Abstract
Health care spending is generally highest among people who need both complex medical care and long-term services and supports, such as adults dually eligible for Medicare and Medicaid. Understanding how different types of complex patients use services over time can inform policies that target this population. High combined Medicare and Medicaid spending are found in two distinct groups of high-cost dual eligibles: older beneficiaries who are nearing the end of life, and younger beneficiaries with sustained need for functional supports. However, both groups have high hospitalization costs. Among high-cost dual eligibles living in the community, those who are older use home and community-based services less than those who are younger. Greater use of such services might provide stable support in the last year or two of life, when illness and functional decline accelerate. Tailored approaches to each population’s distinct needs could yield care of increased value to patients and their families, with the potential to lower costs if patients’ needs can be met with fewer stays in short-term inpatient facilities.
Rising budgetary concerns have intensified the pressure on publicly funded health care programs to reduce costs without compromising quality. The pressure has increased scrutiny on the 24 percent of the federal budget that goes toward health care.1–3 Medicare spending is highly concentrated in a small proportion of beneficiaries, for example in 2012 5 percent of Medicare beneficiaries account for 41 percent of spending in that program.4,5 And with similar concentrated spending in Medicaid, it is not surprising that high-cost patients have become a primary focus for interventions by payers, especially when these patients are dually enrolled in Medicare and Medicaid.6–8
Many dually eligible adults are high cost because they have serious health conditions that require complex medical services (such as physician and hospital care) and care to support functional independence (such as home aides, community services, and facility-based care when needed). While coordination of care is frequently lauded as a path to better management, translating that coordination into practice has been difficult. Care coordination is especially challenging when complex care requires payment from Medicare for medical (acute) services and from Medicaid for long-term services and supports.9–11 The most widespread new payment models, such as Medicare contracts with accountable care organizations and patient-centered medical homes, have primarily addressed Medicare utilization. But new programs, such as state participation in the Financial Alignment Intiative and Medicare Advantage Special Needs Plans of the Centers for Medicare and Medicaid Services (CMS), are integrating acute and long-term care payment and delivery systems.12–14 Understanding how different types of complex patients use services over time can lead to the optimization of service delivery and payment across Medicare and Medicaid.
The dually eligible population likely includes subpopulations with different reasons for high needs and spending. Many previous studies have focused on Medicare or Medicaid when describing who is likely to be high cost, identifying people with multiple chronic medical conditions,15–21 mental illness,22–25 and functional impairment or disabilities.16,17,19,26–29 A parallel literature discusses the high concentration of spending among people who are dying.30–32 Only a few studies have focused on identifying adults whose high service use spans both Medicare and Medicaid,9,13 but they focus on a snapshot in either Medicare or Medicaid, not both. Furthermore, these studies do not show how subgroups differ over time—which is important for program design. For example, older adults may have medical illness and functional loss toward the end of life that require intensive acute care and evolving need for supportive services as they approach death. Alternatively, younger disabled populations can have ongoing high need for long-term services and supports that extends into the foreseeable future.
Managing these different potential patterns of care requires markedly different approaches. Yet dual eligibles are often cast as a single group rather than a heterogeneous population that differs along important dimensions, such as age and nursing home residence. Understanding the very different patterns of service use across these subgroups may provide insights into how the integration of acute and long-term services and supports might be improved to better meet each subgroup’s distinct needs.
To understand patterns of service use and reliance on Medicare verus Medicaid programs over time for high-need dual eligibles, we examined dually eligible beneficiaries with high combined Medicare and Medicaid costs. We determined whether such beneficiaries with high annual cost in a baseline year had persistently high costs in the following year, reverted to a lower-cost group in the following year, or experienced high costs in the year leading up to death. We categorized differences in service use patterns by age and nursing home residence to gain insights into potential areas for improved integration of acute and long-term care for people with serious illnesses. Some of these patients may need shorter-term, palliative care, while others have ongoing need for long-term services and supports.
Study Data And Methods
We conducted an observational cohort study of dually eligible adults ages twenty-one and older who were in the top decile of combined Medicare and Medicaid spending in 2010, following them through 2011. We considered only dually eligible adults with full Medicaid eligibility which makes the eligible for long-term services and supports covered by Medicaid. We used enrollment and claims data for fee-for-service Medicare beneficiaries linked to their Medicaid personal summary file records. We identified dually eligible residents in the thirty-six states33 (and the District of Columbia) that had usable and complete Medicaid Analytic eXtract (MAX) data at the time of this study. States were excluded if data anomaly tables suggested that the utilization or spending data would be inaccurate.34
Beneficiary spending was determined by summing paid amounts in the Medicare files and Medicaid personal summary file. Because payment amounts are not standardized across states, we used the top decile in each state to identify high-cost beneficiaries. Thus, each state’s representation in the study sample was determined by the size of its dual-eligible population. We applied the same methodology to categorize high-cost beneficiaries in 2011. Then we assigned each high-cost beneficiary in 2010 to one of three mutually exclusive categories: persistently high cost (high cost in both 2010 and 2011), died in 2010 or 2011, and reverted to lower-cost in 2011. Service use and spending categories are as reported by Medicare (inpatient, outpatient professional services [from carrier file], hospice, home health, and durable medical equipment) and Medicaid (the same categories as Medicare when serving as the secondary payer, plus inpatient long-term care, home and community-based long-term services, targeted case management, and other wraparound services such as dental services and transportation).
Beneficiaries’ age, sex, race, dual-eligibility status, and date of death were obtained from Medicare enrollment files. People who spent more than a hundred days in a nursing home in 2010 based on Minimum Data Set records were categorized as being nursing home residents. Chronic conditions were identified by the presence of one inpatient or two outpatient claims at least seven days apart in Medicare files for a selected group of Hierarchical Condition Category (HCC) diagnoses that are high cost and chronic, and have at least 2 percent prevalence (for a list of included HCC categories, see online Appendix Table 1).35 We placed high-cost beneficiaries into age-residence categories (younger than sixty-five living in the community, younger than sixty-five in a nursing home, sixty-five and older in the community, and sixty-five and older in a nursing home) and described their characteristics, use of acute (Medicare reimbursed) and long-term services and supports (Medicaid reimbursed), and spending.
Analysis
We first described the differences across age-residence categories of high-cost dual eligibles and differences among high-cost beneficiaries according to their course over time (that is, whether they remained high cost in 2011, died in 2010 or 2011, or reverted to lower-cost in 2011). Our sample size was large enough that all of the differences we found in the descriptive comparisons were significant (p < 0.001). We then performed multinomial logistic regression to model the independent risk factors identifiable in 2010 (the base year) that were associated with whether a person remained high cost or died in 2011, relative to survivors who reverted to lower-cost in that year. This model included individual beneficiary characteristics (age, sex, race, nursing home residence, whether or not the person had three or more chronic conditions, and a flag for each condition) and an indicator for each state to adjust for potential differences in state program characteristics. From this model, we calculated the predicted probability of being persistently high cost or dying associated with age, given the mean characteristics of other variables in the model. To address potential limitations of the multinomial models, we estimated separate logistic models for each outcome. These generated similar predicted probabilities.
Limitations
Our findings should be viewed in light of several potential limitations. First, in a rapidly changing health care environment, it would be ideal to have more recent data. However, 2011 was the most recent year for which complete Medicaid MAX data for the thirty-six states and the District of Columbia were available.
Second, we could not include all states because some Medicaid programs had missing data, often the result of high managed care penetration. However, 55 percent of the US population of dual eligibles lived in the jurisdictions we studied.
Third, the services provided under each category of long-term services and supports (such as home care) can vary across states. Finally, we cannot say whether the use of outpatient services such as home and community-based services prevented the use of inpatient care, because the observational analysis did not allow us to to draw causal inferences.
Study Results
High-cost dual eligible beneficiaries spent an average of $135,343 in 2010 (Exhibit 1). Of this amount, $71,803 was paid by Medicare and $63,540 by Medicaid. High-cost dual eligibles were equally likely to be younger than sixty-five and residing in the community as to be sixty-five or older and living in a nursing home (35 percent for both groups). Twenty-two percent were ages sixty-five and older and living in the community, with only 8 percent being younger than sixty-five and residing in nursing homes. The two nursing home subgroups and community-dwelling people ages sixty-five and older had fairly similar disease profiles, with the exception of a high prevalence of severe mental illness (41 percent) and paralysis (16 percent) in nursing home residents younger than sixty-five and of dementia (71 percent) among older nursing home residents. The community-dwelling group younger than sixty-five had a markedly different chronic illness pattern, with much lower likelihood of having multiple chronic conditions. Only 33 percent of the people in this subgroup had three or more chronic conditions, compared to 69–73 percent in the three other groups.
Exhibit 1.
Characteristics of high-cost adult patients dually eligible for Medicare and Medicaid in 2010, by age and residence
| Age-residence group | |||||
|---|---|---|---|---|---|
| Community | Nursing home | ||||
| All | Age <65 | Age ≥65 | Age <65 | Age ≥65 | |
| Number | 386,886 | 135,509 | 86,389 | 30,091 | 134,897 |
| Percentage of total | 100% | 35% | 22% | 8% | 35% |
| Patient characteristics | |||||
| Age range (years) | |||||
| 21–54 | 27.0% | 67.6% | —a | 42.9% | —a |
| 55–64 | 15.8 | 32.3 | —a | 57.1 | —a |
| 65–74 | 20.0 | —a | 47.8% | —a | 26.8% |
| 75–84 | 21.0 | —a | 34.4 | —a | 38.1 |
| 85 or more | 16.2 | —a | 17.7 | —a | 35.1 |
| Male | 42.5% | 54.4% | 36.4% | 53.6% | 32.0% |
| Race/ethnicity | |||||
| Whiteb | 71.8% | 72.8% | 66.3% | 68.7% | 74.8% |
| Black | 20.1 | 20.7 | 20.2 | 25.0 | 18.4 |
| Hispanic | 8.1 | 6.4 | 13.5 | 6.3 | 6.8 |
| Chronic conditions | |||||
| Renal disease | 41.1% | 29.3% | 53.8% | 43.3% | 44.4% |
| Congestive heart failure | 36.6 | 19.5 | 51.8 | 32.3 | 44.9 |
| Diabetes mellitus | 41.2 | 27.7 | 51.1 | 50.4 | 46.2 |
| Chronic obstructive lung disease | 28.5 | 15.7 | 37.7 | 31.2 | 34.7 |
| Peripheral vascular disease | 16.5 | 9.5 | 23.4 | 17.8 | 18.7 |
| Coronary artery disease | 13.3 | 8.1 | 22.7 | 10.4 | 13.1 |
| Cancer | 6.7 | 4.7 | 13.1 | 4.5 | 5.2 |
| Depression | 20.3 | 15.2 | 14.7 | 32.8 | 26.3 |
| Cerebrovascular disease and stroke | 13.1 | 5.2 | 14.6 | 18.3 | 19.0 |
| Dementia | 38.4 | 8.8 | 35.6 | 35.1 | 70.6 |
| Parkinson’s or Huntington’s disease | 4.4 | 1.1 | 4.6 | 4.4 | 7.8 |
| Severe mental illness | 21.7 | 23.3 | 12.3 | 41.4 | 21.8 |
| Paralysis | 6.1 | 8.2 | 3.8 | 16.4 | 3.2 |
| Liver disease | 4.4 | 1.1 | 4.6 | 4.4 | 7.8 |
| Hematologic or thrombotic disease | 11.8 | 9.3 | 15.5 | 13.7 | 11.5 |
| Cerebral vascular disease or stroke | 14.2 | 5.7 | 16.3 | 19.7 | 20.3 |
| Number of chronic conditions | |||||
| 0 | 13.8 | 31.5 | 6.6 | 5.1 | 2.5 |
| 1–2 | 28.1 | 35.3 | 22.4 | 25.8 | 24.9 |
| 3–4 | 31.8 | 20.7 | 36.6 | 36.5 | 38.9 |
| 5 or more | 26.4 | 12.6 | 34.3 | 32.7 | 33.8 |
| Number of hospitalizations | 1.76 | 1.65 | 1.98 | 2.23 | 1.63 |
| Spending | |||||
| Payer | |||||
| Medicare and Medicaid | $135,343 | $151,851 | $133,304 | $143,497 | $118,248 |
| Medicare only | 71,803 | 55,591 | 90,900 | 89,168 | 71,986 |
| Medicaid only | 63,540 | 96,320 | 42,523 | 54,404 | 46,373 |
| Ratio of Medicare to Medicaid | 1.13 | 0.58 | 2.14 | 1.64 | 1.55 |
| Medicare spending per capita | |||||
| Inpatientc | $48,164 | $34,472 | $61,825 | $61,899 | $50,107 |
| Professional services | 17,043 | 16,748 | 20,263 | 22,565 | 14,046 |
| Hospice | 2,651 | 293 | 1,519 | 1,881 | 5,915 |
| Home health | 2,388 | 2,016 | 5,616 | 1,100 | 982 |
| Medicaid LTSS spending per capita | |||||
| Inpatient nursing facility | $17,789 | $ 1,620 | $ 2,363 | $44,023 | $38,057 |
| Other facilities | 4,967 | 35,410 | 9,175 | 613 | 206 |
| HCBS adult day care | 2,460 | 5,862 | 1,754 | 74 | 27 |
| Home health and personal care | 4,055 | 4,150 | 10,681 | 531 | 501 |
| Residential care | 12,076 | 28,831 | 7,621 | 593 | 659 |
SOURCE Authors’ analysis of linked Medicare and Medicaid data for 2010. NOTES High-cost patients are those in the top decile of spending in their state. All tests for independence across the four age-residence groups (proportions), and comparisons of each group to the “Age ≥65 community dwelling group” (continuous variables) are significant (p < 0.001). Home and community-based services (HCBS) waivers allow states to provide funding for long-term services and supports (LTSS) in the home or community, instead of in an institutional setting.
Not applicable.
Non-Hispanic whites and other races not listed.
Includes at a skilled nursing facility.
Among all high-cost dual eligibles, Medicare and Medicaid spending was fairly even, with a ratio of Medicare to Medicaid spending of 1.1, but this masks the marked differences across subgroups. It is perhaps surprising, given the high cost of nursing home residence, that high-cost dual eligibles living in nursing homes had Medicare spending that was about 60 percent higher than their Medicaid spending. The only group with higher Medicaid spending than Medicare spending was the subgroup younger than sixty-five living in the community. Among this group, high Medicaid spending was driven largely by the cost of residential care as opposed to in-home services. The greatest areas of spending for the high-cost dual eligibles as a group were acute inpatient services (such as hospitalization) and residential services, whether in a nursing home or in community settings.
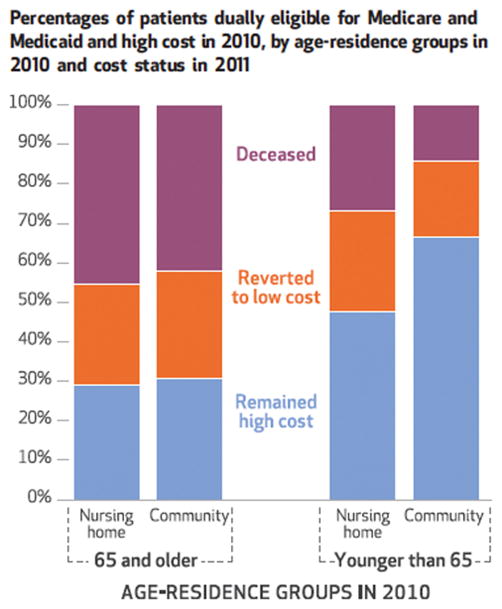
In the second year, only 19–27 percent of high-cost dual eligibles across all age-residence categories reverted to being lower-cost (Exhibit 2). However, the reasons for reversion differed by age. Nearly half of the high-cost dual eligibles ages sixty-five and older in the community or in nursing homes died in 2010 or 2011 and thus did not have ongoing high costs. The small group of adults younger than sixty-five who resided in nursing homes also had a high mortality rate (27 percent), compared to the younger group living in the community (14 percent).
Exhibit 2.
Percentages of patients dually eligible for Medicare and Medicaid and high cost in 2010, by age-residence groups in 2010 and cost status in 2011
Source/Note: SOURCE Authors’ analysis of linked Medicare and Medicaid data for 2010–11. NOTES The test for independence across the four age-residence groups is significant (p < 0.001). High-cost patients are those in the top decile of spending in their state.
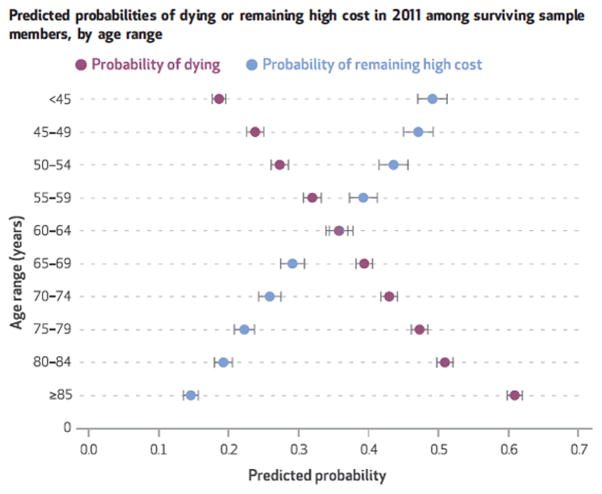
There was a large difference in the predicted probabilities of remaining high cost and of dying that was related to age, independent of other factors (Exhibit 3). Compared to age, other factors (such as specific disease, nursing home residence, race, or sex) had smaller independent associations with death or persistent high costs (for full regression results, see Appendix Table 2).35
Exhibit 3.
Predicted probabilities of dying or remaining high cost in 2011 among surviving sample members, by age range
Source/Notes: SOURCE Authors’ analysis of linked Medicare and Medicaid data for 2010–11. NOTES Predicted probabilities were estimated from a multinomial logistic model that adjusted for sex, race, community versus nursing home residence, whether or not the patient had three or more of sixeen chronic conditions, a flag for each chronic condition, and indicators for state of residence. The error bars indicate 95% confidence intervals. Full regression results are available in online Appendix Table 2 (see Note 35 in text). High-cost patients are those in the top decile of spending in their state.
There was a great deal of similarity in the services used among residents of nursing homes, regardless of age (Exhibit 4). By definition, they all had high nursing home costs, but they also had high use and costs [delete- incurred high costs] for acute inpatient services. Acute inpatient stays drive higher Medicare spending compared with Medicaid spending, despite high nursing facility expenses. This was especially evident among decedents. In fact, among nursing home residents who died before reaching age sixty-five, Medicare inpatient spending was more than twice Medicaid nursing home spending ($78,689 versus $34,381), compared to a less pronounced difference between Medicare and Medicaid spending for older decedents ($54,968 versus $32,889).
Exhibit 4.
Health care utilization and costs in 2010 for high-cost patients dually eligible for Medicare and Medicaid who remained high cost, reverted to lower-cost, or died in 2011, by age-residence groups
| Community | Nursing home | Reverted to lower-cost | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Died | Remained high cost | Died | Remained high cost | ||||||
| Age <65 | Age ≥65 | Age <65 | Age ≥65 | Age <65 | Age ≥65 | Age <65 | Age ≥65 | ||
| Number | 18,321 | 35,963 | 88,088 | 26,747 | 7,830 | 60,773 | 14,168 | 39,470 | 95,526 |
| Percent of total | 5% | 9% | 23% | 7% | 2% | 16% | 4% | 10% | 25% |
| Medicare service use | |||||||||
| Inpatienta | 92% | 95% | 37% | 66% | 91% | 84% | 77% | 73% | 89% |
| Professional services | 100 | 100 | 99 | 100 | 100 | 100 | 99 | 100 | 100 |
| Hospice | 16 | 23 | 0 | 3 | 23 | 35 | 4 | 15 | 5 |
| Home health | 50 | 63 | 17 | 49 | 19 | 15 | 17 | 14 | 41 |
| Medicaid long-term service use | |||||||||
| Inpatient nursing facility | 15% | 26% | 4% | 16% | 94% | 91% | 97% | 94% | 51% |
| Other facilities | 6 | 2 | 27 | 13 | 1 | 0 | 2 | 1 | 3 |
| HCBS waiver and nonwaiver use | |||||||||
| Adult day care | 5% | 4% | 26% | 15% | 1% | 1% | 1% | 1% | 5% |
| Home health | 9 | 12 | 12 | 16 | 3 | 2 | 3 | 2 | 8 |
| Personal care | 23 | 32 | 11 | 28 | 5 | 4 | 5 | 5 | 18 |
| Residential care | 8 | 5 | 36 | 18 | 4 | 4 | 2 | 2 | 6 |
| Other | |||||||||
| Wraparound services | 71 | 67 | 74 | 75 | 69 | 53 | 69 | 55 | 67 |
| Targeted case management | 11 | 7 | 26 | 14 | 4 | 1 | 4 | 2 | 8 |
| HCBS waiver recipient | 26 | 26 | 54 | 40 | 8 | 6 | 7 | 5 | 20 |
| Average spending | |||||||||
| Medicare and Medicaid | $155,403 | $136,860 | $163,328 | $148,163 | $160,824 | $122,534 | $148,071 | $120,460 | $111,851 |
| Medicare only | 120,026 | 112,231 | 34,383 | 64,521 | 114,138 | 80,041 | 82,418 | 64,220 | 76,729 |
| Medicaid only | 35,377 | 24,628 | 128,994 | 83,642 | 46,685 | 42,492 | 65,652 | 56,240 | 35,122 |
| Ratio of Medicare to Medicaid | 3.4 | 4.6 | 0.3 | 0.8 | 2.4 | 1.9 | 1.3 | 1.1 | 2.2 |
| Medicare spending per capita | |||||||||
| Inpatienta | $82,390 | $80,326 | $18,618 | $37,543 | $78,689 | $54,968 | $54,712 | $42,200 | $54,374 |
| Professional services | 29,952 | 22,576 | 12,453 | 19,120 | 28,756 | 15,164 | 23,512 | 14,757 | 16,357 |
| Hospice | 1,503 | 2,533 | 91 | 884 | 3,850 | 8,093 | 1,323 | 5,256 | 1,329 |
| Home health | 3,332 | 5,235 | 1,403 | 5,154 | 1,031 | 852 | 997 | 916 | 3,173 |
| Medicaid LTSS spending per capita | |||||||||
| Inpatient nursing facility | 1,380 | 2,117 | 1,930 | 3,588 | 34,381 | 32,889 | 54,581 | 47,741 | 16,636 |
| Other facilities | 8,427 | 2,592 | 51,105 | 24,902 | 300 | 86 | 980 | 441 | 1,914 |
| HCBS waiver and nonwaiver | |||||||||
| Adult day care | 1,038 | 478 | 8,340 | 4,554 | 31 | 19 | 96 | 34 | 576 |
| Home health | 943 | 3,429 | 1,560 | 8,742 | 191 | 234 | 235 | 297 | 1,508 |
| Personal care | 2,499 | 4,380 | 2,865 | 7,312 | 198 | 197 | 330 | 276 | 2,111 |
| Residential care | 5,471 | 2,183 | 40,593 | 20,273 | 610 | 815 | 669 | 654 | 2,991 |
| Other | |||||||||
| Wraparound services | 4,650 | 3,452 | 10,510 | 6,437 | 1,490 | 684 | 1,926 | 821 | 3,361 |
SOURCE Authors’ analysis of linked Medicare and Medicaid data for 2010–11. NOTES All tests for independence across the nine age-residence-spending groups (proportions) and comparisons of each group to “Age ≥65, living in the community and remained high cost” are significant (p < 0.001). High-cost patients are those in the top decile of spending in their state. The “reverted to lower-cost” group is not split into age-residence groups for ease of presentation. Home and community-based services (HCBS) waivers allow states to provide funding for long-term services and supports (LTSS) in the home or community, instead of in an institutional setting. Percentages may not sum to 100 because of rounding.
Includes at a skilled nursing facility.
Among community-dwelling dual eligibles, there was a striking difference in the ratio of Medicare to Medicaid spending between those who died and those who remained high cost. Among those who died, Medicare spending was about 3.4 or 4.6 times Medicaid spending, while the relationship was reversed among those who remained high cost (0.3 or 0.8 times Medicaid spending). This difference was largely due to decedents’ high utilization of acute inpatient and professional services, while persistently high-cost beneficiaries incurred high spending for long-term services and supports for inpatient care and residential services. The net effect was similar levels of combined Medicare and Medicaid spending but very different patterns in the types of services accounting for that spending. In addition, community-dwelling dual eligibles who survived and had persistently high spending also accessed home and community based services more frequently through Medicaid Waiver programs, compared with decedents. Waivers allow flexibility in the use of home and community-based services.
The contrast between the services used by younger and older community-dwelling dual eligibles warrants mention. First, high-cost dual eligibles ages sixty-five and older receiving end-of-life care had more utilization of [spending for-delete] hospice, nursing home, and Medicare-based home care services than did younger community-dwelling dual eligibles near the end of life (Medicare-reimbursed home care is intended to address short-term needs instead of providing long-term support.) Persistently high-cost community-dwelling dual eligibles ages sixty-five and older likewise used more [delete - incurred more spending for] Medicare-based home care, as opposed to home and community-based long-term services and supports, compared to those younger than sixty-five.
Second, even though dual eligibles younger than sixty-five used more [delete - incurred more spending for] home and community-based services, they still had high spending for long-term services and supports in institutional settings. These settings include nursing homes, intermediate care facilities for people with intellectual disabilities, psychiatric facilities, and residential facilities. Use of residential care and inpatient long-term services and supports paid by Medicaid was over two times higher for younger persistently high-cost duals than for older ones.
Discussion
Dually eligible beneficiaries with high combined Medicare and Medicaid spending fall into two main groups: older beneficiaries nearing the end of life who experience acute hospitalizations and facility-based long-term services and supports care and a younger, community-dwelling group using sustained functional support services in residential settings as well as having high hospital use. An examination of the differences in utilization [delete spending incurred] by these groups for home and community-based long-term services and supports, as opposed to institutional or acute care services, reveals opportunities for improvement for both groups.
The first important insight is that among high-cost dual eligibles ages sixty-five and older, nearly half die and one-quarter revert to lower spending levels by the end of the following year, leaving only about 30 percent persistently high cost (Exhibit 2). This differs dramatically from high-cost community-dwelling dual eligibles younger than sixty-five, two-thirds of whom remain high cost. Previous studies of the persistence of high spending reported that approximately 40 percent of Medicare beneficiaries older than sixty-five remained high cost,21 which is not very different from our result. But the discussion of those findings tends to focus on the implications for those who are persistently high cost, not on how best to serve high-need adults who require medical and supportive services during the short but intense period near the end of life.
It may be more actionable to identify people who are likely to be nearing the end of life, as opposed to likely to be high cost, because the care can be redirected toward the need for intense palliative services for a relatively fixed period of time. The literature suggests that among frail older populations, such as the high-cost elderly dual eligibles we studied, it is possible to predict who is likely to die—although more work is needed to generalize these prediction models to the younger dual eligible population.36–38 Another approach would be to increase palliative care services in the particular settings frequently used by dual eligibles who are highly likely to die in the next year. Those settings include not only nursing homes but also Medicare-reimbursed home care and hospitals.
The second important insight is that 57 percent of high-cost dual eligibles reside in the community and not in nursing homes (Exhibit 1). Within the community-dwelling group, the older high-cost dual eligibles use fewer home and community-based long-term services and supports than younger dual eligibles (Exhibit 4). The difference may be related to eligibility criteria or lengthy delays between application and enrollment, but it also suggests an opportunity to reduce reliance on acute care settings through increased use of home and community-based services. Among younger disabled adults, resources for keeping people as closely linked to the community as possible, such as residential and intermediate care, are in place to facilitate transitions to more independent settings in the community. For older dual eligibles who reside in the community, the current care patterns suggest that as people develop functional limitations and illnesses, they are more likely to use acute, episodic services such as hospitalization and postacute rehabilitation services in response to status changes than to use an anticipatory strategy that relies on long-term services and supports designed to provide ongoing community-based support. The more frequent use of stable, long-term supportive services for older dual eligibles in the community provided by Medicaid, coupled with a focus on meeting their palliative care needs, could reduce their use of acute inpatient settings and nursing facilities.
The third insight is that high-cost dual eligibles often use costly inpatient settings, including all types of acute care hospitals (medical, psychiatric, and rehabilitation) and inpatient long-term services and supports settings, in addition to nursing homes. Among high-cost dual eligibles residing in nursing homes, spending in Medicare exceeds Medicaid nursing home spending largely because of high spending for acute inpatient stays, with even higher acute inpatient spending among dual eligibles younger than sixty-five than among older people. We found the same high spending for acute stays among community-dwelling decedents. Among the younger community-dwelling dual eligibles who remain high cost, spending on other types of inpatient long-term services and supports, such as Medicaid-covered psychiatric facilities and other nonacute care hospitals, is very high (Exhibit 4).
The high use of inpatient care, both acute and in long-term services and supports, for younger dual eligibles suggests that an expansion of medical services and psychiatric care or increased attention to transitions for this segment of the dually eligible population could be explored as a way to improve care and reduce the need for acute hospitalization. Ongoing efforts such as implementation of the INTERACT model to improve transitions to the hospital from nursing homes are examples of a successful strategy that might also have value in other types of long-term services and supports settings.39
Another program, the Dual Eligible Special Needs Plans (D-SNPs), may provide a model that, if successful, could be expanded to a wider population of dual eligibles. D-SNPs are Medicare Advantage plans that provide a managed care option for dual eligibles with high medical and support needs. They are required to contract with states and expected to coordinate services across Medicare and Medicaid. The program’s performance to date demonstrates the challenges of reducing spending in this population, but a subset of D-SNPS called Fully Integrated D-SNPs (FIDE SNPs) that are designed to integrate Medicare and Medicaid benefits has shown better quality outcomes than standard D-SNPs.11 While enrollment in D-SNPs has been increasing since the program was established in 2003, 64 percent of enrollees are concentrated in ten states that have significant experience with managed long-term services and supports.40 To facilitate dissemination of this model, additional studies that demonstrate how FIDE SNPs organize and deliver care to achieve improved outcomes in this high-risk group are needed.
Conclusion
High-cost dual eligibles are a heterogeneous group comprised by older adults nearing the end of life, who use both nursing home and acute hospital care, and community-dwelling people younger than sixty-five who need sustained residential care and other types of long-term services and supports as well as general acute care hospitals. Tailored approaches to these distinct populations are likely to yield care of more value to patients and their families, and to have the potential to lower costs if patients’ needs can be met with fewer stays in short-term inpatient facilities.
Supplementary Material
Acknowledgments
The authors acknowledge their funders, the John A. Hartford Foundation and National Institute of Aging (Grant No. P01 AG19783). They also acknowledge Jared Wasserman at the Dartmouth Institute for his contributions to developing the Medicaid data used in this project.
Contributor Information
Julie P. W. Bynum, Associate professor of medicine at the Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth, in Lebanon, New Hampshire
Andrea Austin, Research scientist at the Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth.
Donald Carmichael, Statistical research analyst at the Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth.
Ellen Meara, Professor of the Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth and a research associate at the National Bureau of Economic Research, in Cambridge, Massachusetts.
Notes
- 1.Congressional Budget Office. The federal budget in 2015: an infographic [Internet] Washington (DC): CBO; 2016. Jan 6, [cited 2017 May 16]. Available from: https://www.cbo.gov/publication/51110. [Google Scholar]
- 2.Klees BS, Wolfe CJ, Curtis CA. Brief summaries of Medicare and Medicaid: Title XVIII and Title XIX of the Social Security Act as of November 10, 2016 [Internet] Baltimore (MD): Centers for Medicare and Medicaid Services; 2016. [cited 2017 May 16]. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MedicareProgramRatesStats/Downloads/MedicareMedicaidSummaries2016.pdf. [Google Scholar]
- 3.California HealthCare Foundation. Where the money goes: understanding Medi-Cal’s high-cost beneficiaries [Internet] Oakland (CA): CHCF; 2010. Jul, [cited on 2017 May 16]. Available from: http://www.chcf.org/publications/2010/07/where-the-money-goes-understanding-medicals-high-cost-beneficiaries. [Google Scholar]
- 4.Reschovsky JD, Hadley J, Saiontz-Martinez CB, Boukus ER. Following the money: factors associated with the cost of treating high-cost Medicare beneficiaries. Health Serv Res. 2011;46(4):997–1021. doi: 10.1111/j.1475-6773.2011.01242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Medicare Payment Advisory Commission. A data book: health care spending and the Medicare program [Internet] Washington (DC): MedPACp; 2016. Jun, [cited 2017 May 16]. Available from: http://www.medpac.gov/docs/default-source/data-book/june-2016-data-book-health-care-spending-and-the-medicare-program.pdf. [Google Scholar]
- 6.Berk ML, Monheit AC. The concentration of health care expenditures, revisited. Health Aff (Millwood) 2001;20(2):9–18. doi: 10.1377/hlthaff.20.2.9. [DOI] [PubMed] [Google Scholar]
- 7.Cohen SB, Yu W. The concentration and persistence in the level of health expenditures over time: estimates for the U.S. population, 2007–2008. Rockville (MD): Agency for Healthcare Research and Quality; 2010. Dec, [Internet] [cited 2017 May 16]. (Statistical Brief No. 309). Available from: https://meps.ahrq.gov/data_files/publications/st309/stat309.shtml. [Google Scholar]
- 8.Stanton MW. The high concentration of U.S. health care expenditures. Rockville (MD): Agency for Healthcare Research and Quality; 2006. [Internet] [cited on 2017 May 16l]. (Publication No. 06-0060). Available from: https://archive.ahrq.gov/research/findings/factsheets/costs/expriach/ [Google Scholar]
- 9.Coughlin TA, Waidmann TA, Phadera L. Among dual eligibles, identifying the highest-cost individuals could help in crafting more targeted and effective responses. Health Aff (Millwood) 2012;31(5):1083–91. doi: 10.1377/hlthaff.2011.0729. [DOI] [PubMed] [Google Scholar]
- 10.Gold MR, Jacobson GA, Garfield RL. There is little experience and limited data to support policy making on integrated care for dual eligibles. Health Aff (Millwood) 2012;31(6):1176–85. doi: 10.1377/hlthaff.2012.0162. [DOI] [PubMed] [Google Scholar]
- 11.Government Accountability Office. Disabled dual-eligible beneficiaries: integration of Medicare and Medicaid benefits may not lead to expected Medicare savings [Internet] Washington (DC): GAO; 2014. Aug, [cited 2017 May 16]. Available from: https://www.gao.gov/assets/670/665491.pdf. [Google Scholar]
- 12.Johnson SR. Reform update: N.Y. joins controversial care-coordination pilot for dual-eligibles. Modern Healthcare [serial on the Internet] 2013 Aug 27; [cited 2017 May 16]. Available from: http://www.modernhealthcare.com/article/20130827/NEWS/308279967.
- 13.Congressional Budget Office. Dual-eligible beneficiaries of Medicare and Medicaid: characteristics, health care spending, and evolving policies [Internet] Washington (DC): CBO; 2013. Jun, [cited on 2017 May 16]. Available from: https://www.cbo.gov/sites/default/files/113th-congress-2013-2014/reports/44308dualeligibles2.pdf. [Google Scholar]
- 14.Gold MR, Jacobson G, Damino A, Neuman T. Special Needs Plans: availability and enrollment [Internet] Menlo Park (CA): Henry J. Kaiser Family Foundation; 2011. Sep, [cited 2017 May 16]. Available from: https://kaiserfamilyfoundation.files.wordpress.com/2013/01/8229.pdf. [Google Scholar]
- 15.CMS.gov. Chronic conditions chartbook: 2011 edition [Internet] Baltimore (MD): Centers for Medicare and Medicaid Services; 2011. Dec, [cited on 2017 May 16]. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/2011ChartBook.html. [Google Scholar]
- 16.Kasper J, O’Malley Watts M, Lyons B. Chronic disease and co-morbidity among dual eligibles: implications for patterns of Medicaid and Medicare service use and spending. Washington (DC): Kaiser Commission on Medicaid and the Uninsured; 2010. Jul, [cited 2017 May 16]. Available from: https://kaiserfamilyfoundation.files.wordpress.com/2013/01/8081.pdf. [Google Scholar]
- 17.Kronick RG, Bella M, Gilmer TP. The faces of Medicaid III: fefining the portrait of people with multiple chronic conditions [Internet] Hamilton (NJ): Center for Health Care Strategies; 2009. Oct, [cited 2017 May 16]. Available from: http://www.chcs.org/media/Faces_of_Medicaid_III.pdf. [Google Scholar]
- 18.Nesse RE. The demographics and economics of chronic disease. Health Aff (Millwood) 2002;21:w125–6. doi: 10.1377/hlthaff.w2.125. [DOI] [PubMed] [Google Scholar]
- 19.Lewin Group. Individuals living in the community with chronic conditions and functional limitations: a closer look [Internet] Washington (DC): Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation; 2010. Jan, [cited 2017 May 16l ]. Available from: https://aspe.hhs.gov/system/files/pdf/75961/closerlook.pdf. [Google Scholar]
- 20.Thorpe KE, Howard DH. The rise in spending among Medicare beneficiaries: the role of chronic disease prevalence and changes in treatment intensity. Health Aff (Millwood) 2006;25(5):w378–88. doi: 10.1377/hlthaff.25.w378. doi:10/1377/hlthaff.25.w378. [DOI] [PubMed] [Google Scholar]
- 21.Congressional Budget Office. High-cost Medicare beneficiaries [Internet] Washington (DC): Congressional Budget Office; 2005. May, [cited 2017 May 16]. Available from: https://www.cbo.gov/sites/default/files/cbofiles/ftpdocs/63xx/doc6332/05-03-medispending.pdf. [Google Scholar]
- 22.Bynum JP, Rabins PV, Weller W, Niefeld M, Anderson GF, Wu AW. The relationship between a dementia diagnosis, chronic illness, Medicare expenditures, and hospital use. J Am Geriatr Soc. 2004;52(2):187–94. doi: 10.1111/j.1532-5415.2004.52054.x. [DOI] [PubMed] [Google Scholar]
- 23.Findley P, Shen C, Sambamoorthi U. Multimorbidity and persistent depression among veterans with diabetes, heart disease, and hypertension. Health Soc Work. 2011;36(2):109–19. doi: 10.1093/hsw/36.2.109. [DOI] [PubMed] [Google Scholar]
- 24.Kurdyak PA, Gnam WH, Goering P, Chong A, Alter DA. The relationship between depressive symptoms, health service consumption, and prognosis after acute myocardial infarction: a prospective cohort study. BMC Health Serv Res. 2008;8:200. doi: 10.1186/1472-6963-8-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Welch CA, Czerwinski D, Ghimire B, Bertsimas D. Depression and costs of health care. Psychosomatics. 2009;50(4):392–401. doi: 10.1176/appi.psy.50.4.392. [DOI] [PubMed] [Google Scholar]
- 26.Boyd C, Leff B, Weiss C, Wolff J, Hamblin A, Martin L. Clarifying multimorbidity patterns to improve targeting and delivery of clinical services for Medicaid populations [Internet] Hamilton (NJ): Center for Health Care Strategies; 2010. Dec, [cited 2017 May 16]. Available from: http://www.chcs.org/media/clarifying_multimorbidity_patterns.pdf. [Google Scholar]
- 27.Kaiser Commission on Medicaid and the Uninsured. Dual eligibles: Medicaid’s role for low-income Medicare beneficiaries [Internet] Washington (DC): The Commission; 2011. May, [cited 2017 May 16l]. Available from: http://www.kff.org/medicaid/4091.cfm. [Google Scholar]
- 28.Machlin S, Cohen S, Yu W. Health care access and expenditures among non-elderly adults with multiple chronic conditions: variations by insurance coverage status, 2007–2008 [Internet] Rockville (MD): Agency for Healthcare Research and Quality; 2011. Apr, [cited 2017 May 16]. (Statistical Brief No. 320). Available from: https://meps.ahrq.gov/data_files/publications/st320/stat320.pdf. [Google Scholar]
- 29.Sevick MA, Zucconi S, Sereika S, Puczynski S, Drury R, Marra R, et al. Characteristics and health service utilization patterns of ventilator-dependent patients cared for within a vertically integrated health system. Am J Crit Care. 1992;1(3):45–51. [PubMed] [Google Scholar]
- 30.Davis MA, Nallamothu BK, Banerjee M, Bynum JP. Identification of four unique spending patterns among older adults in the last year of life challenges standard assumptions. Health Aff (Millwood) 2016;35(7):1316–23. doi: 10.1377/hlthaff.2015.1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Riley GF, Lubitz JD. Long-term trends in Medicare payments in the last year of life. Health Serv Res. 2010;45(2):565–76. doi: 10.1111/j.1475-6773.2010.01082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hogan C, Lunney J, Gabel J, Lynn J. Medicare beneficiaries’ costs of care in the last year of life. Health Aff (Millwood) 2001;20(4):188–95. doi: 10.1377/hlthaff.20.4.188. [DOI] [PubMed] [Google Scholar]
- 33.The states were AL, AK, AR, CA, CT, DE, FL, GA, ID, IL, IN, IA, MD, MA, MI, MN, MO, MS, MT, NV, NH, NM, NY, NC, ND, OH, OK, OR, PA, RI, SC, TX, UT, WA, WV, WY.
- 34.Medicaid Analytic eXtract (MAX) general information [Internet] Baltimore (MD): Centers for Medicare and Medicaid Services; Anomaly reports can be found at CMS.gov. [last modified 2017 Apr 20; cited 2017 May 16]. Availble from: https://www.cms.gov/research-statistics-data-and-systems/computer-data-and-systems/medicaiddatasourcesgeninfo/maxgeneralinformation.html. [Google Scholar]
- 35.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 36.Justice AC, Covinsky KE, Berlin JA. Assessing the generalizability of prognostic information. Ann Intern Med. 1999;130(6):515–24. doi: 10.7326/0003-4819-130-6-199903160-00016. [DOI] [PubMed] [Google Scholar]
- 37.Yourman LC, Lee SJ, Schonberg MA, Widera EW, Smith AK. Prognostic indices for older adults: a systematic review. JAMA. 2012;307(2):182–92. doi: 10.1001/jama.2011.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Amblàs-Novellas J, Murray SA, Espaulella J, Martori JC, Oller R, Martinez-Muñoz M, et al. Identifying patients with advanced chronic conditions for a progressive palliative care approach: a cross-sectional study of prognostic indicators related to end-of-life trajectories. BMJ Open. 2016;6(9):e012340. doi: 10.1136/bmjopen-2016-012340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ouslander JG, Bonner A, Herndon L, Shutes J. The Interventions to Reduce Acute Care Transfers (INTERACT) quality improvement program: an overview for medical directors and primary care clinicians in long term care. J Am Med Dir Assoc. 2014;15(3):162–70. doi: 10.1016/j.jamda.2013.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Verdier J, Kruse A, Lester RS, Philip AM, Chelminsky D. State contracting with Medicare Advantage Dual Eligible Special Needs Plans: issues and options [Internet] Princeton (NJ): Integrated Care Resource Center; 2015. Feb, [cited 2017 May 16]. Available from: http://www.chcs.org/media/ICRC-Issues-and-Options-in-Contracting-with-D-SNPs-FINAL.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.