primary study[9] under NP. The result of this analysis should be interpreted with caution, as PNS is commonly used as the inferior border of NP and superior border of OP and therefore difficult to justify the usage of PNS to represent NP airways. Obtaining a generally accepted consensus about the most accurate and suitable pharyngeal airway measurement locations might lead to more consistent and comparable results across the studies, and ultimately to more valid evidence in the future. Christovam et al[31] have suggested that future studies should focus on a minimum CSP as it is not inferred by regional mean values.
None of the included reviews[18, 29–32] studied any gender related post-surgical pharyngeal airway changes, even though a few of their included primary studies displayed statements about gender related differences. While some[42, 43] could not find any gender related differences at all, others did[15, 44]. A recommendation to perform gender related subgroup analyses in the future might be taken into consideration. The maximum follow-up periods of primary studies vary but many were too short to demonstrate the eventual pharyngeal airway changes after mandibular setback surgery. This could have provided a false negative result on the incidence of post-surgical OSA. Long-term follow-up of at least 2 years post-surgically might be suitable to take into account relapse tendencies after orthognathic surgery.
It would be interesting to study effects of various simultaneous orthognathic procedures on pharyngeal airways. Concomitant orthognathic procedures such as genioplasty and maxillary impaction and their post-surgical impact on pharyngeal airways have not yet been reported adequately in primary studies. Furthermore, mandibular setback techniques (e.g. VSSO or BSSO), the extent of jaw setback movements, the patients’ BMI and the pre-existing history of snoring or other OSAS features are often neglected in patient assessments. The surgeons could then apply such additional clinical information to develop a holistic patient management. Moreover, unreported pre-surgical information of these potential clinical confounders might lead to errors in the interpretation of final treatment outcomes.
Christovan et al[31] have reported that two groups of authors that each has potentially duplicated their results in two different papers[45–48]. This finding was not able to be confirmed as the authors were not accessible[31]. It is very important to identify possible duplicate results during systematic reviews or meta-analyses, as otherwise the false negative or positive results might be reported. On the other hand, the reporting bias is equally important and can yield the same effect to the result of a review too. Although an asymmetry funnel plot was detected in this overview, no asymmetry test for publication bias was performed to prevent misleading the readers about false positive or negative publication bias[25].
Quality assurance in systematic reviews
The AMSTAR[24] assessment revealed a high methodology quality in only half of the here included systematic reviews. In addition to self-declaration, systematic reviews also need to indicate funding or supportive sources for each of their primary papers; this item of the checklist was not fulfilled in any of the included systematic reviews. Besides, only He et al[27] and Mattos et al[18] have discussed the publication bias of their included primary studies, albeit the latter have failed to present a funnel plot in their article.
Language bias might represent another potential study design flaw. Any language restriction might lead to overlook of well suitable studies written in other languages, resulting in a restricted number of articles and analyzed data. Three of the here included systematic reviews[18, 29, 30] limited their search to English literature only, while others[27, 31, 32] did not mention anything about it. Besides, only one review[18] presented a reference list for both included and excluded articles. Others[27, 29–32] referenced only their included articles, another common study flaw of systematic reviews that prevents their reproducibility.
The quality of included primary studies affects directly the quality of each systematic review. Therefore, it is mandatory to assess the quality and/or risk of bias of all included primary studies. One systematic review[30] omitted the evaluation of both issues, most likely because of using the PRISMA Equity 2012[49] instead of the standard PRISMA[23] checklist. The former[49] should only be applied in systematic reviews focusing on health equity, which, however, is not applicable for this topic. Therefore, conclusions of that article should be considered with care. Others [32] have claimed that they have used the CONSORT 2010[50] guideline to assess their included twelve retro- and two prospective primary studies qualitatively. However, they did not provide any explanation on how the included studies were classified into low, medium and high quality. The CONSORT 2010[50] checklist was exclusively developed to evaluate the quality of clinical randomized controlled trials (RCT), hence, it has to be considered less appropriate for non-RCT primary studies. Applying inappropriate assessment tools in systematic reviews might further confuse the readers related to the quality of included primary studies. For example, one retrospective primary study[51] was classified with a moderate quality, even though 1) the number of cases for each procedure, 2) the follow-up period, and 3) the demographic details of patients, like gender and age were not reported.
Among the here presented systematic reviews, no standardized quality assessment tool was used. While the Cochrane Risk of Bias Tool is well-known for RCTs, so far, none has been established for non-RCTs. Inconsistent nomenclature for non-randomized studies, and taxonomies used for differently defined, but similar study designs[52] may further bedazzle researchers in their attempts to classify non-randomized trials. Subsequently, this confusion may complicate the selection of the most appropriate assessment tool. Some researchers[52, 53] have performed comprehensive searches and analyzed quality assessment tools for non-randomized clinical studies or tools that can be used to assess more than one study design. Their recommendations e.g. the Methodological Index for Nonrandomized Studies (MINORS) tool and Thomas tool might be considered useful for future systematic reviews.
The frequently applied GRADE guideline[54] was not used in the here presented overview, as it was developed to address questions related to alternative management strategies, interventions, or policies, but not for questions related to risk or prognosis[54].
Conclusion
Mandibular setback osteotomies cause reduced pharyngeal airway dimensions. Although it has been reported sporadically, evidence that confirms the development of post-surgical OSA was not found. Nevertheless, this potential post-surgical hazard should be taken into serious consideration during the treatment planning of particular orthognathic cases. As moderate evidence exists that double-jaw surgeries may have lesser effect on post-surgical pharyngeal airways, they should be taken into consideration as the method of choice especially in cases with severe dentoskeletal Class III deformities.
Supporting information
(PDF)
(PDF)
(PDF)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This review was supported by the General Research Fund through the Research Grants Council of Hong Kong SAR (project number: HKU 17121915). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of manuscript. The first author is partly funded by this grant to support her PhD study.
References
- 1.Guilleminault C, Riley R, Powell N. Sleep apnea in normal subjects following mandibular osteotomy with retrusion. Chest. 1985;88(5):776–8. Epub 1985/11/01. . [DOI] [PubMed] [Google Scholar]
- 2.Riley RW, Powell NB, Guilleminault C, Ware W. Obstructive sleep apnea syndrome following surgery for mandibular prognathism. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 1987;45(5):450–2. Epub 1987/05/01. . [DOI] [PubMed] [Google Scholar]
- 3.Abdelrahman TE, Takahashi K, Tamura K, Nakao K, Hassanein KM, Alsuity A, et al. Impact of different surgery modalities to correct class III jaw deformities on the pharyngeal airway space. The Journal of craniofacial surgery. 2011;22(5):1598–601. doi: 10.1097/SCS.0b013e31822e5fc2 . [DOI] [PubMed] [Google Scholar]
- 4.Aydemir H, Memikoglu U, Karasu H. Pharyngeal airway space, hyoid bone position and head posture after orthognathic surgery in Class III patients. The Angle orthodontist. 2012;82(6):993–1000. Epub 2012/04/17. doi: 10.2319/091911-597.1 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cakarne D, Urtane I, A. S. pharyngeal airway sagittal dimension in patients with class III skeletal dentofacial deformity before and after bimaxillary surgery Stomatologija. 2003;5:13–6. [Google Scholar]
- 6.Chen F, Terada K, Hua Y, Saito I. Effects of bimaxillary surgery and mandibular setback surgery on pharyngeal airway measurements in patients with Class III skeletal deformities. American journal of orthodontics and dentofacial orthopedics: official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics. 2007;131(3):372–7. Epub 2007/03/10. doi: 10.1016/j.ajodo.2005.06.028 . [DOI] [PubMed] [Google Scholar]
- 7.Degerliyurt K, Ueki K, Hashiba Y, Marukawa K, Nakagawa K, Yamamoto E. A comparative CT evaluation of pharyngeal airway changes in class III patients receiving bimaxillary surgery or mandibular setback surgery. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics. 2008;105(4):495–502. Epub 2008/03/11. doi: 10.1016/j.tripleo.2007.11.012 . [DOI] [PubMed] [Google Scholar]
- 8.Gokce SM, Gorgulu S, Gokce HS, Bengi O, Sabuncuoglu F, Ozgen F, et al. Changes in posterior airway space, pulmonary function and sleep quality, following bimaxillary orthognathic surgery. International journal of oral and maxillofacial surgery. 2012;41(7):820–9. doi: 10.1016/j.ijom.2012.01.003 . [DOI] [PubMed] [Google Scholar]
- 9.Hong JS, Park YH, Kim YJ, Hong SM, Oh KM. Three-dimensional changes in pharyngeal airway in skeletal class III patients undergoing orthognathic surgery. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 2011;69(11):e401–8. Epub 2011/05/17. doi: 10.1016/j.joms.2011.02.011 . [DOI] [PubMed] [Google Scholar]
- 10.Hwang S, Chung CJ, Choi YJ, Huh JK, Kim KH. Changes of hyoid, tongue and pharyngeal airway after mandibular setback surgery by intraoral vertical ramus osteotomy. The Angle orthodontist. 2010;80(2):302–8. Epub 2009/11/13. doi: 10.2319/040209-188.1 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jakobsone G, Neimane L, Krumina G. Two- and three-dimensional evaluation of the upper airway after bimaxillary correction of Class III malocclusion. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics. 2010;110(2):234–42. Epub 2010/06/29. doi: 10.1016/j.tripleo.2010.03.026 . [DOI] [PubMed] [Google Scholar]
- 12.Kitahara T, Hoshino Y, Maruyama K, In E, Takahashi I. Changes in the pharyngeal airway space and hyoid bone position after mandibular setback surgery for skeletal Class III jaw deformity in Japanese women. American journal of orthodontics and dentofacial orthopedics: official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics. 2010;138(6):708e1-10; discussion -9. Epub 2010/12/07. doi: 10.1016/j.ajodo.2010.06.014 . [DOI] [PubMed] [Google Scholar]
- 13.Kobayashi T, Funayama A, Hasebe D, Kato Y, Yoshizawa M, Saito C. Changes in overnight arterial oxygen saturation after mandibular setback. The British journal of oral & maxillofacial surgery. 2013;51(4):312–8. Epub 2012/08/03. doi: 10.1016/j.bjoms.2012.07.004 . [DOI] [PubMed] [Google Scholar]
- 14.Park JW, Kim NK, Kim JW, Kim MJ, Chang YI. Volumetric, planar, and linear analyses of pharyngeal airway change on computed tomography and cephalometry after mandibular setback surgery. American journal of orthodontics and dentofacial orthopedics: official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics. 2010;138(3):292–9. Epub 2010/09/08. doi: 10.1016/j.ajodo.2009.10.036 . [DOI] [PubMed] [Google Scholar]
- 15.Samman N, Tang SS, Xia J. Cephalometric study of the upper airway in surgically corrected class III skeletal deformity. The International journal of adult orthodontics and orthognathic surgery. 2002;17(3):180–90. Epub 2002/10/02. . [PubMed] [Google Scholar]
- 16.Uesugi T, Kobayashi T, Hasebe D, Tanaka R, Ike M, Saito C. Effects of orthognathic surgery on pharyngeal airway and respiratory function during sleep in patients with mandibular prognathism. International journal of oral and maxillofacial surgery. 2014;43(9):1082–90. Epub 2014/07/17. doi: 10.1016/j.ijom.2014.06.010 . [DOI] [PubMed] [Google Scholar]
- 17.Yamada T, Mishima K, Matsumura T, Moritani N, T S. Respiratory status during sleep following orthognathic mandibular setback surgery. Asian J Oral Maxillofac Surg. 2008;20:12–5. [Google Scholar]
- 18.Mattos CT, Vilani GNL, Sant'Anna EF, Ruellas ACO, Maia LC. Effects of orthognathic surgery on oropharyngeal airway: A meta-analysis. International Journal of Oral and Maxillofacial Surgery. 2011;40(12):1347–56. doi: 10.1016/j.ijom.2011.06.020 . [DOI] [PubMed] [Google Scholar]
- 19.Rosario HD, Oliveira GM, Freires IA, de Souza Matos F, Paranhos LR. Efficiency of bimaxillary advancement surgery in increasing the volume of the upper airways: a systematic review of observational studies and meta-analysis. European archives of oto-rhino-laryngology: official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS): affiliated with the German Society for Oto-Rhino-Laryngology—Head and Neck Surgery. 2016. Epub 2016/03/31. doi: 10.1007/s00405-016-4015-4 . [DOI] [PubMed] [Google Scholar]
- 20.Hochban W, Schurmann R, Brandenburg U, Conradt R. Mandibular setback for surgical correction of mandibular hyperplasia—does it provoke sleep-related breathing disorders? Int J Oral Maxillofac Surg. 1996;25(5):333–8. Epub 1996/10/01. . [DOI] [PubMed] [Google Scholar]
- 21.Becker L.A OAD. Overviews of reviews In: Higgins J.P.T. GS, editor. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011] ed: The Cochrane Collaboration; 2011. [Google Scholar]
- 22.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS medicine. 2009;6(7):e1000100 Epub 2009/07/22. doi: 10.1371/journal.pmed.1000100 ; PubMed Central PMCID: PMCPMC2707010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open medicine: a peer-reviewed, independent, open-access journal. 2009;3(3):e123–30. Epub 2009/01/01. ; PubMed Central PMCID: PMCPMC3090117. [PMC free article] [PubMed] [Google Scholar]
- 24.Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10 Epub 2007/02/17. doi: 10.1186/1471-2288-7-10 ; PubMed Central PMCID: PMCPMC1810543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ioannidis JP, Trikalinos TA. The appropriateness of asymmetry tests for publication bias in meta-analyses: a large survey. CMAJ: Canadian Medical Association journal = journal de l'Association medicale canadienne. 2007;176(8):1091–6. Epub 2007/04/11. doi: 10.1503/cmaj.060410 ; PubMed Central PMCID: PMCPMC1839799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ (Clinical research ed). 2011;343:d4002 Epub 2011/07/26. doi: 10.1136/bmj.d4002 . [DOI] [PubMed] [Google Scholar]
- 27.He J, Wang Y, Hu H, Liao Q, Zhang W, Xiang X, et al. Impact on the upper airway space of different types of orthognathic surgery for the correction of skeletal class III malocclusion: A systematic review and meta-analysis. International journal of surgery (London, England). 2017;38:31–40. Epub 2016/12/29. doi: 10.1016/j.ijsu.2016.12.033 . [DOI] [PubMed] [Google Scholar]
- 28.He JL, Wang YJ, Hu HT, Liao Q, Zhang WY, Fan XP. Meta-analysis of the effects of different orthognathic surgeries on the upper airway of patients with skeletal class III malocclusion. [Chinese]. Journal of Shanghai Jiaotong University (Medical Science). 2016;36(10):1467–72 and 77. . [Google Scholar]
- 29.Al-Moraissi EA, Al-Magaleh SM, Iskandar RA, Al-Hendi EA. Impact on the pharyngeal airway space of different orthognathic procedures for the prognathic mandible. International journal of oral and maxillofacial surgery. 2015;44(9):1110–8. Epub 2015/05/31. doi: 10.1016/j.ijom.2015.05.006 . [DOI] [PubMed] [Google Scholar]
- 30.Canellas JV, Barros HL, Medeiros PJ, Ritto FG. Sleep-disordered breathing following mandibular setback: a systematic review of the literature. Sleep & breathing = Schlaf & Atmung. 2016;20(1):387–94. Epub 2015/10/16. doi: 10.1007/s11325-015-1274-z . [DOI] [PubMed] [Google Scholar]
- 31.Christovam IO, Lisboa CO, Ferreira D, Cury-Saramago AA, Mattos CT. Upper airway dimensions in patients undergoing orthognathic surgery: a systematic review and meta-analysis. International Journal of Oral and Maxillofacial Surgery. 2016;45(4):460–71. doi: 10.1016/j.ijom.2015.10.018 [DOI] [PubMed] [Google Scholar]
- 32.Fernandez-Ferrer L, Montiel-Company JM, Pinho T, Almerich-Silla JM, Bellot-Arcis C. Effects of mandibular setback surgery on upper airway dimensions and their influence on obstructive sleep apnoea—a systematic review. Journal of cranio-maxillo-facial surgery: official publication of the European Association for Cranio-Maxillo-Facial Surgery. 2015;43(2):248–53. doi: 10.1016/j.jcms.2014.11.017 . [DOI] [PubMed] [Google Scholar]
- 33.Tan SK, Leung WK, Tang ATH, Zwahlen RA. Letter to the editor on the article article “Impact on the upper airway space of different types of orthognathic surgery for the correction of skeletal class III malocclusion: A systematic review and meta-analysis”. International Journal of Surgery. doi: 10.1016/j.ijsu.2017.03.083 [DOI] [PubMed] [Google Scholar]
- 34.Gurani SF, Di Carlo G, Cattaneo PM, Thorn JJ, Pinholt EM. Effect of Head and Tongue Posture on the Pharyngeal Airway Dimensions and Morphology in Three-Dimensional Imaging: a Systematic Review. Journal of oral & maxillofacial research. 2016;7(1):e1 Epub 2016/04/22. doi: 10.5037/jomr.2016.7101 ; PubMed Central PMCID: PMCPMC4837605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guijarro-Martinez R, Hernandez-Alfaro F, Swennen G, Mareque-Bueno J. Upper airway evaluation using cone-beam computerized tomography (CBCT): Systematic review and results after mono and bimaxillary advancement. International Journal of Oral and Maxillofacial Surgery. 2011;40 (10):e12 . [Google Scholar]
- 36.Indriksone I, Jakobsone G. The upper airway dimensions in different sagittal craniofacial patterns: a systematic review. Stomatologija / issued by public institution "Odontologijos studija" [et al]. 2014;16(3):109–17. . [PubMed] [Google Scholar]
- 37.Guijarro-Martinez R, Swennen GR. Cone-beam computerized tomography imaging and analysis of the upper airway: a systematic review of the literature. Int J Oral Maxillofac Surg. 2011;40(11):1227–37. Epub 2011/07/19. doi: 10.1016/j.ijom.2011.06.017 . [DOI] [PubMed] [Google Scholar]
- 38.Borba AM, Borges AH, Ce PS, Venturi BA, Naclerio-Homem MG, Miloro M. Mandible-first sequence in bimaxillary orthognathic surgery: A systematic review. International Journal of Oral and Maxillofacial Surgery. 2016;45(4):472–5. doi: 10.1016/j.ijom.2015.10.008 . [DOI] [PubMed] [Google Scholar]
- 39.Huang CS, Hsu SS, Chen YR. Systematic review of the surgery-first approach in orthognathic surgery. Biomed J. 2014;37(4):184–90. Epub 2014/08/15. doi: 10.4103/2319-4170.126863 . [DOI] [PubMed] [Google Scholar]
- 40.Lye KW. Effect of orthognathic surgery on the posterior airway space (PAS). Annals of the Academy of Medicine, Singapore. 2008;37(8):677–82. . [PubMed] [Google Scholar]
- 41.Foltan R, Hoffmannova J, Pavlikova G, Hanzelka T, Klima K, Horka E, et al. The influence of orthognathic surgery on ventilation during sleep. International journal of oral and maxillofacial surgery. 2011;40(2):146–9. doi: 10.1016/j.ijom.2010.10.006 . [DOI] [PubMed] [Google Scholar]
- 42.Degerliyurt K, Ueki K, Hashiba Y, Marukawa K, Simsek B, Okabe K, et al. The effect of mandibular setback or two-jaws surgery on pharyngeal airway among different genders. Int J Oral Maxillofac Surg. 2009;38(6):647–52. Epub 2009/02/24. doi: 10.1016/j.ijom.2009.01.010 . [DOI] [PubMed] [Google Scholar]
- 43.Kim NR, Kim YI, Park SB, DS H. Three dimensional cone-beam CT study of upper airway change after mandibular setback surgery for skeletal class III malocclusion patients. Korean J Orthod. 2010;40:145–55. [Google Scholar]
- 44.Nakagawa F, Ono T, Ishiwata Y, Kuroda T. Morphologic changes in the upper airway structure following surgical correction of mandibular prognathism. The International journal of adult orthodontics and orthognathic surgery. 1998;13(4):299–306. Epub 1999/04/10. . [PubMed] [Google Scholar]
- 45.Kim MA, Kim BR, Choi JY, Youn JK, Kim YJ, Park YH. Three-dimensional changes of the hyoid bone and airway volumes related to its relationship with horizontal anatomic planes after bimaxillary surgery in skeletal Class III patients. The Angle orthodontist. 2013;83(4):623–9. Epub 2013/01/15. doi: 10.2319/083112-700.1 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim MA, Kim BR, Youn JK, Kim YJ, Park YH. Head posture and pharyngeal airway volume changes after bimaxillary surgery for mandibular prognathism. Journal of cranio-maxillo-facial surgery: official publication of the European Association for Cranio-Maxillo-Facial Surgery. 2014;42(5):531–5. doi: 10.1016/j.jcms.2013.07.022 . [DOI] [PubMed] [Google Scholar]
- 47.Wang H, Qi S, Wang J, Cai Z, Li C. [Detection to changes in hyoid and tongue positions, and pharyngeal airway following mandibular setback surgery by cone beam CT]. Hua Xi Kou Qiang Yi Xue Za Zhi. 2012;30(6):650–4. Epub 2013/01/22. . [PubMed] [Google Scholar]
- 48.Wang HW, Wang JG, Qi SQ, Cai ZF, Li XH. [Three-dimensional analysis of pharyngeal airway in skeletal Class III patients after sagittal split ramus osteotomy]. Zhonghua kou qiang yi xue za zhi = Zhonghua kouqiang yixue zazhi = Chinese journal of stomatology. 2012;47(4):221–4. Epub 2012/07/18. doi: 10.3760/cma.j.issn.1002-0098.2012.04.007 . [DOI] [PubMed] [Google Scholar]
- 49.Welch V, Petticrew M, Tugwell P, Moher D, J ON, E W, et al. PRISMA-Equity 2012 Extension: Reporting Guidelines for Systematic Reviews with a Focus on Health Equity. PLoS medicine. 2012;9:e1001333 doi: 10.1371/journal.pmed.1001333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC medicine. 2010;8:18 Epub 2010/03/26. doi: 10.1186/1741-7015-8-18 ; PubMed Central PMCID: PMCPMC2860339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Demetriades N, Chang DJ, Laskarides C, Papageorge M. Effects of mandibular retropositioning, with or without maxillary advancement, on the oro-naso-pharyngeal airway and development of sleep-related breathing disorders. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 2010;68(10):2431–6. doi: 10.1016/j.joms.2010.02.033 . [DOI] [PubMed] [Google Scholar]
- 52.Deeks JJ, Dinnes J, D'Amico R, Sowden AJ, Sakarovitch C, Song F, et al. Evaluating non-randomised intervention studies. Health technology assessment (Winchester, England). 2003;7(27):iii-x, 1–173. Epub 2003/09/23. . [DOI] [PubMed] [Google Scholar]
- 53.Zeng X, Zhang Y, Kwong JS, Zhang C, Li S, Sun F, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. Journal of evidence-based medicine. 2015;8(1):2–10. Epub 2015/01/17. doi: 10.1111/jebm.12141 . [DOI] [PubMed] [Google Scholar]
- 54.Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. Journal of clinical epidemiology. 2011;64(4):383–94. Epub 2011/01/05. doi: 10.1016/j.jclinepi.2010.04.026 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.