Abstract
Purpose of review
In the last decade, video-assisted thoracoscopic surgery (VATS) has become a popular method in diagnosis and treatment of acute chest injuries. Except for patients with unstable vital signs who require larger surgical incisions to check bleeding, this endoscopic surgery could be employed in the majority of thoracic injury patients with stable vital signs.
Recent findings
In the past, VATS was used to evacuate traumatic-retained hemothorax. Recent study has revealed further that lung repair during VATS could decrease complications after trauma. Management of fractured ribs could also be assisted by VATS. Early VATS intervention within 7 days after injury can decrease the rate of posttraumatic infection and length of hospital stay. In studies of the pathophysiology of animal models, N-acetylcysteine and methylene blue were used in animals with blunt chest trauma and found to improve clinical outcomes.
Summary
Retained hemothorax derived from blunt chest trauma should be managed carefully and rapidly. Early VATS intervention is a well tolerated and reliable procedure that can be applied to manage this complication cost effectively.
Keywords: blunt chest trauma, retained hemothorax, video-assisted thoracoscopic surgery
INTRODUCTION
Blunt chest trauma accounts for more than 15% of injuries in trauma patients worldwide [1,2]. Falls and traffic accidents are the most frequent causes of trauma. Patients usually experience a large amount of energy transmitted to the entire chest cavity during the injury. After blunt chest injuries, patients may have chest wall destruction and lung parenchyma injuries [3,4▪,5]. Further severe injury to intrathoracic organs can also be found, such as intrathoracic vascular injury, diaphragm rupture, and esophageal injury [6,7]. Moreover, all these injuries may cause hemothorax or pneumothorax, the most common complication that can occur immediately after blunt chest trauma [8].
Appropriate management of blunt chest trauma depends on a patient's vital signs [1]. A tube thoracostomy and emergent thoracotomy are typically performed to control bleeding in patients with hypovolemic shock [9,10]. When patient vital signs are stabilized, the next step is treating posttraumatic complications. Owing to the advances in endoscopic instruments and technology, minimally invasive surgery is widely applied to manage chest trauma [1,11]. The purpose of this review is to understand the complications caused by retained hemothorax and the benefits of minimally invasive surgery for patients experiencing blunt chest trauma. What follows is a summary of our current knowledge of video-assisted thoracoscopic surgery (VATS) used in retained hemothorax of blunt chest trauma.
Box 1.
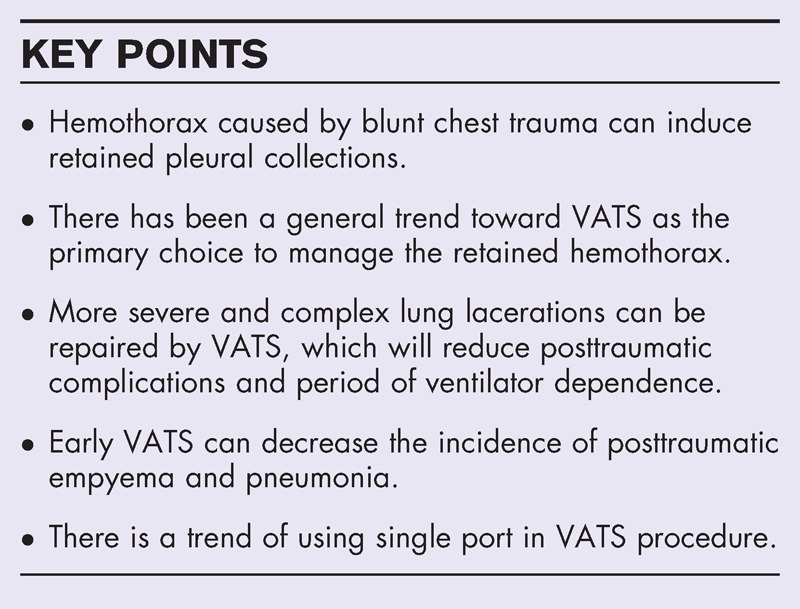
no caption available
HEMOTHORAX AND RETAINED HEMOTHORAX
As early in 1998, Carrillo and Richardson [1] found that hemothorax typically progresses in three manners: complete spontaneous reabsorption of blood within several weeks, progression to fibrothorax, or infection with empyema formation. Adequate drainage is the primary treatment for hemothorax and pneumothorax, and the first choice for drainage is placing a thoracostomy chest tube into the pleural cavity. When adequate pain control and intravenous volume resuscitation are applied, nearly 85% of patients can be treated successfully [1,11]. Although providing a tube thoracostomy is sufficient for treating the majority of hemodynamically stable patients, small amounts of residual blood might accumulate in the pleural cavity after this procedure. These bloody effusions are occasionally entirely resorbed after 4–6 weeks without causing infection [1]. However, patients may experience retained hemothorax because of malposition or poor drainage of chest tubes [12]. According to a study by Richardson et al., retained hemothorax is defined as residual clots at least 500 ml large, or in which at least one-third of the blood in the pleural space cannot be drained by a chest tube after 72 h of initial treatment revealed by a computed tomography (CT) scan [1,11]. The percentage of retained clotted hemothorax varies in numerous research studies; incidence rates from 5 to 30% have been reported. Several studies have suggested that once the volume of retained hemothorax accumulates to 300 ml, surgical intervention should be considered [13▪▪,14,15▪].
DIAGNOSIS OF RETAINED HEMOTHORAX
Retained hemothorax typically occurs at least 24 h after a tube thoracostomy. A sudden decrease of drainage volume indicates that the chest tube is poorly functioning. Serial chest roentgenograms are typically required to detect retained hemothorax. However, to estimate the exact volume of thoracic collections, chest film is unsuitable because volume cannot be accurately defined and is usually underestimated [16,17▪]. Furthermore, it also cannot differentiate lung contusions and pneumonia from hemothorax. Chest CT now is an effective tool for evaluating chest trauma because it can clearly display anatomic structures [16,17▪]. CT scans can also detect lung parenchyma injuries and the exact volume of retained collections. However, the disadvantages of CT scans are patient exposure to high levels of radiation and higher costs compared with chest roentgenograms [18]. When a chest CT scan is performed on patients to detect additional injuries after the chest radiograph has been found to be normal, the scans do not change how patients are treated [17▪,19]. Particularly in asymptomatic pediatric patients, routine use of CT scans is not recommended for unknown causes of blunt trauma injury [20]. Chest sonography, another option for detecting and estimating the volume of retained hemothorax, can provide rapid and accurate diagnosis of traumatic thoracic injuries, such as lung contusions and pleural collections [21,22]. However, similar to a chest radiograph, ultrasonography is ineffective for diagnosing mediastinal hematoma, which can be easily detected by a CT scan [23].
TREATMENT FOR RETAINED HEMOTHORAX
Managing retained hemothorax is one of the most critical treatments for blunt chest trauma. In a study by Ramanathan et al.[24], initial removal of traumatic hemothoraces by using a sterile suction catheter was an effective and relatively simple intervention technique that reduced the possibility of retained hemothorax. Although these retained hemothoraces may be spontaneously reabsorbed 4–6 weeks after trauma, excessive retained hemothorax may lead to additional complications. First, the hemothorax collapses the lung parenchyma. Accompanied by lung contusions and posttraumatic pneumonia, the collapse can produce an entrapped lung and cause acute respiratory failure in the initial phases [24]. Then, fibrothorax may develop in later phases, further reducing pulmonary function. Second, when the hemothorax is contaminated with microbials, empyema may occur. The empyema increases the incidence of respiratory failure and sepsis, both of which increase the length of hospital stay and patient morbidity and mortality. Bradley et al.[25▪▪] also found that an elevated injury severity score, blunt thoracic trauma, and failure to administer periprocedural antibiotics during tube thoracostomy placement were independent risk factors for empyema [25▪▪]. Appropriate surgical management and specific antibiotic therapy should be arranged to ensure improved clinical outcomes [26].
In the past, the primary method for treating retained hemothorax was to perform an additional tube thoracostomy or exploratory thoracotomy. However, the additional chest tubes might be positioned improperly, resulting in inadequate drainage and prolonging the hospital stay [1,16]. Although an exploratory thoracotomy may afford a clear view for locating lesions, this procedure is more invasive. A thoracotomy can be performed by cutting through the muscle of the chest wall and expanding the wound by using a rib expander. These surgical procedures cause further destruction to an injured chest wall and may increase morbidity and mortality [1,11]. Since the 1990s, because of the advance in techniques and instruments of VATS, VATS is now widely accepted by most trauma surgeons [15▪]. VATS can provide excellent visualization of the pleural cavity that is more useful for evacuating the hemothorax than using additional tube thoracostomies. The wounds caused by VATS are much smaller than those caused by a thoracotomy. Therefore, this procedure may prevent further injury to the chest wall. In a study by Schweigert et al.[14], this procedure was shown to be suitable for use in elderly patients. The main functions of VATS include evaluation and control of continued bleeding, early evacuation of a retained hemothorax, evacuation and decortication of posttraumatic empyemas, limited invasive treatment of suspected diaphragmatic injuries, treatment of persistent air leaks, and evaluation of mediastinal injuries. On account of smaller incisions, the cosmetic results are more acceptable. VATS is now used as an alternative method to thoracotomy in selected patients [1] and is typically used in patients with stable vital signs. However, open thoracotomy is still performed on patients experiencing hemorrhagic shock.
SURGICAL METHOD
The detailed method for performing VATS was proposed by Carillo and Richardson in 1998 [1]. To obtain a clearer view of the pleural cavity, double-lumen intubation is effective for collapsing the ipsilateral lung. A patient is placed in the full lateral position, with the ipsilateral arm abducted 90° at the shoulder; this position is identical to that used during a standard thoracotomy. If VATS fails, alternatively performing an open thoracotomy can be easy.
Standard thoracoscopic equipment includes a thoracoscope with a 0° or 30° angle and a xenon light source, as well as two high-resolution video monitors that are located at both sides of the surgical table. Thoracoports are used to position the video camera and surgical instruments. The patient would have usually received tube thoracostomy during initial diagnosis. The thoracoscope can be passed through this wound after the chest tube is removed. According to the suggestion by Carillo, one or two additional incisions can be created; the locations of these extra incisions are determined after an initial inspection of the chest cavity is performed [1,11].
After insertion of the thoracoscope, the adhesions should be released by blunt digital dissection or sharp endoscopic electrocoagulated dissection. Full lung collapse is crucial for inspecting the entire pleural cavity. Blood and clots are removed by using a standard suction instrument or a suction–irrigator system. A sample of fluid is routinely collected for microbiologic assessment [1,11]. In patients with organized thoracic collections, carefully dissecting and peeling away the outer layer with sponge sticks and ring forceps typically enables the outer layer to be removed from the visceral and parietal pleurae, thus completely releasing the trapped lung [1,11]. After completion of this procedure, one or two large-bore chest tubes are placed through the thoracoport incisions. The chest tubes enable continual suction until no evidence of an air leak is present or until the amount of drainage from the thoracic cavity is less than 100 ml/d [1,11].
Because the quality of the endoscopic instruments has improved, incisions created during VATS can be further diminished [27]. After a single incision of 2–3 cm on the lateral chest is made, a specially designed single flexible port is placed through the incision. A 5-mm 0° video thoracoscope, a reticulating grasper, and an Endo-GIA (Covidien, Mansfield, Massachusetts, USA) stapler are introduced through the port channels [28,29]. The advantage of uniport VATS is that only one incision is required.
In the current study, only removing blood clot was occasionally insufficient [13▪▪]. Lung laceration is easily detected in blunt chest injuries. In certain instances, this laceration may produce continual oozing that causes retained hemothorax to accumulate. The edges of a lacerated lung can also undergo necrosis. These necrotic lung tissues are ideal culture media that enable bacterial growth and increase the risk of infection. Therefore, in addition to facilitating removal of retained pleural effusion, VATS also affords the opportunity to repair lung lacerations by using an autostapler. This method can be used to reduce infection rates and improve clinical outcomes [13▪▪]. Blunt chest trauma also typically coincides with ribs fractures. The sharp tip of a fractured rib may penetrate the lungs or other vital organs in the chest [30]. VATS can be applied to resect fractured ribs. In a study performed by Funaki et al.[31], a fractured rib tip was resected using VATS to prevent injury to the descending aorta. The fixation of fractured ribs is a controversial procedure; however, it may result in improved clinical outcomes [32].
TIMING OF VIDEO-ASSISTED THORACOSCOPIC SURGERY
The timing of surgical intervention to remove the retained hemothorax is another critical factor of outcome but is usually influenced by other associated injuries. Within 48–72 h after injury, blood clots can be removed easily through suction by VATS. However, 1 week after injury, adhesions between the visceral and parietal pleura form a tenacious inflammatory outer layer and envelop the lung, thereby increasing the possibility for postoperative complications, such as retained collections or air leaks [1]. Numerous reports have suggested that performing VATS earlier could prevent empyema and reduce the possibility of fibrothorax. Several studies have suggested that surgery should be performed within 3–10 days after the initial blunt chest trauma, and most studies suggest not delaying surgery for more than 10 days because the clotted blood may cause a pleural adhesion, hindering the performance of VATS. Performing VATS earlier may reduce short and long-term morbidity and mortality, operative blood loss, and incidences of fibrothorax and empyema [1]. In a study by Goodman et al.[33], VATS was shown to be well tolerated and effective in managing thoracic trauma in hemodynamically stable patients within the first 24 h after injury. Early performance of VATS also allows early re-expansion of the lung capacity that can restore lung function rapidly and improve clinical outcomes [34▪].
POSTOPERATIVE TREATMENT
Routine chest radiographs during follow-up are required daily. The volume of output from the chest tube and the color of effusions should also be recorded daily to ensure that no obstructions are present. In patients with multiple trauma, who are dependent on a ventilator and prolonged bed rest, the risk of venous thromboembolism may be increased [35]. Early use of noninvasive ventilation in patients with chest trauma (who do not show signs of respiratory distress) may prevent the need for intubation and reduce complications and the length of stay in the ICU [36]. In some patients with respiratory failure, positive ventilation is insufficient to support the lung. Extracorporeal membrane oxygenation may be an additional option [37–39]. Continuous lateral rotational bed therapy may help in preventing or treating respiratory complications in patients with multiple trauma [40]. However, rebleeding may occur. The bleeding site can be embolized with angiography [41]. Hemolytic agents, such as urokinase, have been used in the resolution of retained hemothorax, but the actual benefits remain controversial. Intrapleural tissue plasminogen activator has also been used and appears to be a well tolerated and effective treatment option [42▪▪].
Numerous animal studies have focused on the pathophysiology of blunt trauma and treatments [43]. In a study performed by Kaya et al.[43], blunt trauma was found to cause and prolong inflammatory responses [44]. In a study performed by Topcu-Tarladacalisir et al.[45], administrating N-acetylcysteine to patients after blunt chest trauma facilitated the regulation of oxidative stress and apoptosis. In another animal study, methylene blue was shown to be a beneficial therapeutic treatment for blunt chest trauma [46]. In addition, predictive prognosis factors of blunt chest trauma have been studied [2,47,48]; critical predictors for developing complications are age, chronic lung disease, use of preinjury anticoagulants, and oxygen saturation levels. However, using the number of rib fractures as a predictor of blunt chest trauma is controversial [49].
CONTRAINDICATION
VATS procedures require single-lung anesthesia, the preparation of which can be time consuming; therefore, the major contraindication to VATS for trauma is the presence of hemodynamic instability [1,11]. In patients experiencing thoracic injury with hypovolemic shock, a thoracotomy remains the most appropriate option. However, uncontrolled bleeding or hemodynamically unstable conditions may occur during VATS; therefore, changing the surgical procedure to a thoracotomy should be considered. An obliterated pleural cavity secondary to infection or from previous surgery, a history of bleeding diathesis, or moderate-to-severe obstructive pulmonary disease are also contraindicators for VATS.
COMPLICATIONS OF VIDEO-ASSISTED THORACOSCOPIC SURGERY
Most complications from VATS are related to the procedure itself. Incisional wound bleeding, instruments introduced into lung parenchyma, and wound infections are the most common post-VATS complications. The bleeding that occurs from incisional wounds can be managed by using tight sutures. Punctured lung parenchyma can be treated with an endoscopic autostapler. However, these complications are not severe and can be managed easily.
CONCLUSION
VATS is a well tolerated, reliable, and effective procedure that can be easily applied to manage retained hemothorax after a patient experiences blunt chest trauma with few complications. As an alternative procedure to a thoracotomy, VATS is only slightly more invasive than a tube thoracostomy. In addition to enabling efficient removal and inspection of clots, VATS can also be performed to repair lung lesions and manage rib fractures.
Acknowledgements
None.
Financial support and sponsorship
None.
Conflicts of interest
H.-L.L. was responsible for the conception and design of the study, interpretation of data, drafting, writing and final approval of the article; T.-C.W. was responsible for carrying out most of the clinical studies evaluating the patients and collection of data, and also participated in the drafting and final approval of the article; T.-C.W. and Y.-P.C. were responsible for the conception and design of the study, interpretation of the data, and drafting, writing, and final approval of the article; Y.-P.C. provided important contributions for intellectual content and participated in final approval of the article. The first two authors made equal contributions to this work.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Carrillo EH, Richardson JD. Thoracoscopy in the management of hemothorax and retained blood after trauma. Curr Opin Pulm Med 1998; 4:243–246. [DOI] [PubMed] [Google Scholar]
- 2.Battle C, Hutchings H, Lovett S, et al. Predicting outcomes after blunt chest wall trauma: development and external validation of a new prognostic model. Crit Care (London, England) 2014; 18:R98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Niesler U, Palmer A, Radermacher P, Huber-Lang MS. Role of alveolar macrophages in the inflammatory response after trauma. Shock (Augusta, GA) 2014; 42:3–10. [DOI] [PubMed] [Google Scholar]
- 4▪.Couret D, de Bourmont S, Prat N, et al. A pig model for blunt chest trauma: no pulmonary edema in the early phase. Am J Emerg Med 2013; 31:1220–1225. [DOI] [PubMed] [Google Scholar]; This is a prospective study in an animal model for blunt trauma mechanism. It represents that pulmonary edema does not occur rapidly at early phase of blunt chest trauma even in combination with a large area of lung contusion.
- 5.Khoriati AA, Rajakulasingam R, Shah R. Sternal fractures and their management. J Emerg Trauma Shock 2013; 6:113–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diaz-Miron JL, Dillon PA, Saini A, et al. Left main coronary artery dissection in pediatric sport-related chest trauma. J Emerg Med 2014; 47:150–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen SW, Huang YK, Liao CH, Wang SY. Right massive haemothorax as the presentation of blunt cardiac rupture: the pitfall of coexisting pericardial laceration. Interact Cardiovasc Thorac Surg 2014; 18:245–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ogawa F, Naito M, Iyoda A, Satoh Y. Report of a rare case: occult hemothorax due to blunt trauma without obvious injury to other organs. J Cardiothorac Surg 2013; 8:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nakajima H, Uwabe K, Asakura T, et al. Emergent surgical repair of left ventricular rupture after blunt chest trauma. Ann Thorac Surg 2014; 98:e35–e36. [DOI] [PubMed] [Google Scholar]
- 10.Dominguez KM, Ekeh AP, Tchorz KM, et al. Is routine tube thoracostomy necessary after prehospital needle decompression for tension pneumothorax? Am J Surg 2013; 205:329–332. [DOI] [PubMed] [Google Scholar]
- 11.Casos SR, Richardson JD. Role of thoracoscopy in acute management of chest injury. Curr Opin Crit Care 2006; 12:584–589. [DOI] [PubMed] [Google Scholar]
- 12.John M, Razi S, Sainathan S, Stavropoulos C. Is the trocar technique for tube thoracostomy safe in the current era? Interact Cardiovasc Thorac Surg 2014; 19:125–128. [DOI] [PubMed] [Google Scholar]
- 13▪▪.Chou YP, Kuo LC, Soo KM, et al. The role of repairing lung lacerations during video-assisted thoracoscopic surgery evacuations for retained haemothorax caused by blunt chest trauma. Eur J Cardiothorac Surg 2014; 46:107–111. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this article, the authors propose that repairing lung laceration during VATS in management for retained hemothorax can improve clinical outcomes.
- 14.Schweigert M, Beron M, Dubecz A, et al. Video-assisted thoracoscopic surgery for posttraumatic hemothorax in the very elderly. Thorac Cardiovasc Surg 2012; 60:474–479. [DOI] [PubMed] [Google Scholar]
- 15▪.Oosthuizen GV, Clarke DL, Laing GL, et al. Introducing video-assisted thoracoscopy for trauma into a South African township hospital. World J Surg 2013; 37:1652–1655. [DOI] [PubMed] [Google Scholar]; In this article, the authors suggest that VATS should be performed early instead of second chest drain for retained collections.
- 16.Chardoli M, Hasan-Ghaliaee T, Akbari H, Rahimi-Movaghar V. Accuracy of chest radiography versus chest computed tomography in hemodynamically stable patients with blunt chest trauma. Chin J Traumatol 2013; 16:351–354. [PubMed] [Google Scholar]
- 17▪.Kea B, Gamarallage R, Vairamuthu H, et al. What is the clinical significance of chest CT when the chest x-ray result is normal in patients with blunt trauma? Am J Emerg Med 2013; 31:1268–1273. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this article, the authors found that CT has higher advantage in diagnosis; however, it does not alter the clinical managment.
- 18.Hershkovitz Y, Zoarets I, Stepansky A, et al. Computed tomography is not justified in every pediatric blunt trauma patient with a suspicious mechanism of injury. Am J Emerg Med 2014; 32:697–699. [DOI] [PubMed] [Google Scholar]
- 19.Rodriguez RM, Baumann BM, Raja AS, et al. Diagnostic yields, charges, and radiation dose of chest imaging in blunt trauma evaluations. Acad Emerg Med 2014; 21:644–650. [DOI] [PubMed] [Google Scholar]
- 20.Holscher CM, Faulk LW, Moore EE, et al. Chest computed tomography imaging for blunt pediatric trauma: not worth the radiation risk. J Surg Res 2013; 184:352–357. [DOI] [PubMed] [Google Scholar]
- 21.Leblanc D, Bouvet C, Degiovanni F, et al. Early lung ultrasonography predicts the occurrence of acute respiratory distress syndrome in blunt trauma patients. Intensive Care Med 2014; 40:1468–1474. [DOI] [PubMed] [Google Scholar]
- 22.Brun PM, Bessereau J, Levy D, et al. Prehospital ultrasound thoracic examination to improve decision making, triage, and care in blunt trauma. Am J Emerg Med 2014; 32:817.e1–817.e2. [DOI] [PubMed] [Google Scholar]
- 23.Hsu LW, Chong CF, Wang TL, Wu BH. Traumatic mediastinal hematoma: a potentially fatal condition that may be overlooked by traditional focused assessment with sonography for trauma. Am J Emerg Med 2013; 31:262.e1–262.e3. [DOI] [PubMed] [Google Scholar]
- 24.Ramanathan R, Wolfe LG, Duane TM. Initial suction evacuation of traumatic hemothoraces: a novel approach to decreasing chest tube duration and complications. Am Surg 2012; 78:883–887. [PubMed] [Google Scholar]
- 25▪▪.Bradley M, Okoye O, DuBose J, et al. Risk factors for posttraumatic pneumonia in patients with retained haemothorax: results of a prospective, observational AAST study. Injury 2013; 44:1159–1164. [DOI] [PubMed] [Google Scholar]; A large study in identifying the independent predictors for posttraumatic pneumonia induced by retained hemothorax.
- 26.O’Connor JV, Chi A, Joshi M, et al. Posttraumatic empyema: aetiology, surgery and outcome in 125 consecutive patients. Injury 2013; 44:1153–1158. [DOI] [PubMed] [Google Scholar]
- 27.Wang C. Clinical research on the incision line selection of video-assisted thoracoscopic wedge resection of the lung. Surgeon 2014; 12:17–25. [DOI] [PubMed] [Google Scholar]
- 28.Bayarri CI, de Guevara AC, Martin-Ucar AE. Initial single-port thoracoscopy to reduce surgical trauma during open en bloc chest wall and pulmonary resection for locally invasive cancer. Interact Cardiovasc Thorac Surg 2013; 17:32–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berlanga LA, Gigirey O. Uniportal video-assisted thoracic surgery for primary spontaneous pneumothorax using a single-incision laparoscopic surgery port: a feasible and safe procedure. Surg Endosc 2011; 25:2044–2047. [DOI] [PubMed] [Google Scholar]
- 30.Morimoto Y, Sugimoto T, Sakahira H, et al. Successful management of threatened aortic rupture late after rib fracture caused by blunt chest trauma. Ann Vasc Surg 2014; 28:1035.e11–1035.e13. [DOI] [PubMed] [Google Scholar]
- 31.Funaki S, Inoue M, Minami M, Okumura M. Video-assisted thoracoscopic resection of fractured ribs to prevent descending aorta injury in patient with chest trauma. Ann Thorac Cardiovasc Surg 2014; 20:173–174. [DOI] [PubMed] [Google Scholar]
- 32.Doben AR, Eriksson EA, Denlinger CE, et al. Surgical rib fixation for flail chest deformity improves liberation from mechanical ventilation. J Crit Care 2014; 29:139–143. [DOI] [PubMed] [Google Scholar]
- 33.Goodman M, Lewis J, Guitron J, et al. Video-assisted thoracoscopic surgery for acute thoracic trauma. J Emerg Trauma Shock 2013; 6:106–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34▪.Lin HL, Huang WY, Yang C, et al. How early should VATS be performed for retained haemothorax in blunt chest trauma? Injury 2014; 45:1359–1364. [DOI] [PubMed] [Google Scholar]; One of large studies focused on the time for VATS. Early operation can improve clinical outcomes.
- 35.Kahn SA, Schubmehl H, Stassen NA, et al. Risk factors associated with venous thromboembolism in isolated blunt chest trauma. Am Surg 2013; 79:502–505. [PubMed] [Google Scholar]
- 36.Duggal A, Perez P, Golan E, et al. Safety and efficacy of noninvasive ventilation in patients with blunt chest trauma: a systematic review. Crit Care (London, England) 2013; 17:R142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tseng YH, Wu TI, Liu YC, et al. Venoarterial extracorporeal life support in posttraumatic shock and cardiac arrest: lessons learned. Scand J Trauma Resusc Emerg Med 2014; 22:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ballouhey Q, Fesseau R, Benouaich V, Leobon B. Benefits of extracorporeal membrane oxygenation for major blunt tracheobronchial trauma in the paediatric age group. Eur J Cardiothorac Surg 2013; 43:864–865. [DOI] [PubMed] [Google Scholar]
- 39.Ried M, Bein T, Philipp A, et al. Extracorporeal lung support in trauma patients with severe chest injury and acute lung failure: a 10-year institutional experience. Crit Care (London, England) 2013; 17:R110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wyen H, Wutzler S, Maegele M, et al. Rotational bed therapy after blunt chest trauma: a nationwide online-survey on current concepts of care in Germany. Injury 2013; 44:70–74. [DOI] [PubMed] [Google Scholar]
- 41.Nemoto C, Ikegami Y, Suzuki T, et al. Repeated embolization of intercostal arteries after blunt chest injury. Gen Thorac Cardiovasc Surg 2014; 62:696–699. [DOI] [PubMed] [Google Scholar]
- 42▪▪.Stiles PJ, Drake RM, Helmer SD, et al. Evaluation of chest tube administration of tissue plasminogen activator to treat retained hemothorax. Am J Surg 2014; 207:960–963. [DOI] [PubMed] [Google Scholar]; In this article, the authors propose nonsurgical treatment with tissue plasminogen activator for retained hemothorax.
- 43.Kaya H, Kafali ME, Aydin K, et al. Efficacy of aprotinin treatment on bilateral blunt chest trauma created in rabbits. J Pak Med Assoc 2013; 63:32–37. [PubMed] [Google Scholar]
- 44.Neunaber C, Oestern S, Andruszkow H, et al. Cytokine productive capacity of alveolar macrophages and Kupffer cells after femoral fracture and blunt chest trauma in a murine trauma model. Immunol Lett 2013; 152:159–166. [DOI] [PubMed] [Google Scholar]
- 45.Topcu-Tarladacalisir Y, Tarladacalisir T, Sapmaz-Metin M, et al. N-Acetylcysteine counteracts oxidative stress and protects alveolar epithelial cells from lung contusion-induced apoptosis in rats with blunt chest trauma. J Mol Histol 2014; 45:463–471. [DOI] [PubMed] [Google Scholar]
- 46.Ayvaz S, Aksu B, Karaca T, et al. Effects of methylene blue in acute lung injury induced by blunt chest trauma. Hippokratia 2014; 18:50–56. [PMC free article] [PubMed] [Google Scholar]
- 47.Battle C, Hutchings H, Bouamra O, Evans PA. The effect of preinjury antiplatelet therapy on the development of complications in isolated blunt chest wall trauma: a retrospective study. PloS One 2014; 9:e91284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Battle CE, Hutchings H, James K, Evans PA. The risk factors for the development of complications during the recovery phase following blunt chest wall trauma: a retrospective study. Injury 2013; 44:1171–1176. [DOI] [PubMed] [Google Scholar]
- 49.Whitson BA, McGonigal MD, Anderson CP, Dries DJ. Increasing numbers of rib fractures do not worsen outcome: an analysis of the national trauma data bank. Am Surg 2013; 79:140–150. [PubMed] [Google Scholar]


