Abstract
With CT (computed tomography) chest gaining more importance as a diagnostic tool, chest X-ray especially the lateral view is taken less commonly nowadays. Besides CT chest is also proven to be superior to chest X-ray in patients with major blunt trauma. We are presenting a 68-year old male who was partially treated from outside for a left sided pneumonia. He came to our hospital because of persisting chest pain. Chest X-ray, frontal view (postero-anterior) was almost normal except for a mild opacity in the left lower zone. CT scan of the chest revealed a fluid collection posteriorly enclosed within enhancing pleura. Chest X-ray, left lateral view showed a corresponding posterior pleural based opacity. We are presenting this case to highlight the importance of the lateral view of the chest X-ray. In selected cases there is still a role for the lateral view. With the three dimensional visualization provided by the CT, the lateral view of the chest may be easier to understand. Consequent to the initial diagnosis by CT further follow up can be done with the chest X-ray. In a limited way this mitigates unnecessary expenditure and more importantly prevents the patient from exposure to harmful radiation in the form of repeated CT.
Keywords: Chest X-ray, Lateral view, Computed tomography
1. Introduction
With CT (computed tomography) chest gaining more importance as a diagnostic tool, chest X-ray especially the lateral view is taken less commonly nowadays. An additional lateral view may not yield any more meaningful information than a frontal (postero-anterior) view. Besides CT chest is also proven to be superior to chest X-ray in patients with major blunt trauma. We are presenting a 68-year old male who presented to our hospital with history of fever, cough and left sided chest pain. He was partially treated from outside for a left sided pneumonia. He came to our hospital because of the persisting chest pain. Chest X-ray, frontal view (postero-anterior) was almost normal except for a mild opacity in the left lower zone. CT scan of the chest revealed a fluid collection posteriorly enclosed within enhancing pleura. Chest X-ray, left lateral view showed a corresponding posterior pleural based opacity. We are presenting this case to highlight the importance of the lateral view of the chest X-ray. In selected cases there is still a role for the lateral view. With the three dimensional visualization provided by the CT, the lateral view of the chest may be easier to understand. Consequent to the initial diagnosis by CT further follow up can be done with the chest X-ray. In a limited way this mitigates unnecessary expenditure and more importantly prevents the patient from exposure to harmful radiation in the form of repeated CT.
2. Case report
A 68-year old male presented to our hospital with nine day history of fever, cough and left sided chest pain. The illness started as fever with chills accompanied by cough with mild mucoid expectoration. The chest pain was localized to the left axillary and infra-scapular area; it was catching in nature and increased on inspiration. He was partially treated from outside for a left sided pneumonia. He came to our hospital because of the persisting chest pain.
His past medical history was only remarkable for fairly controlled diabetes. He was a chronic smoker and had stopped smoking only two months prior to this admission. He took alcohol only occasionally. His father had died due to carcinoma of the oropharynx and mother due to complications of chronic obstructive pulmonary disease. He was married and had two children. Both his wife and children were healthy.
On examination his pulse was 92 beats per minute, blood pressure was 140/90 mm of Hg and respiratory rate was 18 breaths per minute. He was afebrile at time of admission. On examination of the chest there were reduced movements in the left axillary and infrascapular areas; breath sounds were also decreased in the same areas. Rest of systemic examination was normal.
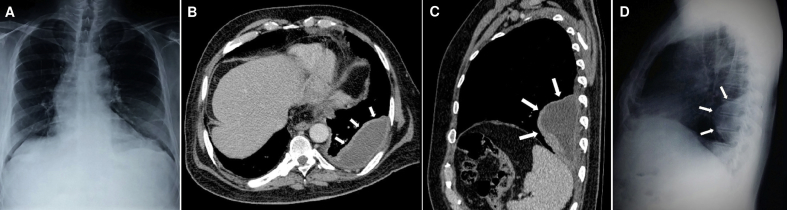
Among his lab results the total WBC count was elevated with neutrophilic leucocytosis and a raised ESR (WBC count: 11,300/mm3, neutrophils: 78%, lymphocytes: 12%, monocytes: 6%, eosinophils: 4% and ESR: 66/1st hour). Chest X-ray was almost normal except for mild opacity in the left lower zone (Fig. 1, A). Electrocardiogram showed a normal sinus rhythm with no significant ST - segment changes. The remaining results from electrolyte panel, liver function tests, renal function tests and coagulation profile were normal. Testing for cardiac troponins was negative.
Fig. 1.
A). Chest X-ray with a mild opacity in the left lower zone. B) & C). CT scan of chest, axial view and sagittal view showing fluid collection posteriorly enclosed within enhancing pleura. D). Chest X-ray, left lateral view showing a corresponding posterior pleural based opacity, 10 × 5 cm projecting into the lung and and blunting of the posterior costo-phrenic recess.
After 6 days of treatment with antibiotics and other symptomatic measures patient's fever and cough subsided, but he continued to have chest pain. Repeat chest X-ray taken was identical to the first one. CT scan of the chest was now ordered. This was followed up with a chest X-ray, left lateral view.
CT scan of the chest revealed a fluid collection posteriorly enclosed within enhancing pleura (Fig. 1- B axial view, arrows and Fig. 1- C sagittal view, arrows). Chest X-ray, left lateral view showed a corresponding posterior pleural based opacity, 10 × 5 cm projecting into the lung and (Fig. 1- D, arrows), and blunting of the posterior costo-phrenic recess.
Patient was continued on antibiotics and anti-inflammatory drugs. A repeat chest X-ray taken 2 weeks after discharge showed almost complete resolution of the opacity (Fig. 2, left lateral view). The patient had also become asymptomatic.
Fig. 2.
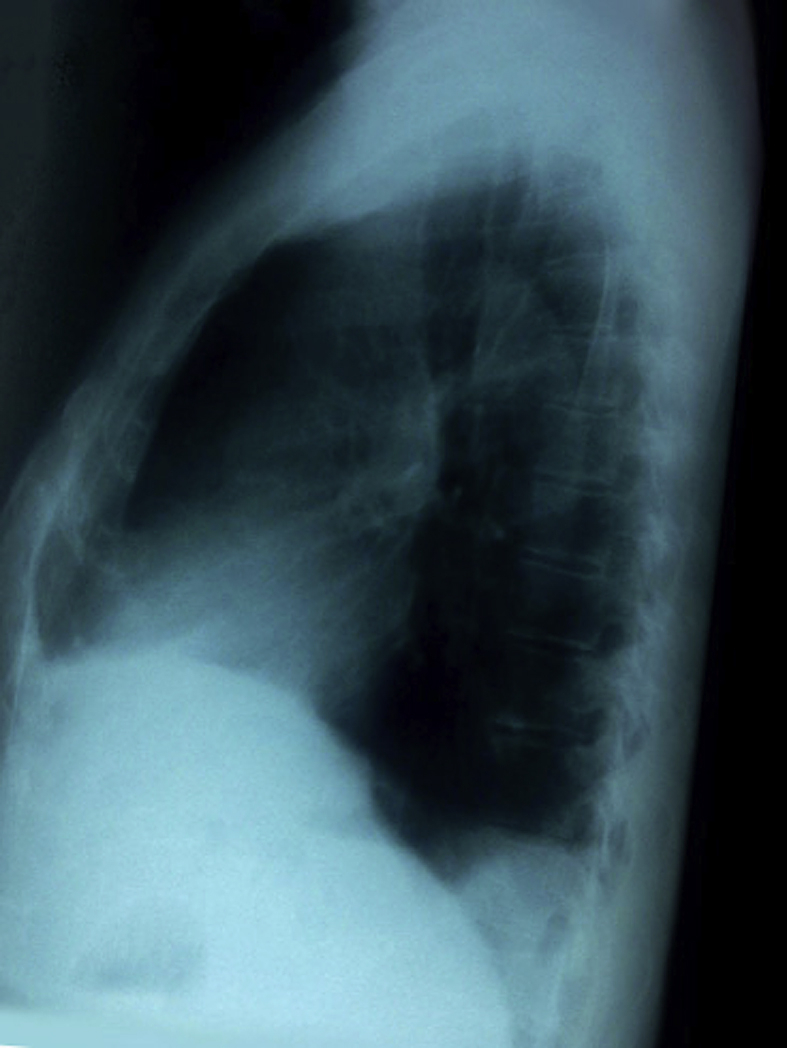
Chest X-ray, left lateral view showing almost complete resolution of the opacity.
3. Discussion
With the emergence of CT chest as a diagnostic modality, chest X-ray especially the lateral view is taken less frequently nowadays. A lateral chest X-ray taken additional to the postero-anterior view may not improve the sensitivity or specificity of detection of conditions like pneumonia [1]. Lateral view of the thorax on the chest X-ray also does not give any additional benefit in detecting small pulmonary nodules [2]. CT chest is also proven to be superior to chest X-ray in patients with major blunt trauma [3], [4].
But advances in imaging technology come at a price; there is the mounting burden of incidental findings on the CT [5]. In some cases they open an opportunity to cure an otherwise fatal disease. In most cases the consequences are however negative; they create unnecessary anxiety and work-up for lesions which turn out to be benign and unlikely to affect the life expectancy of the patient [5].
Increased use of CT also exposes the patient to harmful radiation. By its nature, CT involves larger radiation doses than the more common, conventional x-ray imaging procedures [6]. The main factor that determines the effects of radiation in a tissue or organ is the absorbed dose. Absorbed radiation dose is the energy deposited in the tissue by the radiation beam passing through it and risks associated with radiation exposure are largely determined by this absorbed radiation dose [7].
Taking into account the increasing concern over radiation exposure, the best way to minimize this would simply be to limit the number of CT scans that are prescribed. A radiologist centric approach could be another method. A radiologist recommendation for chest CT to evaluate an abnormal finding on a chest X-ray has been proven to have a higher yield of clinically relevant findings [8].
In selected cases (for example this case) there is still a role for the lateral view of the chest radiograph. With the three dimensional visualization provided by CT as was done in this case, the lateral radiograph of the chest may be easier to understand. But the role of the CT should be likened to a ‘first line of defense’. Consequent to the diagnosis further follow up can be done with the chest radiograph. In a limited way this mitigates unnecessary expenditure and more importantly prevents the patient from exposure to harmful radiation in the form of repeated CT.
4. Summary
Though CT chest has become more popular in recent decades, it is not without dangers. Unnecessary exposure to radiation in the form of avoidable and repeated CT scans is a health hazard not to mention the cost and the presence of incidental findings which create untoward anxiety and concern in the mind of the patient and physician alike. Frontal view (postero-anterior) of the chest by X-ray is a simple yet proven diagnostic modality. Also there may still be a role for chest X-ray, lateral view in selected cases. In this era of ‘investigative medicine’ medical professionals especially the younger generation need to reacquaint themselves of this time tested tool in clinical medicine.
Source of support
There was no source of support.
Presentation at a meeting
This case report was not presented at any meeting.
Conflicting interest
There is none.
Contributor Information
Abraham M. Ittyachen, Email: abyliz@rediffmail.com.
Anuroopa Vijayan, Email: dranuroopamanovihar@gmail.com.
Megha Isac, Email: meghaisac@ymail.com.
References
- 1.Lynch T., Gouin S., Larson C., Patenaude Y. Does the lateral chest radiograph help pediatric emergency physicians diagnose pneumonia? A randomized clinical trial. Acad. Emerg. Med. 2004;11(6):625–629. [PubMed] [Google Scholar]
- 2.Kluthke R.A., Kickuth R., Bansmann P.M., Tüshaus C., Adams S., Liermann D., Kirchner J. The additional value of the lateral chest radiograph for the detection of small pulmonary nodules-a ROC analysis. Br. J. Radiol. 2016;89:20160394. doi: 10.1259/bjr.20160394. Epub 2016 Sep. 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Traub M., Stevenson M., McEvoy S., Briggs G., Lo S.K., Leibman S., Joseph T. The use of chest computed tomography versus chest X-ray in patients with major blunt trauma. Injury. 2007;38(1):43–47. doi: 10.1016/j.injury.2006.07.006. Epub 2006 Oct 11. [DOI] [PubMed] [Google Scholar]
- 4.Hoffstetter P., Dornia C., Schäfer S., Wagner M., Dendl L.M., Stroszczynski C., Schreyer A.G. Diagnostic significance of rib series in minor thorax trauma compared to plain chest film and computed tomography. J. Trauma Manag. Outcomes. 2014;8:10. doi: 10.1186/1752-2897-8-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ding A., Eisenberg J.D., Pandharipande P.V. The economic burden of incidentally detected findings. Radiol. Clin. North Am. 2011;49:257–265. doi: 10.1016/j.rcl.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brenner D.J., Hall E.J. Computed tomography–an increasing source of radiation exposure. N. Engl. J. Med. 2007;357(22):2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 7.Kalra M.K., Maher M.M., Rizzo S., Kanarek D., Shepard J.A. Radiation exposure from chest CT: issues and strategies. J. Korean Med. Sci. 2004;19(2):159–166. doi: 10.3346/jkms.2004.19.2.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harvey H.B., Gilman M.D., Wu C.C., Cushing M.S., Halpern E.F., Zhao J., Pandharipande P.V., Shepard J.A., Alkasab T.K. Diagnostic yield of recommendations for chest CT examination prompted by outpatient chest radiographic findings. Radiology. 2015;275(1):262–271. doi: 10.1148/radiol.14140583. [DOI] [PMC free article] [PubMed] [Google Scholar]