Abstract
Objective
Our purpose was to identify the main food contributors to energy and nutrient intake in children with chronic kidney disease (CKD).
Methods
In this cross-sectional study of dietary intake assessed using Food Frequency Questionnaires (FFQ) in the Chronic Kidney Disease in Children (CKiD) cohort study, we estimated energy and nutrient intake and identified the primary contributing foods within this population.
Results
Completed FFQs were available for analysis in 658 children. Of those, 69.9% were boys, median age 12 years (interquartile range (IQR): 8, 15 years). The average daily energy intake was 1968 kcal/day (IQR: 1523 – 2574 kcal/day). Milk was the largest contributor to total energy, protein, potassium, and phosphorus intake. Fast foods were the largest contributors to fat and sodium intake, the second largest contributors to energy intake, and the third largest contributors to potassium and phosphorus intake. Fruit contributed 12.0%, 8.7% and 6.7% to potassium intake for children aged 2–5, 6–13 and 14–18 years old, respectively.
Conclusions
Children with CKD consumed more sodium, protein, and calories but less potassium than recommended by the National Kidney Foundation guidelines for pediatric CKD. Energy, protein, and sodium intake is heavily driven by consumption of milk and fast foods. Limiting the contribution of fast foods to diet in patients with good appetite may be particularly important for maintaining recommended energy and sodium intake, as overconsumption can increase the risk of obesity and cardiovascular complications in this population.
Keywords: Nutrients intake, Food, Children, Adolescents, Chronic Kidney Disease
Introduction
Optimizing nutritional intake to improve nutritional status is an essential aspect of pediatric chronic kidney disease (CKD) clinical management [1, 2]. Dietary guidance is frequently provided in clinical practice in order to optimize growth and achieve favorable serum chemistry profiles. Dietary guidelines for children with CKD are available [3], with target intakes for protein, sodium, potassium, phosphorus, and total calories, with recommended dietary adjustments based on laboratory monitoring.
Studies of children with CKD have indicated that diet quality and nutrient intake decrease as kidney function declines [4]. Anorexia and poor appetite are common in children with CKD and contribute to inadequate nutrient and caloric intake [5, 6]. Any nutritional intervention to address inadequate intake or abnormal nutritional indexes must focus on dietary composition. However, little is known about diet composition in these children and there is little guidance for clinicians on how best to aid a patient achieve the recommended dietary intake.
We evaluated dietary intake of children with CKD and identified the main food contributors to energy and nutrients intake with the aim of providing information to care providers for tailoring nutritional advice to these children. We contextualized the findings by comparing them to data from the general population.
Methods
Study Design
The Chronic Kidney Disease in Children (CKiD) study is an ongoing multicenter prospective cohort study of children with mild-to-moderate CKD from 57 clinical sites in the United States and Canada. Eligibility criteria for enrollment into the CKiD study included: age 1–16 years, estimated glomerular filtration rate (eGFR) [7] 30–90 ml/1.73 m2, and no previous organ transplantation. The primary glomerular diagnoses were focal segmental glomerulosclerosis (FSG), and hemolytic uremic syndrome (HUS), while primary non-glomerular diagnoses included obstructive uropathy, aplastic/hypoplastic/dysplastic kidneys, and reflux nephropathy. A detailed description of the CKiD study population and study design has been previously reported [7, 8]. The study protocol was approved by the Institutional Review Boards of each participating center and informed consent was obtained from all participants.
Dietary assessment
The Child Harvard Service Food Frequency Questionnaire (HSFFQ) was used to assess dietary intake in the CKiD study. This tool was adapted from the Food Frequency Questionnaire (FFQ) developed and evaluated by Willett et al [9] and designed to be self-administered. However, unlike the original Willett FFQ which focused mainly on intake during the last year, the child HSFFQ was designed to reflect the child’s usual eating habits in the prior 28 days and is validated in Native American and Caucasian children aged 1–5 years old, and in pregnant women [10, 11]. Three similar age-specific versions (2–5, 6–13 and 14–18 years old) were adopted in the CKiD study targeting children aged 1–18 years and assessing dietary information on a total of 86 or 87 food items (depending upon age group). The FFQ was completed by the study coordinator through interview or self-administered by children or their guardian(s). Self-reported intake frequencies (ranging from never in the past 28 days to >6 times per day) were converted to times per day, and estimated portion sizes derived from the general population were applied to estimate daily total consumption for each item [12, 13]. Daily nutrient and caloric intake was then extracted from overall food item consumption using the Nutrition Data System for Research (NDSR, version 2013). Total energy and nutrient intake (including protein, fat, carbohydrate, sodium, potassium and phosphorus) for every child were computed as the sum over all food items. The analysis was restricted to participants who had completed at least 75% of the questionnaire at the baseline visit, with total energy intake in the range 500 to 5000 kcal and percent estimated energy requirement (%EER) between the 2.5th and the 97.5th percentile.
Food grouping
Individual food items were aggregated into 36 mutually exclusive food groups based on the USDA Dietary Sources of Nutrients (DSN) database [14], NHANES classifications of food groups [15], and input from clinical dietitians. Food mixtures were not disaggregated. Fast foods were amalgamated into one composite group that included hamburgers, hotdogs, tacos, burritos, and French fries. Food groups were further subdivided when appropriate to enable better discernment of specific nutrient intake. For example, fruit was assessed as a single group contributing to energy intake, but bananas (given their high potassium content) were treated as a distinct food group when quantifying potassium intake. Food classifications used in this analysis are presented in Supplemental Table 1.
Patient demographic and clinical data
Height and weight were determined as the mean of two independent measurements using a stadiometer and a standing scale, respectively. Age-sex-specific height, weight and body mass index (BMI) z-scores were calculated using US Centers for Disease Control and Prevention (CDC) growth charts from normative data [16]. Family income, race and maternal education information were collected at the baseline visit. Plasma disappearance of iohexol was used to assess glomerular filtration rate (GFR). When GFR could not be directly measured, eGFR from published equations derived from the CKiD population was substituted [7].
Serum potassium, phosphate and albumin were centrally measured enzymaticallyas were total protein and urine creatinine concentrations, on a Bayer Advia 2400 analyzer (Siemns Diagnosis, Tarrytown, NY). Hypoalbuminemia was defined as serum albumin < 3.8 g/dl. Elevated serum phosphate was defined as > 6.5 mg/dl for children <13 years old and > 4.5 mg/dl for children > 13 years. Elevated serum potassium was defined as > 5.2 mEq/L.
Statistical Analyses
Continuous variables are expressed as median and interquartile range (IQR), and categorical variables as frequencies and proportions. Energy and nutrient intake, as well as %EER are described by age category. The mean proportion of each food group/item was calculated as described by Krebs-Smith SM et al [17]. Proportional contributions of each food group to energy and nutrient (carbohydrate, fat, protein, sodium, potassium and phosphorus) intakes were calculated by summing the nutrient content across items within a food group (e.g. cheese) and dividing by the total nutrient intake across all food items for an individual. Food groups were then ranked in terms of their contribution to the energy and nutrient totals. The five top food contributors to sodium, potassium and phosphorus for each age group were compared. When quantitative comparison was appropriate, Wilcoxon signed-rank tests were used to compare the mean contribution of food categories in children with CKD to those in the general population. Statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC). All tests were two-sided and a P value of <0.05 was considered statistically significant.
Results
Baseline Data and Dietary intake
Of the 732 children who provided dietary intake information, 658 children completed >75% of the FFQ at baseline. Compared with the excluded group, children that were included in the analysis were more likely to be Caucasian (68% vs. 54%, P < 0.01), have higher family income (33% vs. 12%, P < 0.01) and higher maternal educational attainment (college, 63% vs. 42%, P < 0.01). Characteristics of the 658 children are presented in Table 1; 59.9% were boys, median age was 12 (IQR: 8, 15) years and median eGFR was 53.5 (IQR: 38.9, 73.5) ml/min/1.73 m2. More than two thirds had not received dietary counseling in clinics (Table 2).
Table 1.
Baseline characteristics of the participants.
| Variables | Median (IQR) or N (%) |
|---|---|
| Male | 394 (59.9) |
| Age (yrs) | 12 (8, 15) |
| Weight z-score | 0.1 (−0.8, 1.0) |
| Height z-score | −0.5 (−1.3, 0.3) |
| BMI z-score | 0.5 (−0.3, 1.4) |
| BMI z-score ≤ −2 | 15 (2.3) |
| BMI z-score ≥ 2 | 62 (9.6) |
| Glomerular disease | 203 (30.9) |
| GFR (ml/min/1.73m2) | 53.5 (38.9, 73.5) |
| Maternal education | |
| High school | 244 (37.9) |
| College and more | 400 (62.1) |
| Race | |
| Caucasian | 447 (67.9) |
| African-American | 97 (14.7) |
| Other | 114 (17.4) |
| Annual Family income | |
| Less than $36000 | 256 (38.9) |
| $36000 to $75000 | 182 (27.7) |
| More than $75000 | 220 (33.4) |
| Hypoalbuminemia | 51 (7.8 ) |
| Hyperkalemia | 45 (7.0) |
| Hyperphosphatemia | 84 (13.1) |
Table 2.
Dietary intakes of energy and nutrients in children with CKD by age at baseline.
| 2–3 years old n=39 |
4–8 years old n=164 |
9–13 years old n=235 |
14–18 years old n=220 |
Overall N=658 |
|
|---|---|---|---|---|---|
| Energy | |||||
| kcal/kg/day | 101 (85, 137) | 86 (63, 109) | 46 (32, 65) | 37 (27, 51) | 52 (34, 80) |
| %EER | 114 (98, 163) | 119 (93, 156) | 91 (66, 125) | 92 (70, 125) | |
| Carbohydrate | |||||
| g/kg/day | 14.3 (11.1, 18.8) | 11.6 (8.2, 15.0) | 5.8 (4.1, 8.5) | 5.0 (3.5, 7.2) | 6.8 (4.4, 10.6) |
| % energy* | 53 (50, 60) | 53 (49, 58) | 52 (47, 56) | 54 (49, 59) | |
| Fat | |||||
| g/kg/day | 3.8 (3.2, 5.3) | 3.1 (2.4, 4.3) | 1.8 (1.2, 2.4) | 1.4 (1.0, 2.0) | 2.0 (1.3, 3.1) |
| % energy* | 34 (30, 38) | 35 (32, 38) | 35 (31, 39) | 34 (30, 37) | |
| Protein | |||||
| g/kg/day | 3.4 (3.0,4.8) | 2.8 (2.1, 3.8) | 1.6 (1.1, 2.2) | 1.3 (1.0, 2.0) | 1.8 (1.2, 2.7) |
| % energy* | 13 (12, 15) | 14 (12, 15) | 14 (12, 16) | 14 (12, 15) | |
| %RDA | 456 ± 168 | 365 ± 172 | 209 ± 119 | 168 ± 85 | |
| Sodium | |||||
| mg/day/kg | 154 (126, 208) | 122 (95, 183) | 74 (49, 99) | 62 (42, 84) | 83 (55, 122) |
| %AI | 238 ± 95 | 265 ± 117 | 207 ± 84 | 274 ± 115 | |
| Potassium | |||||
| mg/kg/day | 146 (125, 202) | 108 (79, 135) | 58 (40, 79) | 49 (33, 66) | 66 (42, 102) |
| %AI | 46 ± 15 | 54 ± 25 | 53 ± 22 | 69 ± 31 | |
| Phosphorus | |||||
| mg/kg/day | 72 (57, 92) | 52 (36, 67) | 28 (20, 38) | 21(15, 32) | 31 (20, 49) |
| %RDA | 81 ± 25 | 98 ± 45 | 96 ± 38 | 116 ± 49 |
Percentage of energy derived from macronutrients; EER – Estimated Energy Requirement, AI – Adequate Intake, RDA – Recommended Dietary Allowance, CKD – Chronic Kidney Disease
Contributions to energy and macronutrients
Dietary sources of energy and protein are presented in Tables 3 and 4, respectively; macronutrients are presented in greater detail in Supplemental Tables 2–5.
Table 3.
Food/food groups source of energy in CKD children among 2–18 years old a
| Ranking | Food groups/itemsa | Mean (%) | Cumulative (%) |
|---|---|---|---|
| 1 | Milk | 7.7 | 7.7 |
| 2 | Fast foods | 6.8 | 14.5 |
| 3 | Bread and rolls | 6.6 | 21.1 |
| 4 | Fruit | 6.1 | 27.2 |
| 5 | Crackers, popcorn, pretzels, chips | 5.6 | 32.8 |
| 6 | Poultry products | 5.3 | 38.1 |
| 7 | Pasta | 5.1 | 43.2 |
| 8 | Beverages | 4.5 | 47.7 |
| 9 | Ready-to-eat cereals | 4.2 | 51.9 |
| 10 | Candy, chocolate and sugary foods | 4.2 | 56.1 |
| 11 | Fruit juice | 3.4 | 59.5 |
| 12 | Pork products | 3.2 | 62.7 |
| 13 | Milk products | 3.1 | 65.8 |
| 14 | Cake, cookies and pie | 3.0 | 68.8 |
| 15 | Biscuit, corn bread, pancakes | 2.8 | 71.6 |
| 16 | Cheese | 2.6 | 74.2 |
| 17 | Nuts and seeds | 2.6 | 76.8 |
| 18 | Yogurt | 2.4 | 79.2 |
| 19 | Pizza | 2.3 | 81.5 |
| 20 | Mayonnaise and Salad dressing | 2.2 | 83.7 |
Food groups (n = 11) contributing at least 1% in descending order: eggs, potatoes, beef, rice, other vegetables, coffee and tea, butter and margarine, vegetable soup and other soup, Fish and fish products, sausage and luncheon meats, and legumes.
Table 4.
Food/food groups source of protein in CKD children among 2–18 years old a
| Ranking | Food groups/itemsa | Mean (%) | Cumulative (%) |
|---|---|---|---|
| 1 | Milk | 13.8 | 13.8 |
| 2 | Poultry products | 12.0 | 25.8 |
| 3 | Fast foods | 8.4 | 34.2 |
| 4 | Pork products | 7.3 | 41.5 |
| 5 | Bread and rolls | 5.4 | 46.9 |
| 6 | Pasta | 5.1 | 52.0 |
| 7 | Cheese | 3.7 | 55.7 |
| 8 | Fish and fish products | 3.7 | 59.4 |
| 9 | Beef | 3.5 | 62.9 |
| 10 | Eggs | 3.4 | 66.3 |
| 11 | Pizza | 3.4 | 69.7 |
| 12 | Nuts and seeds | 3.2 | 72.9 |
| 13 | Yogurt | 3.0 | 75.9 |
| 14 | Ready-to-eat cereals | 2.6 | 78.5 |
| 15 | Chips, crackers, popcorn, pretzels | 2.2 | 80.7 |
| 16 | Biscuit, corn bread, pancakes | 2.1 | 82.8 |
Food groups (n = 10) contributing at least 1% in descending order: sausage and luncheon meats, fruit, legume, candy, chocolate and sugary foods, milk products, vegetable soup and other soup, corn and peas, other vegetables, potatoes, and rice.
Energy intake
Twenty food groups/items each contributed at least 2% to energy intake representing 84% of total energy intake. Median energy intake was 52 (IQR: 34, 80) kcal/kg/day (Table 2) and median EER was 100% (IQR: 75%, 135%). Milk was the top contributor providing 7.7% of total energy intake, which was not significantly different from the general population (7.7% vs. 7.0%, P = 0.27) [15]. Other major contributors were fast foods (6.8%), bread and rolls (6.6%), fruit (6.1%), chips, crackers, popcorn, pretzels (5.6%), poultry products (5.3%) and pasta (5.1%).
Protein intake
Median protein intake of the overall cohort was 1.8 (IQR: 1.2, 2.7) g/kg/day (Table 2), and protein intake in all age groups was higher than the recommended daily allowance (RDA) in healthy children (range: 100–140%). Milk was also the largest food source for protein, contributing 13.8% of the total protein intake on average, which was similar to that reported in the general population (13.2%, p=0.17) [15]. Other important contributors included poultry products (12.0%), fast foods (8.4%), pork products (7.4%) and bread and rolls (5.4%). Restricting to animal protein intake, the highest contributors were milk (19.9%), poultry products (17.4%), pork products (10.8%) and fast foods (10.4%). Restricting to vegetable protein, the highest contributors were bread and rolls (14.9%) and pasta (14.0%).
Carbohydrate intake
The main sources of carbohydrates were fruit (11.4%), bread and rolls (8.6%), beverages (8.3%), pasta (6.7%) and ready-to-eat cereals (6.6%). The contribution of fruit to carbohydrate intake in children with CKD was significantly higher than in the general population (11.4% vs. 3.9%, P < 0.01) [15].
Fat intake
The main food sources for fat intake were fast foods (10.5%), poultry products (8.6%), chips, crackers, popcorn, pretzels (8.2%), milk (7.3%) and cheese (5.8%).
Contribution to sodium, potassium and phosphorus
Dietary sources for sodium and potassium are presented in Tables 5 and 6, and for phosphorus are presented in Supplemental Table 6.
Table 5.
Food/food groups source of sodium in CKD children among 2–18 years old a
| Ranking | Food groups/items | Mean (%) | Cumulative (%) |
|---|---|---|---|
| 1 | Fast foods | 9.4 | 9.4 |
| 2 | Cheese | 7.1 | 16.5 |
| 3 | Poultry products | 6.0 | 22.5 |
| 4 | Bread and rolls | 5.7 | 28.2 |
| 5 | Chips, crackers, popcorn, pretzels | 5.6 | 33.8 |
| 6 | Ready-to-eat cereals | 5.0 | 38.8 |
| 7 | Pork products | 4.9 | 43.7 |
| 8 | Tomato and tomato sauce | 4.8 | 48.5 |
| 9 | Milk | 4.6 | 53.1 |
| 10 | Vegetable soup and other soup | 4.5 | 57.6 |
| 11 | Eggs | 4.1 | 61.7 |
| 12 | Biscuit, corn bread, pancakes | 3.9 | 65.6 |
| 13 | Pasta | 3.6 | 69.2 |
| 14 | Pizza | 3.1 | 72.4 |
| 15 | Rice | 3.0 | 75.4 |
| 16 | Sausage and luncheon meats | 2.8 | 78.2 |
| 17 | Broccoli, Spinach and greens | 2.5 | 80.6 |
| 18 | Mayonnaise and Salad dressing | 2.4 | 83.0 |
| 19 | Legume (beans) | 2.1 | 85.1 |
| 20 | Fish and fish products | 2.0 | 87.1 |
Food groups (n = 5) contributing at least 1% in descending order: corn and peas, beverages, other vegetables, milk products, nuts and seeds.
Table 6.
Food/food groups source of potassium in CKD children among 2–18 years old a
| Ranking | Food groups/items | Mean (%) | Cumulative (%) |
|---|---|---|---|
| 1 | Milk | 15.9 | 15.9 |
| 2 | Fruit | 8.5 | 24.4 |
| 3 | Fast foods | 7.4 | 31.8 |
| 4 | Fruit juice | 7.0 | 38.8 |
| 5 | Potatoes | 4.9 | 43.8 |
| 6 | Tomato and tomato sauce | 3.9 | 47.7 |
| 7 | Yogurt | 3.4 | 51.1 |
| 8 | Banana | 3.3 | 54.4 |
| 9 | Pork products | 3.1 | 57.5 |
| 10 | Vegetable soup and other soup | 3.0 | 60.6 |
| 11 | Ready-to-eat cereals | 3.0 | 63.5 |
| 12 | Poultry products | 3.0 | 66.5 |
| 13 | Milk products | 3.0 | 69.4 |
| 14 | Carrot, sweet potatoes and squash | 2.9 | 72.3 |
| 15 | Nuts and seeds | 2.3 | 74.6 |
| 16 | Other vegetables | 2.3 | 76.9 |
| 17 | Legume (beans) | 2.2 | 79.1 |
Food groups (n = 12) contributing at least 1% in descending order: chips, crackers, popcorn, pretzels, bread and rolls, pasta, pizza, corn and peas, broccoli, spinach and greens, beverage, beef, candy, chocolate and sugary foods, eggs, fish and fish products, biscuit, corn bread, pancakes.
Sodium intake
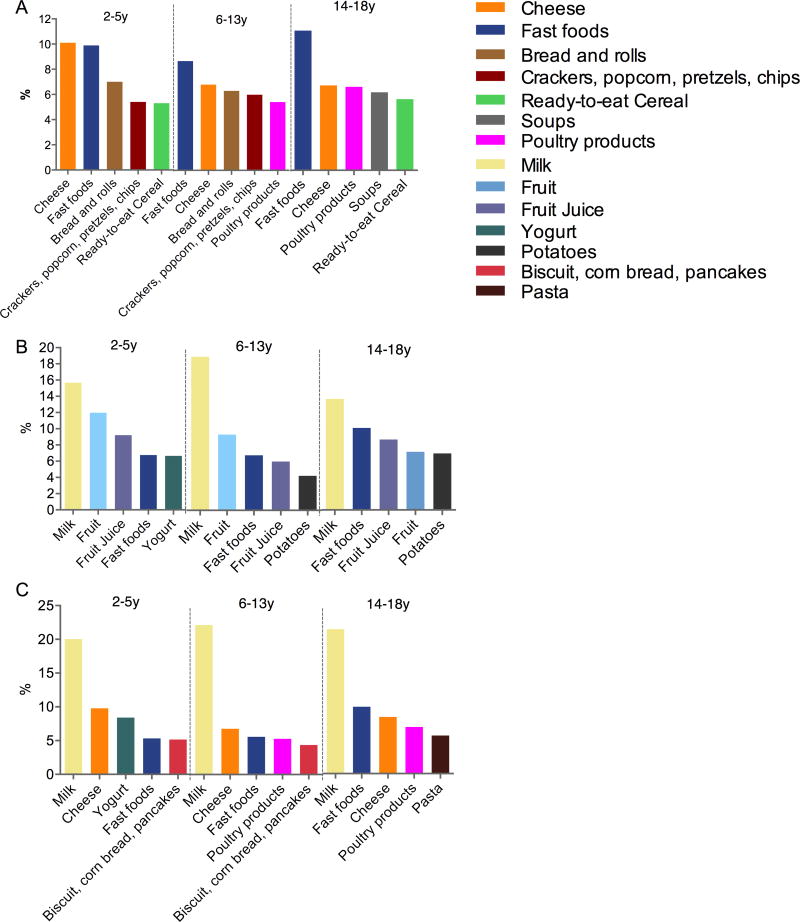
The median sodium intake in the cohort was 83 (IQR: 55, 122) mg /kg/day, which is higher than the recommended level [range: 100% adequate intake (AI) in all age groups] (Table 2). Fast foods were the largest single source of sodium, contributing 9.4% of the total. Other major sources for sodium intake included cheese (7.1%), poultry products (6.0%), bread and rolls (5.7%) and chips, crackers, popcorn, pretzels (5.6%). Stratifying by age group, cheese (10.0%) was the top contributor to sodium intake in children aged 2–5 years old, while fast foods were the main source of sodium for children aged 6–13 (8.8%) and 14–18 (10.2%) years (Figure 1, panel A).
Figure 1.
Top five food sources for sodium, potassium and phosphorus by age A: sodium, B: potassium, C: phosphorus
Potassium and Phosphorus intake
Median potassium intake was 66 (IQR: 42, 102) mg/kg/day while median phosphorus intake was 31 (IQR: 20, 49) mg/kg/day (Table 2). Milk was the largest single contributor to both potassium (15.9%) and phosphorus (20.3%) intake. Compared with percentage contribution (18.8%) in the general population, the contribution of milk to potassium intake in the cohort was significantly lower (P < 0.01). Other important dietary sources of potassium were fruit (excluding bananas; 8.5%), fast foods (7.4%), fruit juice (7.0%) and potatoes (4.9%) and of phosphorus were cheese (7.2%), fast foods (6.3%), poultry products (5.2%) and biscuits, corn bread, pancakes and tortillas (4.5%). By age group, milk was the main potassium and phosphorus source across all ages (Figure 1, panels B and C); fruit contribution to potassium intake for children of 2–5, 6–13 and 14–18 years old were 12.0%, 8.7% and 6.7%, respectively.
Differences in nutrient intake and food contributors by eGFR
Nutrient and energy intake and food contributors were compared across strata of eGFR (<60 ml/min/1.73m2 vs. ≥60 ml/min/1.73m2); no significant differences were found. In addition, food contributors to energy, sodium, potassium and phosphorus intake were also very similar between groups (data not shown).
Discussion
Malnutrition has been reported in children with CKD and can affect growth [2, 18]. Nutritional counseling and intervention is regarded as an effective method for optimizing growth and biochemical balance in children with CKD. However, dietary adherence is poor [19]. This study aimed to identify the main food contributors to energy and nutrients intake in children with CKD and compare them with data from the general population [15, 20] to help determine dietary intervention and counseling strategies.
As noted in healthy children, milk was the top contributor to energy intake. Milk and dairy products are the primary dietary sources of energy, high-quality protein and other nutrients for children in many countries [21]. However, fast foods were the second largest food source of energy, contributing 6.8% to total energy intake. Three food groups (chips/crackers/popcorn/pretzels, beverages and candy/chocolate/sugary foods) contributed calories but added minimal nutritional value. This suggests that children in our cohort over-consume energy-dense, nutrient-poor foods, as has been reported for the general population [22]. Dietary guidelines recommend that children with CKD consume 100% of the age-specific EER individually adjusted for physical activity. Maintaining normal energy intake is important for growth in children with CKD. However, overconsumption of energy may lead to the further complication of obesity [1, 23], which is associated with faster progression of CKD and higher mortality rates in the adult population [24]. Our results suggest that a large percentage of children in the CKiD cohort achieve energy intake levels consistent with and sometimes greater than the EER. A decrease of 50% in the intake of fast food, beverages, chips/crackers/popcorn/pretzels and candy/chocolate/sugary foods could reduce average energy intake in our cohort by 11%, which would eliminate over-consumption in 20% of children in the CKiD cohort who have excess energy intake.
Protein-energy malnutrition is a known complication in children with CKD [18]. Dietary protein intake often decreases as kidney function declines [25, 26]. Within this study however, dietary protein intake in all age groups was higher than the recommended level (range: 100–140% RDA). Excessive protein intake has been reported to impact renal function in adult patients with CKD [27]. A low protein intake in children with CKD has not been shown to delay CKD progression, though it is widely recommended for adult patients [28]. Protein restriction in children with CKD must be cautiously used due to the very important role protein plays in growth. In terms of sources of protein, animal sources (milk, poultry products, fast foods and pork products) contributed to 41.5% of the overall protein intake. Although there is no recommendation for the relative contribution of animal- and plant-based sources of protein, a primary recommendation of the 2010 dietary guideline for Americans is to shift food intake patterns towards a plant-based diet.
Sodium intake was much higher within this cohort than recommended, but similar to the trend observed in the US population [29]. Fast foods contributed 9.4% of the total sodium intake in children with CKD and was higher in the older age group, consistent with a general population trend towards increased processed meat consumption and decreased fruit and dairy consumption as children age [30–32]. High sodium intake is associated with elevated blood pressure and risk of hypertension in children [33]. A randomized trial in adult CKD patients indicated that the CKD population might be more salt sensitive, and a low sodium diet could effectively reduce blood pressure as well as the incidence of cardiovascular complications [34, 35].
Milk was the main source for potassium within this cohort contributing 15.9% to the total. Fruit was the second largest contributor at 8.5%, indicating that children in our study had a relatively high frequency of fruit consumption. However, the overall potassium intake was still lower than recommended, similar to trends in the general population [36]. Only 7% of children in CKD cohort had hyperkalemia – a clinical indicator that could motivate a reduction in potassium intake – suggesting that low potassium intake in the cohort is not the result of clinical factors. The 2010 dietary guidelines for the general population urged increasing dietary intake of fruit, as US children and adolescent intake have consistently failed to meet recommended levels [22, 37, 38] and most children with CKD would similarly benefit from increased fruit consumption and potassium intake.
There are notable limitations in our study. Although FFQs are useful for evaluating long-term dietary habits of children, they are often subject to poor recall, low response rates and intake overestimation [39]. Portion sizes from the general US population were applied to estimate daily energy and nutrient intake, which simplified the questionnaire but underrepresents the variability in portion sizes across the CKiD cohort. In addition, dietary intake may be overestimated in the 4.9% of CKiD participants who reported poor appetite at baseline. Finally, we are unable to accurately estimate absolute intake. However, our findings are useful as an epidemiologic and clinical guide to understanding relative nutritional intake in children with CKD and important food contributors.
Conclusion
Characterizing the major contributors to energy and nutrients in children with CKD is an important part of understanding dietary intake and improving nutritional counseling. Our findings suggest that children with CKD overconsume sodium, protein, and calories relative to recommendations by the National Kidney Foundation. These dietary intake trends within our cohort of children with CKD were similar to that of the general pediatric population. Higher fruit and vegetable intake has been recommended for children in general and may be particularly important in this vulnerable population at risk of acidosis and other blood chemistry imbalances. Limiting intake of fast foods, salty snacks, candies and sugared beverages in patients with good appetite may help children avoid obesity and hypertension that can result from overconsumption of these calorie-dense high-sodium foods.
Supplementary Material
Acknowledgments
Data in this manuscript were collected by the Chronic Kidney Disease in children prospective cohort study (CKiD) with clinical coordinating centers (Principal Investigators) at Children’s Mercy Hospital and the University of Missouri - Kansas City (Bradley Warady, MD) and Children’s Hospital of Philadelphia (Susan Furth, MD, PhD), Central Biochemistry Laboratory (George Schwartz, MD) at the University of Rochester Medical Center, and data coordinating center (Alvaro Muñoz, PhD) at the Johns Hopkins Bloomberg School of Public Health. The CKiD Study is supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases, with additional funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and the National Heart, Lung, and Blood Institute (U01-DK-66143, U01-DK-66174, U01DK-082194, U01-DK-66116). The CKiD website is located at https://www.statepi.jhsph.edu/ckid. We also acknowledge the China Scholarship Council for funding support to Wen Chen.
Abbreviations
- AI
Adequate Intake
- CKiD
Chronic Kidney Disease in Children
- CKD
Chronic kidney disease
- DSN
Dietary Sources of Nutrients
- eGFR
Estimated glomerular filtration rate
- EER
Estimated energy, requirement
- FFQ
Food frequency questionnaire
- IQR
interquartile range
- NHANES
National Health and Nutrition Examination Survey
- NKF
National Kidney Foundation
- RDA
Recommended Dietary Allowance
Footnotes
Ethical statement
The study design and conduct were approved by an external study monitoring board appointed by the National Institute of Diabetes and Digestive and Kidney Diseases and by the institutional review boards of each participating center.
None of the authors declare a conflict of interest.
References
- 1.Norman LJ, Macdonald IA, Watson AR. Optimising nutrition in chronic renal insufficiency--growth. Pediatr Nephrol. 2004;19:1245–1252. doi: 10.1007/s00467-004-1580-3. [DOI] [PubMed] [Google Scholar]
- 2.Apostolou A, Printza N, Karagiozoglou-Lampoudi T, Dotis J, Papachristou F. Nutrition assessment of children with advanced stages of chronic kidney disease-A single center study. Hippokratia. 2014;18:212–216. [PMC free article] [PubMed] [Google Scholar]
- 3.KDOQI Work Group. KDOQI Clinical Practice Guideline for Nutrition in Children with CKD: 2008 update. Executive summary. Am J Kidney Dis. 2009;53:S1–S124. doi: 10.1053/j.ajkd.2008.11.017. [DOI] [PubMed] [Google Scholar]
- 4.Kim H, Lim H, Choue R. Compromised Diet Quality is Associated with Decreased Renal Function in Children with Chronic Kidney Disease. Clin Nutr Res. 2014;3:142–149. doi: 10.7762/cnr.2014.3.2.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheung WW, Paik KH, Mak RH. Inflammation and cachexia in chronic kidney disease. Pediatr Nephrol. 2010;25:711–724. doi: 10.1007/s00467-009-1427-z. [DOI] [PubMed] [Google Scholar]
- 6.Mak RH, Cheung W, Cone RD, Marks DL. Orexigenic and anorexigenic mechanisms in the control of nutrition in chronic kidney disease. Pediatr Nephrol. 2005;20:427–431. doi: 10.1007/s00467-004-1789-1. [DOI] [PubMed] [Google Scholar]
- 7.Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL. New equations to estimate GFR in children with CKD. J Am Soc Nephrol. 2009;20:629–637. doi: 10.1681/ASN.2008030287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Furth SL, Cole SR, Moxey-Mims M, Kaskel F, Mak R, Schwartz G, Wong C, Munoz A, Warady BA. Design and methods of the Chronic Kidney Disease in Children (CKiD) prospective cohort study. Clin J Am Soc Nephrol. 2006;1:1006–1015. doi: 10.2215/CJN.01941205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J, Hennekens CH, Speizer FE. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol. 1985;122:51–65. doi: 10.1093/oxfordjournals.aje.a114086. [DOI] [PubMed] [Google Scholar]
- 10.Blum RE, Wei EK, Rockett HR, Langeliers JD, Leppert J, Gardner JD, Colditz GA. Validation of a food frequency questionnaire in Native American and Caucasian children 1 to 5 years of age. Matern Child Health J. 1999;3:167–172. doi: 10.1023/a:1022350023163. [DOI] [PubMed] [Google Scholar]
- 11.Baer HJ, Blum RE, Rockett HR, Leppert J, Gardner JD, Suitor CW, Colditz GA. Use of a food frequency questionnaire in American Indian and Caucasian pregnant women: a validation study. BMC Public Health. 2005;5:135. doi: 10.1186/1471-2458-5-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murphy SPYA, West Suitor C, Moats S. Child and Adult Care Food Program: Aligning Dietary Guidance for All. Food and Nutrition Board; Institute of Medicine; Washington DC: 2011. [PubMed] [Google Scholar]
- 13.Rockett HR, Colditz GA. Assessing diets of children and adolescents. Am J Clin Nutr. 1997;65:1116S–1122S. doi: 10.1093/ajcn/65.4.1116S. [DOI] [PubMed] [Google Scholar]
- 14.US Department of Agriculture ARS, Nutrient Data Laboratory. USDA National Nutrient Database for Standard Reference, Release 28 2015 Sep; [Google Scholar]
- 15.Keast DR, Fulgoni VL, 3rd, Nicklas TA, O’Neil CE. Food sources of energy and nutrients among children in the United States: National Health and Nutrition Examination Survey 2003–2006. Nutrients. 2013;5:283–301. doi: 10.3390/nu5010283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, Johnson CL. 2000 CDC Growth Charts for the United States: methods and development. Vital and health statistics 11. 2002;246:1–190. [PubMed] [Google Scholar]
- 17.Krebs-Smith SM, Kott PS, Guenther PM. Mean proportion and population proportion: two answers to the same question? J Am Diet Assoc. 1989;89:671–676. [PubMed] [Google Scholar]
- 18.Mastrangelo A, Paglialonga F, Edefonti A. Assessment of nutritional status in children with chronic kidney disease and on dialysis. Pediatr Nephrol. 2014;29:1349–1358. doi: 10.1007/s00467-013-2612-7. [DOI] [PubMed] [Google Scholar]
- 19.Apostolou A, Karagiozoglou-Lampoudi T. Dietary adherence in children with chronic kidney disease: a review of the evidence. J Ren Care. 2014;40:125–130. doi: 10.1111/jorc.12069. [DOI] [PubMed] [Google Scholar]
- 20.Reedy J, Krebs-Smith SM. Dietary sources of energy, solid fats, and added sugars among children and adolescents in the United States. J Am Diet Assoc. 2010;110:1477–1484. doi: 10.1016/j.jada.2010.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dror DK, Allen LH. Dairy product intake in children and adolescents in developed countries: trends, nutritional contribution, and a review of association with health outcomes. Nutr Rev. 2014;72:68–81. doi: 10.1111/nure.12078. [DOI] [PubMed] [Google Scholar]
- 22.Krebs-Smith SM, Guenther PM, Subar AF, Kirkpatrick SI, Dodd KW. Americans do not meet federal dietary recommendations. J Nutr. 2010;140:1832–1838. doi: 10.3945/jn.110.124826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Navaneethan SD, Kirwan JP, Arrigain S, Schreiber MJ, Sehgal AR, Schold JD. Overweight, obesity and intentional weight loss in chronic kidney disease: NHANES 1999-2006. Int J Obes. 2012;36:1585–1590. doi: 10.1038/ijo.2012.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lu JL, Kalantar-Zadeh K, Ma JZ, Quarles LD, Kovesdy CP. Association of body mass index with outcomes in patients with CKD. J Am Soc Nephrol. 2014;25:2088–2096. doi: 10.1681/ASN.2013070754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ikizler TA, Greene JH, Wingard RL, Parker RA, Hakim RM. Spontaneous dietary protein intake during progression of chronic renal failure. J Am Soc Nephrol. 1995;6:1386–1391. doi: 10.1681/ASN.V651386. [DOI] [PubMed] [Google Scholar]
- 26.Quan A, Baum M. Protein losses in children on continuous cycler peritoneal dialysis. Pediatr Nephrol. 1996;10:728–731. doi: 10.1007/s004670050200. [DOI] [PubMed] [Google Scholar]
- 27.Kovesdy CP, Kalantar-Zadeh K. Back to the future: restricted protein intake for conservative management of CKD, triple goals of renoprotection, uremia mitigation, and nutritional health. Int Urol Nephrol. 2016;48:725–729. doi: 10.1007/s11255-016-1224-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wingen A-M, Fabian-Bach C, Schaefer F, Mehls O. Randomised multicentre study of a low-protein diet on the progression of chronic renal failure in children. Lancet. 1997;349:1117–1123. doi: 10.1016/s0140-6736(96)09260-4. [DOI] [PubMed] [Google Scholar]
- 29.Grimes CA, Wright JD, Liu K, Nowson CA, Loria CM. Dietary sodium intake is associated with total fluid and sugar-sweetened beverage consumption in US children and adolescents aged 2–18 y: NHANES 2005–2008. Am J Clin Nutr. 2013;98:189–196. doi: 10.3945/ajcn.112.051508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cooke LJ, Wardle J. Age and gender differences in children’s food preferences. Br J Nutr. 2007;93:741. doi: 10.1079/bjn20051389. [DOI] [PubMed] [Google Scholar]
- 31.Alexy U, Kersting M, Remer T. Potential renal acid load in the diet of children and adolescents: impact of food groups, age and time trends. Public Health Nutr. 2008;11:300–306. doi: 10.1017/S1368980007000328. [DOI] [PubMed] [Google Scholar]
- 32.Washi SA, Ageib MB. Poor diet quality and food habits are related to impaired nutritional status in 13- to 18-year-old adolescents in Jeddah. Nutr Res. 2010;30:527–534. doi: 10.1016/j.nutres.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 33.Yang Q, Zhang Z, Kuklina EV, Fang J, Ayala C, Hong Y, Loustalot F, Dai S, Gunn JP, Tian N, Cogswell ME, Merritt R. Sodium intake and blood pressure among US children and adolescents. Pediatrics. 2012;130:611–619. doi: 10.1542/peds.2011-3870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McMahon EJ, Bauer JD, Hawley CM, Isbel NM, Stowasser M, Johnson DW, Campbell KL. A randomized trial of dietary sodium restriction in CKD. J Am Soc Nephrol. 2013;24:2096–2103. doi: 10.1681/ASN.2013030285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nerbass FB, Pecoits-Filho R, McIntyre NJ, McIntyre CW, Taal MW. High sodium intake is associated with important risk factors in a large cohort of chronic kidney disease patients. Eur J Clin Nutr. 2015;69:786–790. doi: 10.1038/ejcn.2014.215. [DOI] [PubMed] [Google Scholar]
- 36.Tian N, Zhang Z, Loustalot F, Yang Q, Cogswell ME. Sodium and potassium intakes among US infants and preschool children, 2003–2010. Am J Clin Nutr. 2013;98:1113–1122. doi: 10.3945/ajcn.113.060012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guenther PM, Dodd KW, Reedy J, Krebs-Smith SM. Most Americans eat much less than recommended amounts of fruits and vegetables. J Am Diet Assoc. 2006;106:1371–1379. doi: 10.1016/j.jada.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 38.McGuire S. U.S. Department of Agriculture and U.S. Department of Health and Human Services, Dietary Guidelines for Americans, 2010. 7th Edition, Washington, DC: U.S. Government Printing Office, January 2011. Adv Nutr. 2011;2:293–294. doi: 10.3945/an.111.000430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cade J, Thompson R, Burley V, Warm D. Development, validation and utilisation of food-frequency questionnaires - a review. Public Health Nutr. 2002;5:567–587. doi: 10.1079/PHN2001318. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.